Abstract
Objectives. This study assessed progress in achieving clean indoor air in California.
Methods. Data were from large, cross-sectional population-based surveys (1990–1999).
Results. Indoor workers reporting smoke-free workplaces increased from 35.0% (95% confidence interval [CI] = 33.7, 36.3) in 1990 to 93.4% (95% CI = 92.6, 94.2) in 1999. Exposure of nonsmoking indoor workers to secondhand tobacco smoke decreased from 29.0% (95% CI = 27.2, 30.8) to 15.6% (95% CI = 14.1, 17.1). Adults with smoke-free homes increased from 37.6 % (95% CI = 35.1, 40.1) in 1992 to 73.7% (95% CI = 73.2, 74.2) in 1999; nearly half of smokers in 1999 had smoke-free homes. In 1999, 82.2% (95% CI = 81.5, 82.9) of children and adolescents (0–17 years) had smoke-free homes, up from 38.0% (95% CI = 35.1, 40.9) in 1992.
Conclusions. California's advances highlight an important opportunity for tobacco control.
The health hazards of secondhand smoke to nonsmokers were first recognized in the 1972 US surgeon general's report.1 Following numerous population and laboratory investigations, the 1986 surgeon general's report reviewed all of the accumulated evidence and confirmed the health threat.2 Ordinances restricting smoking in public places, including the workplace, became increasingly common.3 Advocacy for clean air came largely from private organizations such as Americans for Nonsmokers' Rights.
The first comprehensive state governmental tobacco control program was initiated in California in 1988, funded by the $0.25 per pack excise tax increase passed by voters as Proposition 99.4 This program was based on accumulated knowledge concerning the most effective tobacco use prevention strategies documented to date, as eventually outlined by the National Cancer Institute.5 Although the importance of clean indoor air was recognized, smoking restrictions in public places, including worksites, were mainly viewed as a means for promoting smoking cessation and for establishing societal antismoking norms. Worksites were seen as a venue for delivery of smoking cessation assistance, and smoking restrictions were promoted as economically beneficial to the employer.5 Another early study suggested that smoke-free workplaces and college settings might interrupt smoking initiation.6
Initially, the California Tobacco Control Program did not include nonsmokers among its “target populations” for whom it established goals.7 Prompted by the release in 1992 of the US Environmental Protection Agency report on the dangers of secondhand smoke,8 protection of nonsmokers from secondhand smoke in the workplace became a program goal.9 A further review published in 1995 by the California Environmental Protection Agency10 and later more widely circulated as a National Cancer Institute monograph11 implicated secondhand smoke not only as a cause of cancer but also as a cause of heart disease and as a contributing cause of respiratory and auricular morbidity in young children. In 1997, clean indoor air in the workplace and for children at school and in the home were touted as program accomplishments, and protection of all nonsmokers from secondhand smoke became a clearly articulated program goal.12
The first statewide law (Assembly Bill 13) mandating clean air in indoor workplaces was enacted in California in 1994; however, application of this law to gaming clubs, bars and taverns, and bar areas of restaurants was delayed until January 1, 1998. Compliance with this law may be problematic in some settings, so monitoring exposure of nonsmokers to secondhand smoke in the workplace is important.
Whereas smoke-free workplaces are now mandated by law in California, smoking restrictions in the home are by agreement among household members. National data indicate that smokers who have smoke-free workplaces are more likely to live in smoke-free homes.13 Workplace smoking restrictions may help establish norms against smoking around nonsmokers and make people more aware of the dangers of secondhand smoke. Having a smoke-free home is the most effective step parents can take to reduce their children's exposure to secondhand smoke.14 A recent study indicated that protection of adolescents with smoking parents occurred in smoke-free homes but not in homes with lesser or no restrictions.15
In this article, we present trends from large population-based surveys of Californians, conducted in 1990, 1992, 1993, 1996, and 1999, indicating that the California Tobacco Control Program has been highly successful in its goal of promoting clean indoor air both in the workplace and in the home.
METHODS
The California Tobacco Surveys
The California Tobacco Surveys are randomdigit-dialed telephone surveys conducted periodically to evaluate the California Tobacco Control Program. A 5-minute screening interview with a household adult (18 years or older) enumerates all household residents and obtains demographic information, including age and smoking status. For the 1990, 1992, 1996, and 1999 California Tobacco Surveys, some adults listed were randomly selected for an extended interview (approximately 25 minutes), with selection probability lower for persons who had not smoked in the last 5 years. Table 1 ▶ presents the details of the various California Tobacco Surveys, and more information is available in summary and technical reports.16
TABLE 1—
Characteristics of California Tobacco Surveys (1990, 1992, 1993, 1996, and 1999)
| 1990 | 1992 | 1993 | 1996 | 1999 | |
| Households | |||||
| Sample | 42 790 | 14 736 | 44 172 | 71 989 | 91 174 |
| Successfully screened | 32 135 | 10 774 | 30 910 | 39 674 | 46 590 |
| Response rate | 75.1% | 73.1% | 70.0% | 55.1% | 51.1% |
| Adult extended interview | |||||
| Enumerateda | 65 139 | 21 870 | 61 848 | 78 337 | 93 555 |
| Targetedb | 32 266 | 11 532 | 30 910c | 25 546 | 21 538 |
| 26 372c | |||||
| Successfully interviewed | 24 296 | 7263 | 30 716c | 18 616 | 14 729 |
| 25 812c | |||||
| Response rate | 75.3% | 71.3% | 99.4%c | 72.9% | 68.4%c |
| 97.9%c |
aPersons aged 18 years or older in household as enumerated by screening respondent.
bPersons targeted for an extended interview.
cBrief interview with screening respondent.
In 1993, because of budgetary constraints, no adult extended interview was done; instead, a brief interview (approximately 5 minutes) was conducted with the screener respondent. In 1996, in addition to the adult extended interview, the brief interview was conducted with the screener respondent (if not selected for an extended interview) so that the methodology would be comparable to that of 1993. Subsequent analyses showed that the estimates from the 1996 adult extended and brief interviews (for the common questions) were very close. Consequently, the 1999 California Tobacco Survey used the same design as the 1990 and 1992 California Tobacco Surveys.
Each survey was weighted so that population estimates could be computed. First, base weights were computed from the probability of household selection and the probability of being selected for an extended interview.16 These base weights were then ratio adjusted to the latest available California census data.
Survey Questions Analyzed
Survey items analyzed for this study included demographics, smoking status, employment status, exposure to smoking in the workplace, presence of smoking restrictions in the home, and exposure to secondhand smoke in places other than the workplace and home. These questions had slight differences in some years, which are delineated in the following paragraphs. However, it is highly unlikely that the observed changes in secondhand smoke exposure were because of these differences.
Smoking status.
In 1990, 1992, and 1993, respondents to the adult extended interview were asked, “Do you smoke cigarettes now?” In 1996 and 1999, the question was changed (“Do you currently smoke cigarettes every day, some days, or not at all?”) to be consistent with national surveys.17,18 Respondents to the 1990, 1992, and 1993 adult extended interviews were classified as current smokers if they answered “yes” to the smoke-now question, and respondents to the 1996 and 1999 adult extended interviews were classified as current smokers if they responded “every day” or “some days.” The remaining respondents were classified as nonsmokers. In 1996, the screener interview retained the older smoke-now question. The new smoking status question was expected to produce slightly higher population smoking prevalence estimates because some respondents who might not admit to smoking now (i.e., being a current smoker) might admit to smoking some days. Screening data on smoking status (including proxy reports) were used to assess whether there were adult smokers in the household.
Smoke-free workplaces and exposure to secondhand smoke.
In 1990 and 1992, respondents were asked, “Which of the following best describes your current employment status? Self-employed, employed by someone else, not employed, or retired.” Those selfemployed or employed by someone else were asked, “Do you currently work outside your home?” Those answering “yes” were asked, “Do you work primarily indoors or outdoors?” Indoor workers outside the home were asked, “Do you/does your employer have an official policy that restricts smoking in any way?” If the answer to that question was “yes,” respondents were asked 2 further questions: “Which of the following best describes (your/your employer's) smoking policy for indoor public or common areas, such as lobbies, rest rooms, and lunch rooms?” and “Which of the following best describes (your/your employer's) smoking policy for areas in which employees work?” The response choices for these 2 questions were (1) not allowed in any, (2) allowed in some, and (3) allowed in all. For the current analysis, we report the percentage of indoor workers who answered “not allowed in any” to both questions. Such workplaces are considered smoke-free. Indoor nonsmoking workers also were asked, “During the past 2 weeks, has anyone smoked in the area in which you work?”
In 1993, only nonsmokers were asked about workplace smoking restrictions. Because previous research indicated that smokers and nonsmokers answer differently,19 the 1993 data were not analyzed for this study. However, as in the 1990 and 1992 surveys, nonsmoking indoor workers in 1993 were asked the question about anyone smoking in their work area in the past 2 weeks.
In 1996 and 1999, all respondents were asked, “Do you currently work for money in an indoor setting, such as an office, plant, or store, outside of your home?” Because nearly all indoor workplaces (except bars and game rooms) should have been smoke-free by law, those who answered “yes” were asked, “Is your place of work completely smoke-free indoors?” Again, nonsmokers were asked the question about exposure to anyone smoking in their work area in the past 2 weeks.
To assess compliance with the smoke-free workplace law, the 1999 California Tobacco Survey asked, “What best describes where you currently work outside your home for money? Do you work (1) in an office, (2) in a plant or factory, (3) in a store or warehouse, (4) in a classroom, (5) in a hospital, (6) in a restaurant or bar, (7) in a vehicle, or (8) in some other indoor setting?” Indoor workers who stated that their workplace was not smoke-free were asked, “For each of the following indoor areas in your building, is smoking allowed in: (1) any indoor work areas, (2) a special smoking room or lounge, (3) a break room or cafeteria, or (4) a hallway or lobby?”
Smoke-free homes.
The 1992 California Tobacco Survey was the first to include a question about smoking restrictions in the home. In that survey, adults who answered the extended interview were asked, “What are the smoking rules or restrictions in your household, if any?'' Respondents could answer as follows: (1) smoking is completely banned, (2) smoking is generally banned with few exceptions, (3) smoking is allowed in some rooms only, or (4) there are no restrictions on smoking. The first answer choice defined a smoke-free home. The 1993, 1996, and 1999 California Tobacco Surveys asked this question of the screener respondent, and the 1996 and 1999 California Tobacco Surveys also asked the question on the adult extended interview. To compute the rate of report of smoke-free homes for smokers, their response was the one considered, but to establish the overall percentage of smoke-free homes or the percentage of children and adolescents living in smoke-free homes, the screener respondent's answer was used. In 1992, only households that had at least 1 completed adult interview could be analyzed, and the least stringent response was used.
Exposure to secondhand smoke outside of work or the home.
The 1999 California Tobacco Survey included the question, “In California, in the past 6 months, that is, since [date computed], have you had to put up with someone smoking near you at any other place besides your home or your workplace?” Respondents answering “yes” were asked, “The last time this happened in California, where were you?” The question was open ended, but the interviewer had precoded categories for the following answers: (1) restaurant, (2) restaurant bar, (3) bar or tavern, (4) pool hall, (5) shopping mall, (6) public park/outdoors, (7) community event, (8) sports event, (9) another person's home, (10) another person's automobile, (11) game room/casino/bingo hall, or (12) other—specify. For the current analysis, we grouped pool hall with game room/casino/bingo hall and community event with sports event.
Statistics
All analyses were performed with the WesVarPC statistical package,20 which takes into account the survey sample designs and uses a jackknife procedure for variance estimation.21 All percentages are reported with 95% confidence intervals (CIs).
RESULTS
Clean Indoor Air in the Workplace
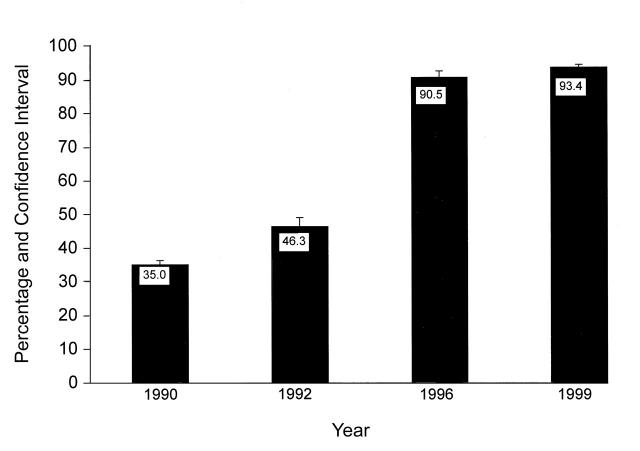
Figure 1 ▶ shows the increase from 1990 to 1999 in the percentage of California indoor workers reporting smoke-free workplaces. In 1990, only 35.0% (95% CI = 33.7, 36.3) of California indoor workers reported working in a clean air environment, but this percentage increased to 93.4% (95% CI = 92.6, 94.2) by 1999. In 1999, indoor workers not reporting smoke-free workplaces could have answered affirmatively about more than 1 of the following workplace policies: 2.4% (95% CI = 1.9, 2.9) perceived that their employer's smoking policy allowed smoking in indoor work areas, 1.5% (95% CI = 1.1, 1.9) perceived that smoking was allowed in special smoking rooms or lounges, 0.9% (95% CI = 0.7, 1.1) said that it was allowed in a break room or cafeteria, and 1.1% (95% CI = 0.8, 1.4) said that it was allowed in a hall or lobby.
FIGURE 1—
Indoor workers reporting smoke-free workplaces (1990, 1992, 1996, and 1999 California Tobacco Surveys).
As expected, a concomitant decrease in work area exposure to secondhand smoke occurred. From 1990 to 1996, the percentage of nonsmoking indoor workers who reported that someone had smoked in their work area within the previous 2 weeks declined by a factor of nearly 60%—from 29.0% (95% CI = 27.2, 30.8) in 1990 to 11.8% (95% CI = 10.3, 13.3) in 1996 (Table 2 ▶). From 1996 to 1999, the percentage reporting exposure increased to 15.6% (95% CI = 14.1, 17.1).
TABLE 2—
Exposure of Nonsmokers to Secondhand Smoke in the Past 2 Weeks in Indoor Work Areas, by Demographic Characteristics (1990, 1993, 1996, and 1999 California Tobacco Surveys)
| 1990 (n = 7293) | 1993 (n = 12 888) | 1996 (n = 5393) | 1999 (n = 4588) | |
| Overall | 29.0 (27.2, 30.8) | 22.4 (21.1, 23.7) | 11.8 (10.3, 13.3) | 15.6 (14.1, 17.1) |
| Sex | ||||
| Male | 35.6 (32.7, 38.5) | 27.6 (25.8, 29.4) | 16.4 (14.0, 18.8) | 18.0 (16.1, 19.9) |
| Female | 22.7 (20.7, 24.7) | 17.1 (15.5, 18.7) | 7.0 (5.5, 8.5) | 13.2 (10.9, 15.5) |
| Age, y | ||||
| 18–24 | 41.6 (36.9, 46.3) | 31.1 (27.4, 34.8) | 17.8 (13.3, 22.3) | 29.8 (25.0, 34.6) |
| 25–44 | 28.0 (25.7, 30.6) | 22.7 (21.1, 24.3) | 12.3 (10.4, 14.2) | 15.3 (13.2, 17.4) |
| 45–64 | 23.3 (20.7, 25.9) | 16.3 (18.4, 18.4) | 8.6 (6.0, 11.2) | 10.5 (7.4, 13.6) |
| ≥ 65 | 16.6 (7.3, 25.9) | 17.9 (12.1, 23.7) | 9.7 (3.1, 16.3) | 11.9 (5.0, 18.8) |
| Race/ethnicity | ||||
| Non-Hispanic White | 25.9 (24.1, 27.7) | 19.0 (17.6, 20.4) | 9.0 (7.3, 10.7) | 12.2 (10.7, 13.7) |
| Hispanic | 39.8 (34.9, 44.7) | 32.2 (28.4, 36.0) | 19.5 (15.7, 23.3) | 20.5 (17.4, 23.6) |
| African American | 22.9 (15.4, 30.4) | 19.5 (15.1, 23.9) | 7.9 (2.7, 13.1) | 16.0 (10.1, 21.9) |
| Asian or Pacific Islander | 27.8 (22.2, 33.4) | 26.4 (21.1, 31.7) | 11.9 (7.9, 15.9) | 19.4 (11.9, 26.9) |
| Other | 29.9 (7.4, 52.4) | 19.7 (10.5, 28.9) | 6.3 (1.0, 11.6) | 12.0 (2.1, 21.9) |
| Education | ||||
| < 12 y | 42.1 (33.5, 50.7) | 35.6 (30.4, 40.8) | 28.7 (21.5, 35.9) | 27.4 (19.8, 35.0) |
| High school graduate | 33.7 (30.2, 37.2) | 28.0 (25.7, 30.3) | 17.1 (13.7, 20.5) | 19.3 (16.3, 22.3) |
| Some college | 30.0 (26.8, 33.2) | 21.6 (19.7, 23.5) | 9.4 (7.3, 11.5) | 15.1 (12.8, 17.4) |
| College graduate | 18.5 (16.8, 20.2) | 13.6 (12.3, 14.9) | 5.1 (3.9, 6.3) | 10.2 (8.2, 12.2) |
Note. Table entries are weighted percentages and 95% confidence intervals. Weights are computed based on the probability of selection for interview and then ratio adjusted to population demographic totals so that estimates are representative of the California population.
Despite the increase in smoke-free workplaces, clean air working environments have not been established equally in all demographic groups. Table 2 ▶ shows that some of the inequities in exposure that existed in 1990 persisted through 1999. In general, males, younger workers, minorities, and the less educated still have higher rates of work area exposure to secondhand smoke. Nonetheless, females, young adults (18–24 years), African Americans, and the more highly educated showed recent increases in exposure.
In 1999, the level of reported exposure to secondhand smoke differed according to workplace type. Nonsmoking workers in hospitals and classrooms reported the least exposure (6.9% [95% CI = 3.4, 10.4] and 7.1% [95% CI = 3.9, 10.3], respectively). Offices also had a relatively low exposure rate of 11.6% (95% CI = 9.8, 13.4). Exposure was much higher for workers in plants and factories (17.9% [95% CI = 9.7, 26.1]), stores and warehouses (24.5% [95% CI = 20.0, 29.0]), and restaurants and bars (31.5% [95% CI = 22.9, 40.1]). Workers whose workplace was a vehicle had an even higher exposure rate: 50.7% (95% CI = 32.0, 69.4). Also, nonsmokers' exposure was related to worksite size. Exposure was 11.8% (95% CI = 10.1, 13.5) in workplaces with more than 50 workers, 17.5% (95% CI = 12.4, 22.6) at very small worksites with fewer than 5 employees, 17.8% (95% CI = 14.9, 20.7) in workplaces with 5 to 24 employees, and 20.6% (95% CI = 15.6, 25.6) in workplaces with 25 to 50 employees.
Clean Indoor Air in the Home
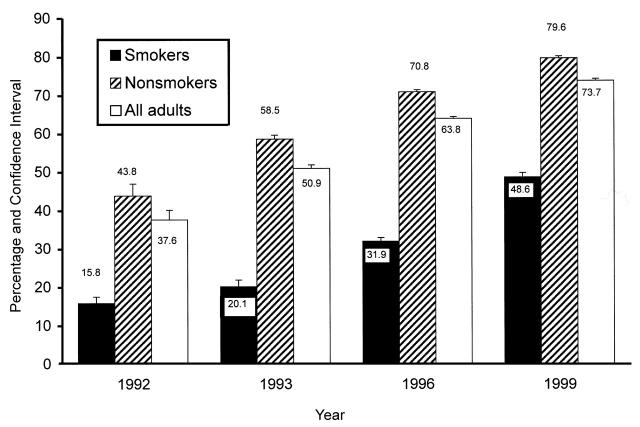
The percentage of Californians reporting smoke-free homes was 73.7% (95% CI = 73.2, 74.2) in 1999, almost a 2-fold increase since 1992 (Figure 2 ▶), when this question was first included in the California Tobacco Survey. Not surprisingly, in each year, nonsmokers were much more likely than smokers to report smoke-free homes, but the margin narrowed over time from nearly a factor of 3 in 1992 to less than a factor of 2 by 1999. In 1999, more than 3 times as many smokers reported living in smoke-free homes as in 1992.
FIGURE 2—
Californians reporting smoke-free homes (1992, 1993, 1996, and 1999 California Tobacco Surveys).
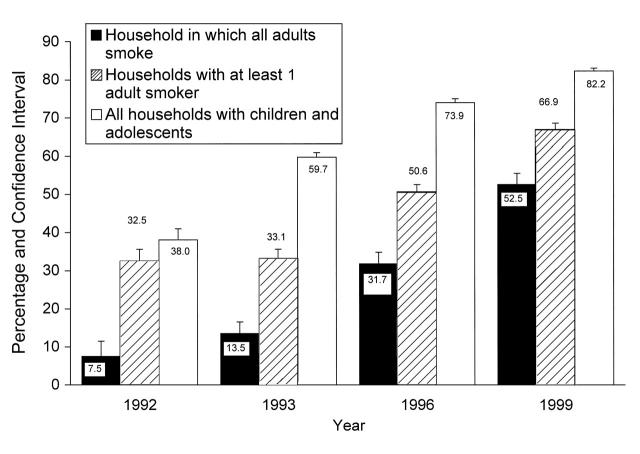
This increase in smoke-free homes has resulted in increased protection of children and adolescents from exposure to secondhand smoke at home. Figure 3 ▶ shows the increase in protection at home from 1992 to 1999 in all California households with children and adolescents (white bars), in homes with at least 1 adult smoker (striped bars), and in homes in which all adults were smokers (black bars). These categories are not mutually exclusive. In 1999, more than 80% of California's children and adolescents were protected from secondhand smoke at home, an increase from just over a third in 1992. Importantly, fewer than 10% of California's children and adolescents were protected from secondhand smoke in homes in which all adults smoked in 1992, whereas more than half were protected in 1999.
FIGURE 3—
Children and adolescents living in smoke-free homes (1992, 1993, 1996, and 1999 California Tobacco Surveys).
As with exposure to secondhand smoke in the workplace, advances in clean air at home were seen in some groups more than in others. Table 3 ▶ indicates that in 1999, Hispanic children and adolescents were more protected from secondhand smoke than were other racial/ethnic groups. However, all groups have shown impressive increases in protection since 1992 and even since 1996.
TABLE 3—
Children and Adolescents Living in Smoke-Free Homes, by Race/Ethnicity (1992, 1993, 1996, and 1999 California Tobacco Surveys)
| 1992 (na = 3756) | 1993 (n = 21 698) | 1996 (n = 25 264) | 1999 (n = 32 511) | |
| Non-Hispanic White | 37.4 (33.9, 40.9) | 58.2 (56.7, 59.7) | 70.9 (69.3, 72.5) | 80.4 (79.4, 81.4) |
| Hispanic | 39.5 (35.1, 43.9) | 62.1 (56.7, 64.7) | 78.0 (77.3, 79.5) | 85.1 (84.2, 86.0) |
| African American | 32.6 (21.9, 43.3) | 55.0 (49.4, 60.6) | 65.7 (61.8, 69.6) | 75.6 (72.4, 78.8) |
| Asian or Pacific Islander | 43.2 (29.1, 57.3) | 65.4 (60.2, 70.6) | 78.2 (75.7, 80.7) | 82.9 (80.8, 85.0) |
| Other | 33.5 (14.4, 52.6) | 53.0 (41.9, 64.1) | 70.0 (66.4, 73.6) | 78.4 (73.4, 83.4) |
Note. Table entries are weighted percentages and 95% confidence intervals. Weights are computed based on the probability of selection for interview and then ratio adjusted to population demographic totals so that estimates are representative of the California population.
aIn 1992, only children and adolescents from households in which an adult completed an extended interview could be included.
Protection in Places Other Than Work or Home
Because of gains in home and workplace protection from secondhand smoke, a new category of nonsmokers is emerging: those who rarely (if ever) are exposed to secondhand smoke. Among nonsmoking adults in 1999, 37.2% (95% CI = 35.7, 38.7) had smoke-free homes, had no workplace exposure in the past 2 weeks, and did not encounter any other situation in the past 6 months in California where they had to put up with someone smoking around them.
The other approximately two thirds of nonsmoking Californians who did report an instance of being around a smoker sometime in the past 6 months in California were most likely to report that the last time such exposure occurred indoors was in a restaurant (13.4% [95% CI = 12.0, 14.8]). Reports of exposure in restaurant bars (2.1% [95% CI = 1.6, 2.6]) and bars or taverns (8.1% [95% CI = 6.9, 9.3]) were relatively lower, reflecting that more people go to restaurants to eat than go to bars. The most frequent place identified was public parks and other outdoor areas (31.8% [95% CI = 30.1, 33.5]). Shopping malls (4.1% [95% CI = 3.4, 4.8]), community and sports events (5.4% [95% CI = 4.5, 6.3]), and game room/casino/bingo hall/pool hall venues (3.2% [95% CI = 2.6, 3.8]) were not frequently mentioned. Reports of exposure to a smoker in other people's homes (12.4% [95% CI = 10.9, 13.9]) were more frequent, but reports of exposure in others' automobiles (3.7% [95% CI = 2.9, 4.5]) were less so.
DISCUSSION
The evidence presented here shows that during the California Tobacco Control Program from 1990 to 1999, marked advances were made in guaranteeing clean indoor air for nonsmokers. In 1999, about 95% of California's indoor workers reported that their workplace was smoke-free. Nearly three quarters of Californians have smoke-free homes, including nearly half of all current smokers, and more than 80% of children and adolescents are protected from exposure at home. Furthermore, more than a third of nonsmoking Californians reported that they had not had to put up with anyone smoking in their presence, outside of work or the home, in the past 6 months.
Despite these impressive gains, further steps are needed to improve the rate of compliance with the clean indoor air law (Assembly Bill 13). The 6.6% of indoor workers who failed to report that their indoor workplace was smoke-free and the 15.6% of indoor workers reporting exposure to secondhand smoke in their work area in the past 2 weeks in 1999 indicate that compliance is not complete. This study cannot determine whether lack of compliance is due to lack of knowledge of the law or lack of enforcement. It also cannot validate self-reports of exposure at work with a biomarker; actual exposure at work may be greater than is reported because of lack of recall. The few workers who stated that their employer's policy allowed smoking in indoor work areas and common areas, such as break rooms, cafeterias, hallways, or lobbies, either have misinformed or noncompliant employers or are themselves misinformed. Although nonsmoking workers in large workplaces (> 50 employees) reported less exposure than did workers in smaller workplaces, there was little difference in exposure for different sized workplaces in the 50-or-fewer-employees group. In particular, no evidence showed that very small workplaces disregard the clean indoor air law more than do moderate-sized workplaces.
Nonsmokers in workplace settings such as stores and warehouses, plants and factories, and restaurants and bars reported particularly high rates of exposure to someone smoking in their work area in the past 2 weeks. Interestingly, nonsmokers protected at work and at home frequently named restaurants as the setting where they most recently had to put up with someone smoking around them. Some of the exposure in restaurants may have occurred in outdoor patios or eating areas. Nevertheless, increased enforcement efforts aimed at restaurant working environments are called for to protect Californians who are still most exposed to secondhand tobacco smoke. Steps to bring these work settings into greater compliance also might serve to address the racial/ethnic and other disparities in protection from secondhand smoke in the workplace. Stores and restaurants frequently employ younger, less educated workers.
The original impetus for workplace smoking restrictions was to encourage smoking cessation, and increasing evidence indicates that such restrictions do affect smoking behavior. A recent review22 of studies addressing the effect of workplace smoking restrictions indicated that 12.5% of the 76.5 billion decrease in annual cigarette consumption in the United States between 1988 and 1994 can be attributed to smoke-free workplaces. Many studies showed declines in smoking prevalence, daily smoking, or cigarette consumption.22 A report from a large national survey indicated that smoking prevalence was 6% lower among indoor workers who worked where smoking was completely banned and that consumption among daily smokers was 14% less than among indoor workers without workplace smoking restrictions.23 However, such effects may not be fully realized if workplaces with smoke-free policies do not actively or consistently enforce them24 or if the bans are not total.23
Heightened public awareness of the dangers of secondhand smoke may be partly responsible for the steadily increasing numbers of Californians reporting that their homes are smoke-free. An analysis of data from the 1996 California Tobacco Survey indicated that current smokers who believed that secondhand smoke causes cancer in nonsmokers and harms the health of children and babies or who lived in households with nonsmoking adults or with children were more likely to report smoke-free homes.25
The findings about nonsmoking adults and children also were present in national data.13 In the California study, female smokers, older smokers, and African American smokers were less likely to report having smoke-free homes.25 Hispanics were more likely to have smoke-free homes than were other racial/ethnic groups. There was little difference by educational level. Hispanic women have low smoking rates,26 and as a group, Hispanics are more likely to be occasional smokers27 who possibly do not need to smoke indoors at home. Thus, the higher rates of smoke-free homes and protection of children and adolescents in this ethnic group are not surprising.
Promoting awareness of the dangers of secondhand smoke through the mass media is a focus of the California Tobacco Control Program. Mass media campaigns appear to reach a large segment of the population, regardless of educational level.28
Both the national and the California studies13,25 found that smokers who live in smoke-free homes smoke less and show more quit attempts than do smokers who live in homes that are not smoke-free. These studies were not longitudinal, so it is not known whether smokers who are trying to quit adopt smoking bans or whether smoking bans lead to quitting behavior. However, it is logical that consumption might be reduced if a smoker can no longer smoke right after awakening or while sitting at the table after a meal; the effort to go outside would be a deterrent to smoking. For smokers trying to quit, not being able to smoke indoors at home may facilitate success by eliminating some of the stimuli to relapse.29,30 The 1996 California Tobacco Survey indicated that smokers abstained from cigarettes longer during their most recent quit attempt if they had smoke-free homes.25
The California Tobacco Control Program goals for 2000 to 2003 include a call to “continue to press for smokefree workplaces, public places, events, schools, and homes.”31 Specific recommendations urge that efforts be directed at increasing the number of clean air outdoor locations (e.g., toddler play lots, bus stops, amusement parks, fairgrounds, concerts, sporting events) and the number of clean air shared living facilities (apartments, townhouses, condominiums); they also suggest that teenagers be educated to be less accepting of secondhand smoke. The racial/ethnic differences in protection from secondhand smoke among indoor workers in the workplace and in the protection of children and adolescents in the home suggest an important opportunity for the special statewide ethnic networks to support and work within these communities to address this issue. Education of parents in culturally sensitive ways about the effects of secondhand smoke on their children and family and encouragement of the adoption of smoke-free homes and cars would be an important contribution for these groups. One recent program by the African American Tobacco Education Network—“Not in Mama's Kitchen”—is an example.31
In contrast to earlier government recommendations for tobacco control strategies,5 a recent report by the Centers for Disease Control and Prevention—Best Practices for Comprehensive Tobacco Control Programs—now mentions eliminating nonsmokers' exposure to environmental tobacco smoke as a goal.32 However, it makes few concrete recommendations, merely stating that programs should promote governmental and voluntary policies to advocate clean indoor air and calling for “strict enforcement of laws against smoking in public places.” The importance of educating the public about the dangers of secondhand smoke and of promoting smoke-free homes is given scant attention. The results from the California Tobacco Control Program suggest that this omission represents a missed opportunity for tobacco control policy development.
Acknowledgments
Preparation of this paper was supported by the Cancer Prevention Research Unit (grant CA72092) funded by the National Institutes of Health. Data for the California Tobacco Surveys were collected under contracts 89-97872 (1990 and 1992), 92-10601 (1993), 95-23211 (1996), and 98-15657 (1999) from the California Department of Health Services, Tobacco Control Section, Sacramento.
Peer Reviewed
E. A. Gilpin specified analyses and wrote the paper. A. J. Farkas reviewed drafts and quality-checked analyses. S. L. Emery reviewed and commented on early preliminary analyses and drafts. C. F. Ake conducted analyses. J. P. Pierce reviewed drafts and helped frame issues discussed in the introduction and literature review.
References
- 1.The Health Consequences of Smoking: A Report of the Surgeon General; 1972. Washington, DC: Public Health Service and Mental Health Administration, US Dept of Health, Education and Welfare; 1972. DHEW publication HSM 72-7516.
- 2.The Health Consequences of Involuntary Smoking: A Report of the Surgeon General. Atlanta, Ga: Centers for Disease Control; 1986. DHHS publication CDC 87-8398.
- 3.Major Local Tobacco Control Ordinances in the United States. Smoking and Tobacco Control Monograph No. 3. Bethesda, Md: National Cancer Institute; 1993. NIH publication 93-3532.
- 4.Bal DG, Kizer KW, Felten PG, Mozar HN, Niemeyer D. Reducing tobacco consumption in California. JAMA. 1990;264:1570–1574. [PubMed] [Google Scholar]
- 5.Strategies to Control Tobacco Use in the United States: A Blueprint for Public Health Action in the 1990's. Smoking and Tobacco Control Monograph No. 1. Bethesda, Md: National Cancer Institute; 1991. NIH publication 92-3316.
- 6.Pierce JP, Naquin M, Gilpin E, Giovino G, Mills S, Marcus S. Smoking initiation in the United States: a role for worksite and college smoking bans. J Natl Cancer Inst. 1991;83:1009–1013. [DOI] [PubMed] [Google Scholar]
- 7.Tobacco Education Oversight Committee. Toward a Tobacco-Free California: A Master Plan to Reduce Californians' Use of Tobacco. Sacramento: California Department of Health Services, Tobacco Control Section; January 1, 1991.
- 8.Respiratory Health Effects of Passive Smoking: Lung Cancer and Other Disorders. Washington, DC: Office of Research and Development and Office of Air and Radiation, US Environmental Protection Agency; 1992. Publication EPA/600/6-90-006F.
- 9.Tobacco Education Oversight Committee. Toward a Tobacco-Free California: Exploring a New Frontier 1993–1995. Sacramento: California Department of Health Services, Tobacco Control Section; February 1993.
- 10.California Environmental Protection Agency (CalEPA). Health Effects of Exposure to Environmental Tobacco Smoke: Final Report. Sacramento, Calif: Office of Environmental Health Hazard Assessment; 1997.
- 11.Health Effects of Exposure to Environmental Tobacco Smoke: The Report of the California Environmental Protection Agency. Smoking and Tobacco Control Monograph No. 10. Bethesda, Md: National Cancer Institute; 1999. NIH publication 99-4645.
- 12.Tobacco Education Research Oversight Committee. Toward a Tobacco-Free California: Renewing the Commitment 1997–2000. Sacramento: California Department of Health Services, Tobacco Control Section; 1997.
- 13.Farkas AJ, Gilpin EA, Distefan JM, Pierce JP. The effects of household and workplace smoking restrictions on quitting behaviors. Tob Control. 1999;8:261–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mannino DM, Siegel M, Husten C, Rose D, Etzel R. Environmental tobacco smoke exposure and health effects in children: results from the 1991 National Health Interview Survey. Tob Control. 1996;5:13–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Biener L, Cullen D, Di ZX, Hammond SK. Household smoking restrictions and adolescents' exposure to environmental tobacco smoke. Prev Med. 1997;26:358–363. [DOI] [PubMed] [Google Scholar]
- 16.Pierce JP, Gilpin EA, Emery SL, et al. Tobacco Control in California: Who's Winning the War? An Evaluation of the Tobacco Control Program, 1989–1996. La Jolla: University of California, San Diego; 1998. Available at: http://ssdc.ucsd.edu/tobacco.
- 17.Benson V, Marano MA. Current estimates from the National Health Interview Survey, 1993. National Center for Health Statistics. Vital Health Stat 10. 1994;No. 1004:10. [PubMed]
- 18.Current Population Survey, September 1992: Tobacco Use Supplement Technical Documentation. Washington, DC: US Bureau of the Census, Data Users Services Division, Data Access and Use Staff; 1992.
- 19.Gilpin EA, Stillman FA, Hartman AM, Gibson JT, Pierce JP. An index for state tobacco control initial outcomes. Am J Epidemiol. 2000;152:727–738. [DOI] [PubMed] [Google Scholar]
- 20.A User's Guide to WesVarPC, Version 2.0. Rockville, Md: Westat Inc; 1996.
- 21.Efron B. The Jackknife, the Bootstrap and Other Resampling Plans. CMBS Regional Conference Series in Applied Mathematics 38. Philadelphia, Pa: Society for Industrial and Applied Mathematics; 1982.
- 22.Chapman S, Borland R, Scollo M, Brownson RC, Woodward S. The impact of smoke-free workplaces on declining cigarette consumption in Australia and the United States. Am J Public Health. 1999;89:1018–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Farrelly MC, Evans WN, Sfekas AES. The impact of workplace smoking bans: results from a national survey. Tob Control. 1999;8:272–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Biener L, Nyman AL. Effect of workplace smoking policies on smoking cessation: results of a longitudinal study. J Occup Environ Med. 1999;41:1121–1127. [DOI] [PubMed] [Google Scholar]
- 25.Gilpin EA, White MM, Farkas AJ, Pierce JP. Home smoking restrictions: which smokers have them and how they are associated with smoking behavior. Nicotine Tob Res. 1999;1:153–162. [DOI] [PubMed] [Google Scholar]
- 26.Navarro AM. Cigarette smoking among adult Latinos: the California Tobacco Baseline Survey. Ann Behav Med. 1996;18:238–245. [DOI] [PubMed] [Google Scholar]
- 27.Gilpin EA, Cavin SW, Pierce JP. Adult smokers who do not smoke daily. Addiction. 1997;92:473–480. [PubMed] [Google Scholar]
- 28.Pierce JP, Macaskill P, Hill D. Long-term effectiveness of mass media led antismoking campaigns in Australia. Am J Public Health. 1990;80:565–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Best JA, Hakstian AR. A situation-specific model for smoking behavior. Addict Behav. 1978;3:79–92. [DOI] [PubMed] [Google Scholar]
- 30.Shiffman S, Gnys M, Richards TJ, Paty JA, Hickcox M, Kassel JD. Temptations to smoke after quitting: a comparison of lapsers and maintainers. Health Psychol. 1996;15:455–461. [DOI] [PubMed] [Google Scholar]
- 31.Tobacco Education Research Oversight Committee. Toward a Tobacco-Free California: Strategies for the 21st Century 2000–2003. Sacramento: California Department of Health Services, Tobacco Control Section; January 2000.
- 32.Best Practices for Comprehensive Tobacco Control Programs—August 1999. Atlanta, Ga: Office of Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion; 1999.