Abstract
Objectives. This study examined the effect of birth cohort on incidence rates of hip fracture among women and men in the Framingham Study.
Methods. Age-specific incidence rates of first hip fracture were presented according to tertile of year of birth for 5209 participants of the Framingham Study, a population-based cohort followed since 1948. Sex-specific incidence rate ratios were calculated by Cox regression to assess the relation between birth cohort and hip fracture incidence.
Results. An increasing trend in hip fracture incidence rates was observed with year of birth for women (trend, P = .05) and men (trend, P = .03). Relative to those born from 1887 to 1900 (incidence rate ratio [IRR] = 1.0), age-specific incidence rates were greatest in the most recent birth cohort, born from 1911 to 1921 (IRR = 1.4 for women, IRR = 2.0 for men), and intermediate in those born from 1901 to 1910 (IRR = 1.2 for women, IRR = 1.5 for men).
Conclusions. Results suggest risk of hip fracture is increasing for successive birth cohorts. Projections that fail to account for the increase in rates associated with birth cohort underestimate the future public health impact of hip fracture in the United States.
Hip fracture is an important public health problem, affecting a large number of elderly individuals and causing significant disability and mortality in this population. Lifetime risk of hip fracture is as high as 16% for White women in the United States.1 As many as 250 000 cases of hip fracture occur in the United States each year,2 and hip fracture is the fourth leading cause of hospitalization among persons aged 85 years and older.3 Approximately 17% of hip fracture patients die within 12 months,4,5 and about one half of hip fracture patients who were relatively independent before the fracture occurred never regain the ability to function independently.6,7
The magnitude of the impact of hip fracture on public health is likely to increase as both the number and relative proportion of elderly people in the population rise.8 Unless measures are taken to reduce the risk for hip fracture, the annual number is estimated to increase to 512 000 by 2040, when hip fracture will account for $16 billion (in 1984 dollars) in medical costs.9,10 It is important to note, however, that these projections assume stable age-specific rates of hip fracture. In contrast, if rates are rising, the burden on our society of disability, pain, mortality, and economic cost caused by hip fracture will be even greater than these predictions.11
The objective of this study was, first, to determine age-specific hip fracture rates in the Framingham Study, a population-based cohort followed for more than 50 years, and, second, to describe the relation between birth cohort and risk of hip fracture. Previous studies have not directly assessed the effect of birth cohort on hip fracture incidence in the United States. Since bone strength in old age is a function of bone mass accretion during the first 2 decades of life as well as bone loss in middle and old age, analysis of hip fracture risk according to birth cohort can help elucidate etiologic clues shared early in life.12,13 While birth cohort and calendar time period are highly interrelated, trends can be missed when reported by calendar time but can become apparent if examined by birth cohort, depending on the calendar time and ages of the population under study.12,14,15 Moreover, characterizing hip fracture rates by birth cohort can help to more accurately predict the future fracture burden on public health.13
METHODS
Participants
The Framingham Study is a population-based cohort established in 1948 in Framingham, Mass. Methods of recruitment and data collection have been described elsewhere.16 Briefly, participants received standardized physical examinations and completed structured questionnaires administered by trained interviewers every 2 years at study visits. Cohort members have been followed closely for all major health events, and follow-up is complete for 99%. Participants included 2875 women and 2334 men with a mean age of 44 years (range = 28–62 years) at baseline.
Hip Fracture Ascertainment
Hip fractures were ascertained by using several overlapping sources. A comprehensive review was conducted of fracture logs and of hospitalization and death records obtained for participants of the Framingham Heart Study since the cohort was established in 1948. Hip fractures were also assessed by interview at each biennial study examination since 1983 (examination 18). For those participants not attending an examination (owing to illness, residence in a nursing home, or being out of state), hip fracture was assessed by telephone interview. Reported hip fractures were confirmed by a review of medical records and radiographic and operative reports obtained from hospitals, nursing homes, and home health care services.
Hip fracture was defined as a first-time fracture of the proximal femur caused by minimal trauma—that is, due to a fall from standing height or less.
Analysis
Age-specific incidence rates were calculated as the number of cases divided by the number of person-years at risk for 5-year age groups. The number of person-years was defined as the years contributed by each participant to each 5-year age group from baseline enrollment to the first of the following events: hip fracture, death, last contact, or closing date for this study (December 31, 1995).
Incidence rate ratios, 95% confidence intervals, and tests for trend were calculated by Cox regression, with age as the time scale.17 Birth cohort was categorized by tertile according to the sex-specific distribution of year of birth for the total number of women and men in the study. Tertiles were chosen to maximize the statistical stability of estimates given the size of the study group. Analyses were conducted for women and men separately.
RESULTS
A total of 309 hip fractures occurred among women and 77 hip fractures occurred among men (Table 1 ▶). Ninety-four percent of cases (n = 362) were confirmed by a review of hospital records, including discharge summaries, operative reports, and radiographic reports. Hospital records were not available for confirmation in 24 cases (6%); however, detailed information on these cases was consistently recorded by physician examiners as part of the standardized medical history of hospitalizations obtained at study examinations. Mean age at fracture was 79 years and 77 years for women and men, respectively. Average duration of study follow-up time was 39 person-years for women and 33 person-years for men.
TABLE 1—
Age-Specific Incidence Rates of Hip Fracture: The Framingham Study, 1948–1996
| Women | Men | |||||
| Age, y | Cases (n = 309) | Person-Years | Incidence Rate (per 103 Person-Years) | Cases (n = 77) | Person-Years | Incidence Rate (per 103 Person-Years) |
| <60 | 11 | 41 515 | 0.26 | 9 | 32 974 | 0.27 |
| 60–64 | 14 | 12 852 | 1.09 | 1 | 9579 | 0.10 |
| 65–69 | 22 | 11 931 | 1.84 | 6 | 8488 | 0.71 |
| 70–74 | 38 | 10 651 | 3.57 | 9 | 7063 | 1.27 |
| 75–79 | 61 | 7874 | 7.75 | 15 | 4678 | 3.20 |
| 80–84 | 68 | 4534 | 15.00 | 15 | 2278 | 6.58 |
| 85–89 | 59 | 2079 | 28.38 | 15 | 809 | 18.84 |
| 90–94 | 28 | 644 | 43.48 | 6 | 196 | 30.61 |
| ≥95 | 8 | 114 | 70.18 | 1 | 22 | 45.45 |
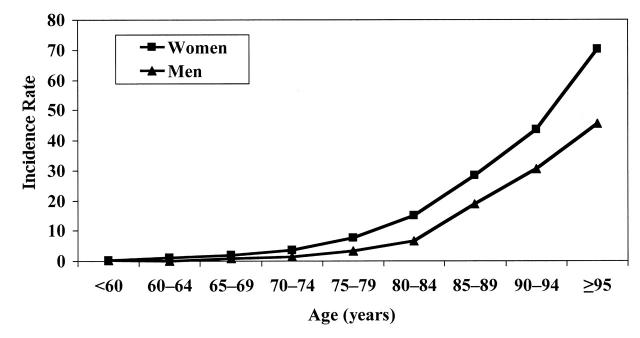
As expected, rates increased exponentially with age for both sexes (Figure 1 ▶). The incidence rate increased from 7.75 per 1000 person-years among women aged 75 to 79 years to 70.18 per 1000 person-years among women aged 95 years and older. For men, the incidence rate increased from 3.2 per 1000 person-years for ages 75 to 79 years to 45.45 per 1000 person-years for ages 95 years and older. Also as expected, risk of fracture was greater among women than among men; for each age group, incidence rates were 1.5 to 2.5 times greater among women than men.
FIGURE 1—
Age-specific incidence rates of hip fracture (per 1000 person-years): The Framingham Study.
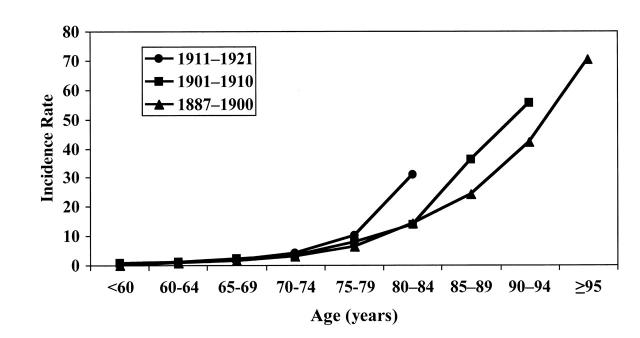
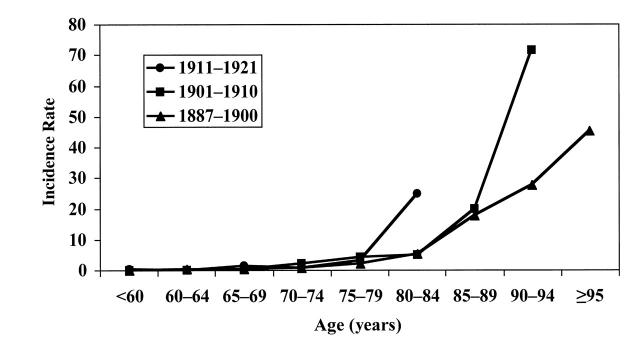
Table 2 ▶ gives the distribution of hip fractures among women and men according to tertile of birth cohort, while age-specific rates are shown in Figures 2 and 3 ▶ ▶. For each birth cohort, the exponential relationship between age and hip fracture risk was evident among women and men. Moreover, rates increased with tertile of birth cohort for both women and men, with the highest rates found among those born between 1911 and 1921, intermediate rates among those born between 1901 and 1910, and lowest rates among those born by 1900.
TABLE 2—
Incidence Rate Ratio (IRR) of Hip Fracture by Tertile of Birth Cohort: The Framingham Study
| Women | Men | |||||
| Birth Cohort | Cases | IRR | 95% CI | Cases | IRR | 95% CI |
| 1887–1900 | 135 | 1.0 | (Reference) | 29 | 1.0 | (Reference) |
| 1901–1910 | 114 | 1.2 | 1.0, 1.5 | 28 | 1.5 | 0.8, 2.5 |
| 1911–1921 | 60 | 1.4 | 1.0, 1.9 | 20 | 2.0 | 1.1, 3.9 |
| Test for trend | P = .05 | P = .03 | ||||
Note. CI = confidence interval.
FIGURE 2—
Age-specific incidence rates of hip fracture (per 1000 person-years) for women, by birth cohort.
FIGURE 3—
Age-specific incidence rates of hip fracture (per 1000 person-years) for men, by birth cohort.
Results from regression analysis are presented in Table 2 ▶. Compared with women born by 1900, incidence was 1.2 times and 1.4 times greater among women born from 1901 to 1910 and from 1911 to 1921, respectively. While 95% confidence intervals for stratum-specific incidence rate ratios included 1.0, the test for trend bordered on statistical significance (P = .05). The positive association between birth cohort and age-specific incidence rates was also seen for men (trend, P = .03). Compared with the earliest birth cohort (1887–1900), risk of fracture was 50% greater for men born from 1901 to 1910 and twice as great for men born in the latest birth cohort (1911–1921).
While the magnitude of the effect of birth cohort appeared greater among men than among women, the test for interaction between birth cohort and sex on risk of fracture was not significant (P = .74).
Analyses were repeated that included only those participants who survived to age 84 years, so that the duration of follow-up time was similar for the 3 birth cohorts. Results did not differ from the findings for the total study group.
DISCUSSION
Results from this study suggest the presence of a birth cohort effect on age-specific incidence rates of hip fracture. Risk of hip fracture increased with year of birth for both women and men. These results are consistent with studies conducted in England18 and Finland19 that reported increasing risk of hip fracture in successive birth cohorts of women and men.
Birth cohort analyses of hip fracture rates in the United States have not been previously reported. Findings from this study, however, are consistent with secular trends observed in Rochester, Minn, where age-specific incidence rates increased from 1928 to 1982 for women aged 75 years and older and for men aged 65 years and older.20 Rodriguez et al.21 also found increasing age-specific hospitalization rates for hip fracture in the United States among both women and men from 1970 to 1983. Increases in age-specific rates among women and men have been observed, in general, from the 1970s to the 1980s and 1990s in England and Wales,22 East Germany,23 Finland,19 Sweden,24 and Norway.25
Some have suggested that hip fracture rates among women and men have been stabilizing or leveling off in recent years in the United States and Europe,20,22,24 and predictions have been made assuming stable age-specific hip fracture rates in the United States.9 The current findings do not support the suggestion that US rates are reaching a plateau. Moreover, projections failing to account for potential birth cohort effects will seriously underestimate the future public health impact of fracture in the United States.11
This study has several potential limitations. The positive relationship between birth cohort and hip fracture rates observed in this study may be due to changes in case ascertainment over the follow-up period. This is unlikely since all hospitalizations, death records, and fracture logs have been comprehensively reviewed for Framingham participants since enrollment. In addition, results were unchanged when analyses were repeated that restricted participants to those who survived to examination 18 (1983), when individuals were directly queried regarding fracture history. Further, rates reported by this and other studies of hip fracture ascertained through examination 18 in Framingham26–29 closely approximate national rates,21,30 suggesting that ascertainment was complete.
Since the closing date for the present study was the end of 1995, the average follow-up time was longer for the oldest birth cohort than for the middle and youngest birth cohorts. Thus, data are not available to calculate incidence rates for the middle birth cohort at age 95 years and older or for the youngest birth cohort at age 85 years and older. To address this limitation, analyses were repeated that included only those individuals who survived to age 84 years so that the years of follow-up time were similar for the 3 birth cohorts. The difference in hip fracture risk among the 3 birth cohorts persisted, and relative risks remained unchanged from the analyses for the total study group.
An alternative explanation for the present findings is that the increased age-specific rates of hip fracture found with year of birth are due to corresponding changes in competing causes of mortality over time. As life expectancy improves with time, the proportion of frail individuals surviving to the oldest ages also increases. As a result, the proportion of frail elderly at increased risk of hip fracture may be greatest in the youngest birth cohort and account for the positive relationship between birth cohort and fracture incidence found in this study.
The increased trend in rates with birth cohort can also be interpreted as evidence for temporal changes in the prevalence of factors involved in achieving and maintaining peak bone mass early in life. The increase in young adult height observed in Western populations for successive birth cohorts has also been suggested to contribute to increasing hip fracture incidence,31–33 since increased height has been shown to be an independent risk factor for hip fracture, possibly through increasing the distance, and therefore the impact, of falls.34–37 In a longitudinal study, Cooper and colleagues38 demonstrated the importance of anthropometric characteristics in early childhood for predicting peak bone mass in women. Evidence for environmental influences operating early in life on risk of hip fracture in old age is also provided by the work of Lauderdale et al.,39 who demonstrated that geographic residence at birth (Northeast, South Atlantic, East South Central, etc.) was strongly associated with hip fracture risk for both women and men, while adult residence was unrelated to fracture incidence.
Results from the present study cannot identify whether or not changes over time in environmental risk factors (in young or old age) are responsible for the increased trend in hip fracture rates with birth cohort. While birth cohort analyses can help to elucidate etiologic clues, the major contribution of this study is the implications of the findings with respect to the accurate prediction of future trends and the public health burden of hip fracture.
This study offers several advantages over previous descriptive studies of hip fracture in the United States. This is the first study to provide incidence rates for a well-defined, population-based cohort, especially one that includes significant numbers of individuals aged older than 80 years. Previous studies have relied upon national2,21,30 or local20 hospital discharge data, which pose several methodological limitations. First, accurately defining denominators for the calculation of rates based on hospital discharge data is difficult owing to lack of information, at the individual level, on persons at risk. Second, in addition to difficulty in tracking changes in the population at risk, methods to classify hip fracture also change over time, posing limitations in the interpretation of rates reported from hospital discharge data. Third, investigators using hospital discharge data cannot always successfully exclude hip fracture cases caused by trauma or avoid duplication of cases due to readmissions or transfers between hospitals. Finally, persons at the end of life may not be hospitalized when they sustain a hip fracture. Consequently, previous studies that ascertained hip fracture cases from hospital discharge data would have underestimated hip fracture rates in the very old and sick, precisely the group of individuals for whom accurate information is critical for determining the public health impact of hip fracture in the United States.
In summary, this study found evidence that hip fracture rates are increasing for women and men with year of birth. Moreover, projections that fail to account for potential birth cohort effects may underestimate the future public health impact of hip fracture in the United States.
Acknowledgments
This work was supported in part by National Institute of Health/National Heart, Lung, and Blood Institute grants T32 AR07598, NIH AR20613, and R01-AR/AG 41398 and NIH/NHLBI contract grant N01-HC-38038.
We wish to thank Kerry Broe for statistical programming for this study.
E. J. Samelson planned the study, analyzed the data, and wrote the paper. Y. Zhang provided statistical support for the study design and data analysis. D. P. Kiel contributed to the formulation of study hypotheses and the interpretation of results. D. P. Kiel, M. T. Hannan, and D. T. Felson supervised data collection and contributed to the writing of the paper.
Peer Reviewed
References
- 1.Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles', or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149:2445–2448. [PubMed] [Google Scholar]
- 2.Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Hip fracture incidence among the old and very old: a population-based study of 745 435 cases. Am J Public Health. 1990;80:871–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.May DS, Kelly JJ, Mendlein JM, Garbe PL. Surveillance of major causes of hospitalization among the elderly, 1988. Morb Mortal Wkly Rep CDC Surveill Summ. 1991;40:7–21. [PubMed] [Google Scholar]
- 4.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Survival experience of aged hip fracture patients. Am J Public Health. 1989;79:274–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper C, Atkinson EJ, Jacobsen SJ, O'Fallon WM, Melton LJ 3rd. Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993;137:1001–1005. [DOI] [PubMed] [Google Scholar]
- 6.Kelsey JL, Hoffman S. Risk factors for hip fracture. N Engl J Med. 1987;316:404–406. [DOI] [PubMed] [Google Scholar]
- 7.Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med. 1997;103(suppl):12S–17S. [DOI] [PubMed] [Google Scholar]
- 8.Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–289. [DOI] [PubMed] [Google Scholar]
- 9.Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop. March 1990:163–166. [PubMed]
- 10.Chrischilles E, Shireman T, Wallace R. Costs and health effects of osteoporotic fractures. Bone. 1994;15:377–386. [DOI] [PubMed] [Google Scholar]
- 11.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407–413. [DOI] [PubMed] [Google Scholar]
- 12.Martyn CN, Cooper C. Prediction of burden of hip fracture. Lancet. 1999;353:769–770. [DOI] [PubMed] [Google Scholar]
- 13.MacMahon B, Pugh TF. Epidemiology: Principles and Methods. Boston, Mass: Little, Brown and Co; 1970.
- 14.Vaupel JW, Yashin AI. Heterogeneity's ruses: some surprising effects of selection on population dynamics. Am Statistician. 1985;39:176–185. [PubMed] [Google Scholar]
- 15.Osmond C, Gardner MJ, Acheson ED. Analysis of trends in cancer mortality in England and Wales during 1951–80, separating changes associated with period of birth and period of death. Br Med J (Clin Res Ed). 1982;284:1005–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dawber TR, Meadors GF, Moore FE. Epidemiological approaches to heart disease: The Framingham Study. Am J Public Health. 1951;41:279–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korn EL, Graubard BI, Midthune D. Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol. 1997;145:72–80. [DOI] [PubMed] [Google Scholar]
- 18.Evans JG, Seagroatt V, Goldacre MJ. Secular trends in proximal femoral fracture, Oxford record linkage study area and England 1968–86. J Epidemiol Community Health. 1997;51:424–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kannus P, Niemi S, Parkkari J, Palvanen M, Vuori I, Jarvinen M. Hip fractures in Finland between 1970 and 1997 and predictions for the future. Lancet. 1999;353:802–805. [DOI] [PubMed] [Google Scholar]
- 20.Melton LJ, O'Fallon WM, Riggs BL. Secular trends in the incidence of hip fractures. Calcif Tissue Int. 1987;41:57–64. [DOI] [PubMed] [Google Scholar]
- 21.Rodriguez JG, Sattin RW, Waxweiler RJ. Incidence of hip fractures, United States, 1970–83. Am J Prev Med. 1989;5:175–181. [PubMed] [Google Scholar]
- 22.Spector TD, Cooper C, Lewis AF. Trends in admissions for hip fracture in England and Wales, 1968–85. Br Med J. 1990;300:1173–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wildner M, Casper W, Bergmann KE. A secular trend in hip fracture incidence in East Germany. Osteoporos Int. 1999;9:144–150. [DOI] [PubMed] [Google Scholar]
- 24.Rogmark C, Sernbo I, Johnell O, Nilsson JA. Incidence of hip fractures in Malmo, Sweden, 1992–1995: a trend-break. Acta Orthop Scand. 1999;70:19–22. [DOI] [PubMed] [Google Scholar]
- 25.Falch JA, Kaastad TS, Bohler G, Espeland J, Sundsvold OJ. Secular increase and geographical differences in hip fracture incidence in Norway. Bone. 1993;14:643–645. [DOI] [PubMed] [Google Scholar]
- 26.Kiel DP, Felson DT, Anderson JJ, Wilson PW, Moskowitz MA. Hip fracture and the use of estrogens in postmenopausal women: The Framingham Study. N Engl J Med. 1987;317:1169–1174. [DOI] [PubMed] [Google Scholar]
- 27.Felson DT, Sloutskis D, Anderson JJ, Anthony JM, Kiel DP. Thiazide diuretics and the risk of hip fracture: results from The Framingham Study. JAMA. 1991;265:370–373. [PubMed] [Google Scholar]
- 28.Felson DT, Kiel DP, Anderson JJ, Kannel WB. Alcohol consumption and hip fractures: The Framingham Study. Am J Epidemiol. 1988;128:1102–1110. [DOI] [PubMed] [Google Scholar]
- 29.Felson DT, Anderson JJ, Hannan MT, Milton R, Wilson PWF, Kiel DP. Impaired vision and hip fracture: The Framingham Study. J Am Geriatr Soc. 1989;37:495–500. [DOI] [PubMed] [Google Scholar]
- 30.Farmer ME, White LR, Brody JA, Bailey KR. Race and sex differences in hip fracture incidence. Am J Public Health. 1984;74:1374–1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reid IR, Chin K, Evans MC, Jones JG. Relation between increase in length of hip axis in older women between 1950s and 1990s and increase in age specific rates of hip fracture. BMJ. 1994;309:508–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reid IR. Has improved nutrition contributed to the hip fracture epidemic? Mol Cell Endocrinol. 1996;123:123–125. [DOI] [PubMed] [Google Scholar]
- 33.Reid IR, Chin K, Evans MC, Cundy T. Longer femoral necks in the young: a predictor of further increases in hip fracture incidence? N Z Med J. 1996;109:234–235. [PubMed] [Google Scholar]
- 34.Meyer HE, Tverdal A, Falch JA. Risk factors for hip fracture in middle-aged Norwegian women and men. Am J Epidemiol. 1993;137:1203–1211. [DOI] [PubMed] [Google Scholar]
- 35.Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women. N Engl J Med. 1995;332:767–773. [DOI] [PubMed] [Google Scholar]
- 36.Meyer HE, Falch JA, O'Neill T, Tverdal A, Varlow J. Height and body mass index in Oslo, Norway, compared to other regions of Europe: do they explain differences in the incidence of hip fracture? European Vertebral Osteoporosis Study Group. Bone. 1995;17:347–350. [DOI] [PubMed] [Google Scholar]
- 37.Hemenway D, Azrael DR, Rimm EB, Feskanich D, Willett WC. Risk factors for hip fracture in US men aged 40 through 75 years. Am J Public Health. 1994;84:1843–1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cooper C, Cawley M, Bhalla A, et al. Childhood growth, physical activity, and peak bone mass in women. J Bone Miner Res. 1995;10:940–947. [DOI] [PubMed] [Google Scholar]
- 39.Lauderdale DS, Thisted RA, Goldberg J. Is geographic variation in hip fracture rates related to current or former region of residence? Epidemiology. 1998;9:574–577. [PubMed] [Google Scholar]