Abstract
Objectives. This study examined the impact of drug coverage generosity on older persons’ prescription events (fills) and expenditures.
Methods. A cross-sectional study was conducted of 6237 older persons from the 1995 Medicare Current Beneficiary Survey. Dependent variables were per capita prescription events and expenditures. Independent variables were insurance type and drug coverage generosity. Control variables included sociodemographic and health status factors.
Results. Regardless of insurance type, per capita prescription events increased as drug coverage generosity improved and then decreased at the most generous level. Per capita prescription expenditures increased as generosity improved; with generous prescription coverage, prescription expenditures were approximately 3 times those with Medicare only.
Conclusions. Even when factors that affect drug use and insurance selection are controlled, prescription coverage generosity influences prescription use. (Am J Public Health. 2002;92:1257–1263)
Medicare beneficiaries (older persons and the disabled) account for 14% of the US population but consume 36.5% of the $831.7 billion spent for health care. Prescription drug use is an essential part of maintaining and improving the well-being of older persons. Older persons, on average, receive 20 prescriptions per year. The range for older persons without drug coverage is 12 to 20 prescriptions per year; for older persons with coverage, the range is 20 to 25.1 The number and type of chronic diseases present in this population that require prescription medication explains, in part, this high use.2,3
Although approximately 91% of community-dwelling older persons either had some form of supplemental health insurance or were enrolled in a Medicare health maintenance organization (HMO) in 1995,4,5 only 53% had stable prescription drug coverage, and this percentage has not increased.6,7 Currently, Congress and the president support the idea of prescription drug coverage for US older persons but differ on its design and payment.8
Previous studies have consistently noted that possession of prescription drug coverage increases prescription expenditure and use.1,7,9–12 The level of coverage generosity, however, varied widely among and within the sources of prescription drug coverage in these studies.1,7,9–12 Moreover, none of these studies examined the association between different levels of generosity of coverage and prescription expenditures and events (fills), nor did they control for health status factors.
Responding to the ongoing debate regarding a Medicare prescription drug benefit, this study examined the relationship between the generosity of outpatient prescription drug coverage for older persons and their outpatient prescription service events and expenditures, controlling for sociodemographic and health status conditions. At the time of this investigation, Medicare Current Beneficiary Survey (MCBS) data from 1991 through 1995 were available as public use files. We examined the 1992 through 1995 MCBS data sets cross-sectionally for our investigation. Results from 1992 through 1994, which are available from the authors, are generally consistent with the 1995 findings reported here.
METHODS
Data Source
The MCBS is a continuous, multipurpose survey sponsored by the Health Care Financing Administration (HCFA) that provides information on health care use and expenditures. In-depth information about the MCBS, its sampling methodology, and its imputation algorithms have been extensively described elsewhere.13–16 The MCBS represents the entire Medicare population (i.e., disabled individuals aged younger than 65 years), as well as community- and institution-dwelling older persons aged 65 and older. Its sampling methodology oversamples older persons aged 85 and older and the nonelderly disabled. Interviews are conducted in the home, and administrative and billing information is linked to survey data by HCFA. Older persons are followed and reinterviewed throughout their transitions between community and institution dwelling. Summary data on inpatient hospital, outpatient hospital, and medical provider services and expenditures are collected from both the household survey and claims data. The survey data are then matched with the claims data to adjust for possible underreporting by MCBS participants, to fill in missing information, and to make corrections in the survey information.17
Prescription use and expenditure information are collected and summarized from thrice-a-year household interviews. The prescription expenditure and event data used in this study are collected and summarized from survey data, with missing data statistically imputed.13
Sample
Study participants were required to have been 65 years or older as of July 1, 1995, to have been participants in the MCBS survey for all of 1995, to have been enrolled in Medicare Part A and B for all of 1995, and to have had at least 1 prescription event during 1995. Older persons were excluded if they died any time during the year, had end-stage renal disease, received any Medicaid benefits, or had partial-year supplemental insurance coverage. These criteria allowed us to focus on the population of interest. After the inclusion and exclusion criteria were applied, 6237 older persons were in the study sample. This study was approved by the University of Minnesota Institutional Review Board, Human Subjects Committee.
Independent Variables
All statistical models contained 2 independent variables, insurance coverage and generosity of outpatient prescription drug coverage. The first variable, insurance coverage, distinguished the type of supplemental insurance coverage a person possessed after Medicare, if any. Insurance coverage was categorized into 6 mutually exclusive types: (1) Medicare HMO; (2) private supplemental, employer purchase (Private-E); (3) private supplemental, independent purchase (Private-I); (4) private supplemental, employer and independent purchase; (5) private supplemental, employer/independent/HMO; and (6) Medicare only, the reference group. All types were included in the overall model fitting, but 2 types (private supplemental, employer and independent purchase; private supplemental, employer/independent/HMO) were too small to generate stable results and are not reported here.
The second variable, generosity of outpatient prescription drug coverage, represented the perceived cost sharing by the older person and was operationally defined as a ratio. Specifically, out-of-pocket expenditures were divided by the total net expenditures for prescriptions (defined as total expenditures for prescriptions paid by subject and insurers minus the prescription expenditure covered by Medicare, because some individuals had prescriptions that were covered by Medicare). For these analyses, the generosity ratio was operationally categorized into 4 levels: (1) none (ratio > 0.99); (2) poor (ratio > 0.80 ≤ 0.99); (3) fair (ratio > 0.20 ≤ 0.80); and (4) good (ratio > 0 ≤ 0.20). These 4 levels were chosen on the basis of a review of the frequency distributions of the ratios, which separated the generosity ratio data roughly into quartiles.
Outcome Variables
Model dependent variables were specific yearly per capita prescription events (fills) and prescription expenditures (expenditures represent cost to the individual as well as the insurer). These variables came directly from the MCBS database.
To better understand the impact of generosity and insurance type on event count, we set up the model equations to compare the event counts of each combination of insurance type and generosity level (e.g., Medicare HMO with fair generosity, Private-I with good generosity) with the event counts of a standardized reference group. The reference group chosen for this study was the Medicare-only insurance type with a generosity of none. These comparisons, called event ratios, also included 95% confidence intervals. With the event count of the reference group standardized to 1.0, the event ratio represents how many more (or fewer) events per person the insurance type and generosity combination group had compared with the Medicare-only group. For example, if an insurance–generosity combination had an event ratio of 1.2, subjects in this group had 20% more prescription events per person compared with subjects in the Medicare-only group who paid for all drugs out-of-pocket.
Similarly, we set up the model equations to compare the expenditures of each combination of insurance type and generosity level with those of the Medicare-only group. These comparisons, called expenditure ratios, also included 95% confidence intervals. The expenditure total of the reference group (Medicare only) was standardized to 1.0.
Control Variables
In all analyses, sociodemographic and health status variables that have been previously shown to influence prescription use or insurance selection were chosen a priori to control for possible confounding effects on older persons’ prescription use and expenditures.2,6,15–25 These control variables included age, race/ethnicity, sex, income, marital status, number of personal activities of daily living (ADL) limitations,26 number of instrumental activities of daily living (IADL) limitations,26 self-perceived health status, number of chronic diseases, census region, and metropolitan residence status.2,6,15–25
Statistical Analyses
Descriptive statistics of the sample populations were calculated for the entire 1995 sample and for the sample categorized by insurance type. Event and expenditure models were built for 1995. In the model analyses that used number of events as the dependent variable, we constructed a log linear model using a Poisson distribution.27 In the model analyses that used prescription expenditure as the dependent variable, expenditure was first transformed to a natural logarithmic scale. This transformation, which served to eliminate a marked skew in the expense data distribution, is a routine procedure for expenditure data.27 After transformation, the residuals from the analyses of variance were roughly normal. An ordinary linear model was then constructed. F test statistics for expenditure models and χ2 test statistics for event models were performed on the independent variable combination, which includes what can be considered the insurance and generosity main effects and their interaction.27,28 SAS PROC GENMOD software was used for all modeling.29
RESULTS
In Table 1 ▶, self-perceived health status, marital status, metropolitan residence status, and income of the sample population were similar to the ratings reported for the total elderly population in 1995.4,30 The sample populations contained greater proportions of White individuals and older individuals with poorer health compared with the total elderly population. The insurance coverage distributions of the sample population were similar to those of US community-dwelling older persons, except that the sample population had a higher percentage of older persons possessing Private-I insurance. Table 1 ▶ also shows the percentage of persons with the 4 insurance types by generosity level. For approximately 80% of older persons in the individually purchased supplemental insurance group (Private-I), prescription generosity was either none or poor. This contrasts with the employer-purchased insurance group (Private-E), in which 70% of the older persons had fair or good prescription generosity. Additionally, approximately 74% of older persons in the Medicare HMO group had fair or good prescription generosity.
TABLE 1.
—Descriptive Statistics (%) of 1995 Sample Population, by Insurance Typea: Medicare Current Beneficiary Survey
| 1995 Sample (n = 6237) | Independent Purchase (Private-I)b(n = 2278) | Employer Purchase (Private-E)c(n = 1913) | Medicare HMOd(n = 791) | Medicare Onlye(n = 517) | |
| Sex | |||||
| Male | 40.7 | 35.5 | 44.1 | 45.2 | 42.5 |
| Female | 59.3 | 64.5 | 55.9 | 54.8 | 57.5 |
| Age | |||||
| 65–74 | 48.9 | 38.6 | 47.1 | 45.6 | 45.3 |
| 75–84 | 37.1 | 42.2 | 38.9 | 38.7 | 35.6 |
| ≥ 85 | 14.0 | 19.2 | 14.0 | 15.7 | 19.1 |
| Race/ethnicity | |||||
| White | 91.2 | 95.1 | 92.3 | 86.0 | 75.1 |
| African American | 6.3 | 3.1 | 5.5 | 9.6 | 20.1 |
| Other | 2.5 | 1.8 | 2.2 | 4.4 | 4.8 |
| Metropolitan status | |||||
| Metro | 73.1 | 62.3 | 76.7 | 90.1 | 66.5 |
| Nonmetro | 26.9 | 37.7 | 23.3 | 9.9 | 33.5 |
| Marital status | |||||
| Married | 54.7 | 49.2 | 61.1 | 57.4 | 46.6 |
| Widowed | 37.4 | 43.8 | 31.5 | 34.4 | 42.4 |
| Divorced/separated | 4.8 | 4.2 | 4.7 | 5.6 | 7.3 |
| Never married | 3.1 | 2.8 | 2.7 | 2.6 | 3.7 |
| Income, $ | |||||
| ≥5000 | 3.5 | 4.1 | 2.4 | 3.7 | 7.8 |
| 5001–10 000 | 17.8 | 22.8 | 9.5 | 18.7 | 37.7 |
| 10 001–15 000 | 20.6 | 22.7 | 17.7 | 21.2 | 25.7 |
| 15 001–20 000 | 15.9 | 15.3 | 17.7 | 15.2 | 10.8 |
| 20 001–25 000 | 13.2 | 11.3 | 16.9 | 15.0 | 5.2 |
| >25 000 | 29.0 | 23.8 | 35.9 | 26.2 | 12.8 |
| No. of chronic diseases | |||||
| 0 | 5.9 | 6.0 | 6.1 | 7.0 | 5.0 |
| 1 | 14.0 | 14.0 | 13.5 | 15.0 | 14.1 |
| ≥2 | 80.1 | 80.0 | 80.4 | 78.0 | 80.9 |
| Self-perceived health status | |||||
| Excellent | 16.3 | 15.5 | 16.5 | 19.9 | 12.8 |
| Very good | 29.1 | 29.5 | 29.4 | 28.7 | 22.0 |
| Good | 31.5 | 31.0 | 32.2 | 32.6 | 29.8 |
| Fair | 17.3 | 18.5 | 16.6 | 12.9 | 23.8 |
| Poor | 5.8 | 5.5 | 5.3 | 5.9 | 11.6 |
| No. of ADLsf | |||||
| 0 | 70.1 | 67.9 | 72.5 | 72.3 | 60.7 |
| ≥2 | 17.0 | 19.4 | 15.5 | 14.0 | 24.4 |
| No. of IADLsg | |||||
| 0 | 74.2 | 72.2 | 75.6 | 75.6 | 65.0 |
| 1 | 14.3 | 14.8 | 14.9 | 13.7 | 15.7 |
| ≥2 | 11.5 | 13.0 | 9.5 | 10.7 | 19.3 |
| Insurance generosity levelh | |||||
| None | 57.6 | 19.1 | 14.5 | 61.1 | |
| Poor | 23.5 | 10.5 | 10.6 | 21.1 | |
| Fair | 15.2 | 42.2 | 53.0 | 13.9 | |
| Good | 3.7 | 28.2 | 21.9 | 3.9 |
aSample n’s by insurance do not add up to 6237; 2 insurance types, although used in model analyses, are not reported here owing to small numbers.
bPrivate-I = persons possessing Part A and Part B Medicare coverage as well as supplemental insurance purchased independently by them.
cPrivate-E = persons possessing Part A and Part B Medicare coverage as well as supplemental insurance through their employer or an employer-based retirement package.
dMedicare HMO = persons enrolled in a Medicare health maintenance organization (HMO) with no supplemental insurance.
eMedicare only = persons possessing Part A and Part B Medicare coverage with no supplemental insurance.
fADLs = activities of daily living (difficulty bathing/showering, walking, dressing, getting in/out of a bed or chair, using a toilet, eating).
gIADLs = instrumental activities of daily living (difficulty in preparing meals, managing money, shopping for groceries or personal items, performing light housework, writing, using a telephone).
hEach level represents an individual’s cost-sharing ratio of prescription medicine for 1995; that is, out-of-pocket expenditure was divided by the total net expenditure for prescriptions (total expenditures for prescriptions paid by subject and insurers). None (ratio > 0.99) indicates that individuals paid more than 99% of their total prescription expenditure; poor (ratio > 0.80 ≤ 0.99) indicates that individuals paid more than 80% and up to 99% of their total prescription expenditure; fair (ratio > 0.20 and ≤ 0.80) indicates that individuals paid more than 20% and up to 80% of their total prescription expenditure; good (ratio > 0 ≤ 0.20) indicates that individuals paid less than 20% of their total prescription expenditure.
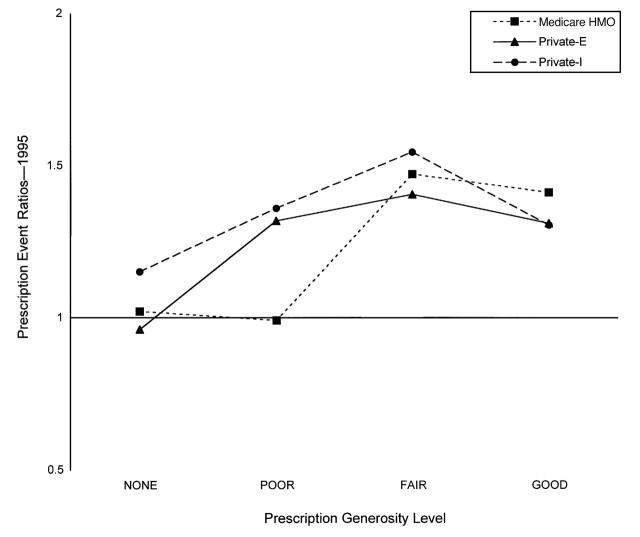
Figure 1 ▶ presents graphically the outpatient prescription event ratios reported in Table 2 ▶. As prescription coverage generosity increases from none to poor to fair, per capita event ratios increase consistently for all insurance groups. Furthermore, the event ratios appear to peak at the fair generosity level and then to decline as generosity becomes good. Per capita event ratios show heaviest use by Private-I type, followed by Private-E, Medicare HMO, and Medicare only. The main effect for the insurance-type variable is significant (χ25 = 13.29; P = .0209). Statistically significant differences were observed among the various insurance–generosity combinations presented in Figure 1 ▶and Table 2 ▶ (χ223 = 193.52; P < .0001).
FIGURE 1.
—1995 prescription event (fill) ratio of each insurance type by prescription generosity level.
TABLE 2.
—Prescription Event Ratios (With 95% Confidence Intervals) of 1995 Sample Populationa: Medicare Current Beneficiary Survey
| Generosity Levelc | ||||
| Insurance Typeb | None | Poor | Fair | Good |
| Private-I | 1.15 (1.03, 1.27) | 1.36 (1.21, 1.51) | 1.54 (1.37, 1.72) | 1.30 (1.09, 1.56) |
| Private-E | 0.96 (0.84, 1.09) | 1.31 (1.15, 1.50) | 1.40 (1.26, 1.56) | 1.30 (1.16, 1.46) |
| Medicare HMO | 1.02 (0.84. 1.22) | 0.98 (0.80, 1.20) | 1.47 (1.31, 1.65) | 1.41 (1.21, 1.63) |
| Medicare only | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
aThe main effect for the insurance-type variable was significant (χ25 = 13.29; P = .0209). Statistically significant differences were observed among the various insurance–generosity combinations (χ223 = 193.52; P < .0001).
bFor explanation of insurance types, see footnotes b through e to Table 1 ▶.
cFor explanation of generosity levels, see footnote h to Table 1 ▶.
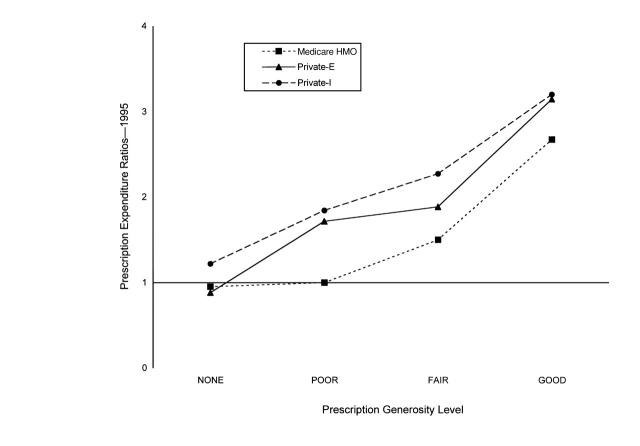
Figure 2 ▶ presents graphically the outpatient prescription expenditure ratios reported in Table 3 ▶. As prescription coverage generosity increases, per capita expenditure ratios rise consistently for all insurance groups. Moreover, these ratios continue to increase at all generosity levels and do not peak or taper off at poor or fair levels. At the highest level of generosity for the private insurance types (Private-E and Private-I), the per capita expenditures are approximately 3 times the Medicare-only baseline expenditure. Again, as in the case of event ratios, Private-I per capita expenditure ratios are greatest, followed by Private-E, Medicare HMO, and the Medicare-only baseline. The main effect for the insurance-type variable is significant (F5 = 10.95; P < .0001). Statistically significant differences were observed among the various insurance–generosity combinations presented in Figure 2 ▶ and Table 3 ▶ (F23 = 28.32; P < .0001).
FIGURE 2.
—1995 Prescription expenditure ratio of each insurance type by prescription generosity level.
TABLE 3.
—Prescription Expenditure Ratios (With 95% Confidence Intervals) of 1995 Sample Populationa: Medicare Current Beneficiary Survey
| Generosity Levelc | ||||
| Insurance Typeb | None | Poor | Fair | Good |
| Private-I | 1.22 (1.05, 1.41) | 1.83 (1.56, 2.16) | 2.27 (1.90, 2.71) | 3.19 (2.41, 4.22) |
| Private-E | 0.88 (0.74, 1.05) | 1.72 (1.40, 2.11) | 1.89 (1.62, 2.21) | 3.15 (2.67, 3.72) |
| Medicare HMO | 0.95 (0.74, 1.22) | 1.00 (0.76, 1.32) | 1.51 (1.27, 1.79) | 2.68 (2.16, 3.36) |
| Medicare only | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
aThe main effect for the insurance-type variable was significant (F5 = 10.95; P < .0001). Statistically significant differences were observed among the various insurance–generosity combinations (F23 = 28.32; P < .0001).
bFor explanation of insurance types, see footnotes b through e to Table 1 ▶.
cFor explanation of generosity levels, see footnote h to Table 1 ▶.
DISCUSSION
This is one of the first studies to show that prescription expenditure rises through all levels of plan generosity, regardless of insurance type. This result is consistent with findings from a study by Davis et al. that compared the prescription expenditures of Medicare beneficiaries who had a prescription coverage benefit with those of beneficiaries without this benefit.7 Their expenditure ratio estimates for HMO, Private-E, and Private-I insurance types were quite consistent with our corresponding insurance types in the fair generosity level. (Our fair generosity level was used in the comparison because Davis et al. did not address generosity level of prescription.) This trend was also seen when we similarly examined data in the 1992, 1993, and 1994 MCBS Cost and Use files.31
In contrast, the Rand Health Insurance Experiment by Leibowitz et al. compared prescription expenditures for 2 groups of individuals, one with generous outpatient prescription coverage and the other with no prescription coverage.32 They found an expenditure ratio that was noticeably less than our ratios for generous (good) coverage. However, their study excluded individuals older than 65 years. It is reasonable to suppose that older persons on fixed or limited incomes might be more sensitive to insurance effect than younger, working members of the population.
Another notable finding from our study is that individuals with the Private-I type of insurance spend more on prescriptions than do individuals without such insurance, even when the specific Private-I insurance provides no prescription benefit at all. Possible reasons for these high expenditures may be that individuals with this type of insurance (1) more frequently visit medical providers and hence obtain more prescriptions, (2) visit medical providers who are specialists and are more likely to prescribe new—and therefore expensive—prescription medications, or (3) purchase more—or more expensive—prescription drugs than do individuals with the other 3 types of insurance.
In our examination of prescription events, we observed that prescription event ratios increased with plan generosity up to the fair level. The fact that use increases with generosity of prescription drug coverage is consistent with data from the Report to the President on Prescription Drug Coverage, Spending, Utilization, and Prices.33 That report, based on MCBS and Medical Expenditure Panel Survey data, found that Medicare beneficiaries with prescription coverage fill nearly 33% more prescriptions each year than do those without prescription coverage.33 There is nothing in the report that provides insight into the effects we observed at the highest generosity levels. Because prescription expenditure ratios showed no corresponding decline but instead continued to rise, one plausible explanation is that generous plans pay for prescriptions in larger quantities (e.g., 100-day supplies instead of 30-day supplies). Another explanation is that, compared with less generous prescription plans, generous plans may cover brand-name drugs even when a generic drug is available or may have no formulary restrictions on high-cost medications. Therefore, even though prescription events may decrease at the most generous level of coverage, the price per event (fill) may increase.
Several potential limitations are associated with our study. First, we did not have prescription policy characteristics with which to develop the generosity variable, because this information was not available in the MCBS data. Therefore, the generosity of the prescription coverage had to be constructed from indirect information and may not necessarily reflect true plan generosity. Second, although we tried to control for self-selection bias (i.e., choosing insurance coverage on the basis of expected use) with sociodemographic and health status factors, we may not have accounted for unknown factors that influence prescription use and expenditure. Third, the MCBS provided no information regarding the restrictiveness of a prescription drug formulary, which itself would influence per capita expenditure. Fourth, because this was a cross-sectional study, no causal inferences could be made. Finally, our expenditure and event ratios are conservative estimates; given that expenditure and event information came from the MCBS household survey, underreporting is probable.7,34
Despite these potential limitations, our study associates more generous prescription coverage with greater prescription expenditure and use among all insurance types, even after sociodemographic and health status variables are controlled. Future research should examine the relationship between the level of older persons’ access to essential pharmacotherapy (especially near-poor older persons and those with chronic disease) and health outcomes, quality of life, active-life expectancy, and changes in other health care expenditures.
Acknowledgments
This study was supported by a Dissertation Fellowship Grant from the Health Care Financing Administration (NIH-HCFA/30-P-91017/5–01), a University of Minnesota Center on Aging Research Graduate Student Award, and Veterans of Foreign Wars–endowed chair in Pharmacotherapy for the Elderly, College of Pharmacy, University of Minnesota.
This report was previously presented in part at the International Society of Pharmacoepidemiology Annual Conference, Toronto, Ontario, August 2001.
The authors would like to thank Ray E. Artz, PhD, for his statistical and editorial assistance, Angeline Carlson, PhD, for her advice in the design of this study, and Joseph T. Hanlon, PharmD, MS, for his valuable comments on an earlier draft of this manuscript.
Human Participant Protection This study has received approval (Federal guidelines 45 CFR Part 46.10[b] category #4) from the Institutional Review Board: Human Subjects Committee of the University of Minnesota. Human Subjects Code Number is 9802E00086.
All 3 authors wrote the manuscript and were involved in conception and design of the study, analysis and interpretation of the data, and drafting and revising the content.
Peer Reviewed
References
- 1.Poisal JA, Murray LA. Growing differences between Medicare beneficiaries with and without drug coverage. Health Aff. 2001;20:74–85. [DOI] [PubMed] [Google Scholar]
- 2.Blaum CS, Liang J, Liu X. The relationship of chronic diseases and health status to the health services utilization of older Americans. J Am Geriatr Soc. 1994;42:1087–1093. [DOI] [PubMed] [Google Scholar]
- 3.Chrischilles E, Foley DJ, Wallace RB, et al. Use of medications by persons 65 and over: data from the Established Populations for Epidemiologic Studies of the Elderly. J Gerontol. 1992;47:M137–M144. [DOI] [PubMed] [Google Scholar]
- 4.Olin GL, Liu H, Merriman B. Health and Health Care of the Medicare Population: Data From the 1995 Medicare Current Beneficiary Survey. Rockville, Md: Westat; 1999.
- 5.Shea D, Stewart RP. Demand for insurance by elderly persons: private purchases and employer provision. Health Econ. 1995;4:315–326. [DOI] [PubMed] [Google Scholar]
- 6.Stuart B, Shea D, Briesacher B. Dynamics in drug coverage of Medicare beneficiaries: finders, losers, switchers. Health Aff. 2001;20:86–99. [DOI] [PubMed] [Google Scholar]
- 7.Davis MH, Poisal JA, Chulis G, Zarabozo C, Cooper B. Prescription drug coverage, utilization, and spending among Medicare beneficiaries. Health Aff. 1999;18:231–243. [DOI] [PubMed] [Google Scholar]
- 8.Iglehart J. Medicare and prescription drugs. N Engl J Med. 2001;344:1010–1015. [DOI] [PubMed] [Google Scholar]
- 9.Stuart B, Grana J. Ability to pay and the decision to medicate. Med Care. 1998;36:202–211. [DOI] [PubMed] [Google Scholar]
- 10.Gianfrancesco F, Baines A, Richards D. Utilization effects of prescription drug benefits in an aging population. Health Care Financ Rev. 1994;15:113–126. [PMC free article] [PubMed] [Google Scholar]
- 11.Long SH. Prescription drugs and the elderly: issues and options. Health Aff. 1994;13:157–174. [DOI] [PubMed] [Google Scholar]
- 12.Stuart B, Coulson NE. Dynamic aspects of prescription drug use in an elderly population. Health Serv Res. 1993;28:237–264. [PMC free article] [PubMed] [Google Scholar]
- 13.England A, Hubbell K, Judkins D, Ryaboy S. Imputation of medical cost and payment data. In: Proceedings of the Section on Survey Research Methods. Alexandria, Va: American Statistical Association; 1994:406–411.
- 14.O’Connell J, Lo A, Ferraro D, Bailey RC. Sampling and Estimation Issues in the Medicare Current Beneficiary Survey. Rockville, Md: Westat; November 1998.
- 15.Chulis GS, Eppig F, Hogan M, Waldo D, Arnett R. Health insurance and the elderly: data from MCBS. Health Care Financ Rev. 1993;14:163–181. [PMC free article] [PubMed] [Google Scholar]
- 16.Eppig F, Chulis GS. Matching MCBS and Medicare data: the best of both worlds. Health Care Financ Rev. 1997;18:211–229. [PMC free article] [PubMed] [Google Scholar]
- 17.Eppig FJ, Edwards B. Computer matching of Medicare Current Beneficiary Survey Data with Medicare claims. In: Richard Warnecke, ed. Proceedings of the Sixth Conference on Health Survey Research Methods; 1995 June 24–26; Breckenridge, Colo. Hyattsville, Md: National Center for Health Statistics; 1996:191–196. DHHS publication PHS 96-1013.
- 18.Davidson B, Sofaer S, Gertler P. Consumer information and biased selection in the demand for coverage supplementing Medicare. Soc Sci Med. 1992;34:1023–1034. [DOI] [PubMed] [Google Scholar]
- 19.Miller RH. Access to ambulatory care among noninstitutionalized, activity-limited persons 65 and over. Soc Sci Med. 1992;34:1237–1247. [DOI] [PubMed] [Google Scholar]
- 20.Wolinsky F, Johnson RJ. The use of health services by older adults. J Gerontol. 1991;46:S345–S357. [DOI] [PubMed] [Google Scholar]
- 21.Holden KC, Smeeding TM. The poor, the rich, and the insecure elderly caught in between. Milbank Q. 1990;68:191–220. [PubMed] [Google Scholar]
- 22.Leon J, Lair T. Functional status of the noninstitutionalized elderly: estimates of ADL and IADL difficulties. In: National Medical Expenditure Survey, Research Finding 4. Rockville, Md: Agency for Health Care Policy and Research; 1990:1–19. PHS publication 90-3462.
- 23.Lubitz J. Health status adjustments of Medicare capitation. Inquiry. 1987;24:362–375. [PubMed] [Google Scholar]
- 24.Kreling DH, Wiederholt JB. Selecting health insurance: the importance of prescription drug coverage and pharmacy factors in consumer decision making. J Pharm Mark Manage. 1987;1(4):3–18. [DOI] [PubMed] [Google Scholar]
- 25.Wolfe B, Gabay M. Health status and medical expenditures: more evidence of a link. Soc Sci Med. 1987;25:883–888. [DOI] [PubMed] [Google Scholar]
- 26.Katz S. Assessing self-maintenance: activities of daily living mobility and instrumental activities of daily living. J Am Geriatr Soc. 1983;31:721–727. [DOI] [PubMed] [Google Scholar]
- 27.Le CT. Applied Categorical Data Analysis. New York, NY: John Wiley & Sons Inc; 1998.
- 28.SAS/STAT Software: Changes and Enhancements Through Release 6.12. Cary, NC: SAS Institute Inc; 1997.
- 29.SAS Version 8 [computer program]. Cary, NC: SAS Institute Inc; 1999.
- 30.Administration on Aging. Older Persons With Mobility and Self-Care Limitations: 1990. Washington, DC: US Dept of Health and Human Services; 1996. Available at: http://www.aoa.dhhs.gov/aoa/stats/moblimit/mobilitylimit.htm. Accessed May 20, 2002.
- 31.Artz MB. The Impact of Outpatient Prescription Drug Coverage on Total and Specific Health Care Expenditure and Service Use of Medicare Beneficiaries, Age Sixty-Five and Older [dissertation]. Minneapolis: University of Minnesota; 2000.
- 32.Leibowitz A, Manning WG, Newhouse JP. The demand for prescription drugs as a function of cost-sharing. Soc Sci Med. 1985;21:1063–1069. [DOI] [PubMed] [Google Scholar]
- 33.Report to the President: Prescription Drug Coverage, Spending, Utilization, and Prices. Rockville, Md: US Dept of Health and Human Services; April 2000. Available at: http://www.aspe.hhs.gov/health/reports/drugstudy. Accessed May 20, 2002.
- 34.Wallihan DB, Stump TE, Callahan CM. Accuracy of self-reported health services use and patterns of care among urban older adults. Med Care. 1999;37:662–670. [DOI] [PubMed] [Google Scholar]