Abstract
Objectives. This study was undertaken to establish the health status of users of complementary and alternative medicine (CAM) services in England.
Methods. A postal questionnaire (response rate: 64%) covering long-standing illness, use of conventional medical and CAM services, and the United Kingdom Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) was sent to more than 14 000 adults in 4 counties.
Results. Sixty percent of CAM users reported having a chronic illness or disability; back pain and bowel problems were the conditions most commonly reported. Regardless of whether chronic illness was reported, CAM users reported poorer health than nonusers, particularly in the dimensions of pain and physical disability, and made more visits to general practitioners.
Conclusions. In England, users of CAM services have poorer physical health than nonusers and make more frequent use of conventional medical services.
In the United States, an estimated 629 million visits were made in 1997 to complementary and alternative medicine (CAM) practitioners. This estimate exceeded the total visits to all US primary health care physicians1 and represented a 47.3% increase in total visits from 1990.1,2 Between 1990 and 1997, expenditures for CAM increased 45.2% and were conservatively estimated at US $21.2 billion in 1997.1 Complementary medicine is used by 20%–50% of the population in many European nations3 and by 48% of the population in Australia.4
In the United Kingdom (UK), Thomas et al.5 surveyed 5010 individuals older than 18 years who were selected from a geographically stratified random sample of 12 English health authority populations. Their results suggested that approximately 10.6% of the adult English population consult a practitioner of 1 of 6 established CAM therapies each year. This study also suggested that as many as half of the UK population could be users of some form of CAM in their lifetimes, whether through over-the-counter purchases or consultations with CAM practitioners.
In 1997, data on health, health-related lifestyles, and use of medical services, including those of CAM practitioners,6 were gathered in a large survey of persons aged 18–64 years who were living in southeast England. We used these survey data to examine the health and demographic profiles of users of CAM practitioner services.
METHODS
Our survey was completed in 1997. Questionnaires were sent to 14 868 adults aged 18–64 years living in the counties of Berkshire, Buckinghamshire, Northamptonshire, and Oxfordshire. Names and addresses were selected at random from computerized registers of general practitioners (GPs) in proportion to the total number of patients registered. Because the proportion of the population not registered with GPs in the United Kingdom is exceedingly small, this sampling frame is representative of the population living in these counties.
We achieved a response rate of 64% (8889 respondents) after adjustment for returns from unknown, inappropriate, or deceased addressees. Although women were more likely to respond than were men, and the elderly more than the young, these response biases were small; the respondent population was broadly representative of both sexes and all sociodemographic groups.6
The questionnaire included the UK SF-36, the anglicized version of the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36), which covers 8 dimensions of health: energy and vitality, general health perception, pain, physical functioning, disabilities (role limitations) due to either physical health or mental health problems, and limitations in social activities due to any health problem. Higher scores denote better health status (0 being the worst state of health and 100 being the best).7 Respondents were asked whether they had any long-standing illnesses, disabilities, or infirmities, which were defined as “anything that has affected your work or other regular daily activities over a period of time or is likely to affect you over a period of time.” Those that responded positively were asked to identify their chronic illness(es) from 15 common conditions on a checklist derived from responses to a similar but open-ended question in a previous survey.8 Social class was coded from respondents’ reported occupational status according to the 1991 Registrar General’s classifications, which give 6 social class groups: I, professional and managerial; II, semiprofessional (e.g., teachers); IIIN, nonmanual–clerical; IIIM, manual–skilled manual work; IV, semiskilled manual work; and VI, unskilled manual work.9
The survey included a question on the use of health care practitioners, both conventional and complementary. The question asked was, “During the last three months, have you been seen by, or consulted, any of the following about your health?” Respondents were asked to circle all applicable responses from the following categories: district nurse, health visitor (a nurse specializing in health education, promotion, and illness prevention in young children), chiropodist, physiotherapist, community psychiatric nurse, family planning clinic, osteopath or chiropractor, counselor or psychotherapist, homeopath, herbalist, acupuncturist, other alternative therapist, religious or spiritual healer, self-help group, no one, or someone else (please specify whom).
Use of GPs’ services was assessed over the past year for the 12 months preceding the survey. The question asked was, “How often have you visited your doctor’s surgery (or health centre) for any reason in the past year? (Do not include visits made when accompanying your children or another patient.)” Respondents were asked to circle responses ranging from never to 6 or more times.
Data were coded, entered, and analyzed with SPSS for Windows 9.0 (SPSS Inc, Chicago, Ill.). For statistical analyses, χ2 tests were used to detect significant differences between any 2 groups (e.g., between sexes) in the proportion of respondents using CAM practitioner services. Both the Crosstabs function in SPSS and the Georgetown University Web Chi Square Calculator13 were used for χ2 tests. The Pearson χ2 was calculated for tests of associations except where small sample sizes were encountered and counts within a cell of a 2 × 2 table had an expected frequency of less than 5, in which case a Fisher exact test was computed. Means were compared with t tests.
To investigate which long-standing illnesses predicted use of each individual type of CAM practitioner, we used a series of multivariate regression models that included all of the following variables: type of long-standing illness, social class, sex, high-level use of general practitioner services (defined as ≥ 4 visits per year), and age. Odds ratios (ORs) were calculated where appropriate. Univariate analyses with χ2 tests were carried out to identify explanatory variables for inclusion in the logistic models. Only those variables that were identified as significant were included. Most variables were dichotomized to allow a greater number of variables to be investigated.10 Missing data account for the slightly differing numbers and percentages in the text and tables. Results were considered significant when P < .05.
RESULTS
Demographic Characteristics of CAM Users
Approximately 1 in 15 respondents (7.8%, n = 695; 95% confidence interval [CI] = 7.3, 8.4) reported that they had consulted a CAM practitioner in the 3 months before the survey. Nearly 1 in 10 women (9.5%) vs roughly 1 in 20 men (5.5%) reported visiting CAM practitioners (P < .001). Use was lowest among those younger than 35 years and highest in the 35–44 age group (9.2% of this age group had consulted a CAM practitioner) (Table 1 ▶). The mean age of respondents who used CAM practitioners was 43.2 years (95% CI = 42.4, 44.1).
TABLE 1.
—Proportion of Survey Respondents Aged 18–64 Years Who Consulted Complementary and Alternative Medicine (CAM) Practitioners in the 3 Months Prior to Survey (N = 8889)
| No. of Respondents (% of Population) | Respondents Using CAM, No. (%) | |
| Sex | ||
| Male | 3863 (43.9) | 214 (5.5) |
| Female | 4938 (56.1) | 471 (9.5) |
| Age group, y | ||
| 18–24 | 980 (11.2) | 42 (4.3) |
| 25–34 | 2003 (22.9) | 137 (6.8) |
| 35–44 | 2129 (24.3) | 195 (9.2) |
| 45–54 | 2112 (24.1) | 177 (8.4) |
| 55–64 | 1529 (17.5) | 128 (8.4) |
Of the 695 respondents who reported that they consulted CAM practitioners, 544 (78.3%) were from nonmanual social classes (I, II, and IIIN), with more than 45% from social class II alone. In the survey population as a whole, 58% of respondents were from nonmanual social classes and 35% were from social class II.
Health Status of CAM Users
Of respondents who indicated that they had visited a CAM practitioner, 417 (60%) also reported at least 1 chronic illness, which is significantly higher than the proportion of the general population reporting chronic illness (41.6%, n = 3697; P < .001). Respondents with chronic illness who used CAM were more likely than those who did not (48.2%, n = 199 vs 40.8%, n = 1328; P < .01) to consult their GPs frequently (≥ 4 times per year). In a multivariate regression analysis, the predictors of CAM use were long-standing illness (OR = 2.07, 95% CI = 1.73, 2.49), nonmanual social class (OR = 2.00; 95% CI = 1.63, 2.45), female sex (OR = 1.60; 95% CI = 1.33, 1.92), and high levels of GP service use (OR = 1.32; 95% CI = 1.09, 1.58).
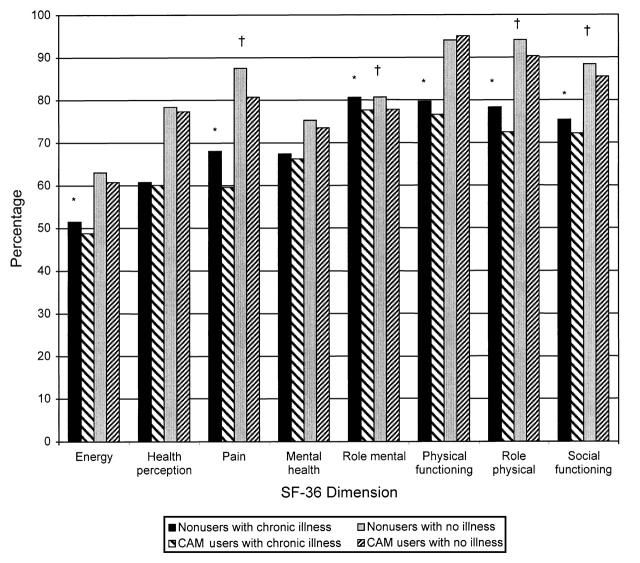
UK SF-36 Scores of CAM users were poorer than those of nonusers in 6 of the 8 SF-36 dimensions defined in Methods, with the exception of mental health and health perception (Figure 1 ▶). The mean difference in pain scores was 8.4 points and in disability due to physical health problems scores, 5.8 points. Mean differences for other dimensions were lower, between 2.8 and 3.2 points.
FIGURE 1.
—SF-36 scores for users and nonusers of CAM both with and without chronic illnesses.
The SF-36 scores of CAM users who did not report chronic illnesses were also lower than those of CAM nonusers in 4 dimensions. The dimension most affected was pain (5.8 points), but disability due to physical and mental health problems and social functioning were also lower in this group. CAM users who did not report chronic illnesses were also more likely than CAM nonusers to consult their GPs frequently during the year (≥ 4 times a year, 24.5%, n = 68 vs 15.5%, n = 761; P < .001).
Chronic Illnesses Associated With Use of CAM Services
The most common chronic illnesses reported by survey respondents were arthritis (17.3%) and back pain (15.6%). Use of CAM practitioners was most common among back pain sufferers (18.0%) and those reporting bowel problems (16.1%). Because back pain was so common in this survey, this condition accounted for 35% of all CAM use. Of those reporting other chronic illnesses, between 10.3% (asthma) and 12.3% (indigestion) had visited a CAM practitioner in the 3 months before the survey, compared with 5.4% of those reporting no long-standing illness. A series of multivariate regression models (Table 2 ▶) was used to investigate which long-standing illnesses predicted the use of each specific CAM practitioner service.
TABLE 2.
—Illnesses That Were Significant Predictors of Visits to Specific Complementary and Alternative Medicine (CAM) Practitioners in Multivariate Regression Modeling
| Illness/Proportion of Sufferers Using CAM, % (n) | |||||||||
| Specific Therapy | Asthma, 10.3 (64) | Arthritis, 11.8 (71) | Anxiety, 12.3 (58) | Problems With Bowels, 16.1 (83) | Back Pain, 18.0 (248) | Indigestion, 12.3 (48) | Depression, 12.0 (70) | Diabetes, 6.2 (8) | Skin Problems, 9.8 (44) |
| Homeopathy | . . . | 2.28 (1.05–4.93) | . . . | 2.57 (1.13–5.84) | . . . | 2.57 (1.13–5.84) | 2.17 (1.07–4.41) | . . . | 2.28 (1.07–4.89) |
| Herbalism | 3.34 (1.40–7.99) | . . . | 2.88 (1.06–7.82) | . . . | . . . | . . . | . . . | . . . | . . . |
| Osteopathy/chiropractic | . . . | . . . | . . . | . . . | 5.60 (4.35–7.21) | . . . | . . . | . . . | . . . |
| Religious/spiritual healing | . . . | . . . | . . . | 2.91 (1.45–5.83) | . . . | . . . | 2.33 (1.13–4.71) | 6.18 (2.03–18.85) | 2.50 (1.07–5.87) |
| Acupuncture | . . . | . . . | . . . | . . . | . . . | . . . | . . . | . . . | . . . |
| “Other” | . . . | . . . | . . . | . . . | . . . | . . . | . . . | . . . | . . . |
Note. Odds ratio (OR) for illnesses that were significant predictors (P < .05) of visits to specific CAM practitioners. CI = 95% for OR (in parentheses). Ellipses indicate an illness is not a significant predictor of visits to specific CAM practitioners.
People who reported suffering from arthritis, indigestion, depression, problems with bowels, and skin problems were more likely than the general population to have visited homeopaths. Asthma and anxiety predicted visits to herbalists. Back pain was the only chronic illness to predict the use of osteopathic/chiropractic services. Bowel problems, depression, diabetes, and skin problems predicted visits to spiritual and religious healers. Respondents who consulted acupuncturists or other CAM practitioners were no more likely than the general population to suffer from any specific chronic illness.
DISCUSSION
This survey demonstrates substantial use of CAM practitioner services among persons aged 18–64 years living in southeast England, particularly women. The rate of use in this survey is comparable to that reported by Thomas et al.5 for people living other parts of England (10.6%), which suggests that the population we surveyed did not differ greatly in terms of CAM use from the population in other parts of England. As might be expected of services that are usually funded out of pocket (in contrast to general medical services, which are free in the United Kingdom), we identified a bias toward higher social classes with respect to CAM use.
Our study has a number of limitations related to the fact that information about CAM services was a small component of the survey. For example, rates of use of CAM practitioners could not be estimated because respondents were not asked about the number of times that they had used a particular CAM therapy. Annual utilization rates could not be calculated because the survey requested data only on the previous 3 months’ use of CAM practitioners. Data on self-medication and use of over-the-counter products were not collected. Other studies, from America1,2,11 and Australia,4 have indicated that self-medication accounts for by far the largest segment of the CAM market. Thomas et al.5 examined over-the-counter purchases of herbal remedies and homeopathic medications over a 12-month period. Their study estimated that, over a period of 1 year, these 2 types of products were purchased by 22.1% of adults in England.
The categories of CAM were broad and general in our study. Herbalism is a heterogeneous treatment modality, encompassing traditional Chinese medicine, Indian ayurvedic medicine, Western herbalism, and other schools of treatment. The combining of osteopathy and chiropractic services into a single category created limitations. Data on patient satisfaction with CAM practitioner services were not available. The response rate of only 64% was less than ideal. The survey was also inherently biased, in that children and people aged 64 years or older were excluded. Nonetheless, this study adds useful information to what is known about CAM use in the United Kingdom.
The majority of CAM users reported suffering from a long-standing illness, disability, or infirmity, and back pain was the most commonly reported of these problems. This majority also reported high levels of use of GPs’ services, which means that this group used CAM services in addition to rather than instead of standard medical services. Although back pain sufferers were more likely to use only chiropractic or osteopathic services, people with a wider range of illnesses were attracted to other CAM services.
SF-36 scores among persons suffering from chronic illness suggest that pain was the most important problem predicting use of CAM services. Disability due to physical health problems was also important. Mental health problems, however, did not appear to be an important predictor of CAM use, as would be expected if there had been a high level of somatizing patients among those using CAM services.
Forty percent of CAM users did not report a chronic illness. Interestingly, however, the SF-36 scores for this group, despite indicating better health relative to CAM users with chronic illness, were worse in 4 of 8 SF-36 dimensions compared with nonusers without illness. Pain and disability due to physical health problems were the dimensions most affected in this group, and mental health problems were no more prevalent than they were in nonusers. CAM users were also more likely than CAM nonusers to be high-level users of GPs’ services, reinforcing the idea that CAM services are used in tandem with standard medical services.
SF-36 scores were recently reported among users of CAM services referred by GPs and hospital doctors to a London hospital outpatient service that provided acupuncture, osteopathy, and homeopathy.12 Such services are unusual in the United Kingdom and are likely to attract people whose conditions have proved resistant to treatment by other medical services. As might be expected in this population, SF-36 scores showed significantly more depression than do the scores we report here. Also in contrast to our findings, although pain scores were low, the most affected health dimensions for this group were physical functioning and disability due to physical health problems. SF-36 scores derived from our study are likely to be more representative of all users of CAM services.
Policymakers in the United Kingdom are demanding further evidence of efficacy, cost effectiveness, and safety of CAM therapies before considering inclusion of their coverage in the National Health Service.13 Meanwhile, a substantial proportion of the general public, both those who are chronically ill and those who are not, are clearly prepared to pay for CAM services out of pocket. The results of this survey suggest that the most important reason for CAM use is to treat pain. Estimates5 suggest that out-of-pocket expenditure for practitioner-mediated CAM therapies in the United Kingdom is approximately £450 million a year. It seems there is room for debate regarding who decides what is and is not effective and on what grounds, at least in the United Kingdom.
Acknowledgments
The Health Services Research Unit, Department of Health, University of Oxford is supported by a grant from the National Health Service research and development program. C.-K. Ong and G. C. Bodeker were supported by a grant from the Henry Smith Charity. The survey was funded by the directors of public health in the 4 counties where our survey was conducted.
We also thank Helen Doll for very helpful statistical advice and guidance.
Human Participant Protection Ethical consent for the survey was obtained from the Oxfordshire Research Ethics Committee, United Kingdom.
C.-K. Ong conducted the analyses presented in this article. The survey was undertaken by S. Stewart-Brown as principal investigator and S. Petersen as research officer; they were responsible for data preparation and univariate analyses of the data. S. Stewart-Brown and G. C. Bodeker suggested the contents of the article structure of the article and helped in the design of the analyses and drafting of the article.
Peer Reviewed
References
- 1.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280:1569–1575. [DOI] [PubMed] [Google Scholar]
- 2.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328: 246–252. [DOI] [PubMed] [Google Scholar]
- 3.Fisher P, Ward A. Complementary medicine in Europe. BMJ. 1994;309:107–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.MacLennan AH, Wilson DH, Taylor AW. Prevalence and cost of alternative medicine in Australia. Lancet. 1996;347:569–573. [DOI] [PubMed] [Google Scholar]
- 5.Thomas KJ, Nicholl JP, Coleman P. Use and expenditure on complementary medicine in England: a population based survey. Complement Ther Med. 2001;9:2–11. [DOI] [PubMed] [Google Scholar]
- 6.Petersen S, Stewart-Brown S, Peto V. Health and Lifestyles in Four Counties: Results from the Third Healthy Lifestyle Survey. Oxford, England: Health Services Research Unit, University of Oxford, 1998:6–8.
- 7.Jenkinson C, Layte R, Wright L, Coulter A. The UK SF-36: An Analysis and Interpretation Manual. Oxford, England: Health Services Research Unit, University of Oxford, 1996.
- 8.Knight M, Stewart-Brown S, Fletcher L. Estimating health needs: the impact of a checklist of conditions and quality of life measurement on health information derived from community surveys. J Public Health Med. 2001;23:179–186. [DOI] [PubMed] [Google Scholar]
- 9.Office of Population Censuses and Surveys. Standard Occupational Classification, Vols 1, 2, and 3. London, England: Her Majesty’s Stationery Office; 1991.
- 10.Harrell FE Jr, Lee KL, Califf RM, Pryor DB, Rosati RA. Regression modelling strategies for improved prognostic prediction. Stat Med. 1984;3:143–152. [DOI] [PubMed] [Google Scholar]
- 11.Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279:1548–1553. [DOI] [PubMed] [Google Scholar]
- 12.Richardson J. Developing and evaluating complementary therapy services: part 2. Examining the effects of treatment on health status. J Altern Complement Med. 2001;7:315–328. [DOI] [PubMed] [Google Scholar]
- 13.House of Lords. Science and Technology Select Committee Report on Complementary and Alternative Medicine. London, England: Her Majesty’s Stationery Office, 2000.
- 14.Georgetown University Web Chi Square Calculator 0.1b. Available at: http://www.georgetown.edu/cball/webtools/web_chi.html. Accessed July 13, 2001.