Abstract
Objectives. This study evaluated a community-based program in China to prevent initiation of drug use in young men.
Methods. Similar intervention and control areas were selected. Village leaders, teachers, and women and youth leaders were recruited to participate in the program. Community activities were organized and intervention activities in schools were implemented. Incidence of new drug users was estimated.
Results. There was a 2.7-fold greater reduction in drug use initiation in the intervention area (1.59% vs 0.60%). Reduction was highest among males aged 15 to 19, single men, illiterate men, and the Jingpo minority. HIV/AIDS knowledge and attitudes and recognition of drug problems were all significantly better in the intervention area.
Conclusions. Community-based intervention programs to prevent drug use can be successful in rural areas of China.
Drug abuse has become a significant problem in China. While the reported number of users increased from 70 000 in 1990 to 901 000 in 2001, a 12.9-fold increase,1 the actual number in 2000 was estimated to be 6 to 8 million.2
The resurgence of drug use, predominately among young males, started in southwest China in the early 1980s.3,4 The prevalence of drug use in Yunnan among males aged 18 to 29 years reached 28% in the epidemic areas in 1994.4 In 1989, the first known epidemic of HIV in China was discovered among injecting drug users in Ruili,5 40% of whom were found to be HIV positive. By 1999, the epidemic had spread to 108 of the 126 counties of Yunnan Province. Ruili and Longchuan counties had the highest prevalence of drug use and HIV infection (40%–80% among injectors).6–14
The populations of the villages in these 2 counties range from 80 to 300 persons. Almost everybody in each village knows who is a drug user. Many drug users have been referred to rehabilitation centers, but the relapse rate is above 95%, indicating that this strategy is failing.
The main drugs used are opium and heroin. Opium is smoked with a pipe. Heroin is used by smoking heroin-laced cigarettes, by “chasing the dragon” (i.e., inhaling vapors), or by intravenous injection3,4 (uncommon before 1984). The proportion of drug users that injected drugs, which was 13.5% in 1988, rose to 41.6% to 44.0% in the period 1994 to 1997 and to 53.3% in 1999.6,11,15,16 Our previous study showed that the incidence of injecting drug use in the 2 groups of villages reported on in this study increased from 10% in 1991 to over 30% in 1994.17 Sharing injection and smoking equipment was common. Among 192 injectors, 140 (73%) had shared equipment at least 3 times and 105 (75%) were regular sharing injectors.18 Unfortunately, knowledge about HIV/AIDS was low among drug users; only 41.8% of all drug users knew that sharing needles for drug injection may spread HIV. Only 12% perceived that they might be infected with HIV.18
Drug use has led to many social problems, the true dimensions of which are probably underestimated. Clearly, there are substantial costs as a result of the direct and indirect damage caused by drugs. A combined and coordinated strategy involving different sectors of the community is needed to effectively address drug prevention.
There has been substantial scientific research on the effectiveness of “community-based” approaches to influence population health behaviors.19–31 Such approaches typically combine interventions to enable families, peers, schools, media, and relevant organizations within a given community to address behavioral and environmental factors. They have been particularly successful in China for family planning.32–34
The rationale for conducting an experimental, community-based drug intervention program was based on several observations. First, drug abuse is prevalent in all the communities of the area bordering Southeast Asia, which is the epicenter of the HIV epidemic in China.3,11 Second, drug use is established in adolescence or early adulthood,4 and it is costly and difficult to change once established. The prevention of drug use would also subsequently eliminate drug injecting and related deaths and HIV infections. Third, drug abuse is a social behavior, embedded in the larger framework of community norms and social support systems that regulate the occurrence of these behaviors. Fourth, community intervention has proven effective for health problems such as smoking. Fifth, an intervention program would complement the efforts being made by the government to eliminate the production, distribution, and smuggling of drugs.35
Finally, a strong social network and health infrastructure existed in these communities that could facilitate the development of a community-based intervention program. The combined effort of the health infrastructure and the social network successfully eradicated the drug abuse problem in China from the 1950s to the 1970s.36 Involving the social network would mobilize community resources for the reduction of drug initiation. For these reasons, a comprehensive community-based program to reduce the incidence of drug initiation among adolescent young adult males was started in Longchuan County in 1997. The results of that study are reported here.
METHODS
Definition of Drugs
Drugs refer to recreational drugs only; these include opium, heroin (now the most commonly used drug), and tranquilizers. Cigarettes and alcohol are not defined as drugs in this study.
Study Design
An unblinded, matched community-based trial to prevent initiation of drug use was implemented in 1997. Thirty-eight villages were selected from the 83 included in our previous study conducted in 1994.4 The selected villages had a high incidence of new drug users in the earlier study. Nineteen villages and 10 schools in one cluster were allocated randomly to the intervention group and 19 villages and 9 schools to the comparison cluster (control area). Both clusters were close to main roads but were separated by a distance of at least 15 miles; between them were uninvolved villages and mountains. Villages close to roads were selected because (1) they had higher rates of drug use and HIV infection and (2) the presence of roads facilitated the initiation and monitoring of intervention activities. Villages were matched only for the prevalence of drug use, based on our previous study,4 and for the number of drug users documented by the Longchuan County Narcotics Control Office in 1996.
There were no intervention activities organized in the control villages. We report only on prevention of new drug users.
Theoretical Frameworks
Theoretical frameworks used to guide the development of the educational intervention included the community organization model, in which community leadership and local residents are mobilized for social action,37 and the behavior change model, based on Bandura’s social learning theory, which suggests that new behaviors can be induced from exposures to powerful models and are maintained through social reinforcements.38 The persuasive influences were considered to be community norms, village leaders, parents and grandparents, significant others, and peers.
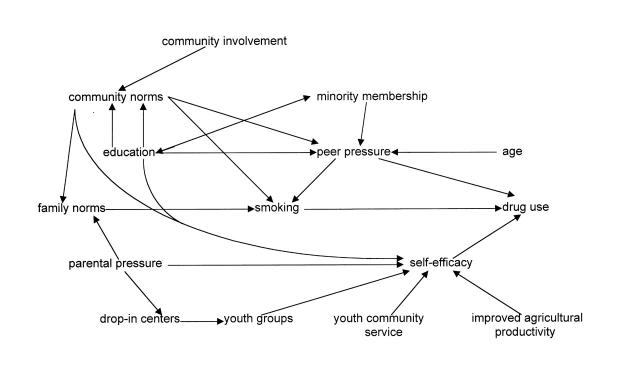
Figure 1 ▶ presents a theoretical model of factors influencing the initiation of drug use, including self-efficacy and youth activities, community service, and instruction on agricultural productivity to increase a sense of self-efficacy. Community involvement in designing and implementing intervention strategies was designed to influence community norms (e.g., smoking, educational attainment, family norms, and peer pressure) that influence the decision to take drugs.
FIGURE 1.
—Model for factors influencing the initiation of drug use: Yunnan, China.
Moral principles,39 as well as pragmatic principles, were used to encourage preadolescents, adolescents, and young adult males to avoid drugs and thereby contribute to the well-being of both the community and themselves. Rural villages are very conservative and tend to interpret issues as “good” or “bad” (evil). Thus, the villages elected to use these concepts in developing their intervention messages. Social marketing principles40,41 were used to guide the design of the educational messages.
Strategies
An effort was made to involve everyone in the community in the intervention activities. Certain groups, however, were in a unique position to intervene; these included community leaders, schoolteachers, and village health workers. Other groups recruited included youth leaders, women’s groups, parents, grandparents, and former drug users. Four overlapping educational strategies were used to encourage each group to play a significant role in the prevention effort: a school approach, a family approach, a community approach, and a clinic approach.
Interventions
In January 1997, Longchuan government and department leaders, village leaders, health workers, and schoolteachers were involved in the intervention planning. Three meetings were initially organized: the first with leaders from the different county government sectors involved in public health and drug problems, the second with village leaders from all 19 villages in the intervention area, and the third with the director of the Longchuan County Education Department and rectors from schools in the intervention area. Workshops and regular meetings for village leaders and others were organized, games and videos with drug prevention messages were provided, and classes to improve literacy and agricultural yield were conducted. School programs were implemented, including didactic work, visits to detoxification centers, and participation in drug intervention activities. A detailed description of the specific intervention activities is available at http://www.ph.ucla.edu/epi/faculty/detels.html.
Evaluation
In October 1998, all males aged 15 to 49 years in both the intervention and control areas were invited to participate in the evaluation survey. The questionnaire was anonymous. The interviewers were not from the villages and had not been involved in the intervention activities. Information collected included personal background, knowledge of and attitudes toward drugs and AIDS, previous and current drug use, and previous and current sexual behaviors. Additional data about drug use in each village were collected from village heads and youth leaders to verify the survey data.
Data Analysis
A cohort was reconstructed on the basis of the results of the 1998 cross-sectional survey. Participants were asked when they had initiated drug use. Thus, the incidence for specific time periods before the survey could be determined retrospectively. This method was first used in the 1994 survey to retrospectively estimate incidence before the crosssectional survey.4 The 17-month period between October 1995 and February 1997 was used to estimate incidence before the intervention was initiated. The 17-month period from May 1997 to September 1998 was used to estimate incidence after the intervention was initiated. The incidence of new drug users was estimated for both 17-month periods, before and after the intervention. The ratios of the change in incidence in the intervention and control areas before and after the initiation of the intervention were calculated to determine the impact of the intervention. A ratio of greater than 1 indicated that the reduction in incidence from the period before to the period after the intervention was greater in the intervention area than in the control area. The Kornfield 95% confidence interval was calculated for these ratios and the Mantel–Haenszel test was used for determining the probabilities. The χ2 test was used for comparing level of knowledge and attitudes between intervention and control groups.
RESULTS
A total of 559 males in the control villages and 748 males in the intervention villages were interviewed, with a response rate of 91% in the intervention villages and 88% in the control villages. There were no significant differences in age distribution or marital status among subjects in the intervention and control communities. The proportion with secondary education was slightly higher in the intervention villages than in the control villages (29.2% vs 22.2%; P < .01). In the intervention villages, however, the proportion belonging to the Jingpo minority was twice that of the control villages (54.6% vs 25.4%; P < .01) and the proportion belonging to the Dai minority was less than half (28.3% vs 56.5%; P < .01). The proportion of Jingpo men who used and injected drugs was much higher than for the other ethnic groups in the areas.4
Table 1 ▶ presents the incidence of new drug users in the 2 areas before and after the intervention program. The incidence decreased in the intervention area from 3.47% to 1.88% and in the control area from 2.10% to 1.50%, a 2.7-fold greater decrease in the intervention villages than in the control villages. The attributable risk reduction was 0.99% for the intervention vs control villages (P = .048). Major decreases were observed in the 15- to 19-year age groups (attributable risk reduction = 4.79%, P < .001; a 1.8-fold relative reduction), among single men (attributable risk reduction = 2.98%, P < .001; a 42.6-fold relative reduction), among the Jingpo ethnic group (attributable risk reduction = 3.01%, P < .001; a 2.9-fold relative reduction), and among the illiterate/semiliterate men (attributable risk reduction = 6.16%, P < .001; a 616-fold relative reduction). For each, the incidence increased in the control villages and decreased in the intervention villages. The incidence dropped to zero among the Han group, the major Chinese ethnicity, in both the intervention and control areas.
TABLE 1.
—Change in Incidence (%) of New Male Drug Users in Intervention and Control Areas Before and After Intervention Program: Longchuan County, Yunnan Province, China
| Intervention Area | Control Area | ||||||||
| Variable | Baseline Period (10/95–2/97) | Follow-Up Period (5/97–9/98) | Percentage-Point Change | Baseline Period (10/95–2/97) | Follow-Up Period (5/97–9/98) | Percentage-Point Change | Attributable Risk Reductiona | Incidence Ratio (95% CI) | P |
| Total | 3.47 (21/606) | 1.88 (11/584) | –1.59 | 2.10 (10/477) | 1.50 (7/466) | –0.60 | –0.99 | 1.3 (1.0, 1.8) | .048 |
| Age, y | |||||||||
| 15–19 | 3.30 (3/91) | 1.14 (1/88) | –2.16 | 0 (0/76) | 2.63 (2/76) | +2.63 | –4.79 | 152 (58, 429)b | <.001 |
| 20–29 | 6.82 (15/220) | 2.94 (6/204) | –3.88 | 4.12 (8/194) | 1.62 (3/185) | –2.50 | –1.38 | 0.9 (0.7, 1.2) | .43 |
| 30–39 | 1.66 (3/181) | 2.25 (4/178) | +0.59 | 1.38 (2/145) | 1.40 (2/143) | +0.02 | +0.57 | 0.8 (0.5, 1.0) | .07 |
| 40–49 | 0 (0/113) | 0 (0/113) | 0 | 0 (0/62) | 0 (0/62) | 0 | |||
| Marital status | |||||||||
| Single | 5.61 (11/196) | 2.70 (5/185) | –2.91 | 2.34 (4/171) | 2.41 (4/166) | +0.07 | –2.98 | 2.1 (1.7, 2.7) | <.001 |
| Married | 2.48 (10/403) | 1.53 (6/392) | –0.95 | 1.98 (6/303) | 1.01 (3/297) | –0.97 | +0.02 | 0.8 (0.6, 1.2) | .23 |
| Others | 0 (0/7) | 0 (0/7) | 0 | 0 (0/3) | 0 (0/3) | 0 | |||
| Ethnic group | |||||||||
| Jingpo | 5.59 (18/322) | 3.63 (11/303) | –1.96 | 3.45 (4/116) | 4.5 (5/111) | +1.05 | –3.01 | 2.0 (1.6, 2.4) | <.001 |
| Dai | 0.60 (1/168) | 0 (0/167) | –0.60 | 0.74 (2/270) | 0.75 (2/268) | +0.01 | –0.61 | 12.2 (4.4, 35.6)b | <.001 |
| Han | 1.83 (2/109) | 0 (0/107) | –1.83 | 5.41 (4/74) | 0 (0/70) | –5.41 | +3.58 | 0.3 (0.1, 1.4)b | .075 |
| Others | 0 (0/7) | 0 (0/7) | 0 | 0 (0/17) | 0 (0/17) | 0 | |||
| Education | |||||||||
| Illiterate/semiliterate | 7.50 (6/80) | 1.35 (1/74) | –6.15 | 0.94 (1/106) | 0.95 (1/105) | +0.01 | –6.16 | 5.6 (4.0, 7.7) | <.001 |
| Primary | 3.47 (12/346) | 2.10 (7/333) | –1.37 | 1.92 (5/260) | 1.57 (4/254) | –0.35 | –1.02 | 1.4 (1.0, 1.8) | .029 |
| Secondary | 1.69 (3/178) | 1.71 (3/175) | +0.02 | 3.60 (4/111) | 1.87 (2/107) | –1.73 | +1.75 | 0.5 (0.4, 0.7) | <.001 |
Note. CI = confidence interval.
aAttributable risk reduction = change in intervention group minus change in control group. Minus signs indicate decreases (i.e., actual reductions); plus signs indicate increases in attributable risk.
bAdjusted by using an incidence of 0.05% to replace 0% for calculating the incidence ratio.
Table 2 ▶ presents the attitudes and knowledge of drug use and AIDS among male villagers. After the intervention, the intervention group had a significantly greater perception of the problems of drug use and the AIDS epidemic in every category and a greater willingness to participate in activities to prevent drug use and AIDS transmission than in the control areas (P < .01). Individuals in the intervention area also had a greater knowledge about risk factors for drug use and knowledge of HIV transmission routes and prevention measures (P < .001).
TABLE 2.
—Attitudes and Knowledge Regarding Drug Use and AIDS Among Male Villagers in Intervention and Control Areas: Longchuan County, Yunnan Province, China, 1998
| Male Non–Drug Users Agreeing, % | Male Drug Users Agreeing, % | |||||
| Control (n = 459) | Intervention (n = 573) | χ2 (P) | Control (n = 100) | Intervention (n = 176) | χ2 (P) | |
| Attitudes | ||||||
| Drug use is a severe problem in my village. | 53.38 | 68.76 | 29.4 (.001) | 55.00 | 74.43 | 11.0 (.001) |
| Use of a drug affects me or my family. | 78.21 | 91.45 | 36.9 (.001) | 93.00 | 97.16 | 2.65 (.103) |
| AIDS is a severe problem in my village. | 24.40 | 40.49 | 29.68 (.001) | 25.00 | 39.20 | 5.73 (.017) |
| AIDS affects me or my family. | 74.95 | 86.04 | 20.5 (.001) | 84.0 | 88.64 | 1.20 (.272) |
| I should participate in preventing drug use/AIDS. | 89.11 | 96.51 | 22.1 (.001) | 90.00 | 96.02 | 4.0 (.045) |
| Knowledge | ||||||
| Knew smoking increases risk of drug use. | 52.29 | 61.43 | 8.71 (.003) | 53.0 | 53.98 | .02 (.876) |
| Correctly identified routes of transmission. | 15.69 | 59.16 | 201.0 (.001) | 14.00 | 52.84 | 40.53 (.001) |
| Had correct knowledge about prevention methods. | 20.92 | 49.04 | 86.95 (.001) | 21.00 | 55.11 | 30.32 (.001) |
| Answered correctly all questions on infection routes and prevention methods. | 5.23 | 37.17 | 147.0 (.001) | 6.0 | 36.36 | 31.06 (.001) |
DISCUSSION
This study used both a concurrent control and a pretest/posttest evaluation strategy. We were thus able to reduce the likelihood that changes observed in the intervention villages were due to changes occurring in the region as a whole. This design increases the likelihood that the greater magnitude of reduction observed in the incidence of new drug users was due to the community efforts organized in the intervention villages. The greater improvement in knowledge and attitudes in the intervention villages provides additional evidence that the program was responsible for the decline. Another advantage of the study was the high response rate (91% in the intervention villages and 88% in the control villages) for the evaluation survey, suggesting that the results are representative of the populations of young persons in the 2 areas. Different staff were involved in the intervention activities and in the pre- and postintervention surveys.
It is particularly encouraging that the greatest reductions were observed in the youngest age groups, among single individuals, among the Jingpo minority group, and among illiterate and semiliterate individuals, the groups most at risk for initiating drug use.4
The intervention involved the villagers themselves. No new outside personnel were hired; key individuals, including the village leaders and the village health workers, were trained in the strategies of community intervention. Key groups in the villages, including the women’s groups and the youth groups, were given the opportunity to express their concerns and to participate in community activities to improve the quality of life in the village. The cost of this community intervention was thus relatively low. This is important because some interventions proposed in previous research studies required resources to which most villages do not have access. Because the intervention described in this study relied, for the most part, on existing resources and personnel, it is feasible to implement in any village. With the exception of the distribution of condoms, most resources, including the technical assistance in agriculture, were already available to the villages. The community intervention program only provided the skills and information needed to bring them to the villages. Most importantly, villagers were given the opportunity to “own” the intervention because they played a key role in the development and implementation of the actual intervention activities. The prior study of the risk factors associated with initiation of drug use among young villagers in this area of China provided information that was useful in constructing the community intervention program.4
It is probable that the programs begun in the third grade of school will be helpful in reducing the incidence of new drug users in the future. Although there is some reluctance to initiate drug and sexual behavior programs in the early grades of school, such education cannot be delayed to the later grades. In most developing countries, most children receive only 6 years of schooling. Interventions introduced beyond grade 6 will not reach most young people, and it is this group of school dropouts, who are poor and relatively uneducated, that are most vulnerable to initiation of drug use.4 This study did demonstrate that villagers are willing to incorporate programs on drug use and HIV/AIDS into the schools even in the early grades.
The relative success of the program in the Yunnan villages may have been due in part to the small size of the villages (typically 50–100 families), which facilitated implementation of community mobilization. Two other factors may have contributed to the success of the program: the awareness of community members of the drug problems of many youths in their villages, and China’s history of successful community interventions in recent years.
There were limitations to this study. Although the villages were matched on the prevalence of drug use from the 1994 survey, both the incidence of drug use and the proportion of Jingpo, the minority group with the highest drug use and lowest education level, were significantly higher in the intervention villages. Thus, the challenge to reduce drug use may have been greater in the intervention areas than in the control areas.
Although the evaluation survey was anonymous, it is impossible to rule out the possibility that young men in the intervention villages were more likely not to report initiating drug use because they had been subjected to intense intervention activities against drug use. In fact, they demonstrated significantly higher levels of knowledge after the intervention than did young men in the control villages. Whether this knowledge convinced them to not initiate drugs or to lie about initiation is difficult to determine. Nonetheless, almost 2% of the young men in the intervention area did report initiating drug use despite the intervention program.
Although the intervention and control villages were separated by mountains and several uninvolved villages, some of the intervention messages and strategies may have reached the control villages as well. The Department of Education was so pleased with the intervention in the schools that it expanded the program 3 months after its start to all the schools in the county, including the schools in the control area. This would have had the impact of reducing the apparent difference in incidence between the intervention and control villages. Thus, our study may have underestimated the effectiveness of the community intervention program.
Because of limited funds, we were not able to extend the intervention and the observation periods beyond one year. This is important, because a key unanswered question is whether the intervention villages will be able to sustain their community activities without periodic reinforcement and whether the reduction in initiating new drug use will be sustained. Barrett and de Palo42 reported on a community-based intervention trial among Thai tribal villages, similar to those in this report, that was initially successful. However, the 6-month follow-up evaluation revealed a problem with sustainability. Perhaps the greatest benefit of this study will be to provide the rationale for support of longer-term studies using this community intervention approach.
In summary, this community intervention, which was based primarily on mobilization of existing community resources, was successful in reducing the incidence of new drug users, at least in the short term. Such an approach may be useful in other countries in which drug users remain a part of both their family and their community.
Acknowledgments
This project was funded by the World AIDS Foundation, grant WAF 112 (96–014).
The authors wish to thank Professor Naihua Duan for his helpful suggestions and Jean Savage and Elizabeth Lim for preparing and editing the manuscript.
Human Participant Protection The protocol for this study was approved by the institutional review boards of the University of California—Los Angeles and of the Chinese Academy of Preventive Medicine.
Z. Wu participated in conceptualizing the intervention project, directed the intervention program and the assessment of the intervention, and wrote the first draft of the manuscript. R. Detels was the principal investigator of the research grant, participated in development of the intervention program and assessment, and led revisions of the drafts of the manuscript. V. Li played a key role in developing the intervention strategies. J. Zhang and J. Li organized and supervised implementation of the intervention strategies.
Peer Reviewed
References
- 1.Annual Report on Drug Control in China, 2001 [in Chinese]. Beijing, China: Office of the National Narcotic Control Committee; February 2002:5.
- 2.Wu Z. Female drug users in China, what we know and what are gaps [in Chinese]. Paper presented at: Workshop of United Nations Drug Control Program and China National Bureau of Narcotics Control; February 22–24, 2001; Nanning, China.
- 3.Zhang W. The number 1 drug in the world. Lan Dun. 1994;115:24–29. [Google Scholar]
- 4.Wu Z, Zhang J, Detels R, et al. Risk factors for initiation of drug use among young males in southwest China. Addiction. 1996;91:1675–1685. [DOI] [PubMed] [Google Scholar]
- 5.Ma Y, Li Z, Zhang K, et al. HIV was first discovered among injection drug users in China [in Chinese]. Chin J Epidemiol. 1990;11:184–185. [Google Scholar]
- 6.Zheng XW, Tian CJ, Yang G, et al. A preliminary study on the behavior of 225 drug abusers and risk factors of HIV infection in Ruili County Yunnan Province [in Chinese]. Chin J Epidemiol. 1991;12:12–14. [PubMed] [Google Scholar]
- 7.Zhang J, Zheng X, Tian C, et al. An epidemiology study on AIDS in Ruili County of Yunnan Province [in Chinese]. Chin J Epidemiol. 1991;12:9–11. [Google Scholar]
- 8.Zhao S, Cheng H, Zhang J, et al. AIDS surveillance in Yunnan Province of China (1986–1990) [in Chinese]. Chin J Epidemiol. 1991;12:72–74. [PubMed] [Google Scholar]
- 9.Sun X, Nan J, Guo Q. AIDS and HIV infection in China. AIDS. 1994;8(suppl 2):S55–S59. [PubMed] [Google Scholar]
- 10.Cheng C, Zheng X, Liu K, Kang L, Hao R. Epidemiology of HIV/AIDS in China [in Chinese]. In: State Council Research Office, ed. Beware of AIDS: For the Survival of the Chinese Nation. Beijing, China: Xin Hua Publishing House; 1993:35–61.
- 11.Zheng X, Tian C, Choi K, et al. Injection drug use and HIV infection in southwest China. AIDS. 1994;8:1141–1147. [DOI] [PubMed] [Google Scholar]
- 12.Xia M, Kreiss JK, Holmes KK. Risk factors for HIV infection among drug users in Yunnan Province, China: association with intravenous drug use and protective effect of boiling reusable needles and syringes. AIDS. 1994;8:1701–1706. [PubMed] [Google Scholar]
- 13.Cheng HH, Zhang JP, Kou JD, et al. HIV/AIDS spread to the whole province of Yunnan [in Chinese]. Chin J Prev Control STD AIDS. 1997;2(2):54–57. [Google Scholar]
- 14.Wu Z. A Report on Investigation of Responses to AIDS in Yunnan [in Chinese]. Beijing, China: National Centre for AIDS Prevention and Control; October 1999.
- 15.Wu Z. Epidemics of HIV/AIDS in China [in Chinese]. In: Wu Z, Qi G, Zhang J, eds. Epidemiology and Intervention of AIDS in China. Beijing, China: Science Press; 1999:39–56.
- 16.National HIV/AIDS Sentinel Surveillance Report in 1999. National Center for AIDS Prevention and Control [in Chinese]. Beijing, China: Ministry of Health and National Center for AIDS Prevention and Control; 2000.
- 17.Wu Z, Detels R, Zhang J, et al. Risk factors for intravenous drug use and sharing equipment among young male drug users in southwest China. AIDS. 1996;10:1017–1024. [DOI] [PubMed] [Google Scholar]
- 18.Wu Z, Zhang J, Detels R, et al. Characteristics of risk-taking behaviors, HIV/AIDS knowledge and risk perception among young males in southwest China. AIDS Educ Prev. 1997;9:147–160. [PubMed] [Google Scholar]
- 19.Farquhar J, Maccoby N, Wood P, et al. Community education for cardiovascular health. Lancet. 1977;1:1192–1195. [DOI] [PubMed] [Google Scholar]
- 20.Salonen J, Puska P, Mustaniemi H. Changes in morbidity and mortality during comprehensive community program to control cardiovascular diseases during 1972–79 in North Karelia. BMJ. 1979;2:1178–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fortmann S, Williams P, Hulley S, Haskell W, Farquhar J. Effect of health education on dietary behavior: The Stanford Three Community Study. Am J Clin Nutr. 1981;34:2030–2038. [DOI] [PubMed] [Google Scholar]
- 22.Puska P, Nissinen A, Salonen J, Tuomilehto J. Ten years of the North Karelia Project: results with community-based prevention of coronary heart disease. Scand J Soc Med. 1983;11:65–68. [PubMed] [Google Scholar]
- 23.Puska P, Nissinen A, Tuomilehto J, et al. The community based strategy to prevent coronary heart disease: conclusions from the ten years of the North Karelia Project. Annu Rev Public Health. 1985;6:147–193. [DOI] [PubMed] [Google Scholar]
- 24.Shea S, Basch CE. A review of five major community-based cardiovascular disease prevention programs, II: intervention strategies, evaluation methods, and results. Am J Health Promot. 1990;4:279–287. [DOI] [PubMed] [Google Scholar]
- 25.Flay BR. Psychosocial approaches to smoking prevention: a review of findings. Health Psychol. 1985;4:449–488. [DOI] [PubMed] [Google Scholar]
- 26.Johnson CA. Prevention and control of drug abuse. In: Last JM, ed. Public Health and Preventive Medicine. 12th ed. Norwalk, Conn: Appleton-Century-Crofts; 1985:1075–1087.
- 27.Botvin G. Substance prevention research: recent developments and future directions. J Sch Health. 1986;56:369–374. [DOI] [PubMed] [Google Scholar]
- 28.Flay BR. Mass media linkages with school-based programs for drug abuse prevention. J Sch Health. 1986;56:402–406. [DOI] [PubMed] [Google Scholar]
- 29.Pentz MA, Dwyer JH, Mackinnon DP, et al. A multicommunity trial for primary prevention of adolescent drug abuse. JAMA. 1989;261:3259–3266. [PubMed] [Google Scholar]
- 30.Perry CL. Community-wide health promotion and drug abuse prevention. J Sch Health. 1986;56:359–363. [DOI] [PubMed] [Google Scholar]
- 31.Hyndman B, et al. Preventing substance abuse through multicomponent community action research projects: lessons from past experiences and challenges for future initiatives. Contemp Drug Probl. 1992;19:133–164. [Google Scholar]
- 32.Kane P, Choi CY. China’s one child family policy. BMJ. 1999;319:992–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li VC, Clayton S. Family planning information, education and communication: current activities in People’s Republic of China. Int Q Community Health Educ. 1991/92;12(2):107–117. [DOI] [PubMed]
- 34.Wang VL. Application of social science theories on health education in family planning in the People’s Republic of China. Am J Public Health. 1976;66:440–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang R, Ni S. China and United Nations Drug Prohibition Department signed an agreement on international cooperation in prohibiting drug abuse [in Chinese]. People’s Daily. May 23, 1995:4.
- 36.Ma MZ. Drug Use in China [in Chinese]. Beijing, China: Beijing Press; 1993.
- 37.Rothman J. Three models of community organization practice, their mixing and phasing. In: Cox FM, Erlich JL, Rothman J, Tropman JE, eds. Strategies in Community Organization. 3rd ed. Itasca, Ill: F. F. Peacock Publishers Inc; 1979:86–102.
- 38.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977.
- 39.Gossop M, Grant M. Preventing and Controlling Drug Abuse. Geneva, Switzerland: World Health Organization; 1990.
- 40.Kotler P, Zaltman G. Social marketing: an approach to planned social change. J Marketing. July 1971;35:3–12. [PubMed] [Google Scholar]
- 41.Kotler P, ed. Marketing for Nonprofit Organizations. 2nd ed. Englewood Cliffs, NJ: Prentice Hall; 1975.
- 42.Barrett ME, de Palo MP. Community-based intervention to reduce demand for drugs in northern Thai tribal villages. Subst Use Misuse. 1999;34:1837–1879. [DOI] [PubMed] [Google Scholar]