Abstract
Objectives. We compared chiropractic practice volume in areas of high versus areas of low or no shortages of primary care providers.
Methods. Using data from a cross-sectional survey of US chiropractors and data from the Bureau of Health Professions’ Area Resource File, we conducted multiple linear and logistic regression modeling of the effects of rural or Health Professional Shortage Area location on chiropractic practice volume and wait times.
Results. Chiropractors in rural and high-shortage areas have busier, higher-volume practices than do those in other locales (after control for other chiropractors in the same market service area).
Conclusions. Chiropractic providers render a substantial amount of care to underserved and rural populations. Health policy planners should consider the full complement of providers available to improve access to care. (Am J Public Health. 2002;92:2001–2009)
Complementary and alternative medicine (CAM) use in the United States has grown markedly.1–3 Evidence suggests that lifetime CAM use increases with age across age cohorts and that half of all CAM patients continue to use CAM for many years.4 Such documented trends have raised awareness and interest in the CAM disciplines,5–7 thus driving further research and discussion about CAM patients’ use and utilization of medical or preventive services,1,8,9 the inclusion of CAM in private insurance and managed care,10–12 and the actual or potential roles of CAM practitioners as additional nonphysician primary care providers in the US health workforce.13–20
Chiropractic health care is among the largest and most high-profile of the established nonallopathic singular health care disciplines, and chiropractic users consistently represent the largest share in surveys of CAM users overall.2,9 A substantial body of rigorous scientific evidence supports the efficacy and effectiveness of spinal manipulation for various conditions.21–27 Additionally, the chiropractic profession has established structures and processes for further developing and disseminating that evidence base and for fostering effective, evidence-based education, training, and practice.28–33
Chiropractic education and clinical training in the 17 accredited chiropractic colleges in the United States combines discipline-specific chiropractic assessment and therapeutic procedures with standard medical diagnosis and procedures, excluding invasive or critical care procedures, pharmacology, and surgery.29,30 Hours of education and training required in chiropractic and medical school curricula are 4820 in the doctor of chiropractic (DC) program, compared with 4670 in the doctor of medicine (MD) program (not counting postgraduate clinical residency hours of MDs). Curricular differences include a greater emphasis on biomechanics, musculoskeletal function, and manual procedures for chiropractic students and a substantially longer mentored clinical experience for medical students in both undergraduate and postgraduate training.34,35
Ongoing interest and efforts relative to practice, research, and policy have been directed toward studying the characteristics of chiropractic patients and practice, the relationship between chiropractic and other health care providers, and the distribution, use, and utilization of chiropractic services. Patient characteristics associated with chiropractic use may include poorer health status,36 older age, reportage of a greater number of chronic health problems, more frequent physician visits, and greater difficulty in obtaining an appointment with a physician.37 Chiropractic patients in rural areas may be more likely than those in more urban locales to present with nonmusculoskeletal complaints.38,39 A high level of satisfaction with chiropractic care and a strong chiropractor–patient relationship40–44 may especially characterize chiropractic practices in rural, medically underserved areas.45
Chiropractic patients may typically use a DC as a first point of contact with the health care system,46 particularly in rural areas.47 Most chiropractic patients self-report that they do not use other providers’ services while under chiropractic care 46; however, more than 97% of DCs report that they refer their patients for medical care as needed.48–51 Slightly more than half of surveyed family physicians report referring patients to DCs.43,49 Bidirectional referral relationships between MDs and DCs may be more active in rural areas,38 among younger or newer practitioners,48,52 and among MDs who feel informed about chiropractic care.52 The majority of surveyed chiropractors convey a self-perception of practicing in a primary care capacity53; they also report that they provide primary care services such as health history assessments and physical examinations of their patients on a routine basis.51,53 An interdisciplinary expert focus group (DCs, MDs, physician assistants, and nurse practitioners) concurred that DCs are able to make diagnoses in more than 90%—and therapeutic contributions in more than half—of primary care activities, although more DCs than other participants perceived a need for physician involvement in primary care activities.54 The position of the chiropractic profession is that prevention and health promotion are integral to chiropractic care,28 and most DCs agree.53,55–57 However, the actual provision of such services varies somewhat among chiropractic providers53,55 and may be related to where their practices are located.45
High DC-to- population ratios are associated with smaller towns.58 Half of surveyed DCs practice in communities with populations under 50 000,53,55 and most rural-practicing DCs also originally come from rural areas.38 Findings on the relationship between locale and chiropractic utilization have been mixed. Hawk59 and Cote et al.60 reported higher rural and higher urban use of chiropractic care, respectively, and Shekelle and Brook61 reported both. Whereas an early ecological-level analysis of 4 regions ranked chiropractic utilization rates in the same order as chiropractors per population,62 a more recent study comparing regions that varied by geography and DC-to-population ratios found no relation between DC density and visit rates, although patterns of treatment (amount of care provided per episode) did vary significantly across geographic sites.61 In a cohort study of chiropractic utilization in a medically underserved rural Iowa area, no relation was found between level of access to physician services (measured as growth in the physician workforce) and the use of chiropractic services.36
Given such a mix of intriguing and sometimes conflicting findings, further work is warranted to clarify our understanding of actual and potential roles of chiropractors in meeting the health care needs of underserved or rural populations. Such studies should include comprehensive and policy-relevant definitions of “underserved,” such as the Health Professional Shortage Area (HPSA) designation. Studies should also include and control for a number of other potential predictors of chiropractic service use (e.g., rurality or DC and population densities) to sort out their differential effects.
It is also important to embed study of chiropractic use within relevant conceptual frameworks and to apply the appropriate methodologies of health services research. For instance, as a dimension of access to health care, wait times (both before and during scheduled and walk-in visits) may be used to measure time barriers or organizational barriers to patients.63 For both conceptual and methodological reasons, consideration of provider-specific market service areas as a useful unit or level of analysis is fundamental, whether as a means of studying issues relative to workforce capacity or access or as the context for studies of provider competition or collaboration.64–70
In an earlier study, 71 we surveyed Missouri chiropractors, comparing chiropractic practices serving high- or whole-shortage HPSAs with those serving low-, part- or nonshortage areas. Chiropractic practices serving high-shortage areas had significantly higher practice volumes (numbers of weekly visits and of annual new patients), even after control for DC density and rural location. Although rural location was a significant predictor of annual new patients, it was not significantly related to number of weekly visits.
As a follow-up to an earlier preliminary single-state survey, our study surveyed a national sample of active, licensed DCs. Specifically, that survey tested (1) the hypothesized relationship between chiropractic practice volume and location in HPSAs or rural areas, and controlled for various characteristics of DCs or their practice environments that might also affect practice volumes, and (2) whether there were differences in wait times between chiropractic practices in high-shortage versus low- or no-shortage HPSAs, or in rural versus nonrural locations.
METHODS
In this descriptive cross-sectional study, we used a 1997 mail survey of a random sample of US chiropractors stratified by zip code region. The sample was drawn from a list of approximately 30 000 DCs compiled from US telephone directory pages (white and yellow) and modified to remove duplicate names and practices. This sampling frame is comparable to the 32 000 estimated actively practicing DCs in the United States (of 46 196 total licensed chiropractors) reported in the National Board of Chiropractic Examiners’ 1993 survey.50 A computer-generated random sample of 2000 DCs was stratified by the 10 zip code regions in the United States; 104 surveys were returned as undeliverable (effective sampled n = 1896).
To maximize the response rate, the survey was administered using hand-addressed envelopes; a personalized, hand-signed cover letter emphasizing the importance of the survey and assuring respondents of anonymity; a postage-paid return envelope; and a user-friendly questionnaire that had been pilot-tested for ease of response and clarity. Follow-up postcard reminders were mailed out 2 weeks after the initial mailing. Response to an initial 3-page survey was 30% (563/1896). A follow-up survey to nonrespondents, shortened to 1 page to decrease respondent burden, yielded an additional 247 responses, for a final survey response rate of 43%. Fifty randomly selected nonrespondents were contacted by telephone. Most nonrespondents stated that they didn’t feel that the survey was important or that they didn’t have the time to complete the survey.
The survey collected baseline demographic data on sex, practice status (full- vs part-time), chiropractic college, and year of graduation. DCs were asked to list up to 5 counties making up their individual market service areas (defined as the entire area from which they drew patients) and were queried on the following items to characterize their individual practices: weekly hours in practice, number of weekly patient office visits, whether nonscheduled patients (i.e., “walk-ins”) were accepted for a same-day initial visit, average wait time for scheduled and nonscheduled patients (in minutes), number of new patients accepted in prior calendar year, and whether new patients were scheduled for an initial visit within 1 day.
Data from each survey were key-entered using double-entry verification and automatic validation schemes and then imported into a Microsoft Access database. The survey data were linked to the Area Resource File (ARF) system of the Health Resources and Services Administration’s Bureau of Health Professions for measures of practice environment (for example, whether any county in the DC’s market service area was designated as a whole-shortage HPSA) average rural/urban continuum code (US Department of Agriculture) across all of the DC’s market counties, and population density. The database was later supplemented with aggregate information on number of DCs per county, obtained from the most extensive list then available (the proprietary mailing list of the newspaper Dynamic Chiropractic, which had been reconciled to a list from the Federation of Chiropractic Licensing Boards).
Analyses of association were conducted using multivariable regression modeling. All models included the same 2 sets of independent variables measuring attributes of individual DCs and of their practice markets. Chiropractor attribute measures were full-time vs part-time practice, male vs female, and years active (computed from date of graduation). Practice market measures included presence of whole-shortage HPSA in market (yes, no), average rurality across market (continuum of 0–9), average population per DC ratio across market, and presence in the practice market of a chiropractic college (yes, no). Four of the 5 continuous dependent variables exhibited substantial skewness and kurtosis (principally due to a very small number of outliers to the right), and we therefore truncated these variables at the 99th percentile to effectively normalize their distributions before we ran separate linear regressions on each. The dependent variables included weekly practice hours, weekly patient visits (truncated with all values > 350 visits subsumed into 1 final value of ≥ 350), annual new patients (truncated at ≥ 800 patients), wait time for walk-in patients (truncated at ≥ 75 minutes), and wait time for scheduled patients (truncated at ≥ 45 minutes). The 2 dichotomous dependent variables—whether walk-in patients were accepted (yes, no) and the wait of new patients for an initial visit (same/next day vs ≥ 2 days)—were modeled through logistic regression. All statistical calculations were performed with SPSS for Windows, Release 7.0 (SPSS Inc, Chicago, Ill).
RESULTS
The survey response rate was 43% (815/1896). The demographics of our respondents were similar to those reported in surveys of US chiropractors from the National Board of Chiropractic Examiners (Table 1 ▶).50,51
TABLE 1.
—Characteristics of Survey Respondents, by Survey
| US DCs,a 1991 | US DCs,b 1998 | Smith and Carber 1997c | |
| Full-time vs part-time, % | 82 | 88 | 93 |
| Male, % | 87 | 81 | 86 |
| Years active, %d | 16.1, 9.0e | ||
| 5–15 | 57 | 47 | |
| ≥ 16 | 25 | 35 | |
| Practice hours/week, % | 35.3, 9.2e | ||
| ≤ 29 | 11 | 17 | |
| 30–39 | 46 | 46 | |
| 40–49 | 33 | 29 | |
| ≥ 50 | 10 | 8 | |
| Chiropractic college attended, % | |||
| Palmer (Davenport, Iowa) | 28 | 22 | 22 |
| National (Chicago, Ill) | 12 | 9 | 10 |
| Life (Marietta, Ga) | 9 | 12 | 10 |
| Logan (St. Louis, Mo) | 8 | 8 | 8 |
| New York CC | 7 | 7 | 10 |
| Los Angeles CC | 7 | 8 | 6 |
| Remaining US colleges (each ≤ 5%) | 27 | 32 | 30 |
| Other non-US college, or US college now closed | 2 | 2 | 4 |
| No. of patient visits/week | 112.2, 69.3e | ||
| No. of annual new patients | 187.1, 151.8e | ||
| New patient wait for initial visit, % scheduled within 1 day | 90 | ||
| Scheduled patient wait time, minutes | 8.2, 6.4e | ||
| Accept walk-in patients, % yes | 91 | ||
| Walk-in patient wait time, minutes | 20.6, 13.1e | ||
Note. DC = Doctor of Chiropractic; CC = chiropractic college. National Board of Chiropractic Examiners (NBCE) data (both years) reflect only DCs practicing full-time.
aData from NBCE.50
bData from NBCE.51
cData collected by Smith and Carber in 1997 and published in this article.
dFor active years, NBCE queried for “Total years in active practice,” whereas Smith and Carber queried for “Year of graduation from chiropractic college.”
eMean and standard deviation.
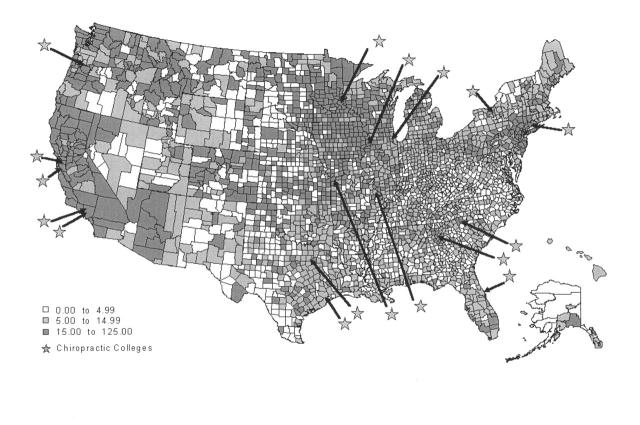
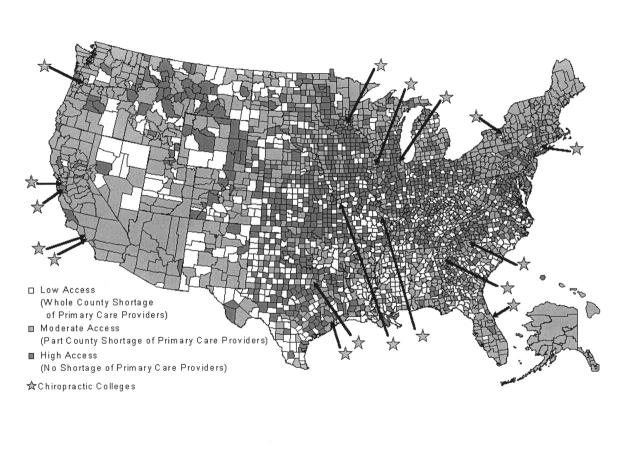
Eighty-eight percent (715/815) of the respondent chiropractors reported providing care to patients from HPSA counties designated as having a whole or partial shortage of health professionals. Of those, 101 DCs served patients from whole-shortage counties. Most DCs (77%) reported drawing their patient base from multiple counties, with 60% reporting patients from a market service area encompassing 3 or more counties. For added perspective, Figures 1 and 2 ▶ ▶ present national distributions of chiropractors, chiropractic colleges, and HPSAs.72–75
FIGURE 1.
—US chiropractors per 100 000 population, by county: 1998.
Note. Distribution has not been adjusted for chiropractic college faculty licenses.
Source: Proprietary mailing list, unpublished; Dynamic Chiropractic [newspaper]; Huntington Beach, Calif; 1998. Courtesy of Palmer Center for Chiropractic Research, Palmer College of Chiropractic, 2002.
FIGURE 2.
—Access to primary medical care providers in the United States.
Source. Area Resource File. Baltimore, MD: Health Resources Services Administration, Bureau of Health Professions; 1996. Courtesy of Palmer Center for Chiropractic Research, Palmer College of Chiropractic, 2002.
Multivariate linear and logistic regression results (Table 2 ▶) indicated that HPSA location was positively related to chiropractic practice volume (measured in visits or patients), even after control for rurality or the density of other chiropractic providers in the practice market. The combined effects of HPSA and rural location are significant and substantial. With each incremental increase of the DC’s rural location index adding another 9 new patients annually to the DC’s patient base, DCs located in extremely rural areas (index = 9) may see an average of 81 more new patients annually (9 × 9) compared with DCs in large metropolitan areas (index = 0). After we factored in the added effect of practice in a high-shortage HPSA location, DCs in high-shortage rural HPSAs may see 127 more new patients annually (81 + 46) than their colleagues in nonshortage urban locales. Post hoc testing for multicollinearity between the independent variables yielded negative results (maximum variance inflation factor = 1.6).
TABLE 2.
—Individual and Market-Level Characteristics Related to Chiropractic Practice Volume and Wait Times: Survey of Doctors of Chiropractic, 1997
| Coefficient (95% CI) | OR (95% CI) | ||||||
| Hours per Weeka(n = 707) | Visits per Weeka(n = 681) | Annual New Patientsa(n = 722) | Walk-In Wait, Minutesa(n = 662)c | Scheduled Patient Wait, Minutesa(n = 733) | Accept Walk-Ins: Yes (0), No (1)b(n = 730) | New Patient Wait for Initial Visit: Same/Next Day (0); ≥2 Days (1)b(n = 732) | |
| Individual DC predictors | |||||||
| Full-time (0), part-time (1) | –16.6 (–18.9, –14.3)*** | –61.6 (–81.7, –41.6)*** | –90.8 (–133.3, –48.2)*** | 0.2 (–4.0, 4.3) | –2.0 (–3.9, –0.03)** | 0.8 (0.3, 2.2) | 1.6 (0.7, 3.5) |
| Male (0), female (1) | –2.8 (–4.5, –1.0)*** | –18.4 (–33.3, –3.5)*** | –32.7 (–64.2, –1.3)** | 4.4 (1.4, 7.5)*** | –0.2 (–1.6, 1.2) | 1.9 (0.9, 3.9)* | 2.6 (1.4, 5.1)*** |
| Years active | –0.07 (–0.13, 0.001)** | 0.3 (–0.3, 0.9) | –0.4 (–1.6, 0.9) | 0.2 (0.06, 0.3)*** | 0.1 (–0.003, 0.11)* | 1.1 (1.0, 1.1)*** | 1.04 (1.01, 1.07)*** |
| Market-level DC predictors | |||||||
| Location within HPSA: no (0), yes (1) | 1.9 (–0.14, 4.0)* | 27.3 (9.8, 44.8)*** | 46.3 (9.3, 83.2)*** | –0.3 (–3.9, 3.2) | 0.9 (–0.8, 2.6) | 0.5 (0.2, 1.2)* | 0.6 (0.2, 1.4) |
| Rurality index: metropolitan (0) to rural (9) | –0.05 (–0.37, 0.27) | –1.6 (–4.3, 1.2) | 9.4 (3.7, 15.1)*** | 0.7 (0.1, 1.2)** | –0.1 (–0.3, 0.2) | 1.2 (1.1, 1.4)*** | 1.1 (1.0, 1.3)* |
| Population per DC | –0.0003 (–0.001,0.000)** | –0.00003 (–0.003, 0.003) | –0.002 (–0.007, 0.004) | –0.0002 (–0.001, 0.000) | 0.0002 (0.000, 0.000) | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) |
| Presence in practice market of a chiropractic college: no (0), yes (1) | 0.4 (–1.3, 2.0) | –14.9 (–29.1, –0.58)** | –14.6 (–44.0, 14.8) | –2.0 (–4.8, 0.9) | 0.2 (–1.2, 1.5) | 1.9 (0.9, 3.8)* | 1.6 (0.8, 3.2) |
| Constant | 58.4 (55.1, 61.7)*** | 197 (168.4, 225.6)*** | 307.8 (248.1, 367.5)*** | 12.5 (6.7, 18.3)*** | 9.2 (6.4, 11.9)*** | β(SE) = –3.6 (0.4)*** | β(SE) = –3.6 (0.4)*** |
Note. DC = Doctor of Chiropractic; CI = confidence interval; OR = odds ratio; HPSA = Health Professional Shortage Area; SE = standard error.
aLinear regression model.
bLogistic regression model.
cIncludes only DCs who reported accepting walk-ins.
*P < .10; **P < .05; ***P < .01.
Wait times do not appear to vary by HPSA location, although practices located in less-populated areas are less inclined to accept walk-in patients, have longer wait times for walk-ins when accepted, and also have generally longer waits for new patients seeking an initial visit. Interestingly, the populationadjusted density of other chiropractors located in a DC’s practice market does not significantly affect either practice volume or wait times.
A previous survey of Missouri-licensed DCs71 suggested that rural location was associated with a greater number of new patients annually but not with a concomitant increase in weekly visits, a finding similarly revealed in this study. Such a finding might be explained by a greater likelihood of newly graduated DCs with growing practices to be located in rural areas (i.e., newer practices would have relatively more new patients). However, a bivariate analysis of year of graduation by rurality on this nationwide sample did not support that hypothesis (Pearson correlation: P < .182).
DISCUSSION
Chiropractic providers render a substantial amount of care to underserved populations such as those in designated health workforce shortage areas. Our study findings indicate that chiropractic practices in high-shortage and rural areas have significantly higher volumes of annual new patients. Possible explanations for this finding are that populations in HPSAs or more rural areas have a higher prevalence of “typical chiropractic conditions” (e.g., back pain or musculoskeletal disorders) or that they are more likely to seek care for such conditions, which could at least partly account for a higher practice volume in those areas. Analyses of data from the National Health Interview Survey did not show differences in the prevalence of back problems by population density after control for the effects of potential confounders, although differences by geographic region—consistent with findings from an earlier study76,77—were seen. There does not appear to be a relationship between care-seeking for back pain and geographic region or population density.78
The limitations of our study must also be considered. Self-reported individual recollections should always be interpreted cautiously, and the limited study design did not allow us to examine potential bias from possible misclassification. The low response rate to our survey of chiropractors is also potentially problematic. If nonrespondents disproportionately represented extremely busy DCs (as their excuses for nonresponse might suggest), then their nonparticipation may also have selectively biased our sample by overemphasizing less busy practitioners. If busier DCs are also more likely to be located in rural or underserved areas, those levels and types of practice/market characteristics may also have been disproportionately underrepresented in our sample and analysis. Future studies along this line may be more informative by directing a more concerted effort toward following up and gathering pertinent information from nonrespondents when possible.
More work needs to be directed toward better clarifying and modeling the relationships between the characteristics of chiropractic market service areas (including health care system factors) and of chiropractic practices and chiropractic patients. Given our study findings of significant differences in practice volume and wait times related to practice location, it appears that chiropractic health care providers may already be serving in some function to fill the gap in health care system capacity in medically underserved or rural areas, or perhaps otherwise substituting for other types of health care services in response to specific patient demand in certain markets. Chiropractic patients in rural or underserved areas may have a greater propensity to also use DCs as a first point of contact47 or for care of nonmusculoskeletal conditions,38,39 and DCs in rural or underserved areas may experience relatively more active bidirectional referral relationships38 or be more likely to provide preventive services.45 If so, the nature of the “cultural or social authority”79 exercised or experienced by chiropractors in the context of their market-specific health care systems and the cultural/social congruence between DCs and their respective patient or market populations may also differ somewhat by locale.
We speculate that chiropractic practices and practitioners may evolve differently in response to the needs and demands of the patient populations specific to their market service areas. The chiropractic profession may actually encompass a heterogeneous set of practitioners with varied disciplinary foci. DCs with patients who have ready access to primary medical care or who are in markets with a medically dominated orientation to health care organization and delivery may focus their emphasis as musculoskeletal specialists. In areas or markets where populations have curtailed use of medical services, either by necessity due to less access or by choice/preference, chiropractors may respond by adopting a broader, more accommodating generalist orientation to chiropractic practice. Chiropractors’ undergraduate and postgraduate preparation to fill such divergent roles80 should be sufficiently comprehensive and appropriate, perhaps necessitating a reexamination of the nature and extent of the current clinical education of DCs. Also, the historical isolation of chiropractic clinical training from medical training and the dearth of opportunities for chiropractic training and practice in varied multidisciplinary clinical settings should be addressed. Our understanding of the actual and potential roles of chiropractic health care in the US health care delivery system is limited at best and warrants additional attention.
The shortage of MDs in rural and underserved areas remains a long-standing and serious problem.81–83 The deployment of non-MD practitioners in varied arrangements and settings offers promise as a viable and sustainable solution to improving primary care access.84–88 As a key nonmedical discipline that has achieved pronounced levels of professionalization28–33 and health system integration and inclusion,6,11,15,89–93 chiropractic health care may serve as a useful example of how health services research and policies on access to care, primary care workforce capacity, and the unmet needs of identified underserved populations13,81–88,94–104 may intersect with research into and policies of evidence-based CAM health care delivery. The extent to which DCs might contribute to addressing this nation’s health workforce needs, particularly those of underserved populations, warrants further investigation. Specifically, more study is needed to document and examine the distribution of chiropractic providers relative to underserved areas, the scope and scale of services provided to chiropractic patients, and the extent to which the population and other health care providers do, or could, avail themselves of professional chiropractic services.
Chiropractic health care providers in the United States are somewhat unevenly distributed, as shown in Figure 1 ▶.72–75 The distribution of college campus—based chiropractic teaching clinics is mapped in Figures 1 and 2 ▶ ▶, although this distribution does not fully reflect all satellite chiropractic teaching sites. Some clustering of chiropractors seems apparent relative to chiropractic college proximity; however, as noted in the legend to Figure 1 ▶, the reported distributions also include chiropractic teaching faculty. We are conducting a study that uses data obtained directly from the chiropractic state licensing boards and chiropractic colleges to map chiropractic provider distribution by county, for future inclusion in the ARF system.105
A continuing relationship with a personal health care provider has the potential to improve patient and practitioner satisfaction, compliance with treatment regimens and schedules, patient disclosure of other problems, and costs of care.106 Policies to improve access to care by promoting the primacy of the relationship between usual-source practitioners and their patients98–101 must include consideration of all practitioners who may already be serving, or have the potential to serve, as patients’ preferred sources of regular care. The DC currently serves a role as a first point of contact with the health care system or as the main source of care for many patients, particularly in rural or underserved areas.46,47 Given also a strong DC–patient relationship,40–45 the congruence of prevention and health promotion strategies with a wellness-oriented model of chiropractic practice,28,32,45,53,55–57 and continued strengthening of its interprofessional acceptance and integration, chiropractic may represent the most substantially overlooked and underutilized US health workforce resource. Chiropractic care essentially serves as an invisible piece of America’s health care safety net.
Health policy and planning would be better directed by considering information on the full complement of providers available to improve access to care. Health services research must include study of the complex dynamics of health services utilization and delivery across all providers and settings, particularly in underserved and rural areas. Most important, practicing DCs and the chiropractic profession must be cognizant of how the patients within their market service areas use chiropractic as a component of their overall health care, and they must assume the necessary responsibility for ensuring that underserved and vulnerable population groups receive appropriate and adequate care.
Acknowledgments
The authors thank the following PCCR staff: Dr Cheryl Hawk, Lori Byrd, and Dr Bob Jansen for help with survey administration and data collection; Lance Corber of the PCCR Office of Data Management for help with data management; and Dr Cyndy Long for assistance with data analysis.
Human Participant Protection No protocol approval was needed for this study.
M. Smith was responsible for study conception and design, data analysis and interpretation, and the writing of the article. L. Carber contributed to data management and analysis and the preparation and editing of the article.
Peer Reviewed
References
- 1.Paramore LC. Use of alternative therapies: estimates from the 1994 Robert Wood Johnson Foundation National Access to Care Survey. J Pain Symptom Manage. 1997;13:83–89. [DOI] [PubMed] [Google Scholar]
- 2.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280:1569–1575. [DOI] [PubMed] [Google Scholar]
- 3.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246–252. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Davis RB, Foster DF, et al. Long-term trends in the use of complementary and alternative medical therapies in the United States. Ann Intern Med. 2001;135:262–268. [DOI] [PubMed] [Google Scholar]
- 5.Wootton JC, Sparber A. Surveys of complementary and alternative medicine: part I. General trends and demographic groups. J Altern Complement Med. 2001;7:195–208. [DOI] [PubMed] [Google Scholar]
- 6.Faass N. Integrating Complementary Medicine Into Health Systems. Gaithersburg, Md: Aspen Publishers, Inc; 2001.
- 7.Cohen MH. Complementary and Alternative Medicine: Legal Boundaries and Regulatory Perspectives. Baltimore, Md: Johns Hopkins University Press; 1998.
- 8.Robinson AR, Crane LA, Davidson AJ, Steiner JF. Association between use of complementary/alternative medicine and health-related behaviors among health fair participants. Prev Med. 2002;34:51–57. [DOI] [PubMed] [Google Scholar]
- 9.Druss BG, Rosenheck RA. Association between use of unconventional therapies and conventional medical services. JAMA. 1999;282:651–656. [DOI] [PubMed] [Google Scholar]
- 10.Pelletier KR, Astin JA. Integration and reimbursement of complementary and alternative medicine by managed care and insurance providers: 2000 update and cohort analysis. Altern Ther Health Med. 2002;8:38–39, 42, 44, 46–48.. [PubMed] [Google Scholar]
- 11.Gordon NP, Sobel DS, Tarazona EZ. Use of and interest in alternative therapies among adult primary care clinicians and adult members in a large health maintenance organization. West J Med. 1998;169:153–161. [PMC free article] [PubMed] [Google Scholar]
- 12.Cleary-Guida MB, Okvat HA, Oz MC, Ting W. A regional survey of health insurance coverage for complementary and alternative medicine: current status and future ramifications. J Altern Complement Med. 2001;7:269–273. [DOI] [PubMed] [Google Scholar]
- 13.Weston JL. Annotated Bibliography of AHCPR Research on Nonphysician Primary Care Providers 1969–1989. Rockville, Md: US Dept of Health and Human Services, Agency for Health Care Policy and Research; 1990. AHCPR publication 90-13.
- 14.Berg JA, Amella E, Gagan MJ, McArthur DB. Integrative therapies in primary care practice. J Am Acad Nurse Pract. 1998;10:541–546. [DOI] [PubMed] [Google Scholar]
- 15.Borkan J. Referrals for alternative therapies. J Fam Pract. 1994;39:545–550. [PubMed] [Google Scholar]
- 16.Cooper RA. Health care workforce for the twenty-first century: the impact of nonphysician clinicians. Ann Rev Med. 2001;52:51–61. [DOI] [PubMed] [Google Scholar]
- 17.Cooper RA, Henderson T, Dietrich CL. Roles of nonphysician clinicians as autonomous providers of patient care. JAMA. 1998;280:795–802. [DOI] [PubMed] [Google Scholar]
- 18.Cooper RA, Laud P, Dietrich CL. Current and projected workforce of nonphysician clinicians. JAMA. 1998;280:788–794. [DOI] [PubMed] [Google Scholar]
- 19.Grumbach K, Coffman J. Physicians and nonphysician clinicians: complements or competitors? JAMA. 1998;280:825–826. [DOI] [PubMed] [Google Scholar]
- 20.Jacoby I, Meyer GS. Creating an effective physician workforce marketplace. JAMA. 1998;280:822–824. [DOI] [PubMed] [Google Scholar]
- 21.Meeker WC, Haldeman S. Chiropractic: a profession at the crossroads of mainstream and alternative medicine. Ann Intern Med. 2002;136:216–227. [DOI] [PubMed] [Google Scholar]
- 22.Aker PD, Gross AR, Goldsmith CH, Peloso P. Conservative management of mechanical neck pain: systematic overview and meta-analysis. BMJ. 1996;313:1291–1296. [PMC free article] [PubMed] [Google Scholar]
- 23.Anderson R, Meeker WC, Wirick BE, Mootz RD, Kirk DH, Adams A. A meta-analysis of clinical trials of spinal manipulation. J Manipulative Physiol Ther. 1992;15:181–194. [PubMed] [Google Scholar]
- 24.Assendelft WJ, Koes BW, Knipschild PG, Bouter LM. The relationship between methodological quality and conclusions in reviews of spinal manipulation. JAMA. 1995;274:1942–1948. [PubMed] [Google Scholar]
- 25.Hurwitz EL, Aker PD, Adams AH, Meeker WC, Shekelle PG. Manipulation and mobilization of the cervical spine. A systematic review of the literature. Spine. 1996;21:1746–1760. [DOI] [PubMed] [Google Scholar]
- 26.Koes BW, Assendelft WJ, van der Heijden GJ, Bouter LM. Spinal manipulation for low back pain. An updated systematic review of randomized clinical trials. Spine. 1996;21:2860–2871. [DOI] [PubMed] [Google Scholar]
- 27.Shekelle PG, Adams AH, Chassin MR, Hurwitz EL, Brook RH. Spinal manipulation for low-back pain. Ann Intern Med. 1992;117:590–598. [DOI] [PubMed] [Google Scholar]
- 28.Haldeman S, Chapman-Smith D, Petersen DM, eds. Guidelines for Chiropractic Quality Assurance and Practice Parameters: Proceedings of the Mercy Center Consensus Conference. Gaithersburg, Md: Aspen Publishers, Inc; 1993.
- 29.Lawrence DJ. Chiropractic medicine. In: Jonas WB, Levin JS, eds. Essentials of Complementary and Alternative Medicine. Philadelphia, Pa: Lippincott Williams & Wilkins; 1999:275–288.
- 30.Chapman-Smith D. An overview of the profession of chiropractic. In: Faass N, ed. Integrating Complementary Medicine Into Health Systems. Gaithersburg, Md: Aspen Publishers, Inc; 2001:157–163.
- 31.Council on Chiropractic Education. Available at: http://www.cce-usa.org. Accessed December 15, 2001.
- 32.Association of Chiropractic Colleges. Available at: http://chirocolleges.org. Accessed December 15, 2001.
- 33.Federation of Chiropractic Licensing Boards. Available at: http://www.fclb.org. Accessed December 15, 2001.
- 34.Coulter I, Adams A, Coggan P, Wilkes M, Gonyea M. A comparative study of chiropractic and medical education. Altern Ther Health Med. 1998;4:64–75. [PubMed] [Google Scholar]
- 35.Freedman KB, Bernstein J. The adequacy of medical school education in musculoskeletal medicine. J Bone Joint Surg Am. 1998;80:1421–1427. [DOI] [PubMed] [Google Scholar]
- 36.Yesalis CE 3rd, Wallace RB, Fisher WP, Tokheim R. Does chiropractic utilization substitute for less available medical services? Am J Public Health. 1980;70:415–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cleary PD. Chiropractic use: a test of several hypotheses. Am J Public Health. 1982;72:727–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barnett K, McLachlan C, Hulbert J, Kassak K. Working together in rural South Dakota: integrating medical and chiropractic primary care. J Manipulative Physiol Ther. 1997;20:577–582. [PubMed] [Google Scholar]
- 39.Hawk C, Long CR, Boulanger KT. Prevalence of nonmusculoskeletal complaints in chiropractic practice: report from a practice-based research program. J Manipulative Physiol Ther. 2001;24:157–169. [PubMed] [Google Scholar]
- 40.Carey TS, Garrett J, Jackman A, McLaughlin C, Fryer J, Smucker DR. The outcomes and costs of care for acute low back pain among patients seen by primary care practitioners, chiropractors, and orthopedic surgeons. The North Carolina Back Pain Project. N Engl J Med. 1995;333:913–917. [DOI] [PubMed] [Google Scholar]
- 41.Wardwell WI. The Connecticut survey of public attitudes toward chiropractic. J Manipulative Physiol Ther. 1989;12:167–173. [PubMed] [Google Scholar]
- 42.Shekelle PG, Markovich M, Louie R. Factors associated with choosing a chiropractor for episodes of back pain care. Med Care. 1995;33:842–850. [DOI] [PubMed] [Google Scholar]
- 43.Cherkin DC, MacCornack FA, Berg AO. Managing low back pain—a comparison of the beliefs and behaviors of family physicians and chiropractors. West J Med. 1988;149:475–480. [PMC free article] [PubMed] [Google Scholar]
- 44.Coulehan JL. Chiropractic and the clinical art. Soc Sci Med. 1985;21:383–390. [DOI] [PubMed] [Google Scholar]
- 45.Maust A. The Chiropractic Patient in Rural, Health Professional Shortage Areas of the United States: An Exploratory Analysis. Richmond, Va: Research Dimensions Incorporated; December 1994.
- 46.Sawyer CE, Ramlow J. Attitudes of chiropractic patients: a preliminary survey of patients receiving care in a chiropractic teaching clinic. J Manipulative Physiol Ther. 1984;7:157–163. [PubMed] [Google Scholar]
- 47.Callahan D, Cianciulli A. The Chiropractor as a Primary Health Care Provider in Rural, Health Professional Shortage Areas of the US. Arlington, Va: Foundation for Chiropractic Education and Research; April 1994.
- 48.Sawyer CE, Bergmann TF, Good DW. Attitudes and habits of chiropractors concerning referral to other health care providers. J Manipulative Physiol Ther. 1988;11:480–483. [PubMed] [Google Scholar]
- 49.Mainous AG 3rd, Gill JM, Zoller JS, Wolman MG. Fragmentation of patient care between chiropractors and family physicians. Arch Fam Med. 2000;9:446–450. [DOI] [PubMed] [Google Scholar]
- 50.Christensen MG, Delle Morgan DR. Job Analysis of Chiropractic: A Project Report, Survey Analysis, and Summary of the Practice of Chiropractic Within the United States. Greeley, Colo: National Board of Chiropractic Examiners; 1993.
- 51.Christensen MG, Kerkoff D, Kollasch MW. Job Analysis of Chiropractic: A Project Report, Survey Analysis, and Summary of the Practice of Chiropractic Within the United States. Greeley, Colo: National Board of Chiropractic Examiners; 2000.
- 52.Cherkin D, MacCornack FA, Berg AO. Family physicians’ views of chiropractors: hostile or hospitable? Am J Public Health. 1989;79:636–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hawk C, Dusio ME. A survey of 492 US chiropractors on primary care and prevention-related issues. J Manipulative Physiol Ther. 1995;18:57–64. [PubMed] [Google Scholar]
- 54.Gaumer GL, Walker A, Su S. Chiropractic and a new taxonomy of primary care activities. J Manipulative Physiol Ther. 2001;24:239–259. [DOI] [PubMed] [Google Scholar]
- 55.Hawk C, Dusio ME. Chiropractors’ attitudes toward training in prevention: results of a survey of 492 US chiropractors. J Manipulative Physiol Ther. 1995;18:135–140. [PubMed] [Google Scholar]
- 56.Rupert RL, Manello D, Sandefur R. Maintenance care: health promotion services administered to US chiropractic patients aged 65 and older, part II. J Manipulative Physiol Ther. 2000;23:10–19. [PubMed] [Google Scholar]
- 57.Rupert RL. A survey of practice patterns and the health promotion and prevention attitudes of US chiropractors. Maintenance care: part I. J Manipulative Physiol Ther. 2000;23:1–9. [DOI] [PubMed] [Google Scholar]
- 58.Gesler WM. The place of chiropractors in health care delivery: a case study of North Carolina. Soc Sci Med. 1988;26:785–792. [DOI] [PubMed] [Google Scholar]
- 59.Hawk C, Long CR. Factors affecting use of chiropractic services in seven Midwestern states of the United States. J Rural Health. 1999;15:233–239. [DOI] [PubMed] [Google Scholar]
- 60.Cote P, Cassidy JD, Carroll L. The treatment of neck and low back pain: who seeks care? who goes where? Med Care. 2001;39:956–967. [DOI] [PubMed] [Google Scholar]
- 61.Shekelle PG, Brook RH. A community-based study of the use of chiropractic services. Am J Public Health. 1991;81:439–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mugge RH. Persons Receiving Care From Selected Health Care Practitioners. United States, 1980. Washington, DC: National Center for Health Statistics, Public Health Service; 1984:1–19. National Medical Care Utilization and Expenditure Survey, Series B Descriptive Report No. 6. DHHS publication 84-20206. [PubMed]
- 63.Dutton D. Financial, organizational and professional factors affecting health care utilization. Soc Sci Med. 1986;23:721–735. [DOI] [PubMed] [Google Scholar]
- 64.Hassinger EW, Hu BL, Hastings DV, McNamara RL. Changes in number and location of health practitioners in a 20-county rural area of Missouri. Public Health Rep. 1975;90:313–318. [PMC free article] [PubMed] [Google Scholar]
- 65.Phibbs CS, Robinson JC. A variable-radius measure of local hospital market structure. Health Serv Res. 1993;28:313–324. [PMC free article] [PubMed] [Google Scholar]
- 66.Carpenter ES, Plessas DJ. Estimating hospital service areas using mortality statistics. Health Serv Res. 1985;20:19–26. [PMC free article] [PubMed] [Google Scholar]
- 67.Drosness DL, Lubin J. Planning can be based on patient travel. Mod Hosp. 1966;10:92–94. [PubMed] [Google Scholar]
- 68.Garnick DW, Luft HS, Robinson JC, Tetreault J. Appropriate measures of hospital market areas. Health Serv Res. 1987;22:69–89. [PMC free article] [PubMed] [Google Scholar]
- 69.Morrisey MA, Sloan FA, Valvona J. Defining geographic markets for hospital care. Law Contemp Probl. 1988;51:165–194. [PubMed] [Google Scholar]
- 70.Makuc DM, Haglund B, Ingram DD, Kleinman JC, Feldman JJ. Health service areas for the United States. Vital Health Stat 2. 1991;No. 112:1–102. [PubMed]
- 71.Smith M, Parry A. The practice of chiropractic in health professional shortage areas in Missouri. Journal of the Neuromusculoskeletal System. 1998;6:17–23. [Google Scholar]
- 72.Smith M, Carber L. Creating an accurate database of the chiropractic healthcare workforce for use in health services research. Conference Proceedings of the 2000 Association of Chiropractic Colleges Annual Conference (ACC 2000); March 2000; San Antonio, Tex.
- 73.Smith M, Carber L, Morschhauser S. Establishing a database of US chiropractic health manpower data: Furthering the development of research infrastructure. Conference Proceedings of the 1999 Association for Health Services Research 16th Annual Meeting (AHSR 1999); June 1999; Chicago, Ill.
- 74.Smith M, Wiese G, Phongphua C. Chiropractic educational institutions and practices within the context of health care systems and policies. Conference Proceedings of the 1999 World Federation of Chiropractic Biennial Congress (WFC 1999); May 1999; Auckland, New Zealand.
- 75.Smith M. Ongoing surveys of chiropractic practices in primary care shortage areas and Native American areas: report of findings and methodological issues. Conference Proceedings of the 2000 International Conference of Spinal Manipulation (ICSM 2000); September 2000; Minneapolis, Minn.
- 76.Hurwitz EL, Morgenstern H. Correlates of back problems and back-related disability in the United States. J Clin Epidemiol. 1997;50:669–681. [DOI] [PubMed] [Google Scholar]
- 77.Deyo RA, Tsui-Wu YJ. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine. 1987;12:264–268. [DOI] [PubMed] [Google Scholar]
- 78.Hurwitz EL, Morgenstern H. The effect of comorbidity on care seeking for back problems in the United States. Ann Epidemiol. 1999;9:262–270. [DOI] [PubMed] [Google Scholar]
- 79.Starr P. The Social Transformation of American Medicine. New York, NY: Basic Books, Inc; 1982.
- 80.Rosser WW. Approach to diagnosis by primary care clinicians and specialists: is there a difference? J Fam Pract. 1996;42:139–144. [PubMed] [Google Scholar]
- 81.Scott HD, Bell J, Geller S, Thomas M. Physicians helping the underserved: the Reach Out program. JAMA. 2000;283:99–104. [DOI] [PubMed] [Google Scholar]
- 82.Rabinowitz HK, Diamond JJ, Markham FW, Hazelwood CE. A program to increase the number of family physicians in rural and underserved areas: impact after 22 years. JAMA. 1999;281:255–260. [DOI] [PubMed] [Google Scholar]
- 83.Jones TF, Culpepper L, Shea C. Analysis of the cost of training residents in a community health center. Acad Med. 1995;70:523–531. [DOI] [PubMed] [Google Scholar]
- 84.Mundinger MO, Kane RL, Lenz ER, et al. Primary care outcomes in patients treated by nurse practitioners or physicians: a randomized trial. JAMA. 2000;283:59–68. [DOI] [PubMed] [Google Scholar]
- 85.Pathman DE, Taylor DH, Konrad TR, et al. State scholarship, loan forgiveness, and related programs: the unheralded safety net. JAMA. 2000;284:2084–2092. [DOI] [PubMed] [Google Scholar]
- 86.Forrest CB, Whelan EM. Primary care safety-net delivery sites in the United States: a comparison of community health centers, hospital outpatient departments, and physicians’ offices. JAMA. 2000;284:2077–2083. [DOI] [PubMed] [Google Scholar]
- 87.Shi L, Samuels ME, Konrad TR, Ricketts TC, Stoskopf CH, Richter DL. The determinants of utilization of nonphysician providers in rural community and migrant health centers. J Rural Health. 1993;9:27–39. [DOI] [PubMed] [Google Scholar]
- 88.Gupta GC, Konrad TR. Allied health education in rural health professional shortage areas of the United States. JAMA. 1992;268:1127–1130. [PubMed] [Google Scholar]
- 89.Baird R. Entering the front door: hospitals include chiropractic services. J Am Chiropractic Assoc. 1999;36:32–40. [Google Scholar]
- 90.Astin JA, Marie A, Pelletier KR, Hansen E, Haskell WL. A review of the incorporation of complementary and alternative medicine by mainstream physicians. Arch Intern Med. 1998;158:2303–2310. [DOI] [PubMed] [Google Scholar]
- 91.Jensen GA, Mootz RD, Shekelle PG, Cherkin DC Insurance coverage of chiropractic services. In: Cherkin DC, Mootz RD, eds. Chiropractic in the United States: Training, Practice, and Research. Rockville, Md: Agency for Health Care Policy and Research; December 1997:39–48. AHCPR publication 98-N002.
- 92.Mootz RD, Meeker WC. A survey of referral habits of American Back Society Symposium attendees. Chiropractic Technique. 1994;6:1–4. [Google Scholar]
- 93.Crock R, Jarjoura J, Polen A, Rutecki GW. Confronting the communication gap between conventional and alternative medicine: a survey of physicians’ attitudes. Altern Ther Health Med. 1999;5:61–66. [PubMed] [Google Scholar]
- 94.Andersen R, Aday LA. Access to medical care in the US: realized and potential. Med Care. 1978;16:533–546. [DOI] [PubMed] [Google Scholar]
- 95.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 96.Freeman HE, Blendon RJ, Aiken LH, Sudman S, Mullinix CF, Corey CR. Americans report on their access to health care. Health Aff (Millwood). 1987;6:6–8. [DOI] [PubMed] [Google Scholar]
- 97.Povar GJ. Primary care: questions raised by a definition. J Fam Pract. 1996;42:124–128. [PubMed] [Google Scholar]
- 98.Lambrew JM, DeFriese GH, Carey TS, Ricketts TC, Biddle AK. The effects of having a regular doctor on access to primary care. Med Care. 1996;34:138–151. [DOI] [PubMed] [Google Scholar]
- 99.Fiscella K. Is lower income associated with greater biopsychosocial morbidity? Implications for physicians working with underserved patients. J Fam Pract. 1999;48:372–377. [PubMed] [Google Scholar]
- 100.Buseman S, Amundson LH. Rural health care networks in South Dakota. S D J Med. 1993;46:361–363. [PubMed] [Google Scholar]
- 101.Bartman BA, Clancy CM, Moy E, Langenberg P. Cost differences among women’s primary care physicians [see comments]. Health Aff (Millwood). 1996;15:177–182. [DOI] [PubMed] [Google Scholar]
- 102.Spiegel JS, Rubenstein LV, Scott B, Brook RH. Who is the primary physician? N Engl J Med. 1983;308:1208–1212. [DOI] [PubMed] [Google Scholar]
- 103.Kohrs FP, Mainous AG 3rd. The relationship of health professional shortage areas to health status. Implications for health manpower policy. Arch Fam Med. 1995;4:681–685. [DOI] [PubMed] [Google Scholar]
- 104.Moscovice I, Wellever A, Christianson J, Casey M, Yawn B, Hartley D. Understanding integrated rural health networks. Milbank Q. 1997;75:563–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Smith M. Palmer Center for Chiropractic Research. Assessment of the current supply and distribution of the chiropractic workforce [active contract under HRSA/BHP National Center for Health Workforce Information and Analysis]. Government contract order no. 01–0556(P); 2002.
- 106.Dietrich AJ, Marton KI. Does continuous care from a physician make a difference? J Fam Pract. 1982;15:929–937. [PubMed] [Google Scholar]