More than 110 000 (16%) of the 696 000 US military personnel who served in the 1991 Persian Gulf War have been granted service-connected disability compensation.1 This is 2 to 3 times the rate that followed World War II (8.6%), the Korean Conflict (5%), or the Vietnam War (9.6%).1 Although many veterans report serious impairments in daily functioning, no research, to our knowledge, has assessed the health impact of Gulf War syndrome as measured by a systematic case definition.
In 1997, Haley et al. described a case definition of Gulf War syndrome composed of 3 primary symptom complexes (syndromes) beginning during or shortly after the war.2–4 This case definition, identified by a factor analysis of symptoms in 249 members of a battalion that served in the war, was found to be strongly associated (relative risks of 4 to 8) with self-reported wartime exposures to low-level chemical nerve agents and other cholinesterase-inhibiting chemicals,4 genetic susceptibility to chemical nerve agents and other organophosphates,5,6 abnormal audiovestibular tests indicating brainstem dysfunction,3,7 evidence of basal ganglia and brain stem neuronal loss as measured by magnetic resonance spectroscopy,8,9 and abnormal brain dopamine production.10 Results were recently replicated in an independent sample of Gulf War veterans.11
In 1998, we conducted a nested case–control study at the University of Texas Southwestern Medical Center involving individuals from a naval reserve battalion; 22 subjects with the highest scores on one of the 3 Haley syndrome factor scales were selected as case patients.2,3 This criterion allowed selection of subjects with symptoms most typical of the case definition irrespective of symptom severity (not measured) and total number of symptoms, and thus there was no bias for or against severity of illness. Sixteen healthy veterans matched with case patients in regard to age, sex, and education level were selected from the same battalion to serve as controls.3
We administered the Medical Outcomes Study 36-Item Short Form (MOS SF-36) self-report questionnaire, a validated, widely accepted measure of general health, functional status, and well-being, to assess the functional status and well-being of the case patients and controls.12 Because of the existence of population-based, noninstitutionalized norms, this questionnaire serves as the “gold standard” for comparisons among illnesses. Hundreds of published studies have applied the instrument in such comparisons.12
We found that the level of impairment of ill Gulf War veterans meeting the Haley case definition was generally far worse than that of patients with common illnesses known to have a substantial negative impact, including congestive heart failure, type 2 diabetes, recent acute myocardial infarction, chronic obstructive pulmonary disease, and clinical depression (Figure 1 ▶).12 Moreover, a repeated measures analysis of variance (F1,20 = 18, P < .001) showed that the impact of Haley's “confusion–ataxia” syndrome was substantially worse than that of his “impaired cognition” and “central pain” syndromes, confirming earlier published observations.2–5,7,8,10 In other settings, low MOS SF-36 scores such as those revealed in this study have been shown to be highly predictive of inability to work at a paying job.12
FIGURE 1.
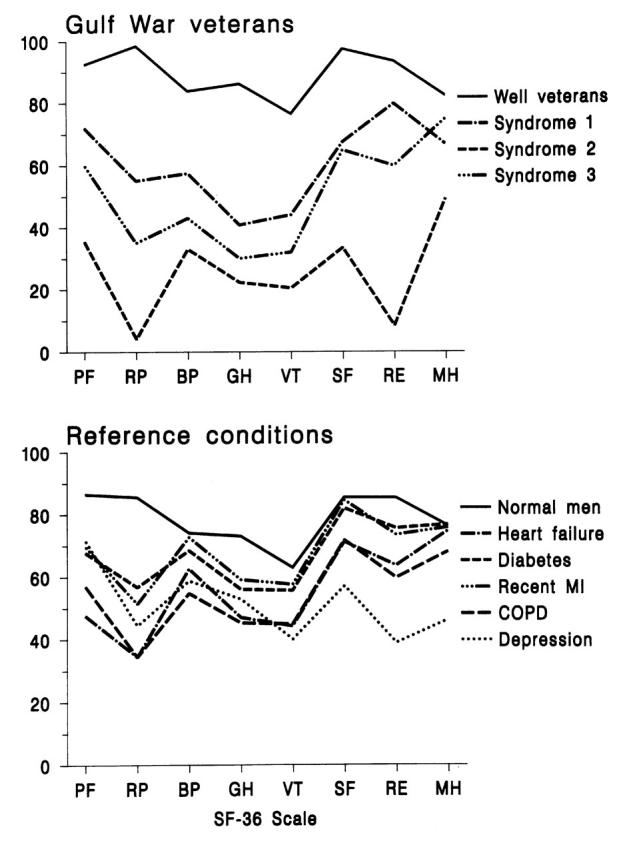
—Medical Outcomes Study 36-Item Short Form (MOS SF-36) scores among Gulf War veteran case patients and controls (top) and MOS SF-36 scores for 6 reference medical conditions (bottom).
A previous survey suggested that MOS SF-36 scores were only slightly lower in samples of Gulf War veterans than in nondeployed military personnel residing in Iowa, giving rise to the view that Gulf War–related illness has a small impact on functional status and well-being.13 However, the Iowa study reported the scores of ill Gulf War veterans combined with those of the far larger veteran population, thus obscuring the true disability level of the former group. By separating ill Gulf War veterans by means of a case definition, our study demonstrated severely diminished functional status and quality of life among those affected, commensurate with our clinical observations. This finding, coupled with previous research,1–10 suggests that many veterans are seriously impaired by brain illnesses or injuries sustained in the Gulf War.
Acknowledgments
This study was supported by the US Army Medical Research and Materiel Command under cooperative agreement DAMD17-97-2-7025; by US Public Health Service grant M01-RR00633; and by a grant from the Perot Foundation, Dallas, Tex.
The study protocol was approved by the institutional review board of the University of Texas Southwestern Medical Center, and all subjects gave written informed consent before participating.
R. W. Haley developed the epidemiologic study design, selected the subjects, and managed the overall data collection. A. M. Maddrey and H. K. Gershenfeld selected the functional status evaluation measure. A. M. Maddrey supervised the collection of data and calculation of the indices of functional status. R. W. Haley analyzed the data and wrote the first draft of the paper. H. K. Gershenfeld and A. M. Maddrey participated in analyzing and interpreting the data and in revising the paper.
Peer Reviewed
References
- 1.Statement of Joseph Thompson, undersecretary for benefits, Department of Veterans Affairs, before the House Committee on Veterans' Affairs, Subcommittee on Benefits, October 26, 1999. Available at: http://www.veterans.house.gov/hearings/schedule106/oct99/10-26-99/dva.htm. Accessed November 17, 2001.
- 2.Haley RW, Kurt TM, Hom J. Is there a Gulf War syndrome? Searching for syndromes by factor analysis of symptoms. JAMA.1997;277:215–222. [PubMed] [Google Scholar]
- 3.Haley RW, Hom J, Roland PS, et al. Evaluation of neurologic function in Gulf War veterans: a blinded case–control study. JAMA. 1997;277:223–230. [PubMed] [Google Scholar]
- 4.Haley RW, Kurt TL. Self-reported exposure to neurotoxic chemical combinations in the Gulf War: a cross-sectional epidemiologic study. JAMA. 1997;277:231–237. [PubMed] [Google Scholar]
- 5.Haley RW, Billecke S, La Du BN. Association of low PON1 type Q (type A) arylesterase activity with neurologic symptom complexes in Gulf War veterans. Toxicol Appl Pharmacol. 1999;157:227–233. [DOI] [PubMed] [Google Scholar]
- 6.Mackness B, Durrington PN, Mackness MI. Low paraoxonase in Persian Gulf War veterans self-reporting Gulf War syndrome. Biochem Biophys Res Commun. 2000;276:729–732. [DOI] [PubMed] [Google Scholar]
- 7.Roland PS, Haley RW, Yellin W, Owens K. Vestibular dysfunction in Gulf War syndrome. Otolaryngol Head Neck Surg. 2000;122:319–329. [DOI] [PubMed] [Google Scholar]
- 8.Haley RW, Marshall WW, McDonald GG, Daugherty M, Petty F, Fleckenstein JL. Brain abnormalities in Gulf War syndrome: evaluation by 1H magnetic resonance spectroscopy. Radiology.2000;215:807–817. [DOI] [PubMed] [Google Scholar]
- 9.Meyerhoff DJ, Lindgren J, Hardin D, Griffis JM, Weiner MW. Metabolic abnormalities in the brain of subjects with Gulf War illness. Proc Intl Soc Mag Reson Med. 2001;994.
- 10.Haley RW, Fleckenstein JL, Marshall WW, McDonald GG, Kramer GL, Petty F. Effect of basal ganglia injury on central dopamine activity in Gulf War syndrome: correlation of proton magnetic resonance spectroscopy and plasma homovanillic acid. Arch Neurol. 2000;57:1280–1285. [DOI] [PubMed] [Google Scholar]
- 11.Haley RW, Luk GD, Petty F. Use of structural equation modeling to test the construct validity of a case definition of Gulf War syndrome: invariance over developmental and validation samples, service branches and publicity. Psychiatry Res. 2001;102:175–200. [DOI] [PubMed] [Google Scholar]
- 12.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston, Mass: Health Institute; 1997.
- 13.Iowa Persian Gulf Study Group. Self-reported illness and health status among Gulf War veterans: a population-based study. JAMA. 1997;277:238–245. [PubMed] [Google Scholar]


