Abstract
Objectives. This study determined the percentage of adverse outcomes in US men attributable to combat exposure.
Methods. Standardized psychiatric interviews (modified Diagnostic Interview Schedule and Composite International Diagnostic Interview assessments) were administered to a representative national sample of 2583 men aged 18 to 54 in the National Comorbidity Survey part II subsample.
Results. Adjusted attributable fraction estimates indicated that the following were significantly attributable to combat exposure: 27.8% of 12-month posttraumatic stress disorder, 7.4% of 12-month major depressive disorder, 8% of 12-month substance abuse disorder, 11.7% of 12-month job loss, 8.9% of current unemployment, 7.8% of current divorce or separation, and 21% of current spouse or partner abuse.
Conclusions. Combat exposure results in substantial morbidity lasting decades and accounts for significant and multifarious forms of dysfunction at the national level.
Horrific combat experiences were among the defining phenomena of the 20th century. Although exposure to combat is a well-known risk factor for posttraumatic stress disorder (PTSD),1–6 PTSD research has focused on individual costs rather than on the societal costs (e.g., national burden of illness) associated with exposure to combat. To date, the proportion of cases of PTSD among US males that is attributable to combat exposure remains undetermined. Although research has demonstrated high rates of psychiatric comorbidity among people with combatrelated PTSD,1,4,6–8 little is known about the proportion of other forms of psychiatric morbidity, such as substance abuse and major depressive disorders, attributable to combat exposure. Combat-related PTSD has also been linked to occupational morbidity9,10 and interpersonal violence in relationships with female partners.11,12 The population attributable fractions of these adverse outcomes that are associated with combat exposure have never, to our knowledge, been estimated. The aim of this study was to determine the population attributable fractions of a variety of pathologic outcomes among US males aged 18 to 54 years.
METHODS
Sample
Data were derived from the National Comorbidity Survey (NCS),13 a study designed to examine the distribution, correlates, and consequences of psychiatric disorders in a nationally representative US sample. The survey was based on a stratified, multistage area probability sample of persons aged 15 to 54 years in the noninstitutionalized civilian population. From 1990 through 1992, the NCS surveyed 8098 persons. The response rate was 82.4%. Informed consent was obtained from all respondents and also from parents of minors. Further details about the NCS are provided elsewhere.6,13
All 8098 respondents were administered the part I interview. Part II included a more thorough assessment of risk factors and secondary diagnoses, including PTSD, not included in the core diagnostic interview. Part II was a subsample of respondents that included all respondents aged 15 to 24 years (99.4% of whom completed part II), all others who screened positive in part I for a lifetime prevalence of any psychiatric disorder (98.1% of whom completed part II), and a random subsample of other respondents (99% of whom completed part II). Part II was completed by 5877 respondents. Weights provided by the NCS were used to make the sample representative of the general US population6 on major sociodemographic characteristics. Given that no women in the NCS reported combat trauma, and that men aged 15 to 17 years could not have been exposed to combat, the sample was restricted to men aged 18 to 54 years. The resulting number of male respondents 18 years and older was 2583, which was reduced to 2578 owing to missing combat exposure data. The weighted sample size (Nw) was 2521.
Measures
The NCS asked questions for each of 11 types of specific traumatic experiences, 1 of which was exposure to combat. Among the weighted sample of 2521, 179 (7.1%) reported that they had been exposed to combat.
The NCS used a modified version of the Composite International Diagnostic Interview,14,15 a comprehensive, fully standardized interview used to assess mental disorders according to the definitions and criteria found in the Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition (DSM-III-R).16 Diagnoses for major depressive disorder and substance use disorders (alcohol abuse without dependence, alcohol dependence, drug abuse without dependence, drug dependence) were based on established criteria, excluded requirements for related functional impairments, and were generated by the Composite International Diagnostic Interview program.17 Field trial data have confirmed their reliability and validity.18
PTSD was assessed in the NCS with a modified version of the Revised Diagnostic Interview Schedule.19 Symptom questions in the Diagnostic Interview Schedule were used to evaluate PTSD criteria B through D (where B = “re-experiencing,” C = “avoidance,” and D = “hyperarousal”). The diagnosis of PTSD did not require that DSM-III-R criterion F, which stipulates that the symptoms cause distress or impairment in important areas of functioning, be met. Diagnostic Interview Schedule coding rules for these criteria were applied to obtain a diagnosis of PTSD. Criteria B through D were evaluated for only 1 event per respondent. Respondents who reported experiencing more than 1 event were asked which of these events was the “most upsetting.” Because the NCS focused on PTSD symptomatology resulting from only the “most upsetting” trauma, the lifetime prevalence of PTSD may have been underestimated because PTSD resulting from other traumas was not assessed. PTSD as an outcome variable reflected meeting criteria within the 12 months before the interview. PTSD as a mediator variable reflected meeting criteria for PTSD at some point more than 12 months before the interview.
Other analyzed variables included age, race, “urbanicity,” socioeconomic status (SES) in family of origin, current unemployment, having been fired or lost a business in the last year, current divorce, and current abuse of one's spouse or partner. Currently married or cohabitating men were asked to look at a list of current behaviors toward their spouses or partners. Those who responded that they grabbed, pushed, shoved, threw things at, slapped, spanked, kicked, bit, hit or tried to hit, beat up, choked, burned, or scalded their current partner or spouse “often” or “sometimes” were coded “1 = yes” for spouse or partner abuse. Men who answered “never” or “rarely” to these behaviors were coded “0 = no.” “Urbanicity” was defined as residence in a county with 250 000 or more residents, vs areas with fewer residents. Low SES in the family of origin was coded positively either if the major source of financial support before 15 years of age was welfare, financial aid, a foster home, or an orphanage or if the primary wage earner had less than 12 years of formal schooling and a Census Occupation Code of 300 or higher (e.g., clerical workers, laborers). Each of these characteristics was identified by us or others1,3,6,12,19,20 as associated with exposure to combat, the onset of PTSD, or both.
Analyses
Population attributable fractions of psychiatric disorders and behavioral outcomes represent the percentage of all cases of each outcome among the exposed and unexposed that would not have occurred if exposure had not occurred.21 We used the formula
 |
, where AF is the population attributable fraction, p is the proportion exposed in the entire cohort (p = .071 for combat), and RR is the relative risk of negative outcomes given combat exposure. We estimated relative risks from generalized linear models by means of a logarithmic link function and a binomial error structure with an adjustment to ensure that the predicted probabilities remained within the 0–1 range.22 A likelihood ratio-based χ2 statistic was used to evaluate their significance. One set of analyses used unadjusted relative risks. Another set of analyses used relative risks adjusted for age (years), race (White or other), urbanicity, and low SES in family of origin, because prior results suggest that these factors may confound the relationship between combat exposure and the likelihood of functional impairment.
Path models were used to examine the ways in which PTSD mediated the effects of combat exposure on the examined recent or current adverse outcomes. Using the SAS version 6.12 “CALIS”23 procedure, we simultaneously estimated the direct effects of combat exposure on current vs prior-12-month outcomes and the indirect effects of combat exposure mediated through history of PTSD before the 12 months preceding the NCS interview. Tetrachoric correlations were used to estimate path coefficients for dichotomous outcomes.24
RESULTS
The relative risks and population attributable fractions for psychiatric and behavioral outcomes associated with combat exposure among men are displayed in Table 1 ▶. Unadjusted estimates reveal that combat exposure contributed significantly to 12-month PTSD, 12-month major depressive disorder, current unemployment, 12-month job loss, current separation or divorce, and current spouse or partner abuse.
TABLE 1.
—Relative Risks (RRs) and Population Attributable Fractions (AFs) for Psychiatric and Behavioral Outcomes Associated With Exposure to Combat
| Unadjusted | Adjusteda | |||||
| Outcome | RR (95% CI) | AF, % (95% CI) | P | RR (95% CI) | AF, % (95% CI) | P |
| 12-month PTSDb | 4.87 (2.78, 8.11) | 21.6 (11.2, 33.6) | <.001 | 6.42 (3.44, 11.65) | 27.8 (14.8, 43.1) | <.001 |
| 12-month depressionb | 1.56 (1.00, 2.30) | 3.8 (0.0, 8.4) | .048 | 2.12 (1.33, 3.21) | 7.4 (2.3, 13.6) | .002 |
| 12-month substance abuseb | 1.10 (0.54, 1.97) | 0.7 (NE, 6.4) | NS | 2.22 (1.06, 4.15) | 8.0 (0.4, 18.3) | .036 |
| Current unemploymentb | 1.86 (1.23, 2.69) | 5.8 (1.6, 10.7) | .004 | 2.37 (1.55, 3.44) | 8.9 (3.8, 14.8) | <.001 |
| 12-month job lossc | 2.40 (1.45, 3.74) | 8.9 (3.0, 16.0) | .001 | 2.90 (1.70, 4.70) | 11.7 (4.6, 20.5) | <.001 |
| Current separation/divorceb | 3.22 (2.37, 4.26) | 13.6 (8.9, 18.8) | <.001 | 2.20 (1.62, 2.91) | 7.8 (4.2, 12.0) | <.001 |
| Current spouse/partner abused | 3.30 (1.35, 7.01) | 15.2 (2.7, 32.0) | .011 | 4.40 (1.68, 10.49) | 21.0 (5.0, 42.6) | .004 |
Note. PTSD = posttraumatic stress disorder; CI = confidence interval; NS = not significant; NE = could not be estimated. For all men in part II sample (see Methods) 18 years or older, n = 2583. For missing data for combat exposure, n = 5. NW refers to the size of the weighted sample. All estimates are based on weighted samples.
aEstimates adjust for age, race (White or other), urbanicity, and low socioeconomic status in family of origin.
bn = 2578; NW = 2521; proportion of the sample indicating combat exposure = 0.071.
cTwelve-month job loss among those currently employed. n = 2248; NW = 2137; proportion of sample indicating combat exposure = 0.070.
dCurrent spouse or partner abuse among those currently cohabitating. n = 1337; NW = 1644; proportion of sample indicating combat exposure = 0.078.
In models that adjusted for several potential confounding influences, all assessed outcomes were significantly associated with combat exposure. The adjusted relative risk for 12-month PTSD associated with combat exposure was 6.42 (27.8% attributable to combat exposure); for 12-month major depressive disorder the adjusted relative risk was 2.12 (7.4% attributable to combat exposure) and for 12-month substance abuse it was 2.22 (8.0% attributable to combat exposure). Adjusted relative risks were 2.37 for current unemployment (8.9% attributable to combat exposure), 2.9 for 12-month job loss (11.7%), 2.2 for current divorce or separation (7.8%), and 4.4 for current spouse or partner abuse (21.0%).
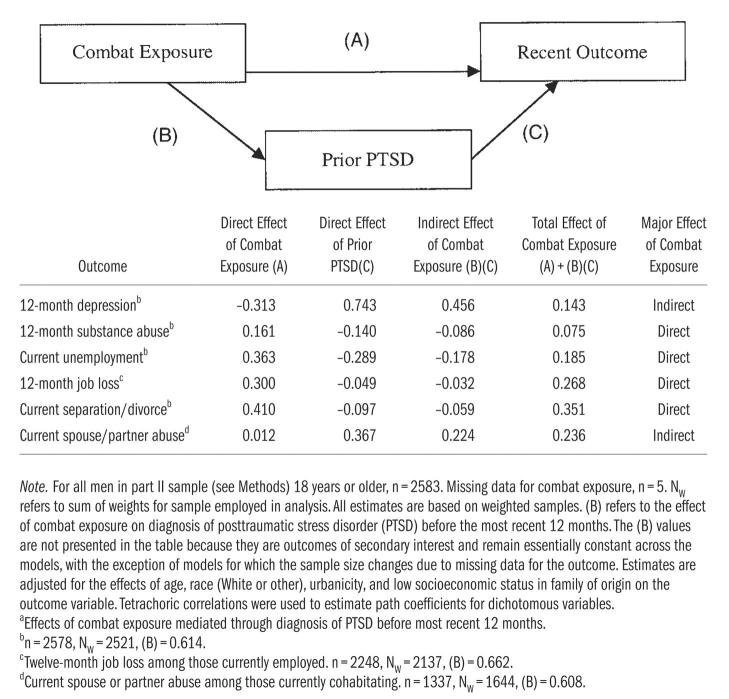
The results of the path analyses displayed in Figure 1 ▶ (and accompanying table) suggest that most of the assessed outcomes (4 of 6, 66.7%) were primarily direct consequences of combat exposure. For example, the direct effect of combat exposure accounted for most of the total effect in the prediction of 12-month substance abuse. In the path models, lifetime PTSD (predating the 12 months before the NCS interview) was negatively associated with the likelihood of 12-month substance abuse (the inverse association between prior history of PTSD and 12-month substance abuse was confirmed in additional analyses yielding a tetrachoric correlation of –0.05). A similar pattern was found for the direct effects of combat exposure on current unemployment, 12-month job loss, and current separation or divorce from a partner or spouse. For each of these outcomes, the direct effects of combat exposure accounted for the largest proportion of the model's total effect, with the prior history of PTSD demonstrating an inverse association with each outcome.
FIGURE 1.
—Direct, indirect,a and total effects of combat exposure on psychiatric and behavioral outcomes.
By contrast, meeting criteria for major depressive disorder within the prior 12 months was primarily an indirect consequence of combat exposure that was mediated by a strong direct effect of prior history of PTSD. In fact, combat exposure had a negative direct effect on 12-month major depressive disorder when the prior history of PTSD was entered into the model. The current abuse of one's spouse or partner was also primarily an indirect effect of combat exposure mediated through prior history of PTSD.
DISCUSSION
The findings of this study provide new information on the long-lasting negative influence of combat exposure on our nation's mental, social, and economic health. Given that significant fractions of psychiatric illness in the year before the NCS interview, current unemployment, job loss, marital dissolution, and spouse abuse would probably not have occurred had these men not been directly exposed to war, the results highlight the considerable and enduring societal costs of exposing men to combat. On an individual level, the results also document the profound and persistent detrimental effects of combat exposure on male veterans and their spouses or partners.
Despite the fact that for most NCS respondents combat had occurred during the Vietnam War—over 2 decades before the NCS assessment—adjusted estimates indicate that without exposure to combat, nearly 30% of the 12-month cases of PTSD and 21% of current abuse of one's partner or spouse would probably not have occurred had these men not been exposed to combat. The latter result supports the “cycle of trauma” hypothesis described by Byrne and Riggs,12 who also found escalated violence toward female partners among Vietnam War veterans who had been traumatized in combat. Consistent with this, as the path models suggest, spouse or partner abuse was principally an indirect consequence of combat that was mediated through PTSD. Similarly, the effect of combat exposure on 12-month major depressive disorder was primarily an indirect effect mediated through a history of PTSD predating the year before the interview. These results suggest that when PTSD does not occur following combat exposure, male veterans would not be expected to commit spouse or partner abuse or to have major depressive disorder long after combat. Further, these results suggest that effective treatment of combat-related PTSD might prevent enduring or late-onset spouse abuse and major depressive disorder among male veterans.
By contrast, combat exposure had a direct effect on current unemployment and job loss. Adjusted estimates reveal that nearly 9% of current unemployment and nearly 12% of recent 12-month job loss could be attributed to combat exposure. These results are generally consistent with the occupational morbidity observed by Engel et al.9 in their study of Gulf War veterans, although they examined the influence of PTSD and not combat exposure per se. The path models illustrate how combat directly affected current or recent occupational morbidity—an effect that was not mediated by PTSD. These findings suggest that something particular to the war experience, and not a function of combat-related PTSD, makes it difficult to remain employed. Similarly, the findings also provide new information indicating a significant, relatively large direct effect of combat exposure on rates of current separation and divorce that was not mediated by PTSD.
The results of this report reveal that in models adjusting for confounding factors such as urbanicity and SES in family of origin, 8% (P < .04) of 12-month substance abuse disorders are attributable to combat exposure. Nevertheless, in contrast with studies that indicate high rates of substance abuse among veterans with PTSD,1,7,8,25 path modeling suggested that the effect of combat exposure on 12-month substance abuse was direct and not mediated by a prior history of PTSD (which itself was negatively associated with 12-month substance abuse).
Several limitations of the study deserve mention. First, the NCS is a cross-sectional survey and not a prospective, longitudinal study. The dating of events was incomplete and the history of psychiatric illness was based on retrospective reports provided by the respondent. Because combat exposure does not appear to be randomly assigned to people in the general population and no prospective prewar measures of adjustment and psychopathology were available in the NCS, future research that follows men from before entering war through combat exposure and forward in time to assess long-term outcomes of combat would be needed to determine, in a more conclusive way, the causal chain of events suggested in this report.
Another limitation is that PTSD was assessed with respect to the single most upsetting trauma, which could have resulted in an underestimate of the prevalence of PTSD in this sample. In addition, given the stigma associated with outcomes such as being physically abusive to one's spouse or partner, these events may have been underreported. Future studies that document PTSD associated with each traumatic exposure a respondent reports and that use objective records of abuse (e.g., police reports, reports by witnesses) are needed to confirm the results presented in this study.
The recent deployment of US special operations forces and the call to active duty of thousands of American soldiers to fight the “war on terrorism” reawakens a long-dormant interest in understanding the societal costs of war. By documenting the enduring negative effects of combat exposure on the nation's mental, social, and occupational health, this report demonstrates the lasting and pernicious effects of exposing US citizens to war.
Acknowledgments
This work was supported in part by NIMH grant MH56529 and a grant from the American Foundation for Suicide Prevention.
H. G. Prigerson, P. K. Maciejewski, and R. A. Rosenheck planned the study. P. K. Maciejewski conducted the analyses. All authors contributed to the writing of the paper.
Peer Reviewed
References
- 1.Kulka R, Schlenger W, Fairbank J, et al. Trauma and the Vietnam War Generation. New York, NY: Brunner/Mazel; 1990.
- 2.Mellman TA, Randolph CA, Brawman-Mintzer O, Flores LP, Milanes FJ. Phenomenology and course of psychiatric disorders associated with combat-related posttraumatic stress disorder. Am J Psychiatry.1992;149:1568–1574. [DOI] [PubMed] [Google Scholar]
- 3.Foy DW, Sipprelle RC, Rueger DB, Carroll EM. Etiology of posttraumatic stress disorder in Vietnam veterans: analysis of premilitary, military, and combat exposure influences. J Consult Clin Psychol. 1984;52:79–87. [DOI] [PubMed] [Google Scholar]
- 4.Helzer JE, Robins LN, McEvoy L. Post-traumatic stress disorder in the general population. Findings of the Epidemiologic Catchment Area Survey. N Engl J Med. 1987;317:1630–1634. [DOI] [PubMed] [Google Scholar]
- 5.Fontana A, Rosenheck R. Posttraumatic stress disorder among Vietnam theater veterans: a causal model of etiology in a community sample. J Nerv Ment Dis. 1994;182:677–684. [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry.1995;52:1048–1060. [DOI] [PubMed] [Google Scholar]
- 7.True WR, Goldberg J, Eisen SA. Stress symptomatology among Vietnam veterans: analysis of the Veterans Administration Survey of Veterans II. Am J Epidemiol. 1988;177:154–159. [DOI] [PubMed] [Google Scholar]
- 8.Sierles FS, Chen J-J, McFarland RE, Taylor MA. Posttraumatic stress disorder and concurrent psychiatric illness: a preliminary report. Am J Psychiatry.1983;140:1177–1179. [DOI] [PubMed] [Google Scholar]
- 9.Engel CC, Ursano R, Magruder C, et al. Psychological conditions diagnosed among veterans seeking Department of Defense care for Gulf War–related health concerns. J Occup Environ Med. 1999;4:384–392. [DOI] [PubMed] [Google Scholar]
- 10.Savoca E, Rosenheck R. The civilian labor market experience of Vietnam-era veterans: the influence of psychiatric disorders. J Ment Health Policy Econ. 2001;3:199–207. [DOI] [PubMed] [Google Scholar]
- 11.Beckham JC, Feldman ME, Kirby AC. Atrocities exposure in Vietnam combat veterans with chronic posttraumatic stress disorder: relationship to combat exposure, symptom severity, guilt and interpersonal violence. J Trauma Stress.1998;11:777–785. [DOI] [PubMed] [Google Scholar]
- 12.Byrne CA, Riggs DS. The cycle of trauma: relationship aggression in male Vietnam veterans with symptoms of posttraumatic stress disorder. Violence Vict. 1996;11:213–225. [PubMed] [Google Scholar]
- 13.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. [DOI] [PubMed] [Google Scholar]
- 14.Composite International Diagnostic Interview, Version 1.0. Geneva, Switzerland: World Health Organization; 1990.
- 15.Robins LN, Wing J, Wittchen H-U, Helzer JE. The Composite International Diagnostic Interview: an epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry.1988;45:1069–1077. [DOI] [PubMed] [Google Scholar]
- 16.Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition. Washington, DC: American Psychiatric Association; 1987.
- 17.Composite International Diagnostic Interview Computer Programs, Version 1.1. Geneva, Switzerland: World Health Organization; 1990.
- 18.Wittchen H-U. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. [DOI] [PubMed] [Google Scholar]
- 19.Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry.1991;48:216–222. [DOI] [PubMed] [Google Scholar]
- 20.Davidson JR, Hughes D, Blazer DG, George LK. Post-traumatic stress disorder in the community: an epidemiological study. Psychol Med. 1991;21:713–721. [DOI] [PubMed] [Google Scholar]
- 21.Greenland S. Applications of stratified analysis method. In: Rothman KJ, Greenland S, eds. Modern Epidemiology. 2nd ed. Philadelphia, Pa: Lippincott-Raven Publishers; 1998:295–297.
- 22.Wacholder S. Binomial regression in GLIM: estimating risk ratios and risk differences. Am J Epidemiol. 1986;123:174–184. [DOI] [PubMed] [Google Scholar]
- 23.SAS, Version 6.12 [computer program]. Cary, NC: SAS Institute Inc; 1996.
- 24.Bollen K. Structural Equations With Latent Variables. New York, NY: John Wiley & Sons Inc; 1989:433–446.
- 25.Jordan BK, Schlenger WE, Hough R, et al. Lifetime and current prevalence of specific psychiatric disorders among Vietnam veterans and controls. Arch Gen Psychiatry.1991;48:207–215. [DOI] [PubMed] [Google Scholar]