Abstract
This study examined (1) the relationship between income inequality and mortality among all counties in the contiguous United States to ascertain whether the relationships found for states and metropolitan areas extend to smaller geographic units and (2) the influence of minority racial concentration on the inequality–mortality linkage.
Methods. This county-level ecologic analysis used data from the Compressed Mortality Files and the US Census. Weighted least squares regression models of age-, sex-, and race-adjusted county mortality rates were estimated to examine the additive and interactive effects of income inequality and minority racial concentration.
Results. Higher income inequality at the county level was significantly associated with higher total mortality. Higher minority racial concentration also was significantly related to higher mortality and interacted with income inequality.
Conclusions. The relationship between income inequality and mortality is robust for counties in the United States. Minority concentration interacts with income inequality, resulting in higher mortality in counties with low inequality and a high percentage of Blacks than in counties with high inequality and a high percentage of Blacks.
Higher levels of inequality have been associated with a variety of societal problems, including higher mortality.1,2 Prior research has examined the relationship between income inequality and mortality for states and metropolitan areas in the United States.1,3–5 This research used different measures of income inequality and, with few exceptions,6,7 found strong relationships between income inequality and mortality. High levels of inequality, poverty, and mortality often are found in areas that have high concentrations of minorities, in particular Blacks.2,8 Despite this evidence, few studies have examined the influence of minority racial concentration on the relationship between inequality and mortality (for exceptions, see LaVeist9 and Jackson et al.10). In this study we addressed whether the income inequality gradient in mortality extends to the county level and whether counties with high concentrations of Blacks have higher mortality than counties with similar levels of inequality but a low or no predominance of Blacks.
The disadvantaged position of Blacks in US society is well documented. Blacks are disproportionately found in lower-income categories11 and have higher mortality. The reasons suggested for higher mortality among Blacks vary greatly12–15 but include genetic variation, lifestyle and cultural differences, socioeconomic disadvantage, and the social and psychological consequences of discrimination.16–18
Research on the effect of income inequality on mortality within nations offers 2 principal pathways through which income inequality operates. The negative consequences may be exacerbated in communities with high concentrations of minorities. First, Daly et al.7 and Lynch et al.5 posit that political units with highly unequal income distributions are less likely to invest in affordable housing, education, environmental protection, economic development, and other resources required for the health of their populations. This underinvestment has negative consequences for the health of poor and middle-class individuals.
Second, as Daly et al. note, “inequitable income distribution may directly affect people's perceptions of their social environment, which may in turn have an impact on their health.”7(p319) This postulated psychosocial pathway linking health and mortality stems from the conditions in highly inequitable communities that result in lower social cohesion, inequities in social and political influence, and less willingness to participate in community activities.19 Further, Wilkinson20 argues that the impacts of inequality result less from the experience of inferior material conditions than from social meanings that individuals give to their circumstances and from the effects of stress on both the endocrine and the immune systems. While the exact pathways through which income inequality influences mortality are still being defined, there is strong agreement that the determinants of health and mortality include factors beyond the level of the individual.10,16,21–25
Patterns of underinvestment in infrastructure are especially likely to be observed in areas with concentrations of minorities26–29 and a White power elite. There also is evidence that Blacks live in areas with higher levels of income inequality.27,30–33 Despite their lower income levels, controlling for individual income accounts for only about one third of the greater mortality risk among Blacks34 and controlling for health risk factors explains only an additional 31% of the racial differential in mortality.18
The residential segregation still experienced by Blacks2,8 is a continual reminder of their lower status. This may be especially true for those in poor center-city neighborhoods and in the small towns of the rural South. As LaVeist9 points out, “many middle-income Blacks are forced to live in socioenvironmental conditions that—although superior to those of low-income Blacks—are not consistent with their economic status.” In addition, local power structures are often based on economic rather than political power, so the control over resources and decision making often remains in the hands of a local economic (usually White) elite.24,29,35
We extend prior research by examining income inequality and mortality for the counties of the contiguous United States. Most earlier research used states or metropolitan areas as the unit of analysis. We use county-level data for 2 reasons. First, local (substate-level) inequality is likely to produce the largest variation in local infrastructure and perceptions of relative status. Whereas neighborhoods may be important in metropolitan counties, nonmetropolitan residents are more likely to view the county as an important economic and social unit. The availability and accessibility of health care and of educational, civic, cultural, job, environmental, and recreational opportunities are largely determined at the local level and influenced by local structures. The county is often the decision-making unit for providing and organizing local services. Moreover, recent research on income inequality and morbidity reveals stronger relationships at the county level than among census tracts.36 Second, the areas excluded from earlier studies (e.g., nonmetropolitan counties) have higher income inequality, on average.37 Including all counties in the contiguous United States provides a more representative picture of the full experience of Americans.
METHODS
Data on mortality and population were extracted from the Compressed Mortality File produced by the National Center for Health Statistics. This file is a county-level database that permits calculation of county-level total mortality rates. These are 5-year averages (1988–1992, centered on 1990) and are annualized rates. The rates were adjusted by age and sex, or by age, sex, and race, with the 1990 US population used as the standard. An average of 5 years of data was used to increase the stability of rates for counties with smaller populations and fewer deaths. Even when multiple years of data are used, the variance in death rates generally is larger for counties with smaller populations, indicating the need to weight the analysis by using the inverse of the variance of the county mortality rates.5 Thus, we estimated county-level models by using weighted least squares regression.
A total mortality rate combines all residents in a county; each racial group thereby contributes to the calculation of the county's total mortality rate through its proportion in the population and through the race-specific mortality rates. Thus, there are 2 approaches to incorporating the effects of race in ecologic models. The first is to control race by adding to the multivariate model an independent variable reflecting racial concentration. Racial concentration was measured by the percentage of the county population that was Black in 1990. We selected percentage that was Black because it reflects the predominance of the minority group in the county.10
The second approach is to standardize the dependent variable for racial composition by using age-, sex-, and race-adjusted total mortality rates. In this case, the racial composition of the US population is used as the standard and the total county mortality rates are standardized, so that each county has the same race, age, and sex composition.38 Race then affects the overall mortality rate for the county through differences in the race-specific mortality rates or through other factors (e.g., underinvestment) associated with racial concentration. We used both approaches.
County-level data on household income inequality were obtained from the 1990 US Census.39 We used the 90th:10th percentile share ratio as our measure of income inequality, which is simply the ratio of the share of household income held by the top 10% of households divided by the share of household income held by the bottom 10%.40,41 Census data report numbers of households in particular income categories, so to calculate the 90:10 ratio, we assumed that households were equally distributed within an income category. We used county per capita income as a measure of income levels in each county. Median household size for each county also was included.
Using the results from the estimated models, we derived measures of excess mortality. We determined excess mortality by dividing the income inequality measure into quartiles and using the quartiles as independent variables in the regression models. Because the lowest inequality quartile is used as the reference group, the difference in mortality rates between the lowest inequality quartile (Q1) and the highest inequality quartile (Q4)—the excess mortality due to highest inequality—is the estimated coefficient for Q4.5
RESULTS
Age- and Sex-Adjusted Total Mortality
Descriptive statistics for the variables in the model appear in the first column of Table 1 ▶. The model of income inequality and mortality for 3067 counties in the contiguous United States is shown as the base model, model 1 of Table 1 ▶.
TABLE 1.
—Weighted Least Squares Model Results From Analysis of Total Mortality Rates for 3067 Counties in the Contiguous United States
| Age- and Sex-Adjusted Total Mortality Rate (Mean = 875.9; SD = 113.6; Range = 415–1838) | Age, Sex, and Race-Adjusted Total Mortality Rate (Mean = 841.0; SD = 121.17; Range = 270–1468) | ||||||
| Descriptive Statistics, Mean (SD) [Minimum– Maximum] | Base Model (Model 1) Coefficient (SE) | Base + % Black (Model 2)a Coefficient (SE) | Base + % Black Interactions (Model 3) Coefficient (SE) | Base Model (Model 4)a Coefficient (SE) | Base + % Black Base Model (Model 5)b Coefficient (SE) | Base + % Black Interactions (Model 6)b Coefficient (SE) | |
| Intercept | 899.21*** (11.21) | 899.31*** (9.55) | 900.02*** (9.47) | 757.46*** (12.53) | 745.20*** (11.68) | 747.70*** (11.53) | |
| 2nd quartile income inequality (Q2) | 47.27–55.00 | 30.19*** (3.77) | 19.26*** (3.23) | 10.85*** (3.68) | 72.14*** (4.31) | 62.82*** (4.04) | 59.30*** (4.67) |
| 3rd quartile income inequality (Q3) | 55.09–65.00 | 74.31*** (3.90) | 46.90*** (3.42) | 55.25*** (3.90) | 94.86*** (4.45) | 69.93*** (4.30) | 81.78*** (5.05) |
| 4th quartile income inequality (Q4) | 65.05 and up | 108.53*** (4.16) | 42.33*** (4.04) | 46.74*** (4.88) | 129.67*** (4.56) | 83.60*** (4.75) | 110.22*** (5.71) |
| 90th: 10th percentile income share ratio | 56.54 (11.41) | ||||||
| [26.97–112.18] | |||||||
| Per capita income | 11 094 (2645) | –0.009*** (0.00039) | –0.009*** (0.00034) | –0.009*** (0.00034) | –0.002*** (0.00043) | –0.002*** (0.0004) | –0.003*** (0.0004) |
| [3417–28 381] | |||||||
| Median household size | 2.12 (0.33) | 13.31*** (4.65) | 13.12*** (3.96) | 12.98*** (3.93) | 20.55*** (5.11) | 24.25*** (4.76) | 21.277*** (4.69) |
| [2.0–4.0] | |||||||
| % Black | 8.53 (14.32) | 3.76*** (0.11) | 4.38*** (0.44) | 2.71*** (0.12) | 5.95*** (0.54) | ||
| [0–86.12] | |||||||
| Q2 × % Black | 1.23* (0.52) | –1.199 (0.62) | |||||
| Q3 × % Black | –1.32* (0.48) | –3.45*** (0.58) | |||||
| Q4 × % Black | –0.78 (0.47) | –4.16*** (0.57) | |||||
| R2 | 0.341 | 0.522 | 0.53 | 0.233 | 0.335 | 0.356 | |
| Excess mortality (rounded to integers)c | 109 | 42 | 47 | 130 | 84 | 110 | |
Note. All analyses are weighted by the inverse of the variance in mortality rates for that county.
aGray-shaded coefficients are statistically different from those in model 1.
bGray-shaded coefficients are statistically different from those in model 4.
cExcess mortality is the difference in estimated mortality rates between the high and low quartiles of income inequality, after control for other variables. Because the reference group in the models is the lowest quartile of income inequality, the excess mortality is the same as the estimated coefficient for the highest quartile of income inequality, Q4.
*P ≤ .05; **P ≤ .01; ***P ≤ .001 for a 2-tailed test.
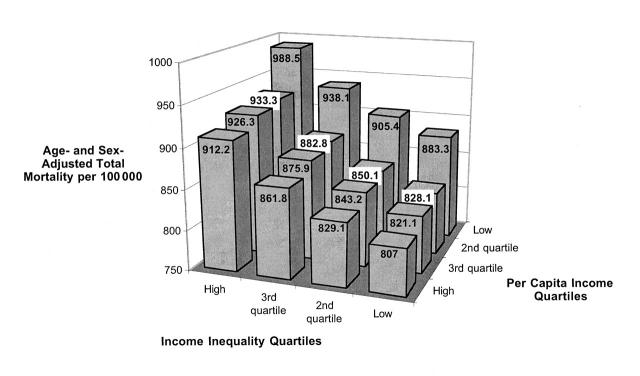
All coefficients are statistically significant in influencing age- and sex-adjusted mortality, and income inequality has a strong effect. There clearly is a gradient, such that there are 108.5 more deaths per 100 000 people in a year in counties with the highest income inequality than in those in the lowest quartile. Higher per capita income is associated with lower mortality rates. A $1000 increase in per capita income corresponds to a decline of 9 deaths per 100 000 people. Figure 1 ▶ displays the joint distribution of age- and sex-adjusted mortality for quartiles of income inequality and per capita income after adjustment for median household size.
FIGURE 1.
—Age- and sex-adjusted total mortality rates, by income inequality quartile and per capita income, in 3067 counties in the contiguous United States.
The combined effects of high income inequality and low per capita income result in an age-adjusted mortality rate (988.5 per 100 000) over 22% higher than in counties where per capita income is high and inequality is low (807 per 100 000)—a difference of 181 excess deaths per 100 000 people. We find a larger gradient across income inequality levels within per capita income category than across per capita income levels within income inequality levels.
Model 2 in Table 1 ▶ shows the results of adding the percentage of Blacks to model 1. This significantly increases the variance explained (R2 increases from 0.341 to 0.522), and it reduces the coefficients for income inequality quartiles (the bivariate correlation of percentage of Blacks and 90:10 ratio is 0.43). When percentage of Blacks is added to model 2, excess mortality declines to 42 deaths per 100 000, down from 109 deaths per 100 000 in model 1. The coefficients for Q3 and Q4 (the 2 higher-inequality quartiles) are not statistically different, so the gradient extends only through Q3. This suggests an interaction between levels of inequality and concentrations of Blacks in the counties. Each percentage point increase in the percentage of Blacks corresponds with 3.8 additional deaths per 100 000 people per year.
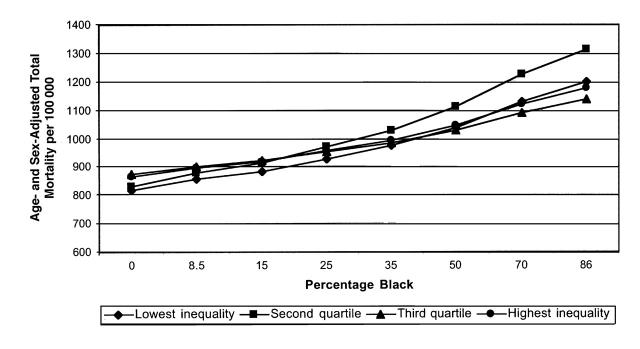
Model 3 includes interactions of the percentage of Blacks and the income inequality quartiles. The coefficients for the main effects are not statistically different from those in model 2, but the interaction effects are statistically significant. To aid in interpreting the interaction effects, Figure 2 ▶ shows the plot of estimated mortality based on the model coefficients and selected levels of percentage of Blacks. At a low percentage of Blacks, mortality is lowest and increases slightly from the lowest inequality to the third quartile of inequality—consistent with a slight gradient of mortality with increasing income inequality. As the percentage of Blacks exceeds 15%, the gap in mortality among inequality quartiles grows. At the highest percentage of Blacks in the data set (86%), the predicted mortality rate is highest among persons living in counties in the second quartile of income inequality and lowest among those in counties in the third quartile of inequality. Using percentage of Blacks, however, does not separate the effects on the mortality rate of different racial composition across counties from the other effects that might be associated with minority concentrations.
FIGURE 2.
—Estimated age- and sex-adjusted mortality rates, by income inequality quartile and percentage of Blacks, in 3067 counties in the contiguous United States.
Age-, Sex-, and Race-Adjusted Total Mortality
To eliminate the effects of local variations in racial composition in the calculation of the dependent variable, we standardized the mortality rate for age, sex, and race. The estimated coefficients for the base model using the age-, sex-, and race-adjusted total mortality rate are shown in Table 1 ▶, model 4. The gradient of mortality with income inequality reappears in this model, and the coefficients are statistically larger for the inequality quartiles in this model than in the base model using the age- and sex-adjusted total mortality rate (model 1). The largest increase is from the lowest quartile (Q1 or reference group) to the second quartile (Q2) of income inequality, 72 deaths per 100 000. There are 130 excess deaths per 100 000 due to high inequality in this model specification, compared with 108.5 per 100 000 in model 1.
The reappearance of the gradient of mortality with income inequality in model 4 suggests that the reduction in the mortality–inequality gradient when percentage of Blacks was added in earlier models was due either to race-specific differences in mortality rates or to other factors related to minority concentration. Clearly, the reduction is not just a “racial composition effect.”
Even when age-, sex-, and race-adjusted total mortality is used, percentage of Blacks is associated with higher mortality rates—each percentage point increase in the Black population increases mortality by 2.7 deaths per 100 000 (model 5). As in the earlier model, the income inequality gradient in mortality is reduced, with the reduction occurring primarily in the third and highest inequality quartiles, again suggesting an interaction effect. This model increases the explained variance substantially (R2 increases from 0.233 to 0.335).
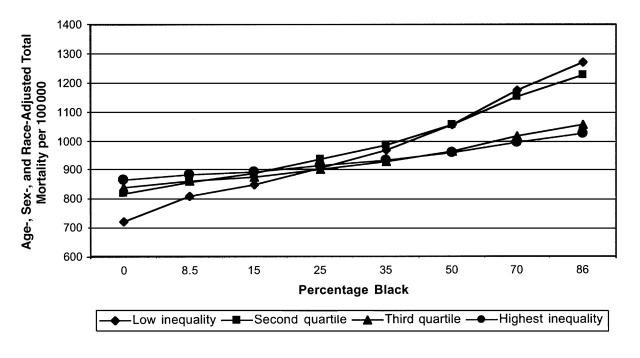
Adding the percentage of Blacks by inequality quartile interaction terms (model 6 in Table 1 ▶) causes the main effects of inequality to return to a clear gradient, such that higher inequality is associated with higher mortality. The interaction terms suggest, however, that the influence of inequality declines as the percentage of Blacks increases, and that this is especially pronounced at higher levels of inequality. This relationship is shown in Figure 3 ▶, which is based on age-, sex-, and race-adjusted mortality rates predicted from model 6.
FIGURE 3.
—Estimated age-, sex-, and race-adjusted total mortality rates, by income inequality quartile and percentage of Blacks, in 3067 counties in the contiguous United States.
Figure 3 ▶ shows a marked interaction between the percentage of Blacks and income inequality levels. At the lowest levels of percentage of Blacks, the income inequality gradient in mortality is as expected—counties with the highest inequality have the highest mortality rates. These lines tend to cross over in counties in the middle range of the percentage of Blacks. Beyond a concentration of about 25% Black, there is a divergence in mortality rates, with counties in the 2 lowest income inequality quartiles showing the highest mortality and counties in the 2 highest income inequality quartiles having lower mortality rates. At the extreme, counties with a population that is 86% Black and with lowest income inequality have the highest mortality (1270 per 100 000), followed closely by counties with the second lowest inequality (1226 per 100 000). The estimated mortality rates for the 2 highest income inequality quartiles in the counties with high concentrations of Blacks are more than 200 deaths per 100 000 fewer than in the low-inequality counties (1055 per 100 000 and 1022 per 100 000 for the third and highest inequality counties, respectively).
DISCUSSION
The findings from our ecologic analysis of counties in the contiguous United States show that counties with higher income inequality have higher mortality rates than counties with low income inequality, consistent with studies conducted using states or metropolitan areas. This analysis extends prior studies by using smaller political units (counties) and by including counties in rural as well as urban areas. Thus, the full range of income inequality and mortality found in the contiguous United States is represented in the analysis.
Our second contribution rests with the exploration of the association of concentrations of Blacks in a county with income inequality and total mortality rates. When levels of income inequality, per capita income, and household size are controlled for, counties with higher concentrations of Blacks have higher mortality rates. These results do not necessarily indicate that higher mortality in counties with high concentrations of Blacks results from higher mortality among Blacks. This is one possible explanation, supported by individual-level studies showing that racial differences in mortality can be partially attributed to variations in lifestyle, health, and cultural and socioeconomic status between Whites and Blacks. An alternative explanation is that all residents in these areas have higher mortality because they face poorer availability of services or experience other stresses related to living in an area with high concentrations of minorities.9,10
Standardizing the county mortality rate for the effects of racial composition provided a more stringent test of whether concentrations of Blacks are associated with mortality rates. With adjustments to the dependent variable for race, as well as for age and sex, the influence of minority concentration on mortality rates operated through the race-specific mortality rates or through the pathways of underinvestment in infrastructure. In addition, feelings of relative deprivation exacerbated by a county containing high concentrations of minorities may have exerted an effect. When income inequality and per capita income levels are controlled for, a higher percentage of Blacks in a county was associated with greater mortality.
Most interesting in this analysis, however, was that adding the percentage of Blacks eliminated the income inequality gradient in mortality for the highest levels of inequality. The interaction between percentage of Blacks and income inequality that this result suggests was substantiated in the analysis, indicating a complex relationship between minority concentration, income inequality, and county-level mortality rates.
Including the interaction terms revealed the income inequality gradient in mortality for counties with no Blacks or a low percentage of Blacks—counties with higher income inequality had higher mortality rates. The pattern was reversed among counties with relatively high minority concentrations; here, counties with low levels of income inequality had the highest mortality rates, while counties with the highest levels of income inequality had the lowest mortality rates.
Counties with high concentrations of Blacks and low income inequality may have limited class distinctions and, most likely, low income levels. While county per capita income is controlled in the model, it may be inadequate to capture the historical underinvestment in services and infrastructure that may have occurred in these counties.26,28,42,43 In addition, the control for per capita income does not reflect the substantial differences in wealth between Whites and Blacks.25 Differences in behavior and lifestyle undoubtedly account for some of the elevated mortality in counties with extremely high concentrations of minorities. Because we used county-level data and an ecologic analysis, we were unable to determine how individual mortality risks are affected by incomes or by behavioral and lifestyle factors, nor to determine whether Blacks have higher mortality than Whites. We were able to assess how county-level attributes (e.g., per capita income, percentage of Blacks, income inequality) are associated with population-based, county-level total mortality rates.
The mechanisms that operate to explain the lower mortality rates in counties with high income inequality and high concentrations of Blacks may reflect the historic location of Blacks in rural counties of the Southern Black Belt.42 These counties may have Black populations that are sufficiently large to suggest the existence of a Black middle class, which may provide a base for political accountability and action35 and increased social cohesion in the Black community. Both of these have been associated with lower mortality.9,44 Ethnic and racial enclave communities of sufficient size may help generate a sense of community and self-sufficiency and lessen feelings of relative deprivation.9,45 The presence of a middle class or upper class also may increase investment in infrastructure, as suggested in theoretic models relating income inequality and mortality. These explanations of the pattern of interactions are speculative. The level of income inequality within ethnic enclave communities, the cultural, lifestyle, and health risk behaviors in these communities, and their relationship with mortality have not been examined. More intensive study of particular types of communities (e.g., those with high concentrations of minorities) would contribute to explaining these relationships.
These findings do not undermine the importance of the linkage between income inequality and mortality at the ecologic level; rather, they suggest a need for a better understanding of the pathways through which income inequality and mortality are related. Explaining how and why this occurs is critical to our understanding of the basic relationship between the many dimensions of inequality and mortality. Identifying the community-level pathways through which income inequality influences mortality provides policymakers at local, state, and federal levels with more explicit targets for policy intervention at the community level, targets that may be more politically feasible than the redistribution of income from the wealthy to the poor and the middle class.
Acknowledgments
Support for this research was provided by Agricultural Experiment Station Project 3692 in the College of Agricultural Sciences at the Pennsylvania State University and by the Population Research Institute, the Pennsylvania State University, which has core support from the National Institute of Child Health and Human Development (P30 HD28263).
We would like to thank Don Gensimore for his assistance in preparing the data from the Compressed Mortality Files. We acknowledge the helpful comments of the reviewers.
Peer Reviewed
References
- 1.Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87:1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Massey DS. The age of extremes: concentrated affluence and poverty in the twenty-first century. Demography. 1996;33:395–412. [PubMed] [Google Scholar]
- 3.Kaplan GA, Pamuk ER, Lynch JW, Cohen RD, Balfour JL. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. BMJ. 1996;312:999–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kawachi I, Kennedy BP. The relationship of income inequality to mortality: does the choice of indicator matter? Soc Sci Med. 1997;45:1121–1127. [DOI] [PubMed] [Google Scholar]
- 5.Lynch JW, Kaplan GA, Pamuk ER, et al. Income inequality and mortality in metropolitan areas of the United States. Am J Public Health. 1998;88:1074–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fiscella K, Franks P. Poverty or income inequality as predictor of mortality: longitudinal cohort study. BMJ. 1997;314:1724–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daly MC, Duncan GJ, Kaplan GA, Lynch JW. Macro-to-micro links in the relation between income inequality and mortality. Milbank Q. 1998;76:315–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Massey DS, Denton NA. American Apartheid: Segregation and the Making of the Underclass. Boston, Mass: Harvard University Press; 1993.
- 9.LaVeist TA. Segregation, poverty and empowerment: health consequences for African Americans. Milbank Q. 1993;71:41–64. [PubMed] [Google Scholar]
- 10.Jackson SA, Anderson RT, Johnson NJ, Sorlie PD. The relation of residential segregation to all-cause mortality: a study in Black and White. Am J Public Health. 2000;90:615–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levy F. New Dollars and Dreams: American Incomes and Economic Change. New York, NY: Russell Sage Foundation; 1998.
- 12.LeClere FB, Rogers RG, Peters KD. Ethnicity and mortality in the United States: individual and community correlates. Soc Forces. 1997;76:169–198. [Google Scholar]
- 13.Manton KG, Patrick C, Johnson K. Health differentials between Blacks and Whites: recent trends in mortality and morbidity. Milbank Q. 1987;65:129–199. [PubMed] [Google Scholar]
- 14.Menchick PL. Economic status as a determinant of mortality among Black and White older men: does poverty kill? Popul Stud. 1993;47:427–436. [Google Scholar]
- 15.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol. 1995;21:349–386. [Google Scholar]
- 16.Hummer RA. Black–White differences in health and mortality: a review and conceptual model. Sociol Q. 1996;37:105–125. [Google Scholar]
- 17.Kabat GC, Morabia A, Wynder EL. Comparison of smoking habits of Blacks and Whites in a case–control study. Am J Public Health. 1991;81:1483–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Otten MW, Teutsch SM, Williamson DF, Marks JS. The effect of known risk factors on the excess mortality of Black adults in the United States. JAMA. 1990;263:845–850. [PubMed] [Google Scholar]
- 19.Wilkinson KP. The Community in Rural America. New York, NY: Greenwood; 1991.
- 20.Wilkinson RG. The epidemiological transition: from material scarcity to social disadvantage? Daedalus. 1994;123:61–77. [PubMed] [Google Scholar]
- 21.Evans RG, Barer ML, Marmor TR, eds. Why Are Some People Healthy and Others Not? New York, NY: Aldine de Gruyter; 1994.
- 22.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;(extra issue):80–94. [PubMed]
- 23.Lynch JW, Kaplan GA. Understanding how inequality in the distribution of income affects health. J Health Psychol. 1997;2:297–314. [DOI] [PubMed] [Google Scholar]
- 24.Neser WB, Tyroler HA, Cassel JC. Social disorganization and stroke mortality in the Black population of North Carolina. Am J Epidemiol. 1971;93:166–175. [DOI] [PubMed] [Google Scholar]
- 25.Robert SA. Socioeconomic position and health: the independent contribution of community socioeconomic context. Annu Rev Sociol. 1999;25:489–516. [Google Scholar]
- 26.Colclough G. Uneven development and racial composition in the deep South: 1970–1980. Rural Soc. 1988;53:73–86. [Google Scholar]
- 27.Colclough G. Industrialization, labor markets and income inequality among Georgia counties: 1970–1980. Res Rural Soc Dev. 1989;4:207–222. [Google Scholar]
- 28.Ramsey M. Community, Culture and Economic Development: The Social Roots of Local Action. Albany: State University of New York Press; 1996.
- 29.Zekeri A. Community action in Alabama's Black Belt timber-dependent communities. Soc Ind Res. 1997;39:203–228. [Google Scholar]
- 30.Garofalo G, Fogarty MS. Urban income distribution and the urban hierarchy–equality hypothesis. Rev Econ Stat. 1979;61:381–388. [Google Scholar]
- 31.Beggs JJ, Villemez WJ, Arnold R. Black population concentration and Black–White inequality: expanding the consideration of place and space effects. Soc Forces. 1997;76:65–92. [Google Scholar]
- 32.Grant DS II, Parcel TL. Revisiting metropolitan racial inequality: the case for a resource approach. Soc Forces. 1990;68:1121–1142. [Google Scholar]
- 33.Tienda M, Lii D. Minority concentration and earnings inequality: Blacks, Hispanics, and Asians compared. Am J Sociol. 1987;93:141–165. [Google Scholar]
- 34.Sorlie P, Rogot E, Anderson R, Johnson NJ, Backlund E. Black–White differences by family income. Lancet. 1992;340:346–350. [DOI] [PubMed] [Google Scholar]
- 35.Duncan CM. Worlds Apart: Why Poverty Persists in Rural America. New Haven, Conn: Yale University Press; 1999.
- 36.Soobader M, LeClere FB. Aggregation and the measurement of income inequality: effects on morbidity. Soc Sci Med. 1999;48:733–744. [DOI] [PubMed] [Google Scholar]
- 37.Tolbert CM, Lyson TA. Earnings inequality in the nonmetropolitan United States: 1967–1990. Rural Soc. 1992;57:494–511. [Google Scholar]
- 38.Shryock HS, Siegel JS. The Methods and Materials of Demography. Vol 1. Washington, DC: US Government Printing Office; 1971.
- 39.Census of Population and Housing, 1990 (United States): Summary Tape File 3C [computer file]. Washington, DC: Bureau of the Census; 1991.
- 40.Allison PD. Measures of inequality. Am Sociol Rev. 1978;43:865–880. [Google Scholar]
- 41.Braun D. Multiple measures of US income inequality. Rev Econ Stat. 1988;70:398–405. [Google Scholar]
- 42.Falk WW, Talley CR, Rankin BH. Life in the forgotten South: the Black Belt. In: Lyson TA, Falk WW, eds. Forgotten Places: Uneven Development in Rural America. Lawrence: University of Kansas Press; 1993:53–75.
- 43.Hylund S, Timberlake M. The Mississippi Delta: change or continued trouble. In: Lyson TA, Falk WW, eds. Forgotten Places: Uneven Development in Rural America. Lawrence: University of Kansas Press; 1993:76–101.
- 44.Egolf B, Lasker J, Wolf S, Potvin L. The Roseto effect: a 50-year comparison of mortality rates. Am J Public Health. 1992;82:1089–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Portes A, Jensen L. What's an ethnic enclave? The case for conceptual clarity. Am Sociol Rev. 1987;52:768–769. [Google Scholar]