Abstract
Purpose
Anisometropia is a common cause of amblyopia. The relationship between anisometropia, patient age, and the development of amblyopia is unknown. Photoscreening identifies children with anisometropia in a manner that is not biased by visual acuity and allows a unique opportunity to evaluate how patient age influences the prevalence and depth of anisometropic amblyopia.
Methods
A statewide preschool photoscreening program screened 120,000 children and identified 792 with anisometropia greater than 1.0 diopter. Age was correlated with visual acuity and amblyopia depth. Data were compared with those from 562 strabismic children similarly identified.
Results
Only 14% (6/44) of anisometropic children aged 1 year or less had amblyopia. Prevalence was 40% (32/80) for 2-year-olds, 65% (119/182) for 3-year-olds, and peaked at 76% (age 5). Amblyopia depth also increased with age. Moderate amblyopia prevalence was 2% (ages 0 to 1), 17% (age 2), and rose steadily to 45% (ages 6 to 7). Severe amblyopia was rare prior to age 4, 9% at age 4, 14% at age 5, and 9% at ages 6 to 7. In contrast, children with strabismus had a stable prevalence of amblyopia (30% at ages 0 to 2, 42% at ages 3 to 4, 44% at ages 5 to 7).
Conclusions
Younger children with anisometropic refractive error have a lower prevalence and depth of amblyopia than do older children. By age 4, when most children undergo traditional screening, amblyopia has usually already developed. New vision screening technologies that allow early detection of anisometropia provide ophthalmologists an opportunity to intervene early, perhaps retarding, or even preventing, the development of amblyopia.
INTRODUCTION
Amblyopia is derived from the Greek word amblyos, meaning dull, and opia, meaning vision. It refers to a decrease in best-corrected visual acuity in an eye having no organic pathology.1 Amblyopia is primarily a cortical phenomenon, caused by unequal competitive inputs from the two eyes into primary visual cortex area 17, although additional structural and functional abnormalities have been observed in the lateral geniculate nucleus of amblyopic animals and humans1 (see “Background” section for review).
During the last decade, new techniques for preschool vision screening have become increasingly commonplace. These allow early detection of children who have amblyopia. Unlike traditional optotype tests, which evaluate acuity or visual function directly, these new techniques identify problems that are associated with the development of amblyopia, rather than amblyopia itself. Photoscreening, noncycloplegic autorefraction, and the other new techniques detect high refractive errors (myopia, astigmatism, and hyperopia), anisometropia, media opacities, and ocular misalignment. These abnormalities are collectively referred to as amblyopiogenic factors. A rationale for the implementation of these technologies is that earlier detection and treatment of amblyopiogenic factors may reduce or prevent amblyopia, but no data exist to support this notion.
There are at least two potential problems that limit the usefulness of technologies that detect amblyogenic factors. The first is that they do not directly detect amblyopia. Instead, they detect levels of refractive error and ocular misalignment that are known to be associated with amblyopia development. Because the levels of refractive error that produce amblyopia in each individual are highly variable (many patients with moderate anisometropia may never develop amblyopia, whereas others with only mild anisometropia can have significant amblyopia), photoscreening by necessity overdetects children and therefore refers some of them unnecessarily.
Another problem with this new technology is that the natural history of an identified amblyopiogenic factor in a child who has good vision is unknown, because such patients have never been studied. A child who has an amblyogenic factor at age 2 may not have any problem at age 4. Thus, it is unclear whether or not early screening using the new techniques, with the resultant earlier detection and treatment of amblyopia, provides any additional advantage over waiting until visual acuity can be tested directly.
During the past decade, this author has had the opportunity to examine many children referred from photoscreening programs, both volunteer-led and from physician offices. Many of these children, especially very young ones, often have good visual acuity despite high levels of anisometropia. However, older children with anisometropia often have amblyopia. This is in contrast to my experience prior to the introduction of photoscreening, when most anisometropic children had amblyopia, and it was often severe. It was unclear if this difference represented a sampling bias, whereby anisometropic children without amblyopia had not been previously detected (and therefore not examined), or if amblyopia developed very early in anisometropic children, prior to the age where they could be screened using traditional techniques. This was the rationale for performing this study
The overall aim of this thesis is to test the hypothesis that anisometropic amblyopia develops as a function of the duration of anisometropia (ie, the age of the patient). If it can be demonstrated that older patients with anisometropia are more likely to have amblyopia than younger ones, or to have more severe amblyopia, then support could be provided for early screening, because the earlier treatment afforded by early screening could potentially prevent the development of amblyopia in at-risk patients. If, however, the prevalence and depth of anisometropic amblyopia are independent of age, then the extra time and expense associated with earlier vision screening are not warranted. To test this hypothesis, data obtained from a statewide photoscreening program for preschool children were examined. This program has been developed and previously validated. This study examines the visual acuity results from children referred following photoscreening, examined formally, and found to have anisometropia.
BACKGROUND
AMBLYOPIA: THE NATURE OF THE PROBLEM
Amblyopia is a significant public health problem. It is the leading cause of monocular vision loss in young and middle-aged Americans.2,3 Having amblyopia increases the risk of vision loss in the fellow eye.4–6 Amblyopia is also associated with decreased financial productivity during a lifetime; a recent study by Membreno and colleagues7 demonstrated that treating amblyopia is cost-effective compared with most ophthalmologic and nonophthalmologic medical treatments.
There are three primary types of amblyopia: anisometropic, strabismic, and deprivation. Anisometropic amblyopia occurs in children having a difference in refractive error between the eyes, typically hyperopia or astigmatism, and occurs in the more ametropic eye. In this study, anisometropia refers to a difference in refractive error between the eyes, in any meridian, of greater than 1.0 diopter. Strabismic amblyopia results from ocular misalignment, typically esotropia. Deprivation amblyopia is produced by media opacities such as cataract, corneal opacities, and vitreous hemorrhage, and is typically the most severe form. Anisometropic, strabismic, and deprivation amblyopia are all associated with a decrease in best-corrected visual acuity in one eye. Anisometropia was the cause of amblyopia in 37% of the 409 patients enrolled into the recent, large, prospective, multicenter Amblyopia Treatment Study 1 (ATS 1).8 Strabismus was the etiology in 38%, and a combination of anisometropia and strabismus was seen in 24%. Bilateral amblyopia, caused by high refractive error, can also occur, and is called isoametropic amblyopia, but is beyond the scope of this paper. Bilateral amblyopia can also be caused by deprivation in both eyes, when media opacities are bilateral.
A unifying facet of all forms of amblyopia is a critical period (or “sensitive period”),9 during which the afferent visual system is considered relatively plastic and is capable of rearranging synaptic connections based upon the relative strength of afferent inputs from each eye. This plasticity extends for a variable period, depending upon the type and severity of the amblyopia, and is thought to be the physiologic basis for improvement in visual acuity during amblyopia treatment. Classic teaching is that amblyopia must be detected early and the pathology (strabismus, media opacity, or asymmetric refractive error) must be addressed prior to beginning treatment for amblyopia.1 Afferent inputs from the affected eye are then reestablished or strengthened by using patching, atropine, or other forms of penalization of the fellow eye. An overwhelming body of evidence has been accumulated over the last 5 years to demonstrate that amblyopia does not typically resolve without treatment10 and that amblyopia treatment is extremely effective in restoring vision.11–15
During the last decade, the detection and treatment of amblyopia have received increased emphasis. Amblyopia has been recently targeted by Healthy People 2000 as an important disease to detect. There is increased interest in detecting amblyopia, as evidenced by the multicentered, National Eye Institute–funded Vision in Preschoolers (VIP) study.16 Finally, the Pediatric Eye Disease Investigative Group has initiated and completed several multicentered controlled clinical trials evaluating different treatments for amblyopia.11–15
Despite improved understanding of the causes of amblyopia, and the recognized importance of treating amblyopia at an early stage, much controversy exists regarding the best methods to detect amblyopia. In literate children, adolescents, and adults, visual acuity can be tested directly by using traditional techniques, such as Snellen letters, ETDRS letters, or other optotype-based acuity charts. Amblyopia is much more difficult to detect at younger ages, however, because such children are not literate and cannot read eye charts. Screening techniques for visual acuity assessment in the preliterate child that do not rely on direct assessment of acuity are difficult to teach, difficult to learn, and difficult to validate. These techniques, such as forced-choice preferential looking and sweep VEP, rely upon highly skilled professionals and are therefore limited to laboratory testing. Clearly, there are not enough adequately trained individuals to test visual function using such methods on each of the 4 million US children born each year.
The increasing recognition of amblyopia as a significant public health problem in the developed world has produced an increased desire to identify children early. New technology that screens younger children has had preliminary validation and is becoming more widely utilized. There are no data, however, to suggest that earlier detection of at-risk children can prevent amblyopia development, by allowing earlier treatment. This thesis seeks to test that notion.
THE UNKNOWN NATURAL HISTORY OF ANISOMETROPIA
The natural history of uncorrected anisometropia is unknown. Specifically, the prevalence of anisometropia at various ages, the natural history of treated and untreated eyes, vis-à-vis changes in the amount of anisometropia over time, and factors that predispose the anisometropic eye to become amblyopic are not well established. Most previous studies of anisometropic children select patients who have anisometropia in association with amblyopia. The advent of photoscreening allows a unique opportunity to study asymptomatic children with anisometropia from large populations without bias, because photoscreening detects children without respect to their visual acuity. Therefore, one can evaluate visual function in children identified by photoscreening to determine how anisometropia perturbs the afferent visual system during childhood.
The remainder of this section examines the literature evaluating the prevalence of anisometropia and anisometropic amblyopia, the risk factors for developing amblyopia, and the clinical and laboratory characteristics of anisometropic amblyopia in humans and nonhuman mammals. Putative mechanisms underlying the development of amblyopia are also studied.
PREVALENCE OF ANISOMETROPIA, ANISOMETROPIC AMBLYOPIA, AND THE NATURAL HISTORY OF ANISOMETROPIC REFRACTIVE ERROR
Clinical and epidemiologic studies have assessed the prevalence of anisometropia and anisometropic amblyopia. Some studies report the prevalence of anisometropia, whereas others report the prevalence of anisometropic amblyopia. Many of these studies are subject to selection bias, especially those from a clinical setting, because many children with anisometropia do not develop amblyopia, do not present for treatment, and therefore are not included in the study. A summary of prevalence data from many large studies is seen in Table 1. Similar studies have been summarized by Saunders.17
TABLE 1.
PUBLISHED STUDIES OF THE PREVALENCE OF ANISOMETROPIA AND AMBLYOPIA
| AUTHOR | POPULATION | n | TECHNIQUE | PREVALENCE ANISOMETROPIA | PREVALENCE ANISOMETROPIC AMBLYOPIA | % PREVALENCE OF AMBLYOPIA* |
|---|---|---|---|---|---|---|
| Atkinson and Braddick18 | Infants (6 to 9 months) | 1,096 | Photorefraction | 1.3% | — | — |
| DeVries (1985)139 | Elementary school students | 1,356 | Children in hospital population | 2.0% (26/1,356) | 1.30% (17/1,356) | 67% (17/26) |
| Almeder et al 21 | Children (3 months to 9 years) | 686 | Examination | 2.8% | — | — |
| Abolfotouk (1994)140 | Elementary school students (male) | 971 | School examination | — | <1.00% | 27% |
| Attebo (1998)141 | Australian adults (over 49 years) | 3,654 | Examination | — | 1.60% | — |
| Lithander (1998)142 | Primary school students | 6,292 | Acuity screening | — | 0.44% | — |
| Yamashita et al (1999)22 | Japanese school children (6 to 11 years) | 350 | Cycloplegic refraction | 4.3% | — | — |
| Brown (2000)143 | Australian adults (40 to 92 years) | 4,721 | Examination | — | 1.50% | — |
| Quek et al(2004)26 | Singapore students (15 to19 years) | 946 | Noncycloplegic autorefraction | 11.2% | — | — |
| Tong et al (2004)144 | Singapore students (7 to 9 years) | 1,979 | Noncycloplegic autorefraction | 1.6% | — | — |
| Mayer et al (2001)145 | Healthy infants (1 to 48 months) | 514 | Cycloplegic retinoscopy | 1.0% | — | — |
Prevalence of amblyopia in subjects with known anisometropia.
The prevalence of anisometropia at various ages averages approximately 2% (range, 1% to 11%). Atkinson and Braddick18,19 demonstrated that fewer than 1.5% of infants (6 to 9 months of age) showed anisometropia greater than or equal to 1.5 diopters. However, a PhD thesis by Thompson20 found that cycloplegic retinoscopy was able to demonstrate anisometropia of greater than 1.0 diopter in over 14% of newborn infants. Many other prevalence studies have been performed, but they vary widely depending upon the population age, the technique for determining the refractive error, and the definition of anisometropia.
Anisometropic amblyopia is less common than anisometropia and typically affects less than 1.5% of the population (Table 1). Prevalence studies of anisometropic amblyopia have biases similar to those of anisometropia. The prevalence of anisometropic amblyopia in patients with anisometropia is probably in the neighborhood of 25% to 60%. Hence, not all patients with anisometropia develop amblyopia.
The natural history of anisometropic refractive error, especially in young children, is not well established. An anisometropic child’s refractive error can change substantially over time. Almeder and colleagues21 followed 19 anisometropic subjects (2.8% of 686 volunteer infants). He found that at least 11 had the anisometropia resolve. Yamashita and associates22 found that 15.7% of 350 rural Japanese children had a significant change in the amount of anisometropia with age, that up to 3.1% developed greater than 1.0 diopter spherical anisometropia, and up to 4.3% developed greater than 1.0 diopter of cylindrical anisometropia. Abrahamsson and colleagues23 longitudinally followed 310 children with astigmatism during 3 years from age 1 to 4. Although the prevalence of superimposed anisometropia remained relatively constant at approximately 11%, fewer than one half of the children with anisometropia present at age 1 still had the anisometropia present at age 4. Children with persistent anisometropia developed amblyopia in approximately 25% of cases. The resolution of anisometropic refractive error in many individuals may account for the clinical observation that some older patients with amblyopia seem to have no identifiable etiology for their unilateral decrease in vision; previous anisometropia may have produced the amblyopia prior to resolving. Thus, it appears that transient anisometropia is common and may not produce amblyopia in all young children, whereas persistent anisometropia may create a substantial risk of amblyopia.
After visual maturity, anisometropia may still develop, even in healthy eyes. A meta-analysis by Weale24 demonstrates that the prevalence of anisometropia in patients without amblyopia increases linearly, approximately 1%, for each 7-year period. A trend for increasing anisometropia with age is also supported by studies of Bourne and colleagues25 and Quek and associates.26 The reason for the development of anisometropia in some adult eyes is unclear, but Almeder and colleagues have suggested that much anisometropia observed in adults is actually not the cause, but instead may be the result, of preexisting amblyopia.21 It therefore appears that prevalence data from adults should not be extrapolated to children.
RISK FACTORS FOR DEVELOPING AMBLYOPIA IN ANISOMETROPIC CHILDREN
For years, the most important factor in determining the depth of anisometropic amblyopia was thought to be the magnitude of anisometropia. Lyle,27 in Worth and Chavasse’s Squint, postulated such a relationship. This has become more controversial since then. Helveston28 could not find any such relationship in a study of 57 patients of various ages. Helveston’s subjects all had amblyopia, however, and adults (who may have had a change in anisometropia over time) were included. Nevertheless, it had been thought that the increasing blur that occurs with an increased degree of anisometropia causes the afferent inputs to the primary visual cortex from the more anisometropic eye to be relatively less robust, and this results in amblyopia. We now recognize that additional factors, other than blur, must play a role in causing amblyopia. Some children with only mild anisometropia develop severe amblyopia, whereas others tolerate significant anisometropia without developing amblyopia. Dadeya and colleagues29 have demonstrated that normal individuals, with induced anisometropia, have a deterioration in binocular vision with increasing levels of anisometropia, and this may determine which eyes become amblyopic.
Anisometropia of 1.0 diopter appears to be the threshold for developing amblyopia. Ingram and Walker30 found that patients having 1.0 diopter or more of anisometropia had a slight increase in risk for the development of strabismus or amblyopia in a case-control sibling study. Latvala and coworkers31 also demonstrated anisometropia of 1.0 diopter or more to be a risk factor for the development of amblyopia in a study of 109 amblyopic patients.
The magnitude of anisometropia probably does influence the development of amblyopia,32 despite the early findings of Helveston.28 In a large clinic-based study of 167 anisometropes (>2.0 diopters) in Thailand and 472 anisometropes (>1.0 diopter) in Indiana, 100% of children with hyperopic meridional anisometropia greater than or equal to 3.5 diopters developed amblyopia, whereas the prevalence of amblyopia was less for lower degrees of anisometropia.33 Similar results were reported by Sen,34 although this was probably a republication of the Thailand clinic population data reported above. Rutstein and Corliss35 found the depth of amblyopia in 60 untreated anisometropic amblyopes to be related to the degree of anisometropia. A study of 67 patients by Kivlin and Flynn36 reported a similar relationship, as did studies by Townshend and colleagues37 and by Dolezalova.38 Kutschke and colleagues39 could not find a relationship between magnitude of anisometropia and amblyopia depth in a retrospective study of 124 children, but most of her patients had good acuity, limiting the ability to find differences. The above retrospective studies thus provide weak support for the concept that higher-magnitude anisometropia is a significant risk factor for the development of amblyopia.
Longitudinal studies of anisometropic children have provided more robust support for this concept. Further analysis of 20 of the anisometropic children in the cohort reported originally by Abrahamsson and colleagues23 demonstrated that (1) 60% of children with anisometropia greater than 3 diopters developed amblyopia, (2) an increasing amount of anisometropia over time was associated with amblyopia development in all cases, and (3) 90% of children with anisometropia greater than 3 diopters at 1 year of age had at least that amount at age 10 years.32 It is therefore likely that increasing anisometropia is also a risk factor for amblyopia and that increasing and high levels of anisometropia should be treated early.
It is unclear from the Abrahamsson studies23 if early treatment of observed anisometropia would prevent the amblyopia from developing or reduce the amount of anisometropia. It is possible that the increase in anisometropia observed in these children may either be in some way related to amblyopia that has already occurred, or be due to another unobserved abnormality that predisposes the eye to develop amblyopia and then anisometropia. These scenarios were raised by Fielder in an editorial highlighting the Abrahamsson and Sjostrand article.40 Another study supporting the notion that amblyopia precedes anisometropia development demonstrated that the magnitude of anisometropia appears to increase in strabismic patients who have a fixation preference for one eye.41 Lepard42 and Nastri and associates43 have shown that the refraction of the fixating eye becomes more myopic, whereas the amblyopic eye remains hypermetropic, furthering the notion that amblyopia leads to anisometropia, at least in some individuals.
In addition to persistent or increasing anisometropia, and large-magnitude anisometropia, age is also important in determining which anisometropic children develop amblyopia. A delayed age at presentation is usually seen in patients with anisometropic compared with other types of amblyopia. Only 15% of anisometropic amblyopia was identified prior to the age of 5 years during a 4-year study in Leicestershire.44 Woodruff and associates45 found that the age of presentation for patients with anisometropic amblyopia (5.6 years) was much greater than that for patients with other types of amblyopia. Chua and colleagues46 found that patients with pure anisometropic amblyopia were identified the latest of all patients with amblyopia. There are two possible explanations for these observations. First, it could simply be a sampling bias, that is, the other types of amblyopia are usually associated with a cosmetically noticeable strabismus, which drives care, whereas anisometropic patients present later because there is no identifiable defect. Alternatively, since anisometropic patients are older at presentation, it may be that anisometropia takes time to produce amblyopia.
The relationship between anisometropia, subnormal binocularity, and the development of amblyopia has been best studied by Weakley.47,48 His excellent studies have evaluated patients who were examined in a pediatric ophthalmology clinic and found to have anisometropia, or anisometropic amblyopia. Like all of the above clinic-based studies, they suffer from a selection bias, because they tend to include only those patients referred on account of decreased acuity, or found to have anisometropia on an examination spurred by a family history of an eye problem (D. R. Weakley, oral communication, 2004). Therefore, those patients having anisometropia without amblyopia or strabismus, and those with mild anisometropic amblyopia, are likely to be underrepresented. Nevertheless, Weakley’s conclusions provide significant insights into the development of amblyopia. His study of 411 patients with varying levels of anisometropia demonstrated an increased risk of amblyopia once spherical hypermetropic anisometropia exceeded 1 diopter.47 Increasing levels of spherical hypermetropic anisometropia beyond this threshold were also associated with an increasing depth and prevalence of amblyopia. Similar results were seen with spherical myopic anisometropia of greater than 2 diopters, although the sample size was much smaller.
Weakley and associates49,50 also studied the effect of anisometropia on the development and breakdown of accommodative esotropia. In this evaluation of 345 patients, anisometropia greater than or equal to 1 diopter increased the risk of developing accommodative esotropia. It also increased the risk that a nonaccommodative esodeviation would develop and was the only risk factor found for the development of a nonaccommodative esotropia in patients with low levels of hypermetropia. Although this study was also biased by the lack of inclusion of patients with anisometropia and good acuity, it still conclusively demonstrates the powerful effect of anisometropia on the development of esotropia and amblyopia.
Therefore, it appears clear that anisometropia greater than 1.0 diopter is a threshold for amblyopia development. In addition, increasing levels of anisometropia, high levels of anisometropia, and persistent anisometropia in older children are all associated with amblyopia. However, it remains unclear if one can prevent amblyopia by optically correcting anisometropia at an early age.
MECHANISMS RESPONSIBLE FOR THE DEVELOPMENT OF AMBLYOPIA IN PATIENTS WITH ANISOMETROPIA
Anisometropia may produce amblyopia by causing a loss of foveal resolution in the less focused eye, by localized mechanisms of foveal inhibition (development of a suppression scotoma), or by loss of stereo acuity and binocular function (perhaps caused by loss of resolution or by a suppression scotoma). There is support for each of these mechanisms in the literature. Studies of normal human subjects have demonstrated that induced anisometropia greater than 1 diopter causes abnormalities in resolution and induction of a suppression scotoma.51 Larger magnitudes of simulated anisometropia in normal subjects produce larger suppression scotomas,52 suggesting that foveal suppression in the defocused eye may be the cause of decreased stereopsis. A similar impact of increasing levels of induced anisometropia on stereopsis and binocular vision has also been demonstrated.53,54 However, these studies were performed on adults with normal binocular vision, who had anisometropia induced optically. Therefore the results may not be transferable directly to patients with naturally occurring anisometropia.
Studies of adults having anisometropia have tended to confirm these mechanisms. Tomac and Birdal55 evaluated binocular visual function and fusion in 25 anisometropic adults and found that amblyopia depth was more related to a deterioration in binocularity than to the magnitude of the anisometropia. This suggests that a suppression scotoma, rather than induced blur, may be responsible for the production of amblyopia. Holopigian and colleages56 evaluated stereoacuity and binocular summation (the improvement in one eye’s detection performance when a subthreshold pattern is presented to the fellow eye) in adult anisometropic amblyopes. Anisometropic amblyopes had normal summation and normal stereoacuity at low spatial frequencies (large separation between objects) of contrast. However, at high spatial frequencies (minimal separation between contrasted objects), summation was absent and stereopsis was nil. Stereoacuity was subnormal at intermediate spatial frequencies. This suggests that anisometropia affects both stereopsis and summation.
Behavioral studies of monkeys have confirmed some of the observed human findings. Monkeys reared with alternating monocular defocus have demonstrated that clinical suppression can occur with as little as 1.5 diopters of anisometropia and that the severity of the suppression correlates with the magnitude of the anisometropia.57 Likewise, a relationship between the degree of anisometropia induced by unilateral optical defocus in macaque monkeys correlates with the degree of amblyopia.58
The available human and animal studies therefore support the notion that monocular blur in anisometropic individuals leads to reduced binocular stereoacuity, a suppression scotoma, and amblyopia development.
CHARACTERISTICS OF ANISOMETROPIC AMBLYOPIA
Psychophysical Testing
The primary psychophysical defect observed in patients with anisometropic amblyopia is in high spatial frequency contrast sensitivity. The resolution necessary for best-corrected visual acuity represents high contrast (between the letters and their surround) at high spatial frequencies (closeness of letters). Bradley and Freeman59 tested 10 patients with anisometropic amblyopia and found that their greatest defect was at high spatial frequencies. At low spatial frequencies, there were only small differences between the eyes, which could be accounted for by optical magnification differences caused by the anisometropia. The intereye difference in spatial frequency contrast sensitivity in patients with anisometropic amblyopia correlates with the magnitude of anisometropia.59 The observation that anisometropic amblyopia is associated primarily with loss of high spatial frequency contrast sensitivity, with resultant defects in steroacuity and summation, has also been demonstrated by other investigators.56,60,61
The high spatial frequency contrast sensitivity defects in anisometropic amblyopes are important clinically. Friendly and colleagues62 tested the visual acuity of 32 orthotropic anisometropic amblyopic children using Teller visual acuity tests and compared them to the results of acuity testing using Bailey-Lovie-Ferris charts. They found that anisometropic amblyopes are often inaccurately found to be normal when tested using Teller visual acuity cards alone, possibly because Teller acuity is generally a low spatial frequency test at the attention level typical for very young children.
In marked contrast to anisometropic patients, those having strabismic amblyopia and those with a combination of strabismic and anisometropic amblyopia have other defects, primarily in localization, that appear to be independent of contrast sensitivity.61 The prevalence of anisometropia or strabismus as the underlying etiology appears to play a role in which type of deficit is present. Contour information is abnormal primarily in strabismic, but not anisometropic, amblyopia.63 However, this is controversial, and some studies of untreated orthotropic anisometropic amblyopes have demonstrated contour integration deficits.63 Strabismic and anisometropic amblyopia can also be distinguished by the longer interocular increment time in strabismic patients compared to anisometropes with respect to reaction time.64 Clinically, the differences between anisometropic amblyopia and strabismic amblyopia include differences in resolution/vernier acuity and recognition/resolution acuity ratios in the two groups.65
Hardman Lea recently demonstrated that approximately 45% of anisometropic amblyopes have a microtropia rather than bifoveal fixation.66 However, it is unclear whether the lack of bifoveal fixation is caused by the secondary amblyopia, or if the anisometropia itself produces a microtropia by limiting monocular function in the more hypermetropic eye.
Findings in Animals With Experimentally Induced Anisometropic Amblyopia
Behavioral observations in nonhuman primates reared with experimentally induced amblyopia are similar to those seen in humans. Monkeys reared with anisometropia caused by defocusing myopic contact lenses have spatial frequency-selective deficits in stereopsis, and in contrast sensitivity, that depend upon the degree of the anisometropia.67 Similar defects are seen in grating acuity.68 These results correlate with anatomic abnormalities in the dorsal lateral geniculate nucleus,68 where laminae innervated by the deprived eye show a marked reduction in cross-sectional area.
Physiologic studies on the visual cortex of similarly reared primates demonstrate a decreased number of cortical cells that can be activated by the amblyopic eye. This decrease is related to the depth of the amblyopia69,70 and is seen more with anisometropia than strabismus.
Whereas classic teaching is that primates with deprivation amblyopia, produced by unilateral eye lid suture, have abnormalities in ocular dominance column size,1 this may not be true for primates with induced anisometropic amblyopia; ocular dominance columns in layer 4 C of visual cortex area 17 were normal in a naturally occurring anisometropic amblyopic macaque monkey.71 This confirms a previous anatomic study72 of a human subject with anisometropic amblyopia who also had normal ocular dominance column width. Thus, it is possible that anisometropic amblyopia may have much of its pathophysiology caused by impairments in binocular function, rather than by anatomic differences in the visual cortex.71 This may also explain why many patients who have anisometropic amblyopia respond simply to spectacles alone,73–75 and why patients with anisometropic amblyopia are more likely to improve at later periods in life.75
Laboratory Abnormalities in Anisometropic Amblyopia
Functional Magnetic Resonance Imaging (MRI).
The results from functional MRI appear to confirm previous psychophysical, electrophysiologic, and anatomic findings. Patients with anisometropic amblyopia have suppressed f-MRI-measured calcarine cortex activation primarily at higher spatial frequencies but not at lower spatial frequencies.76 A second f-MRI study showed decreased activation of the portions of the lateral geniculate nucleus and the visual cortex corresponding to the affected eye of a patient with anisometropic amblyopia.77
Visual Evoked Potentials (VEPs).
Because amblyopia is thought to result from abnormalities in the visual cortex, the VEP should be abnormal, and this has been known for years.78 The VEP abnormalities are related to the loss of high spatial frequency contrast sensitivity and can be marked in anisometropic amblyopes.79 Recent studies, however, have focused attention on the anatomic location of the VEP abnormalities. Anisometropic amblyopia is associated primarily with abnormal parvocellular rather than magnocellular visual system function,80 which is why the dorsal layers of the LGN are most abnormal.68 Parvocellular pathways tend to reflect foveal visual function and account for the relatively greater defects in central rather than peripheral visual function observed in amblyopic individuals. Not surprisingly, multifocal VEPs are attenuated most in the central region of the visual field, with less effect in the periphery.81 In contrast, patients with strabismic amblyopia, who have greater visual defects in the nasal field than the temporal field,82,83 have similar abnormalities in multifocal VEP.
Anterior Afferent Visual Pathway Abnormalities in Amblyopia
In the 1970s, Ikeda and Wright84 suggested that amblyopia may be caused by abnormalities in the anterior afferent visual pathways, rather than the visual cortex, based on studies of kittens raised with an artificially induced strabismus.80 This result cast doubt on the classic teaching that amblyopia is entirely cortical in nature.1 Recently, Lempert and Porter85 have suggested that amblyopic eyes have abnormalities in their optic disc and in axial length compared with fellow eyes, and that the difference in disc size of amblyopic eyes is not simply related to axial length.86 The presence of small relative afferent pupillary defects in amblyopic eyes,87–89 and abnormalities in pupil perimetry of amblyopic eyes,83 also suggests anterior afferent visual system involvement. Another study has demonstrated that the retinal nerve fiber layer may be abnormal in anisometropic amblyopia,90 but this has not been confirmed.91 Therefore, whether or not amblyopia may be associated with subtle abnormalities in the amblyopic eye, or pregeniculate afferent visual pathways, remains a subject of controversy.
The above clinical and experimental observations suggest that anisometropic amblyopia is caused by the prolonged effect of defocus and the resultant blur of images that fall on the fovea. This results in perturbed binocularity and abnormal high spatial frequency contrast sensitivity. An associated microstrabismus with eccentric fixation may also be an important factor. These differences can account for most of the psychophysical abnormalities seen in patients with anisometropic amblyopia. The more subtle abnormalities in lower spatial frequency contrast sensitivity are primarily due to the optical effects of the differences in refraction.61 Anisometropic amblyopia is primarily an abnormality in central (foveal) function. Strabismic amblyopia, in contrast, is related to abnormalities in localization and contour and is more full-field in nature.61 These differences likely underlie the clinical differences in treatment response between these groups.
TREATMENT OF ANISOMETROPIC AMBLYOPIA
The accepted treatment for anisometropic amblyopia consists first of correcting the refractive error, and then, if acuity is not improved, actively treating amblyopia. Treatment options for anisometropic amblyopia that still remain following a spectacle phase include atropine penalization,11,15 occlusion with patching or contact lenses,92 and combined atropine and optical therapy.93
Treatment success is likely related to the magnitude of anisometropia. Kivlin and Flynn36 found success was more likely in patients having lower amounts of hypermetropic anisometropia. Hussein and associates94 recently studied 104 children aged 3 to 8 years with anisometropic amblyopia to determine risk factors for treatment failure. Astigmatism of greater than 1.50 diopters in the amblyopic eye was associated with an adjusted relative risk of 5.78 (confidence limits, 1.27 to 26.5); however, anisometropia of 3.0 diopters or more of spherical equivalent did not appear to be a risk factor for treatment failure. Patients with treated anisometropic amblyopia appear to be more likely to deteriorate following the cessation of treatment if they have anisometropia greater than 1.75 diopters.95
The effect of age on treatment response is unclear. Cobb and associates96 studied 112 patients with anisometropic amblyopia who were treated and found that the presenting degree of anisometropia and amblyopia correlated with the final visual outcome, but that age had no effect. Kivlin and Flynn’s study of 67 anisometropic amblyopes also found that younger patients were more likely to be treated successfully.36 However, a relationship between age at presentation and final posttreatment acuity could not be confirmed in a study by Hardman Lea and associates97 of 55 children with pure anisometropic amblyopia. Age greater than 6 years was associated with a significant (4.69) relative risk (confidence limits, 1.55 to 14.2) of treatment failure in a recent study of anisometropic amblyopes by Hussein and colleagues.94 Kutschke and colleagues39 did not find a relationship between age and outcome, perhaps because 82% of their patients eventually reached 20/40 or better acuity. ATS 111 did not find an age effect, but did not include patients over age 6 years. A large study encompassing 961 patients over a 30-year period demonstrated that anisometropic amblyopia could be successfully treated in two thirds of patients and that success was related to the age at which therapy was initiated and the depth of visual loss before treatment.98 A multivariate analysis of these data demonstrated that the most important factors indicating a successful outcome were patient age and depth of vision loss before treatment began.99
In older patients, compliance with occlusion therapy appears to be related to treatment success.100,101 Hussein and colleagues94 found that poor compliance with treatment was a significant risk factor for treatment failure (relative risk, 5.47; confidence interval, 1.7 to 17.6) in a retrospective study of 104 anisometropic amblyopic children.
Recently, several case series have demonstrated that patients with anisometropic amblyopia can have successful treatment even if initiated after a child reaches age 7 years.92,102,75 Results from the prospective randomized ATS 3 study of treatment in children older than 7 years has also demonstrated that some improvement can occur in such children, especially those not having had previous treatment.103 The magnitude of improvement, however, appears to be less than that observed in younger children.
During the last few years, and as a result of the series of prospective ATS studies75 and others,73 the role of spectacles alone in improving the visual acuity of a significant number of patients with anisometropia is gaining recognition. It may be that spectacles decrease foveal blur in patients whose amblyopia is caused only by a decrease in resolution. Those who are less responsive to spectacles may have a suppression scotoma and are the ones who will eventually need occlusion or penalization. This dichotomy of mechanisms in patients with anisometropic amblyopia would reconcile the observations of the lack of anatomical changes in the lateral geniculate nucleus observed by Horton and associates71,72 with the animal studies that did show such changes.68–70 It would also explain the extended critical period for the improvement of visual acuity in many patients with anisometropic amblyopia, observed in both uncontrolled92,102 and tightly controlled studies,75,103 while explaining why other patients, especially those having had previous treatment, do not seem to improve at a later age.103
Treatment of anisometropic amblyopia can be highly successful. In ATS 1, 78% of patients with pure anisometropic amblyopia reached an outcome of 3 lines improvement or 20/30 acuity. A retrospective study by Kutschke and colleagues39 demonstrated that 82% of patients with anisometropic amblyopia of various ages had eventual visual acuities of 20/40 or better. Similar results were obtained by Beardsell and colleagues, where 95% of patients with pure anisometropic amblyopia achieved 20/30 visual acuity or better.104
As visual acuity improves in patients with anisometropic amblyopia, so does stereopsis. A study by Lee and Isenberg105 demonstrated that stereo acuity improves with improvement in visual acuity, in a significant, linear relationship. However, this study did not control for the improvement in acuity.
It should be noted that treatment of anisometropia in patients with severe anisometropic myopia and amblyopia has also been recently been attempted using refractive surgery and the excimer laser.106–108
SCREENING FOR AMBLYOPIA
Traditionally, amblyopia screening has been performed in children of literate age by direct, objective testing of visual acuity. Time-honored techniques use symbols, pictures, letters, or some other optotype, and monocular testing. Referral criteria typically are 2 or more lines of acuity difference between the eyes but vary both by age and by the organization publishing the criteria.109 Other traditional techniques screen for stereopsis, binocularity, or strabismus. Despite the time-honored nature of traditional screening, most of the techniques used for preschool vision screening are variable in their application, and none has been adequately validated in large field populations using nonprofessional screeners.110 Several of these techniques have been evaluated in the three-phase VIP study.16 However, the only optotype-based target found to be acceptable in phase 1 of the VIP study (Lea symbols) recently produced “disappointing” results111 in children under 4 years of age112 and has been shown to overestimate acuity by as much as 2 lines in amblyopia.113
Other methods of vision screening, such as noncycloplegic retinoscopy16 and forced choice preferential looking, do not require subject input. However, these screening methods are not generalizable to a population of lay screeners for widespread use in the 4 million US preschoolers born yearly and will not be further discussed. Experimental tests of binocular suppression110,114 require subject input and have yet to receive widespread acceptance.
Photorefractive vision screening has achieved widespread notoriety during the last decade.115 Photorefractive screening makes use of a flash of light from a camera, the resulting red reflex from the ocular fundus, and the Purkinje reflex from the cornea. Formal analysis of these reflexes can estimate the manifest refractive error of an eye and the ocular alignment. Most photoscreeners are either on- or off-axis. Off-axis photoscreeners are currently most popular.
The MTI photoscreener is the most widely used off-axis (eccentric) photoscreener,116–119 although other photoscreening systems have been studied and reported upon.120–124 Photorefraction is still considered to be in its infancy and is not yet well validated. The most valid concerns relate to standardization of interpretation and varying levels of sensitivity to detect low-magnitude refractive error.115,125 Experts also disagree about the magnitude of refractive error that should be detected by photoscreening; a consensus statement has recently been published in an attempt to standardize validation studies.126 Despite these concerns, photoscreening is receiving increased attention as a possible method to screen vision of preliterate children.115 Further discussion of the various types of photoscreening instruments, and their reported validation, is beyond the scope of this review.
Other new techniques of preschool vision screening include cycloplegic autorefraction (Retinomax Plus127; Welch Allyn SureSight127), noncycloplegic autorefraction (Retinomax128), video autorefraction,129 and wave-front analysis.130 Other instruments for automated preschool vision screening are in further development and will increase in availability and usability in the future.
A universal problem with all nontraditional techniques of vision screening is that none detects amblyopia directly. Instead, all rely upon the detection of amblyopiogenic factors, which are those factors most often associated with the development of amblyopia (primarily high hyperopia, anisometropia, media opacities, and strabismus). Because refractive error is highly variable in early years, and because many patients with anisometropia never develop amblyopia, the relative usefulness of such screening remains controversial. Nevertheless, if it can be demonstrated that amblyopia develops at different rates in patients as a function of age, if amblyopia can be treated more successfully at a younger age, or if amblyopia can be prevented by intervening earlier, support for such screening techniques will be garnered.
The VIP study recently evaluated several types of vision screening technologies, both traditional and contemporary, in preschool children and those enrolled in Head Start programs, in phase 1 of a three-phase study.16 All screenings were carried out by trained doctors who had experience in examining children. The MTI photoscreener, using the referral criteria described and published118 above, had a specificity of 94% with a sensitivity of 55% to detect what VIP defined as “very important” disorders, and a sensitivity of 63% to identify amblyopia.16 In the VIP, a post hoc analysis was carried out for all techniques except photoscreening, whereby the referral criteria for all the other techniques were altered to yield fixed specificities of 90% and 94%, and then reapplied to the screened population to determine sensitivity. This was apparently done in order to allow all techniques to be directly compared to one another. (The photoscreening sites were not given the opportunity to adjust their referral criteria to decrease specificity to 90%; this would have increased sensitivity.) The resultant analysis showed four techniques to have highest sensitivity. Phase 2 of the VIP study has included only those four techniques (Lea symbols, noncycloplegic retinoscopy, Welch Allen SureSight, Nikon Retinomax). It should be noted that the sensitivity of these four techniques to detect amblyopia when specificity was raised to 94% was not reported and that extrapolation of the VIP data suggests that photoscreening may have compared favorably with other techniques to detect amblyopia at 94% specificity. In addition, the legitimacy of a post hoc analysis of referral criteria is open to question, especially given the relatively small number of children in each category; whether or not such altered criteria can maintain high sensitivity when tested on another population is unclear. Finally, it should be noted that the nonautomated techniques (Lea symbols and noncycloplegic retinoscopy) will probably lose efficiency when performed by lay screeners in phases 2 and 3 of the VIP study, whereas it is unlikely that photoscreening would have had a similar loss.
HYPOTHESIS
The purpose of this thesis is to evaluate whether early vision screening can decrease the prevalence or severity of anisometropic amblyopia. New technologies are available that allow preschool vision screening to occur at an earlier age. This study hypothesizes that older children with anisometropia are more likely to have amblyopia, and are more likely to have severe amblyopia, than are younger children. If amblyopia develops as a function of duration of anisometropia in preschool children, young children would have a lower prevalence and depth of amblyopia than those identified at a later age. This result would allow for mandates encouraging early preschool vision screening to detect high levels of refractive error and anisometropia in young children. Alternatively, if the prevalence of amblyopia does not change as a function of age in anisometropic children, then the delay in treatment that necessarily results from waiting until amblyopia can be detected directly using subjective tests of visual acuity can be justified.
This study seeks to evaluate the prevalence of amblyopia in patients of various ages with a known diagnosis of anisometropia. Whereas previous studies have had a selection bias to over-include patients with abnormal acuity and to exclude patients with equal acuity, there is now an opportunity to study a large cross-section of anisometropic children. Photoscreening should identify anisometropic patients without amblyopia at a rate equal to that of patients with similar magnitude anisometropia and amblyopia.
METHODS
This study analyzes the visual acuity results from those children who were examined formally following referral from the Tennessee statewide preschool photoscreening program and found to have anisometropic refractive error (> 1.0 diopter). The description of the program and details regarding its development and validation are summarized below. Whereas many of the details and validation have been previously published,118,131,132 they are summarized here so that the data can be reviewed in context and so that the process can be understood. The entire data set relating to visual acuity and refractive error, which is described below, is original and has not been previously published. This study has approval from the Vanderbilt University Medical Center Institutional Review Board.
VOLUNTEER-LED PHOTOSCREENING IN TENNESSEE: THE PROCESS
The photoscreening program in Tennessee is performed primarily by volunteers. Beginning in September 1997, volunteer members from 223 local Lions Clubs (encompassing approximately 6,700 members) throughout the state were trained to take pictures of children using the MTI photoscreener. The Lions Club volunteers contact local day-care centers, Mother’s Day Out programs, Sunday schools, and other places where defined populations of children will be present, to arrange a vision screening at that site. Informed consent is obtained from the parents prior to screening. Up to three photographs (average, 1.4) are taken of each child in an attempt to obtain a photograph suitable for interpretation. Children ages 1 through 5 years (up to 72 months) are eligible for screening.
Early in the program, the suggested age range for screening was 6 to 48 months, but a previous study demonstrated low positive predictive values and low likelihood of intervention for children aged 6 to 12 months, and high positive predictive values for 4- to 5-year-old children.131 The current age range (12 to 71 months) has been used since January 1, 2000.
Following the screening, the photoscreening photographs are returned to the Vanderbilt Ophthalmic Imaging Center for interpretation. Interpretation is carried out by a staff of trained professionals based on a set of predetermined criteria, which this author has developed118 and validated.132 The criteria were originally designed to have a low referral rate (4%), which produces a high specificity, at the expense of relatively low sensitivity. High refractive errors, however, are well detected: these criteria detect 89% of anisometropia of 2.0 diopters or greater, 70% of nonstrabismic hyperopia of 5.0 diopters or greater, and 82% of astigmatism of 3.0 diopters or greater, with a false-positive rate of about 27%.132
The decision was made to have a low sensitivity to detect amblyopiogenic factors of low and moderate magnitude deliberately, because a low referral rate and a low false-positive rate were desired. When the program was developed, photoscreening was not well accepted, and the program was designed to be carried out by volunteers. It was recognized that high overreferral rates would doom the program in the minds of the volunteers, the pediatricians who needed to provide authorization for referral for an eye examination, and the eye doctors who would be performing the follow-up. Therefore, the referral criteria were targeted to detect only the most significant amblyopiogenic factors.
The referral criteria were designed to detect children having the amblyopiogenic factors listed in Table 2.118 This list was derived in 1997, based on consensus at that time. It is remarkably similar to the American Association for Pediatric Ophthalmology and Strabismus (AAPOS) consensus factors,126 and to the VIP study vision screening standards for criteria important to detect.16 One potentially significant difference is the program’s definition of anisometropia at greater than 1.0 diopter, rather than 1.5 diopters, as in the AAPOS and the VIP criteria. The program’s examination failure criteria have not been modified since publication of these two consensus statements, because they did not appear particularly different, and several studies have demonstrated that the risk of developing amblyopia increases with anisometropia greater than 1.0 diopter.30,31,47,48
TABLE 2.
EYE EXAMINATION FAILURE CRITERIA (AMBLYOPIOGENIC FACTORS)
| Anisometropia (sph or cyl) > 1.00 D |
| Any manifest strabismus |
| Hyperopia > +3.50 D in any meridian |
| Myopia < −3.00 D in any meridian |
| Any media opacity |
| Astigmatism > 1.5 D at 90° or 180° |
| 1.0 D at oblique axis |
Adapted from Donahue et al.118
Children who are referred from photoscreening receive a letter from the screening headquarters, which is at Vanderbilt University. Full-time, employed staff send a letter to parents of all referred children. The letter provides important background information about amblyopia, and the names of optometrists and ophthalmologists in their local areas who have agreed to examine their child and forward the results of the examination back to us at Vanderbilt. The consent form for the screening also allows release of data from the local doctor’s office, in order to comply with regulations of the Health Insurance Portability and Accounting Act.
At the formal examination, ophthalmologists and optometrists perform visual acuity testing by using age-appropriate targets, cover testing for the detection of strabismus, and cycloplegic refraction. Examinations that do not include cycloplegic refraction are termed inadequate and are not included in the analysis.
Follow-up data are reviewed weekly by Vanderbilt Ophthalmic Imaging Center personnel in conjunction with the pediatric ophthalmologist who oversees the program. Photographs of all referred children are reviewed and referral is confirmed, and examination results from all children having follow-up are evaluated. Specific attention is paid to the correlation between the suspected reason for referral and the formal examination results. Patients are formally classified into having strabismus, anisometropia, hyperopia, astigmatism, or myopia (in that order of hierarchy) on the basis of the formal examination results and the amblyopiogenic factors listed in Table 2. Finally, agreement between the photoscreening interpretation and the formal examination result is entered into a database, along with other examination information regarding the child. Analysis of the records in the database can be made to evaluate screening performance.
Two changes have been considered in the original referral criteria. An early study of ophthalmologist and optometrist treatment patterns found that patients referred with suspected astigmatism had a low likelihood (positive predictive value) of having an amblyopiogenic factor, and that children under the age of 2 years who were referred for suspected astigmatism almost never had intervention by the examining doctor.131 Therefore, a category called borderline, suggesting a rescreening in 1 year, was instituted for children 2 years and younger who were referred for suspected astigmatism. A second revision was considered following a proposal by Tong133 to alter referral criteria based on suspected hypermetropia. Analysis of Tong’s proposed criteria134 found that employing these criteria would not increase amblyopia detection substantially, and this change was not made.
DATA REVIEW AND ANALYSIS
This study sought to determine the prevalence of amblyopia as a function of child age in anisometropic children. The Microsoft Outlook database was queried to list all children who were referred from a screening, had a follow-up formal eye examination, and had a final diagnosis of anisometropia (without strabismus). Patients were analyzed according to the age (in years) at the time of the screening, the type of doctor performing the examination, the presence and severity of amblyopia, the degree of anisometropia determined by cycloplegic retinoscopy, and the visual acuity. Amblyopia was defined as a 2-line decrease in acuity (mild amblyopia). A 4-line decrease in amblyopia was considered moderate amblyopia, and a decrease in acuity of 6 or more lines was considered severe amblyopia. For preliterate children who had fixation preference testing to detect amblyopia, CSUM (central, steady, unmaintained) versus CSM (central, steady, maintained) was considered mild amblyopia, UCSUM (uncentral, steady, unmaintained) was considered moderate amblyopia, and UCUSUM (uncentral, unsteady, unmaintained) was considered severe amblyopia. Patients not having visual acuity documented by the examining doctor were eliminated from analysis.
For comparison, similar analyses were made for patients having strabismus, based upon age at screening and type of examining eye doctor. It should be noted that in this study, anisometropic children with superimposed strabismus were classified as strabismic; thus all anisometropic individuals were orthotropic. Statistical testing used paired t tests, χ2, and Fisher exact test as appropriate.
RESULTS
The data presented represent children screened from September 1, 1997, through December 31, 2003 (Table 3). During this period, 119,311 children had screening attempted. Photoscreening was successful 96.7% of the time; 5,548 children were referred, and 4,140 (74.7%) presented for follow-up. Overall, 2,867 examined children (73.7% of those examined) were found to have an amblyopiogenic factor. Seven hundred ninety-two children aged zero through 7 years were found to have anisometropia of greater than 1.0 diopter, without coexisting strabismus on formal evaluation. Of these children, 380 were examined by optometrists, 134 by general ophthalmologists, and 278 by pediatric ophthalmologists (Table 4).
TABLE 3.
PHOTOSCREENING DATA IN TENNESSEE (SEPTEMBER 1997 THROUGH DECEMBER 31, 2003)
| Number of children screened | 119,311 |
| Photographs taken | 161,830 |
| Successful screening* | 115,445 (96.76%) |
| Number of children passed | 109,897 (92.11%) |
| Number of children referred | 5,548 (4.65%) |
| Number of children examined | 4,140 (74.70%) |
| Children with documented anisometropia† | 792 |
A successful screening is defined as having a photograph of adequate quality to be interpreted by the Vanderbilt Ophthalmic Imaging Center.
Anisometropia >1.0 D on cycloplegic refraction; these subjects are the focus of this investigation.
TABLE 4.
RESULTS FROM EVALUATIONS OF ANISOMETROPIC CHILDREN (n = 792)*
| EXAMINING DOCTOR | n | ACUITY DOCUMENTED | NO ACUITY DOCUMENTED |
|---|---|---|---|
| Optometrist | 380 | 325 (86%) | 55 (14%) |
| Ophthalmologist | 134 | 124 (93%) | 10 (7%) |
| Pediatric ophthalmologist | 278 | 273 (98%) | 5 (2%) |
P < .0001.
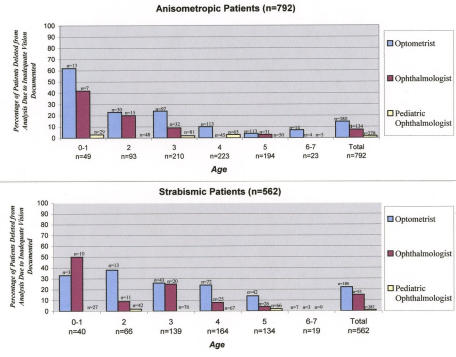
Some children had no visual acuity documented by the examining doctor, despite requests for such data (Table 4). This included 55 patients (14%) evaluated by optometrists, 10 patients evaluated by ophthalmologists (7%), and five patients (2%) evaluated by pediatric ophthalmologists (P < .0001, Fisher exact test, optometrists versus all ophthalmologists; P < .01, Fisher exact test, pediatric ophthalmologist versus general ophthalmologist). This difference was highly statistically significant and was present at each age until age 5 years (Figure 1, top). These data were more striking when children aged 3 or younger (typically preverbal) were evaluated (Table 5). Acuity was documented in 155 (98.1%) of 158 children 3 years old or younger evaluated by pediatric ophthalmologists, in 45 (83%) of 54 children evaluated by general ophthalmologists, and in 102 (73%) of 140 children evaluated by optometrists. After age 3, the percentage of children having documented visual acuity was similar for those seen by pediatric ophthalmologists (118 of 120, or 98.3%) and general ophthalmologists (79 of 80, or 98.8%), but still lower for children examined by optometrists (223 of 240, or 92.9%). The 70 anisometropic children not having visual acuity data documented were eliminated from further analysis. “Fix and follow” acuity or “sees well” was considered to be documented acuity, although it is extremely subjective and probably not a good indicator of the presence of amblyopia. Patients with no acuity documented either had the acuity line in follow-up left blank or had a comment such as “too young to test,” “not cooperative,” “could not read,” or a similar statement.
FIGURE 1.
The percentage of patients deleted from analysis because visual acuity was not documented is plotted for various ages for anisometropic children (top) and those having strabismus (bottom). The training and qualifications of the examining doctor are also represented for each age group. Above each vertical bar is the number of patients in the age group examined by the respective type of eye doctor; below the age is the total number of children in that age group.
TABLE 5.
ANISOMETROPIC PATIENTS WITHOUT ACUITY DOCUMENTED BY AGE
|
TYPE OF DOCTOR |
||||
|---|---|---|---|---|
| AGE (YEARS) | OPTOMETRIST | GENERAL OPHTHALMOLOGIST | PEDIATRIC OPHTHALMOLOGIST | TOTAL |
| 0 to 1 | 8/13 (62%) | 3/7 (42%) | 1/29 (3%) | 12/49 (25%) |
| 2 | 7/30 (23%) | 3/15 (20%) | 0/48 (0%) | 10/93 (11%) |
| 3 | 23/97 (24%) | 3/32 (9%) | 2/81 (2%) | 28/210 (13%) |
| 4 | 11/113 (10%) | 0/45 (0%) | 2/65 (3%) | 13/223 (6%) |
| 5 | 5/113 (4%) | 1/31 (3%) | 0/50 (0%) | 6/194 (3%) |
| 6 to 7 | 1/14 (7%) | 0/4 (0%) | 0/5 (0%) | 1/23 (4%) |
| Total | 55/380 (14.5%) | 10/134 (7.4%) | 5/278 (1.8%) | 70/792 (9%) |
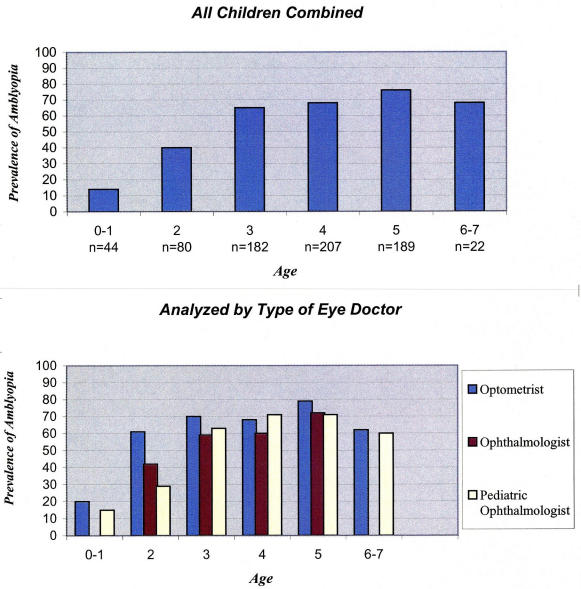
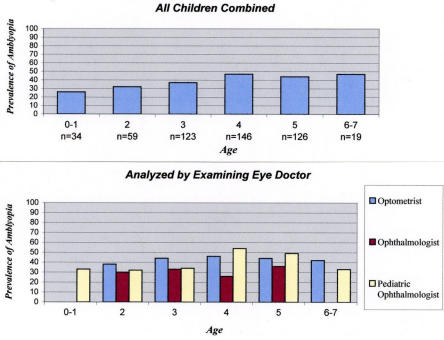
Figure 2A (top) shows the prevalence of amblyopia as a function of age in patients with orthotropic anisometropia. Only 6 of 44 patients (14%) aged 1 year or less had amblyopia. Thirty-two (40%) of 80 2-year-old children had amblyopia, whereas the prevalence rose to 65% in 3-year-old children (119 of 182). The prevalence of amblyopia peaked at 76% for 5-year-old children but was relatively similar for ages 4 through 7 (Table 6A).
FIGURE 2A.
The prevalence of amblyopia in patients having anisometropic refractive error is shown for each age group (top). The total number of children in each age group is shown below the age. Data are similar when evaluated with respect to the type of doctor performing the examination (bottom).
TABLE 6A.
NUMBER OF CHILDREN WITH AMBLYOPIA BY AGE: ANISOMETROPIA
|
NO. WITH AMBLYOPIA |
|||||
|---|---|---|---|---|---|
| AGE (YEARS) | NO. WITH NO AMBLYOPIA | MILD | MODERATE | SEVERE | TOTAL |
| 0 to 1 | 38 | 5 | 1 | 0 | 6/44 (14%) |
| 2 | 48 | 18 | 9 | 5 | 32/80 (40%) |
| 3 | 63 | 66 | 46 | 7 | 119/182 (65%) |
| 4 | 68 | 73 | 47 | 19 | 139/207 (67%) |
| 5 | 46 | 87 | 29 | 27 | 143/189 (76%) |
| 6 to 7 | 7 | 5 | 8 | 2 | 15/22 (68%) |
The prevalence rate for amblyopia as a function of age in anisometropic children remained remarkably similar when evaluated by type of eye doctor (Table 7A). Amblyopia was detected in 15% of children (5 of 33) under the age of 2 examined by pediatric ophthalmologists, in 20% (1 of 5) of such children examined by optometrists, and in none of six such patients examined by general ophthalmologists. The prevalence of amblyopia increased proportionately with age and remained relatively constant at and after age of 4 (Figure 2A, bottom).
TABLE 7A.
PREVALENCE OF AMBLYOPIA BY AGE AND EXAMINING DOCTOR: ANISOMETROPIA
|
TYPE OF DOCTOR |
|||
|---|---|---|---|
| AGE (YEARS) | OPTOMETRIST | GENERAL OPHTHALMOLOGIST | PEDIATRIC OPHTHALMOLOGIST |
| 0 to 1 | 1/5 (20%) | 0/6 (0%) | 5/33 (15%) |
| 2 | 14/23 (61%) | 5/12 (42%) | 13/45 (29%) |
| 3 | 52/74 (70%) | 17/29 (59%) | 50/79 (63%) |
| 4 | 67/99 (68%) | 26/43 (60%) | 46/65 (71%) |
| 5 | 87/110 (79%) | 23/32 (72%) | 34/48 (71%) |
| 6 to 7 | 8/13 (62%) | 4/4 (100%) | 3/5 (60%) |
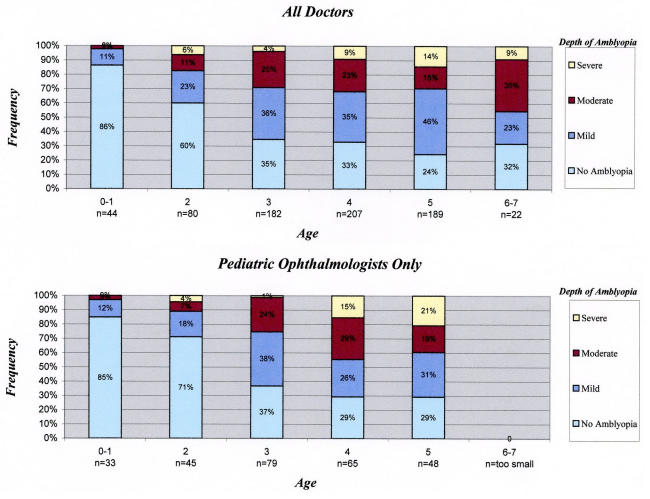
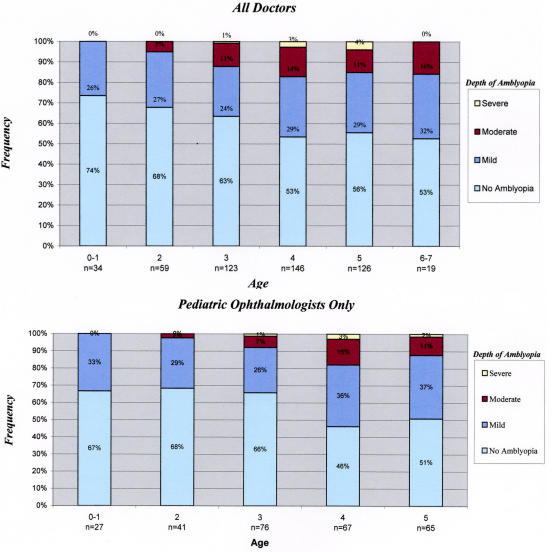
In addition to younger children with anisometropia having a lower prevalence of amblyopia, the severity of the amblyopia was less in young children (Table 6B). The severity of amblyopia by age for patients with anisometropia is shown graphically in Figure 3, top. Patients were divided into mild amblyopia (2 to 3 lines), moderate amblyopia (4 to 5 lines), and severe amblyopia (6 or greater lines). Although 14% of anisometropic children under 2 years of age had amblyopia (6 of 44), it was mild in five of the six and moderate in only one (2% of examined children). Moderate amblyopia began to increase in frequency at age 2, when amblyopia of moderate or greater degree was observed in 17% of examined children (Table 6A). This proportion rose steadily to represent 45% of all examined 6- and 7-year-old children. Similarly, severe amblyopia was rare prior to age 4, affecting only 4% of 3-year-old children with anisometropia. However, severe amblyopia affected 9% of 4-year-old children and 14% of 5-year-olds (Figure 3, top).
TABLE 6B.
SEVERITY OF AMBLYOPIA BY AGE*: ANISOMETROPIA
|
AMBLYOPIA |
|||
|---|---|---|---|
| AGE (YEARS) | MILD | MODERATE | SEVERE |
| 0 to 1 | 14% | 4% | 0% |
| 2 | 40% | 18% | 6% |
| 3 | 65% | 29% | 4% |
| 4 | 67% | 32% | 9% |
| 5 | 76% | 30% | 14% |
| 6 to 7 | 68% | 45% | 9% |
Percentage of examined children having amblyopia of that level or greater magnitude.
FIGURE 3.
The prevalence and depth (see “Methods” section) of amblyopia in anisometropic children are analyzed as a function of child age. Children were classified as having no amblyopia or mild, moderate, or severe amblyopia. The number of children in each age group is below the age. Results from all examining doctors are shown at top; data from children evaluated by pediatric ophthalmologists are shown at bottom. Only five children aged 6 to 7 were examined by pediatric ophthalmologists.
The data correlating age with depth of amblyopia are even more robust when the analysis is limited only to those children who were evaluated by pediatric ophthalmologists (Figure 3, bottom). Only 3% of children (1 of 33) under the age of 2 who were evaluated by pediatric ophthalmologists had moderate amblyopia; none had severe amblyopia. The prevalence of moderate or severe amblyopia rose to 11% of 2-year-olds (5 of 45), 25% of 3-year-olds (20 of 79), 45% (29 of 65) at age 4, and 40% (19 of 48) at age 5. Only five children aged 6 or 7 were evaluated by pediatric ophthalmologists, and three had amblyopia. It should be noted that age 3 is the earliest that children can be screened using traditional techniques, and by this age, amblyopia was firmly entrenched and often moderate or severe.
To compare all the results by age, and rule out that an age-associated bias in acuity testing produced the observed results, the 562 patients who were referred from the Tennessee screening program and found to have strabismus on formal examination were evaluated. Visual acuity was not documented in 56 children (10%) (Figure 1, bottom). Acuity data were provided for 78% (140 of 180) of children examined by optometrists, for 85% (81 of 95) of those seen by general ophthalmologists, and for 99% (285 of 287) of pediatric ophthalmologists (P < .001) (Figure 1, bottom). The 56 patients not having documented acuity were excluded from analysis.
Results from the 506 patients having acuity data are shown in Figure 2B. The prevalence of amblyopia was less related to age than it was for anisometropic children. Children under 2 had amblyopia in 26% (9 of 34) of cases (Table 7B). Twenty-seven of these 34 patients were seen by pediatric ophthalmologists, and amblyopia was elicited only in these patients (33% of the time). The prevalence of amblyopia in strabismic children aged 2 through 7 ranged from 32% to 47% (Figure 2B, top). It was remarkably consistent whether the patients were seen by general ophthalmologists, optometrists, or pediatric ophthalmologists, although there was a trend for general ophthalmologists to report a lower prevalence of amblyopia than did the optometrists or pediatric ophthalmologists (Figure 2B, bottom). Thus, the age-related increase in amblyopia preference observed so strongly with anisometropic amblyopia was not as apparent for strabismic amblyopia.
FIGURE 2B.
For comparison with Figure 2A, similar prevalence data as a function of age are provided for all strabismic patients (top) and, additionally, based upon the type of doctor performing the examination (bottom). The number of strabismic children aged 0 to 1 was very small for optometrists (n = 2) and comprehensive ophthalmologists (n = 5).
TABLE 7B.
PREVALENCE OF AMBLYOPIA BY AGE AND EXAMINING DOCTOR: STRABISMUS
|
TYPE OF DOCTOR |
||||
|---|---|---|---|---|
| AGE (YEARS) | OPTOMETRIST | GENERAL OPHTHALMOLOGIST | PEDIATRIC OPHTHALMOLOGIST | TOTAL |
| 0 to 1 | 0/2 (0%) | 0/5 (0%) | 9/27 (33%) | 9/34 (26%) |
| 2 | 3/8 (38%) | 3/10 (30%) | 13/41 (32%) | 19/59 (32%) |
| 3 | 14/32 (44%) | 5/15 (33%) | 26/76 (34%) | 45/123 (37%) |
| 4 | 26/56 (46%) | 6/23 (26%) | 36/67 (54%) | 68/146 (47%) |
| 5 | 16/36 (44%) | 9/25 (36%) | 32/65 (49%) | 56/126 (44%) |
| 6 to 7 | 3/7 (43%) | 3/3 (100%) | 3/9 (33%) | 9/19 (47%) |
In addition, although there was a trend for strabismic amblyopia to increase in severity in older children, the trend was not as apparent in patients with strabismus as it was for anisometropia (Figure 4; Table 8). Moderate or severe amblyopia affected 13% and 20%, respectively, of children in the 3-year-old and older age-groups, and severe amblyopia was rare at all ages, never affecting more than 4% of strabismic children.
FIGURE 4.
The prevalence and depth of amblyopia in strabismic children are analyzed as a function of child age. Children were classified as having no amblyopia or mild, moderate, or severe amblyopia (see “Methods” section). The number of children in each age-group is below the age. Results from all examining doctors are shown at top; data from children evaluated by pediatric ophthalmologists are shown at bottom. Only nine children aged 6 to 7 were examined by pediatric ophthalmologists; three had amblyopia.
TABLE 8A.
NUMBER OF CHILDREN WITH AMBLYOPIA BY AGE: STRABISMUS
|
NO. WITH AMBLYOPIA |
|||||
|---|---|---|---|---|---|
| AGE (YEARS) | NO. WITH NO AMBLYOPIA | MILD | MODERATE | SEVERE | TOTAL |
| 0 to 1 | 25 | 9 | 0 | 0 | 9/34 (26%) |
| 2 | 40 | 16 | 3 | 0 | 19/59 (32%) |
| 3 | 78 | 30 | 14 | 1 | 45/123 (37%) |
| 4 | 78 | 43 | 21 | 4 | 68/146 (47%) |
| 5 | 70 | 37 | 14 | 5 | 56/126 (44%) |
| 6 to 7 | 10 | 6 | 3 | 0 | 9/19 (47%) |
TABLE 8B.
SEVERITY OF AMBLYOPIA BY AGE*: STRABISMUS
|
AMBLYOPIA |
|||
|---|---|---|---|
| AGE (YEARS) | MILD | MODERATE | SEVERE |
| 0 to 1 | 26% | 0% | 0% |
| 2 | 32% | 5% | 0% |
| 3 | 37% | 12% | 1% |
| 4 | 47% | 17% | 3% |
| 5 | 44% | 15% | 4% |
| 6 to 7 | 47% | 16% | 0% |
Percentage of examined children having amblyopia of that level or greater magnitude.
DISCUSSION
Previous studies have demonstrated that anisometropia can be a powerful amblyopiogenic factor, due to either the decreased resolution caused by optical defocus at the fovea29,59 or the production of active suppression.51,52 Anisometropia begins to be associated with amblyopia when it exceeds approximately 1 diopter,30,47,48 and the prevalence and depth of amblyopia then become related to the magnitude of the anisometropia.23,33–38,47,48 Small sample sizes and selection bias have produced inconsistencies in the literature with respect to the influence of patient age on the risk of developing amblyopia (see “Introduction” and “Background” sections for details). The largest study to date of patients with anisometropic amblyopia98,99 suggested that the most important factors in determining the response of amblyopia to treatment were the age of the patient and the depth of the amblyopia.
Previous prevalence studies and demographic reports of amblyopia in anisometropic patients are biased because patients who have anisometropia and good visual acuity are unlikely to be included, since they are nearly always asymptomatic. The patients without amblyopia who are included in these studies are typically those having a family history of amblyopia or other eye problem,47,48 whose parents bring them in to “make sure everything is okay.”
This study evaluated a large population of patients with known anisometropia. By utilizing children referred from photoscreening rather than those referred on account of poor acuity, there was an opportunity to evaluate how the prevalence and depth of amblyopia are related to the duration of anisometropia and the patient age. This is important because photoscreening and other screening technologies emphasize early detection of children at risk for amblyopia. Finding an increasing prevalence of amblyopia with age would support such early screening. Conversely, the lack of a relationship between age and amblyopia prevalence would suggest that early screening is not warranted.
This study found that amblyopia is rare in anisometropic children under the age of 2 years, affecting only 14% of such children. The prevalence of amblyopia rises rapidly, however, and by age 3, nearly two thirds of children having greater than 1.0 diopter anisometropia have developed amblyopia (Figure 2A, top). The prevalence of amblyopia increases only slightly after this. This finding is extremely important, because traditional screening cannot occur until at least age 3. This study suggests that by this age, amblyopia has already occurred in most children in whom it will develop. Additionally, these results suggest that nearly 30% of young anisometropic children probably never develop amblyopia. If anisometropia is present but then regresses, as has been hypothesized,21,23,32,40,41 this number could be even higher.
Although the prevalence of anisometropic amblyopia does not increase after age 3, the depth of amblyopia does. Fewer than 4% of children aged 3 or younger have severe amblyopia. However, the prevalence of both moderate and severe amblyopia increases for children older than age 3 (Figure 3). Moderate amblyopia (4 lines of acuity difference) begins to appear at age 2 and affects over 30% of anisometropic children aged 3 to 7. Severe anisometropic amblyopia (6 lines of difference) is restricted primarily to children aged 4 or older.75,103 Thus, screenings that target children at this age or older identify a population of children who have more extensive disease than they would have had if they had been identified earlier. Because mild anisometropia can often be treated with spectacles, it is likely that amblyopia can be prevented by similar treatment if it is instituted early, when amblyopia is mild. Technology that identifies children with anisometropic refractive error prior to the age of 4 years, therefore allowing their early treatment, should reduce the proportion and depth of amblyopia.
Children with strabismus have a lower prevalence of amblyopia than do children with anisometropia at all ages. They have less severe amblyopia as well. Hence, anisometropia appears to be a more powerful amblyopiogenic factor than strabismus, and the duration of anisometropia also appears to be more important than the duration of strabismus with respect to the development and depth of amblyopia.
Three types of eye doctors provided care for these children. The results are remarkably consistent with respect to the type of doctor performing the examination. Whereas optometrists failed to assess visual acuity more often than did comprehensive ophthalmologists or pediatric ophthalmologists, especially in younger children, the presence of amblyopia and its depth did not appear to depend upon the type of doctor performing the examination. It is unlikely that any bias was caused by eliminating from analysis those children whose vision could not be tested. The majority of excluded children were seen by optometrists and potentially may have had a lower prevalence of amblyopia if parents with a family history of amblyopia brought their children more often to ophthalmologists for the formal examination. There is no evidence that this occurred, however. Only five of 278 children seen by pediatric ophthalmologists were excluded because acuity was not documented, and the amblyopia prevalence data obtained from those children are the most robust.
There are several limitations to these data. First, since photoscreening has a high specificity when the published Tennessee referral criteria are used, there is a resultant reduction in sensitivity, particularly to detect low-magnitude refractive error. Therefore, many children with mild and moderate levels of anisometropia were likely not detected and thus not included in this study. As a result, this study probably overidentified children having high-magnitude anisometropia and, therefore, probably overestimates the prevalence of amblyopia. This limitation should occur at all age-groups, however, be independent of the type of eye doctor, and therefore probably not impact the conclusions. The net bias is probably less than that obtained in previous studies, where children with anisometropia but good acuity were underreported.
Visual acuity was tested and documented in a nonstandard method in this study. Local optometrists and ophthalmologists were asked to provide best-corrected acuity, using either an induced tropia technique or an age-appropriate target, to measure visual acuity. It is unclear how consistently these directions were followed, and this information was unavailable. If fixation preference testing overestimates amblyopia in young children,135 the increase in prevalence of amblyopia with age is even more striking than what is reported here. The crowding phenomenon or other problems (eg, fatigue, inattention) that increase variability in acuity testing of amblyopic children might have introduced some bias. This might produce a falsely higher prevalence of amblyopia in older children, in whom vision is more likely to be directly tested, than in younger children. This is, in fact, what was found. On the other hand, using isolated letters to test acuity would have decreased the detection of amblyopia.111 Finally, it is unclear how often the visual acuity was reported as best-corrected, as requested, rather than uncorrected acuity. This bias could falsely increase the observed prevalence of amblyopia, but affect all age-groups equally, and not influence the conclusion.
Because the preschool children studied were different ages, they required different types of acuity testing. This study attempted to standardize the visual acuity data to adjust for different depths of amblyopia at various ages. However, it is unclear how appropriate this standardization was across the age groups. Therefore, there may be an overestimation or underestimation of the prevalence of severe amblyopia in the youngest children. This was the rationale for also including acuity data from patients with strabismic amblyopia in an attempt to control for this potential bias. These biases in acuity testing techniques, reporting techniques, and standardization methods should theoretically have also been present for strabismic children of the same age. The lack of a parallel trend in increasing prevalence of amblyopia with age in patients with strabismus supports that the observations are not simply caused by age-dependent differences in visual acuity testing methodologies. It is reassuring that the prevalence of amblyopia in strabismic patients, approximately 40%, is similar to the recognized 25% to 40% prevalence of amblyopia in esotropic patients.1,136,137 It may be that strabismic children who are prone to develop amblyopia do so much more quickly than anisometropic children and therefore already have amblyopia on presentation.
Previous studies (documented in the “Introduction” section) have suggested that many children with anisometropia lose their anisometropia during development,21,23,32,40,41 presumably due to emmetropization or some other process. Other studies have suggested that anisometropia develops as a result of amblyopia, in contrast to traditional teaching that anisometropia causes amblyopia.40,42,43 How does one reconcile these previous studies with the data in this study, demonstrating that nearly 70% of anisometropic children who are old enough to test with optotypes (age 4 or older) are already amblyopic? This is most likely a result of several of the above biases: First, there was a tendency to preferentially study children with the most severe anisometropia, who were most likely to develop amblyopia, and least likely to spontaneously resolve.32 Second, the resolution of anisometropia during emmetropization may bring with it a restoration of normal acuity with the resultant loss of amblyopia; this is essentially what occurs when one treats anisometropic amblyopic patients with spectacles (ie, the acuity gets better).75,103 In this study, the effects of a period of spectacle correction on acuity were not assessed.
Concerns such as those raised above can only be answered with a large-scale, prospective, long-term (years), observational (noninterventional) study of children with anisometropia. However, the study’s sample size would need to be enormous. Cycloplegic refraction would need to be performed on approximately 20,000 to 30,000 healthy infants to identify a cohort similar to the sample reported here; even a cohort of size 790 might be insufficient to adequately address issues such as the development of amblyopia and the resolution of amblyopia over years during emmetropization. Furthermore, the ethics of failing to treat an identified child with dense anisometropic amblyopia simply to determine the natural history would be highly suspect, especially given this study’s data that suggest that amblyopia depth increases with time. Hence, it is unlikely such a study will ever occur.
Several recent studies have demonstrated that many patients with anisometropic amblyopia have significant improvement following a period of spectacle correction.74,75,103 The visual acuity data in this study were obtained at the first visit, prior to any such period of spectacle wearing. Thus, many of the patients identified as having amblyopia in this study could potentially have been treated with spectacles alone and still had substantial improvement in acuity. Whether or not a correctable deficit in visual acuity truly represents amblyopia (in the sense of recognized anatomic and physiologic changes in the visual cortex and other afferent visual areas) is likely to become controversial in the future. It may be that long-standing foveal blur and optical defocus produce correctable “amblyopia” by a different mechanism than that which causes the residual defect observed following a spectacle phase. This second deficit, which is more classic amblyopia, may be due to the presence of active foveal suppression, require penalization to treat, and have age-adjusted improvement rates more similar to what traditional teaching suggests.
SUMMARY
Traditional visual screening is essentially limited to children aged 4 and older. Although successful field testing of large numbers of 3-year-old children has been reported (using trained eye doctors with expertise in preschool vision screening techniques),16 it is unlikely that such success will ever be able to be transferred adequately to field testing in large numbers because of testability issues with less well-trained screeners. Newer technologies, such as photoscreening, photorefraction, and noncycloplegic autorefraction, provide the opportunity to evaluate younger children in very large numbers. It has been unclear if earlier detection of at-risk children provides significant benefit to warrant continued development of such technology.
Previous studies have demonstrated that photoscreening can be highly effective in identifying children who have amblyopiogenic factors, provided the screening setting is highly controlled.118,131,132,134,138 This study found that children with anisometropic refractive error are less likely to have amblyopia if they are detected at a young age. The prevalence and severity of anisometropic amblyopia rise with increasing age (and presumably with anisometropia duration) but have already levelled off prior to the age when most children can be screened using traditional techniques. Therefore, traditional screening identifies children who are already at a disadvantage with respect to disease progression.
Instituting vision screening at a very early age will detect children with anisometropic refractive error prior to the development of amblyopia. This will allow ophthalmologists the opportunity to intervene with treatment and attempt to prevent amblyopia or retard its further development. The efficacy of such treatment with respect to amblyopia prevention will be the focus of further investigations.
ACKNOWLEDGMENTS
The author wishes to express his gratitude to many individuals whose assistance made this work possible, including mentors Denis O’Day, MD, Vanderbilt University Medical Center, and Al Biglan, MD, University of Pittsburgh; and Tammy Johnson, MPH, Lions Clubs of America, who helped develop the program in Tennessee. I also wish to thank the volunteer Lions Club members who screened the children and the ophthalmologists and optometrists in Tennessee who evaluated the referred children and shared their results with us.
Footnotes
Supported by the Tennessee Lions Charities, Lions Clubs International Foundation, State of Tennessee; by a Career Development Award to the author from Research to Prevent Blindness, Inc, New York, New York; and by an unrestricted grant from Research to Prevent Blindness, Inc.
REFERENCES
- 1.von Noorden GK. Binocular Vision and Ocular Motility. 6th ed. St Louis: Mosby; 2002.
- 2.Ederer F, Krueger DE. Report on the National Eye Institute’s Visual Acuity Impairment Survey Pilot Study Bethesda, Maryland: Office of Biometry and Epidemiology, National Eye Institute, National Institutes of Health, Public Health Service, Dept of Health and Human Services; 1984:81–84.
- 3.Attebo K, Mitchell P, Cumming R, et al. Prevalence and causes of amblyopia in an adult population. Ophthalmology. 1998;105:154–159. doi: 10.1016/s0161-6420(98)91862-0. [DOI] [PubMed] [Google Scholar]
- 4.Tommila V, Tarkkanen A. Incidence of loss of vision in the healthy eye in amblyopia. Br J Ophthalmol. 1981;65:575–577. doi: 10.1136/bjo.65.8.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahi J, Logan S, Timms C, et al. Risk, causes, and outcomes of visual impairment after loss of vision in the non-amblyopic eye: a population-based study. Lancet. 2002;360:597–602. doi: 10.1016/s0140-6736(02)09782-9. [DOI] [PubMed] [Google Scholar]
- 6.Chua B, Mitchell P. Consequences of amblyopia on education, occupation, and long term vision loss. Br J Ophthalmol. 2004;88:1119–1121. doi: 10.1136/bjo.2004.041863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Membreno JH, Brown MM, Brown GC, et al. A cost-utility analysis of therapy for amblyopia. Ophthalmology. 2002;109:2265–2271. doi: 10.1016/s0161-6420(02)01286-1. [DOI] [PubMed] [Google Scholar]
- 8.Pediatric Eye Disease Investigator Group. The clinical profile of moderate amblyopia in children younger than 7 years. Arch Ophthalmol. 2002;120:281–287. [PubMed] [Google Scholar]
- 9.von Noorden GK, Crawford ML. The sensitive period. Trans Ophthalmol Soc U K. 1979;99:442–446. [PubMed] [Google Scholar]
- 10.Simons K, Preslan M. Natural history of amblyopia untreated owing to lack of compliance. Br J Ophthalmol. 1999;83:582–587. doi: 10.1136/bjo.83.5.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol. 2002;120:268–278. doi: 10.1001/archopht.120.3.268. [DOI] [PubMed] [Google Scholar]
- 12.Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121:603–611. doi: 10.1001/archopht.121.5.603. [DOI] [PubMed] [Google Scholar]
- 13.Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110:2075–2087. doi: 10.1016/j.ophtha.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Pediatric Eye Disease Investigator Group. A comparison of atropine and patching treatments for moderate amblyopia by patient age, cause of amblyopia, depth of amblyopia, and other factors. Ophthalmology. 2003;110:1632–1638. doi: 10.1016/S0161-6420(03)00500-1. [DOI] [PubMed] [Google Scholar]
- 15.Pediatric Eye Disease Investigator Group. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111:2076–2085. doi: 10.1016/j.ophtha.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt P, Maguire M, Dobson V, et al. Vision in Preschoolers Study Group. Comparison of preschool vision screening tests as administered by licensed eye care professionals in the Vision In Preschoolers Study. Ophthalmology. 2004;111:637–650. doi: 10.1016/j.ophtha.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 17.Saunders KJ. Early refractive development in humans. Surv Ophthalmol. 1995;40:207–216. doi: 10.1016/s0039-6257(95)80027-1. [DOI] [PubMed] [Google Scholar]
- 18.Atkinson J, Braddick O. Vision screening and photorefraction—the relation of refractive errors to strabismus and amblyopia. Behav Brain Res. 1983;10:71–80. doi: 10.1016/0166-4328(83)90152-3. [DOI] [PubMed] [Google Scholar]
- 19.Atkinson J, Braddick O, Durden K, et al. Screening for refractive errors in 6–9 month old infants by photorefraction. Br J Ophthalmol. 1984;68:105–112. doi: 10.1136/bjo.68.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thompson CM. Objective and Psychophysical Studies of Infant Visual Development [PhD thesis]. Birmingham, UK: University of Aston; 1987.
- 21.Almeder LM, Peck LB, Howland HC. Prevalence of anisometropia in volunteer laboratory and school screening populations. Invest Ophthalmol Vis Sci. 1990;31:2448–2455. [PubMed] [Google Scholar]
- 22.Yamashita T, Watanabe S, Ohba N. A longitudinal study of cycloplegic refraction in a cohort of 350 Japanese schoolchildren. Anisometropia. Ophthalmic Physiol Opt. 1999;19:30–33. doi: 10.1046/j.1475-1313.1998.00407.x. [DOI] [PubMed] [Google Scholar]
- 23.Abrahamsson M, Fabian G, Sjostrand J. A longitudinal study of a population based sample of astigmatic children. II. The changeability of anisometropia. Acta Ophthalmol (Copenh) 1990;68:435–440. doi: 10.1111/j.1755-3768.1990.tb01672.x. [DOI] [PubMed] [Google Scholar]
- 24.Weale RA. On the age-related prevalence of anisometropia. Ophthalmic Res. 2002;34:389–392. doi: 10.1159/000067040. [DOI] [PubMed] [Google Scholar]
- 25.Bourne RR, Dineen BP, Ali SM, et al. Prevalence of refractive error in Bangladeshi adults: results of the National Blindness and Low Vision Survey of Bangladesh. Ophthalmology. 2004;111:1150–1160. doi: 10.1016/j.ophtha.2003.09.046. [DOI] [PubMed] [Google Scholar]
- 26.Quek TP, Chua CG, Chong CS, et al. Prevalence of refractive errors in teenage high school students in Singapore. Ophthalmic Physiol Opt. 2004;24:47–55. doi: 10.1046/j.1475-1313.2003.00166.x. [DOI] [PubMed] [Google Scholar]
- 27.Lyle TK. Worth and Chavasse’s Squint. 8th ed. Philadelphia: Blakiston; 1950:138.
- 28.Helveston EM. Relationship between degree of anisometropia and depth of amblyopia. Am J Ophthalmol. 1966;62:757–759. doi: 10.1016/0002-9394(66)92207-0. [DOI] [PubMed] [Google Scholar]
- 29.Dadeya S, Kamlesh, Shibal F. The effect of anisometropia on binocular visual function. Indian J Ophthalmol. 2001;49:261–263. [PubMed] [Google Scholar]
- 30.Ingram RM, Walker C. Refraction as a means of predicting squint or amblyopia in preschool siblings of children known to have these defects. Br J Ophthalmol. 1979;63:238–242. doi: 10.1136/bjo.63.4.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Latvala ML, Paloheimo M, Karma A. Screening of amblyopic children and long-term follow-up. Acta Ophthalmol Scand. 1996;74:488–492. doi: 10.1111/j.1600-0420.1996.tb00605.x. [DOI] [PubMed] [Google Scholar]
- 32.Abrahamsson M, Sjostrand J. Natural history of infantile anisometropia. Br J Ophthalmol. 1996;80:860–863. doi: 10.1136/bjo.80.10.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tanlamai T, Goss DA. Prevalence of monocular amblyopia among anisometropes. Am J Optom Physiol Opt. 1979;56:704–715. doi: 10.1097/00006324-197911000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Sen DK. Anisometropic amblyopia. J Pediatr Ophthalmol Strabismus. 1980;17:180–184. doi: 10.3928/0191-3913-19800501-13. [DOI] [PubMed] [Google Scholar]
- 35.Rutstein RP, Corliss D. Relationship between anisometropia, amblyopia, and binocularity. Optom Vis Sci. 1999;76:229–233. doi: 10.1097/00006324-199904000-00026. [DOI] [PubMed] [Google Scholar]
- 36.Kivlin JD, Flynn JT. Therapy of anisometropic amblyopia. J Pediatr Ophthalmol Strabismus. 1981;18:47–56. doi: 10.3928/0191-3913-19810901-12. [DOI] [PubMed] [Google Scholar]
- 37.Townshend AM, Holmes JM, Evans LS. Depth of anisometropic amblyopia and difference in refraction. Am J Ophthalmol. 1993;116:431–436. doi: 10.1016/s0002-9394(14)71400-x. [DOI] [PubMed] [Google Scholar]
- 38.Dolezalova V. Relation of anisometropia and the extent of amblyopia. Cesk Slov Oftalmol. 1998;54:127–130. [PubMed] [Google Scholar]
- 39.Kutschke PJ, Scott WE, Keech RV. Anisometropic amblyopia. Ophthalmology. 1991;98:258–263. doi: 10.1016/s0161-6420(91)32307-8. [DOI] [PubMed] [Google Scholar]
- 40.Fielder AR, Moseley MJ. Anisometropia and amblyopia—chicken or egg? Br J Ophthalmol. 1996;80:857–858. doi: 10.1136/bjo.80.10.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ingram RM, Gill LE, Lambert TW. Emmetropisation in normal and strabismic children and the associated changes of anisometropia. Strabismus. 2003;11:71–84. doi: 10.1076/stra.11.2.71.15104. [DOI] [PubMed] [Google Scholar]
- 42.Lepard CW. Comparative changes in the error of refraction between fixing and amblyopic eyes during growth and development. Am J Ophthalmol. 1975;80:485–490. doi: 10.1016/0002-9394(75)90212-3. [DOI] [PubMed] [Google Scholar]
- 43.Nastri G, Perugini GC, Savastano S, et al. The evolution of refraction in the fixing and the amblyopic eye. Doc Ophthalmol. 1984;56:265–274. doi: 10.1007/BF00159077. [DOI] [PubMed] [Google Scholar]
- 44.Shaw DE, Fielder AR, Minshull C, et al. Amblyopia—factors influencing age of presentation. Lancet. 1988;2:207–209. doi: 10.1016/s0140-6736(88)92301-x. [DOI] [PubMed] [Google Scholar]
- 45.Woodruff G, Hiscox F, Thompson JR, et al. The presentation of children with amblyopia. Eye. 1994;8:623–626. doi: 10.1038/eye.1994.156. [DOI] [PubMed] [Google Scholar]
- 46.Chua BE, Johnson K, Martin F. A retrospective review of the associations between amblyopia type patient age, treatment compliance and referral patterns. Clin Exp Ophthalmol. 2004;32:175–179. doi: 10.1111/j.1442-9071.2004.00794.x. [DOI] [PubMed] [Google Scholar]
- 47.Weakley DR. The association between anisometropia, amblyopia, and binocularity in the absence of strabismus. Trans Am Ophthalmol Soc. 1999;97:987–1021. [PMC free article] [PubMed] [Google Scholar]
- 48.Weakley DR., Jr The association between nonstrabismic anisometropia, amblyopia and subnormal binocularity. Ophthalmology. 2001;108:163–171. doi: 10.1016/s0161-6420(00)00425-5. [DOI] [PubMed] [Google Scholar]
- 49.Weakley DR, Jr, Birch E. The role of anisometropia in the development of accommodative esotropia. Trans Am Ophthalmol Soc. 2000;98:71–76. discussion 76–79. [PMC free article] [PubMed] [Google Scholar]
- 50.Weakley DR, Jr, Birch E, Kip K. The role of anisometropia in the development of accommodative esotropia. J AAPOS. 2001;5:153–157. doi: 10.1067/mpa.2001.114662. [DOI] [PubMed] [Google Scholar]
- 51.Legras R, Hornain V, Monot A, et al. Effect of induced anisometropia on binocular through-focus contrast sensitivity. Optom Vis Sci. 2001;78:503–509. doi: 10.1097/00006324-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 52.Simpson T. The suppression effect of simulated anisometropia. Ophthalmic Physiol Opt. 1991;11:350–358. [PubMed] [Google Scholar]
- 53.Oguz H, Oguz V. The effects of experimentally induced anisometropia on stereopsis. J Pediatr Ophthalmol Strabismus. 2000;37:214–218. doi: 10.3928/0191-3913-20000701-08. [DOI] [PubMed] [Google Scholar]
- 54.Brooks SE, Johnson D, Fischer N. Anisometropia and binocularity. Ophthalmology. 1996;105:1139–1143. doi: 10.1016/s0161-6420(96)30555-1. [DOI] [PubMed] [Google Scholar]
- 55.Tomac S, Birdal E. Effects of anisometropia on binocularity. J Pediatr Ophthalmol Strabismus. 2001;38:27–33. doi: 10.3928/0191-3913-20010101-09. [DOI] [PubMed] [Google Scholar]
- 56.Holopigian K, Blake R, Greenwald MJ. Selective losses in binocular vision in anisometropic amblyopes. Vision Res. 1986;26:621–630. doi: 10.1016/0042-6989(86)90010-6. [DOI] [PubMed] [Google Scholar]
- 57.Wensveen JM, Harwerth RS, Smith EL., III Clinical suppression in monkeys reared with abnormal binocular visual experience. Vision Res. 2001;41:1593–1608. doi: 10.1016/s0042-6989(00)00319-9. [DOI] [PubMed] [Google Scholar]
- 58.Kiorpes L, Wallman J. Does experimentally-induced amblyopia cause hyperopia in monkeys? Vision Res. 1995;35:1289–1297. doi: 10.1016/0042-6989(94)00239-i. [DOI] [PubMed] [Google Scholar]
- 59.Bradley A, Freeman RD. Contrast sensitivity in anisometropic amblyopia. Invest Ophthalmol Vis Sci. 1981;21:467–476. [PubMed] [Google Scholar]
- 60.Hess RF, Holliday IE. The spatial localization deficit in amblyopia. Vision Res. 1992;32:1319–1339. doi: 10.1016/0042-6989(92)90225-8. [DOI] [PubMed] [Google Scholar]
- 61.McKee SP, Levi DM, Movshon JA. The pattern of visual deficits in amblyopia. J Vis. 2003;3:380–405. doi: 10.1167/3.5.5. [DOI] [PubMed] [Google Scholar]
- 62.Friendly DS, Jaafar MS, Morillo DL. A comparative study of grating and recognition visual acuity testing in children with anisometropic amblyopia without strabismus. Am J Ophthalmol. 1990;110:293–299. doi: 10.1016/s0002-9394(14)76347-0. [DOI] [PubMed] [Google Scholar]
- 63.Chandna A, Pennefather PM, Kovacs I, et al. Contour integration deficits in anisometropic amblyopia. Invest Ophthalmol Vis Sci. 2001;42:875–878. [PubMed] [Google Scholar]
- 64.McKerral M, Polomeno RC, Lepore F, et al. Can interocular pattern reversal visual evoked potential and motor reaction time differences distinguish anisometropic from strabismic amblyopia? Acta Ophthalmol Scand. 1999;77:40–44. doi: 10.1034/j.1600-0420.1999.770110.x. [DOI] [PubMed] [Google Scholar]
- 65.Birch EE, Swanson WH. Hyperacuity deficits in anisometropic and strabismic amblyopes with known ages of onset. Vision Res. 2000;40:1035–1040. doi: 10.1016/s0042-6989(00)00011-0. [DOI] [PubMed] [Google Scholar]
- 66.Hardman Lea SJ, Snead MP, Loades J, et al. Microtropia versus bifoveal fixation in anisometropic amblyopia. Eye. 1991;5:576–584. doi: 10.1038/eye.1991.100. [DOI] [PubMed] [Google Scholar]
- 67.Wensveen JM, Harwerth RS, Smith EL., III Binocular deficits associated with early alternating monocular defocus. I. Behavioral observations. J Neurophysiol. 2003;90:3001–3011. doi: 10.1152/jn.00976.2002. [DOI] [PubMed] [Google Scholar]
- 68.Maguire GW, Smith EL, III, Harwerth RS, et al. Optically induced anisometropia in kittens. Invest Ophthalmol Vis Sci. 1982;23:253–264. [PubMed] [Google Scholar]
- 69.Kiorpes L, Kiper DC, O’Keefe LP, et al. Neuronal correlates of amblyopia in the visual cortex of macaque monkeys with experimental strabismus and anisometropia. J Neurosci. 1998;18:6411–6424. doi: 10.1523/JNEUROSCI.18-16-06411.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Smith EL, III, Chino YM, Ni J, et al. Residual binocular interactions in the striate cortex of monkeys reared with abnormal binocular vision. J Neurophysiol. 1997;78:1353–1362. doi: 10.1152/jn.1997.78.3.1353. [DOI] [PubMed] [Google Scholar]
- 71.Horton JC, Hocking DR, Kiorpes L. Pattern of ocular dominance columns and cytochrome oxidase activity in a macaque monkey with naturally occurring anisometropic amblyopia. Vis Neurosci. 1997;14:681–689. doi: 10.1017/s0952523800012645. [DOI] [PubMed] [Google Scholar]
- 72.Horton JC, Stryker MP. Amblyopia induced by anisometropia without shrinkage of ocular dominance columns in human striate cortex. Proc Natl Acad Sci U S A. 1993;90:5494–5498. doi: 10.1073/pnas.90.12.5494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Moseley MJ, Fielder AR, Irwin M, et al. Effectiveness of occlusion therapy in ametropic amblyopia: a pilot study. Br J Ophthalmol. 1997;81:956–961. doi: 10.1136/bjo.81.11.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Clarke MP, Wright CM, Hrisos S, et al. Randomised controlled trial of treatment of unilateral visual impairment detected at preschool vision screening. BMJ. 2003;327:1251–1256. doi: 10.1136/bmj.327.7426.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pediatric Eye Disease Investigator Group. A prospective, pilot study of treatment of amblyopia in children 10 to <18 years old. Am J Ophthalmol. 2004;137:581–583. doi: 10.1016/j.ajo.2003.08.043. [DOI] [PubMed] [Google Scholar]
- 76.Choi MY, Lee KM, Hwang JM, et al. Comparison between anisometropic and strabismic amblyopia using functional magnetic resonance imaging. Br J Ophthalmol. 2001;85:1052–1056. doi: 10.1136/bjo.85.9.1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Miki A, Liu GT, Goldsmith ZG, et al. Decreased activation of the lateral geniculate nucleus in a patient with anisometropic amblyopia demonstrated by functional magnetic resonance imaging. Ophthalmologica. 2003;217:365–369. doi: 10.1159/000071353. [DOI] [PubMed] [Google Scholar]
- 78.Hoyt CS, Nickel BL, Billson FA. Ophthalmological examination of the infant. Developmental aspects. Surv Ophthalmol. 1982;26:177–189. doi: 10.1016/0039-6257(82)90078-9. [DOI] [PubMed] [Google Scholar]
- 79.Sokol S. Abnormal evoked potential latencies in amblyopia. Br J Ophthalmol. 1983;67:310–314. doi: 10.1136/bjo.67.5.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shan Y, Moster ML, Roemer RA, et al. Abnormal function of the parvocellular visual system in anisometropic amblyopia. J Pediatr Ophthalmol Strabismus. 2000;37:73–78. doi: 10.3928/0191-3913-20000301-05. [DOI] [PubMed] [Google Scholar]
- 81.Yu M, Brown B, Edwards MH. Investigation of multifocal visual evoked potential in anisometropic and esotropic amblyopes. Invest Ophthalmol Vis Sci. 1998;39:2033–2040. [PubMed] [Google Scholar]
- 82.Donahue SP, Wall M, Kutzko KE, et al. Automated perimetry in amblyopia: a generalized depression. Am J Ophthalmol. 1999;27:312–321. doi: 10.1016/s0002-9394(98)90327-0. [DOI] [PubMed] [Google Scholar]
- 83.Donahue SP, Moore P, Kardon RH. Automated pupil perimetry in amblyopia: generalized depression in the involved eye. Ophthalmology. 1997;104:2161–2167. doi: 10.1016/s0161-6420(97)30046-3. [DOI] [PubMed] [Google Scholar]
- 84.Ikeda H, Wright MJ. Properties of LGN cells in kittens reared with convergent squint: a neurological demonstration of amblyopia. Exp Brain Res. 1976;25:63–77. doi: 10.1007/BF00237326. [DOI] [PubMed] [Google Scholar]
- 85.Lempert P, Porter L. Dysversion of the optic disc and axial length measurements in a presumed amblyopic population. J AAPOS. 1998;2:207–213. doi: 10.1016/s1091-8531(98)90054-4. [DOI] [PubMed] [Google Scholar]
- 86.Lempert P. The axial length/disc area ratio in anisometropic hyperopic amblyopia: a hypothesis for decreased unilateral vision associated with hyperopic anisometropia. Ophthalmology. 2004;111:304–308. doi: 10.1016/j.ophtha.2003.05.020. [DOI] [PubMed] [Google Scholar]
- 87.Greenwald MJ, Folk ER. Afferent pupillary defects in amblyopia. J Pediatr Ophthalmol Strabismus. 1983;20:63–67. doi: 10.3928/0191-3913-19830301-06. [DOI] [PubMed] [Google Scholar]
- 88.Portnoy JZ, Thompson HS, Lennarson L, et al. Pupillary defects in amblyopia. Am J Ophthalmol. 1983;96:609–614. doi: 10.1016/s0002-9394(14)73418-x. [DOI] [PubMed] [Google Scholar]
- 89.Kase M, Nagata R, Yoshida A, et al. Pupillary light reflex in amblyopia. Invest Ophthalmol Vis Sci. 1984;25:467–471. [PubMed] [Google Scholar]
- 90.Yen MY, Cheng CY, Wang AG. Retinal nerve fiber layer thickness in unilateral amblyopia. Invest Ophthalmol Vis Sci. 2004;45:2224–2230. doi: 10.1167/iovs.03-0297. [DOI] [PubMed] [Google Scholar]
- 91.Bozkurt B, Irkec M, Orhan M, et al. Thickness of the retinal nerve fiber layer in patients with anisometropic and strabismic amblyopia. Strabismus. 2003;11:1–7. doi: 10.1076/stra.11.1.1.14091. [DOI] [PubMed] [Google Scholar]
- 92.Mintz-Hittner HA, Fernandez KM. Successful amblyopia therapy initiated after age 7 years: compliance cures. Arch Ophthalmol. 2000;118:1535–1541. doi: 10.1001/archopht.118.11.1535. [DOI] [PubMed] [Google Scholar]
- 93.Kaye SB, Chen SI, Price G, et al. Combined optical and atropine penalization for the treatment of strabismic and anisometropic amblyopia. J AAPOS. 2002;6:289–293. doi: 10.1067/mpa.2002.127920. [DOI] [PubMed] [Google Scholar]
- 94.Hussein MA, Coats DK, Muthialu A, et al. Risk factors for treatment failure of anisometropic amblyopia. J AAPOS. 2004;8:429–434. doi: 10.1016/j.jaapos.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 95.Levartovsky S, Oliver M, Gottesman N, et al. Long-term effect of hypermetropic anisometropia on the visual acuity of treated amblyopic eyes. Br J Ophthalmol. 1998;82:55–58. doi: 10.1136/bjo.82.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cobb CJ, Russell K, Cox A, et al. Factors influencing visual outcome in anisometropic amblyopes. Br J Ophthalmol. 2002;86:1278–1281. doi: 10.1136/bjo.86.11.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hardman Lea SJ, Loades J, Rubinstein MP. The sensitive period for anisometropic amblyopia. Eye. 1989;3:783–790. doi: 10.1038/eye.1989.122. [DOI] [PubMed] [Google Scholar]
- 98.Flynn JT, Schiffman J, Feuer W, et al. The therapy of amblyopia: an analysis of the results of amblyopia therapy utilizing the pooled data of published studies. Trans Am Ophthalmol Soc. 1998;96:431–450. [PMC free article] [PubMed] [Google Scholar]
- 99.Flynn JT, Woodruff G, Thompson JR, et al. The therapy of amblyopia: an analysis comparing the results of amblyopia therapy utilizing two pooled data sets. Trans Am Ophthalmol Soc. 1999;97:373–390. [PMC free article] [PubMed] [Google Scholar]
- 100.Loudon SE, Polling JR, Simonsz HJ. A preliminary report about the relation between acuity increase and compliance in patching therapy for amblyopia. Strabismus. 2002;10:79–82. doi: 10.1076/stra.10.2.79.8143. [DOI] [PubMed] [Google Scholar]
- 101.Loudon SE, Polling JR, Simonsz HJ. Electronically measured compliance with occlusion therapy for amblyopia is related to visual acuity increase. Graefes Arch Clin Exp Ophthalmol. 203;241:176–180. doi: 10.1007/s00417-002-0570-z. [DOI] [PubMed] [Google Scholar]
- 102.Mohan K, Saroha V, Sharma A. Successful occlusion therapy for amblyopia in 11- to 15-year-old children. J Pediatr Ophthalmol Strabismus. 2004;41:89–95. doi: 10.3928/0191-3913-20040301-08. [DOI] [PubMed] [Google Scholar]
- 103.Scheiman MM, Hertle RW, Beck RW, et al. A randomized trial of treatment of atropine in children 7 to <18 years old. Arch Ophthalmol. 2005;123:557–558. doi: 10.1001/archopht.123.4.437. [DOI] [PubMed] [Google Scholar]
- 104.Beardsell R, Clarke S, Hill M. Outcome of occlusion treatment for amblyopia. J Pediatr Ophthalmol Strabismus. 1999;36:19–24. doi: 10.3928/0191-3913-19990101-05. [DOI] [PubMed] [Google Scholar]
- 105.Lee SY, Isenberg SJ. The relationship between stereopsis and visual acuity after occlusion therapy for amblyopia. Ophthalmology. 2003;110:2088–2092. doi: 10.1016/S0161-6420(03)00865-0. [DOI] [PubMed] [Google Scholar]
- 106.Autrata R, Rehurek J. Clinical results of excimer laser photorefractive keratectomy for high myopic anisometropia in children: four-year follow-up. J Cataract Refract Surg. 2003;29:694–702. doi: 10.1016/s0886-3350(02)01896-5. [DOI] [PubMed] [Google Scholar]
- 107.Holopainen JM, Moilanen JA, Saaren-Seppala H, et al. Unilateral photorefractive keratectomy for myopic anisometropia improves contrast sensitivity. Ophthalmology. 2004;111:1095–1101. doi: 10.1016/j.ophtha.2003.09.038. [DOI] [PubMed] [Google Scholar]
- 108.Paysse EA, Hamill MB, Hussein MA, et al. Photorefractive keratectomy for pediatric anisometropia: safety and impact on refractive error, visual acuity, and stereopsis. Am J Ophthalmol. 2004;138:70–78. doi: 10.1016/j.ajo.2004.01.044. [DOI] [PubMed] [Google Scholar]
- 109.Ciner EB, Dobson V, Schmidt PP, et al. A survey of vision screening policy of preschool children in the United States. Surv Ophthalmol. 1999;43:445–457. doi: 10.1016/s0039-6257(99)00021-1. [DOI] [PubMed] [Google Scholar]
- 110.Simons K. Preschool vision screening: rationale, methodology and outcome. Surv Ophthalmol. 1996;41:3–30. doi: 10.1016/s0039-6257(97)81990-x. [DOI] [PubMed] [Google Scholar]
- 111.Repka MX. Use of Lea symbols in young children. Br J Ophthalmol. 2002;86:489–490. doi: 10.1136/bjo.86.5.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Becker R, Hubsch S, Graf MH, et al. Examination of young children with Lea symbols. Br J Ophthalmol. 2002;86:513–516. doi: 10.1136/bjo.86.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Graf MH, Becker R, Kaufmann H. Lea symbols: visual acuity assessment and detection of amblyopia. Graefes Arch Clin Exp Ophthalmol. 2000;238:53–58. doi: 10.1007/s004170050009. [DOI] [PubMed] [Google Scholar]
- 114.Simons K, Avery KE, Novak A. Small-target random dot stereogram and binocular suppression testing for preschool vision screening. J Pediatr Ophthalmol Strabismus. 1996;33:104–113. doi: 10.3928/0191-3913-19960301-09. [DOI] [PubMed] [Google Scholar]
- 115.Committee on Practice and Ambulatory Medicine and Section on Ophthalmology; American Academy of Pediatrics. Use of photoscreening for children’s vision screening. Pediatrics. 2002;109:524–525. doi: 10.1542/peds.109.3.524. [DOI] [PubMed] [Google Scholar]
- 116.Cooper CD, Gole GA, Hall JE, et al. Evaluating photoscreeners II: MTI and fortune videorefractor. Aust N Z J Ophthalmol. 1999;27:387–398. doi: 10.1046/j.1440-1606.1999.00261.x. [DOI] [PubMed] [Google Scholar]
- 117.Tong PY, Macke JP, Bassin RE, et al. Screening for amblyopia in preverbal children with photoscreening photographs. III. Improved grading criteria for hyperopia. Ophthalmology. 2000;107:1630–1636. doi: 10.1016/s0161-6420(00)00336-5. [DOI] [PubMed] [Google Scholar]
- 118.Donahue SP, Johnson TM, Leonard-Martin TC. Screening for amblyogenic factors using a volunteer lay network and the MTI photoscreener. Initial results from 15,000 preschool children in a statewide effort. Ophthalmology. 2000;107:1637–1644. doi: 10.1016/s0161-6420(00)00298-0. [DOI] [PubMed] [Google Scholar]
- 119.Ottar WL, Scott WE, Helgado SI. Photoscreening for amblyogenic factors. J Pediatr Ophthalmol Strabismus. 1995;32:289–295. doi: 10.3928/0191-3913-19950901-06. [DOI] [PubMed] [Google Scholar]
- 120.Enzenauer RW, Freeman HL, Larson MR, et al. Photoscreening for amblyogenic factors by public health personnel: the Eyecor Camera System. Ophthalmic Epidemiol. 2000;7:1–12. [PubMed] [Google Scholar]
- 121.Kennedy RA, Thomas DE. Evaluation of the iScreen digital screening system for amblyogenic factors. Can J Ophthalmol. 2000;35:258–262. doi: 10.1016/s0008-4182(00)80075-7. [DOI] [PubMed] [Google Scholar]
- 122.Kovtoun TA, Arnold RW. Calibration of photoscreeners for single-subject, contact-induced hyperopic anisometropia. J Pediatr Ophthalmol Strabismus. 2004;41:150–158. doi: 10.3928/0191-3913-20040501-07. [DOI] [PubMed] [Google Scholar]
- 123.Williams C, Lumb R, Harvey I, et al. Screening for refractive errors with the Topcon PR2000 Pediatric Refractometer. Invest Ophthalmol Vis Sci. 2000;41:1031–1037. [PubMed] [Google Scholar]
- 124.Angi MR, Pucci V, Forattini F, et al. Results of photorefractometric screening for amblyogenic defects in children aged 20 months. Behav Brain Res. 1992;49:91–97. doi: 10.1016/s0166-4328(05)80198-6. [DOI] [PubMed] [Google Scholar]
- 125.Simons BD, Siatkowski RM, Schiffman JC, et al. Pediatric photoscreening for strabismus and refractive errors in a high-risk population. Ophthalmology. 1999;106:1073–1080. doi: 10.1016/S0161-6420(99)90243-9. [DOI] [PubMed] [Google Scholar]
- 126.Donahue SP, Arnold RW, Ruben JB. Preschool vision screening: What should we be detecting and how should we report it? Uniform guidelines for reporting results of preschool vision screening studies. J AAPOS. 2003;7:314–316. doi: 10.1016/s1091-8531(03)00182-4. [DOI] [PubMed] [Google Scholar]
- 127.Steele G, Ireland D, Block S. Cycloplegic autorefraction results in pre-school children using the Nikon Retinomax Plus and the Welch Allen SureSight. Optom Vis Sci. 2003;80:573–577. doi: 10.1097/00006324-200308000-00010. [DOI] [PubMed] [Google Scholar]
- 128.Cordonnier M, Kallay O. Non-cycloplegic screening for refractive errors in children with the hand-held autorefractor Retinomax: final results and comparison with non-cycloplegic photoscreening. Strabismus. 2001;9:59–70. doi: 10.1076/stra.9.2.59.701. [DOI] [PubMed] [Google Scholar]
- 129.Schimitzek T, Haase W. Efficiency of a video-autorefractometer used as a screening device for amblyogenic factors. Graefes Arch Clin Exp Ophthalmol. 2002;240:710–716. doi: 10.1007/s00417-002-0524-5. [DOI] [PubMed] [Google Scholar]
- 130.Schimitzek T, Schworm HD. Wave-front analysis as screening technique for amblyogenic ametropia with and without cycloplegia. Strabismus. 2003;11:133–143. doi: 10.1076/stra.11.3.133.16648. [DOI] [PubMed] [Google Scholar]
- 131.Donahue SP, Johnson TM. Age-based refinement of referral criteria for photoscreening. Ophthalmology. 2001;108:2309–2314. doi: 10.1016/s0161-6420(01)00810-7. [DOI] [PubMed] [Google Scholar]
- 132.Donahue SP, Johnson TJ, Ottar W, et al. Sensitivity of photoscreening to detect high magnitude amblyogenic factors. Referral Criteria for Photoscreening. J AAPOS. 2002;6:86–92. doi: 10.1067/mpa.2002.121168. [DOI] [PubMed] [Google Scholar]
- 133.Tong PY. Screening for amblyopia in preverbal children with photoscreening photographs: II. Sensitivity and specificity of the MTI photoscreener. Ophthalmology. 2000;107:1623–1629. doi: 10.1016/s0161-6420(00)00293-1. [DOI] [PubMed] [Google Scholar]
- 134.Donahue SP, Johnson TM. Screening with photoscreening photographs. Ophthalmology. 2004;111:604–605. doi: 10.1016/j.ophtha.2003.12.028. [DOI] [PubMed] [Google Scholar]
- 135.Wright K, Edelman PM, Walonker F, et al. Reliability of fixation preference testing in diagnosing amblyopia. Arch Ophthalmol. 1986;104:449–555. doi: 10.1001/archopht.1986.01050160105023. [DOI] [PubMed] [Google Scholar]
- 136.Diamond GR. Esotropia. In: Yanoff M, Duker JS, eds, Ophthalmology. 2nd ed. St Louis: Mosby; 2004:580.
- 137.von Noorden GK. A reassessment of essential esotropia. Edward Jackson Memorial Lecture. Am J Ophthalmol. 1988;105:1–10. doi: 10.1016/0002-9394(88)90113-4. [DOI] [PubMed] [Google Scholar]
- 138.Donahue SP. How often are spectacles prescribed in normal preschool children? J AAPOS. 2004;8:224–229. doi: 10.1016/j.jaapos.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 139.DeVries J. Anisometropia in children: analysis of a hospital population. Br J Ophthalmol. 1985;69:504–507. doi: 10.1136/bjo.69.7.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Abolfotouh MA, Badawi I, Faheem Y. Prevalence of amblyopia among schoolboys in Abha city, Asir Region, Saudi Arabia. J Egypt Public Health Assoc. 1994;69:19–30. [PubMed] [Google Scholar]
- 141.Attebo K, Mitchell P, Cumming R, et al. Prevalence and causes of amblyopia in an adult population. Ophthalmology. 1998;105:154–159. doi: 10.1016/s0161-6420(98)91862-0. [DOI] [PubMed] [Google Scholar]
- 142.Lithander J. Prevalence of amblyopia with anisometropia or strabismus among schoolchildren in the Sultanate of Oman. Acta Ophthalmol Scand. 1998;76:658–662. doi: 10.1034/j.1600-0420.1998.760604.x. [DOI] [PubMed] [Google Scholar]
- 143.Brown SA, Weih LM, Fu CL, et al. Prevalence of amblyopia and associated refractive errors in an adult population in Victoria, Australia. Ophthalmic Epidemiol. 2000;7:249–258. [PubMed] [Google Scholar]
- 144.Tong L, Saw SM, Chia KS, et al. Anisometropia in Singapore school children. Am J Ophthalmol. 2004;137:474–479. doi: 10.1016/j.ajo.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 145.Mayer DL, Hansen RM, Moore BD, et al. Cycloplegic refractions in healthy children aged 1 through 48 months. Arch Ophthalmol. 2001;119:1625–1628. doi: 10.1001/archopht.119.11.1625. [DOI] [PubMed] [Google Scholar]