Abstract
There has been vigorous debate between the “social capital” and “neomaterialist” interpretations of the epidemiological evidence regarding socioeconomic determinants of health. We argue that levels of income inequality, social capital, and health in a community may all be consequences of more macrolevel social and economic processes that influence health across the life course.
We discuss the many reasons for the prominence of social capital theory, and the potential drawbacks to making social capital a major focus of social policy. Intervening in communities to increase their levels of social capital may be ineffective, create resentment, and overload community resources, and to take such an approach may be to “blame the victim” at the community level while ignoring the health effects of macrolevel social and economic policies.
IT HAS LONG BEEN established that socioeconomic factors are major determinants of health and mortality.1 The term “socioeconomic status” is used in widely varying contexts; sometimes it is used to refer to social class, sometimes to social status, sometimes to position in a social hierarchy, and often simply as a generic term for specific socioeconomic factors such as income, education, area characteristics, and occupation. These are all strongly related to overall health,2 although the patterns are different for different diseases. Childhood deprivation is important for some causes of adult ill health (e.g., stomach cancer, stroke), later life circumstances are important for others (e.g., accidents, violence, lung cancer), and cumulative socioeconomic circumstances are important for yet others (e.g., coronary heart disease, chronic obstructive pulmonary disorder).3
The recent renewed interest in socioeconomic determinants of health has stemmed in part from the increases in socioeconomic inequalities, particularly in anglophone countries, during the 1980s and 1990s. There has also been particular emphasis on evidence that income inequality is positively associated with national mortality rates4,5 as well as with state mortality rates within the United States.6,7 If this evidence is correct, this is clearly of crucial importance, since it implies that “development” in itself may not automatically be good for health, and that the way in which the gross national product (GNP) is shared within the population may be as important as its absolute level. Thus, in some countries, a large increase in GNP has been accompanied by little benefit in terms of health, whereas some relatively poor countries (e.g., China, Jamaica, Costa Rica) and states (e.g., Kerala in India) have made major improvements in health care and life expectancy.8,9
This much would be accepted by most researchers into socioeconomic determinants of health. However, there is little agreement on the explanations for these patterns or what they mean for social policy. In particular, there has been vigorous debate between proponents of the “social capital” and “neomaterialist” interpretations of the epidemiological evidence10–15 that mirror, at the community level, the traditional debates between proponents of the structural/materialist and behavioral/lifestyle interpretations of the epidemiological evidence at the individual level.16 A common line of argument for the social capital approach has been that (1) income inequality is a major determinant of national mortality rates; (2) the mechanism by which this occurs is that increased income inequality reduces “social capital,” which in turn results in poorer health in the relevant communities; and (3) the most likely explanation for this mechanism involves psychosocial factors.
The evidence for these propositions and the possible reasons why social capital theory has received such prominence deserve consideration, as do the potential drawbacks of making social capital a major focus of social policy. Levels of income inequality, social capital, and health in a community may all be consequences of more macrolevel social and economic processes that influence health across the life course. The danger is that focusing on communities and intervening to increase their levels of social capital may be ineffective, create resentment, and overload community resources, and to take such an approach may be to “blame the victim” at the community level while ignoring the health effects of macrolevel social and economic policies.
INCOME INEQUALITY AND HEALTH
Rodgers was the first to formally examine the links between income inequality and health, arguing that the curvilinear association between individual income and health meant that countries with greater income inequality would experience lower life expectancy.17 Wilkinson independently rediscovered the relationship between income inequality and health,18 and he argued, in a seminal paper that has sparked a decade-long debate, that income inequality had an effect on population health independent of the effect of individual income.4
The evidence that income inequality is one of the major determinants of population health is tenuous. For example, the last 15 years has seen a continuing substantial fall in mortality rates in New Zealand at a time when the country has experienced a major increase in income inequality19 (Figure 1 ▶). Similar patterns have been seen in Finland, Britain, Japan, and the United States.12 Furthermore, absolute levels of GNP continue to be associated with national mortality rates, although the associations may be weaker for wealthier countries.12,20 This is not to say that factors such as income inequality are not important. However, they are probably not the major determinants of population health, at least in the short term, since they cannot alter what has gone before and life expectancy is dependent on lifetime social circumstances, not simply on recent social conditions.3,15
FIGURE 1—
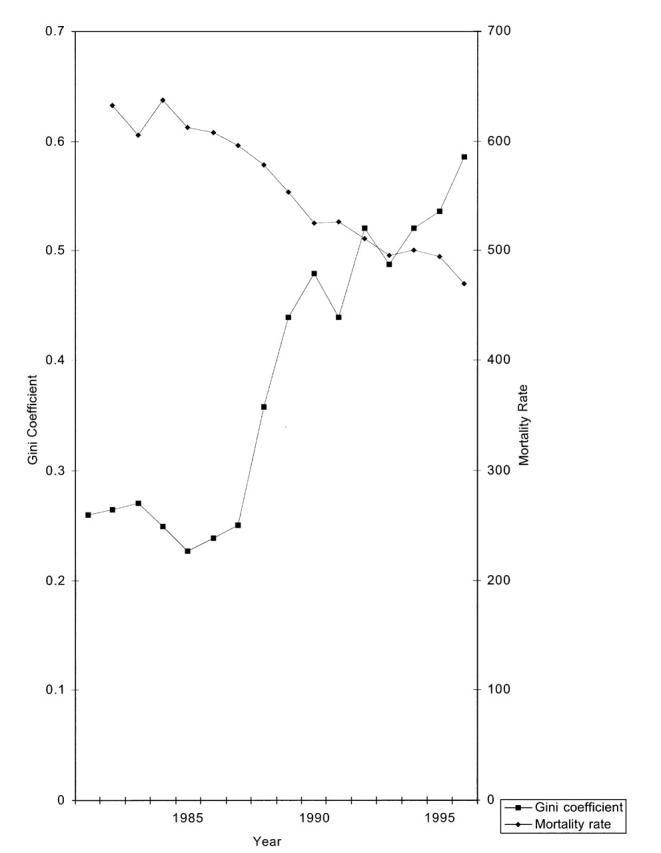
Time trends in income inequality (measured by the Gini coefficient) and age-standardized mortality rates (per 100 000 population) in New Zealand.
There are some exceptions to this, including the rapid and catastrophic fall in life expectancy in Eastern Europe after 1989,21 which was influenced in part by an increase in binge drinking consequent on drastic economic restructuring. But even during this period of considerable economic change (and increase in income inequality), the changes in cause-specific mortality rates continue to reveal the influence of social conditions many decades ago. For example, stomach cancer rates continued their steady decline,22 probably reflecting improvements in living conditions in the childhood of these cohorts and thus cohort decreases in Helicobacter pylori infection in people now dying in late adulthood.3
A recent comprehensive analysis of the cross-national associations between income inequality and health23 produced quite different findings from those of Wilkinson.4,5 The associations that did exist between income inequality and health were largely limited to child health outcomes, whereas a positive association between income inequality and national mortality rates was seen for those aged 65 years and older. The authors commented that higher income inequality within the United States and within the selected countries included in Wilkinson’s original analysis4 was probably associated with the unequal distribution of many powerful determinants of health, whereas this may not be the case for the larger group of countries included in the more recent analysis. A striking feature of the updated examination of the association of income inequality and health is that even with more recent data the associations are seen for the group of countries originally included by Wilkinson, but not in the larger group of countries (Figure 2 ▶).
FIGURE 2—
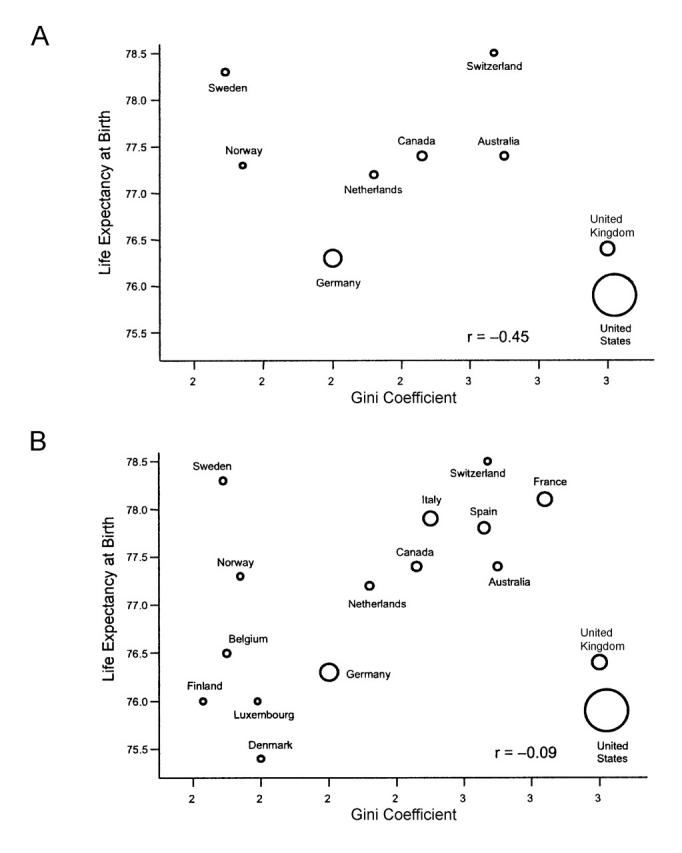
Income inequality and life expectancy (from Lynch et al.23) for the same 9 countries reported by Wilkinson et al.,10 but with information updated to 1989–1991 (A) and with the addition of the other 7 countries for which income inequality data are now available for the period 1989–1991.
Note. Circles represent country population size.
Across the United States degree of income inequality is associated with a wide range of factors that may influence health, with greater income inequality associated with higher unemployment, higher proportions of people without health insurance, lower per capita medical spending, lower rates of high school graduation, and a higher proportion of the population with non-European ancestry.7 Indeed, statistical adjustment for ethnicity statistically accounts for all of the association between income inequality and health within the United States.24,25 Similarly, adjustment for education—a marker of early-life social circumstances as well as later-life socioeconomic position26—also accounted for all of the association between income inequality and mortality in a recent US study.27 Furthermore, recent studies from Denmark28 and Japan29 found that the associations between income inequality and mortality28 or self-rated health29 disappeared when the findings were adjusted for individual income. Thus, the “evidence favoring a negative correlation between income inequality and life expectancy has disappeared,”30(p1) and it appears that the associations that do exist are primarily due to effects of individual income rather than true contextual effects of income inequality.31
Thus income inequality and health outcomes may be related across the United States because in this context income inequality reflects many current and past social and environmental factors that have important health effects. Across countries, the association between current income inequality and these social and environmental factors may or may not exist depending on the choice of countries and their historical, cultural, political, and economic contexts. Jurisdictions that allow income inequality to increase may often be those that also systematically underinvest in education, welfare, health care, and a range of social institutions that serve as safety nets for people in unfavorable circumstances, and in these circumstances income inequality, both currently and in the past, will be related to health outcomes. When this dependence no longer holds—for example, when a rapid increase in income inequality has occurred but bodies such as trade unions have been able to resist the dismantling of hard-won rights such as health care and welfare—the association with health outcomes will not be seen. In this view the association between income inequality and health is not automatic; this is in contrast to the position that sees income inequality as having a necessary and direct influence on health outcomes through the consequences of perceptions of inequality on psychological factors and community-level social capital.5
SOCIAL CAPITAL
The concept of social capital has recently been mobilized within the health field primarily as a possible explanation for findings with respect to inequalities in health, and in particular for the relationship between income inequality and health (see, for example, Kawachi et al.32). However the concept of social capital was developed for different purposes, and its major relevance is outside the area of health inequalities.33–41 Social capital has been defined as “the features of social organization, such as civic participation, norms of reciprocity, and trust in others, that facilitate cooperation for mutual benefit.”32(p1491) Social capital is thus a community-level variable whose individual-level counterpart is measured by a person’s social networks, although social capital is probably more than just the sum of individual-level social networks. Since social networks are associated with health at the individual level (although the direction of causal association and degree to which it is due to confounding by other factors is uncertain), it is plausible that social capital could be associated with health at the community level.
The social capital hypothesis is supported by evidence that indicators of social capital, such as trust and belonging to and volunteering for community organizations, are strongly related to mortality rates. In the United States, Kawachi et al.32 analyzed data from 39 states and found that mortality rates were strongly related to per capita density of membership in voluntary groups and by levels of “social trust” as measured by the proportion of state residents who believed statements such as “Most people would try to take advantage of you if they got the chance.” The associations remained, but were diminished, when the analyses were adjusted for poverty levels. The authors concluded that disinvestment in social capital appears to be one of the pathways through which income inequality influences mortality rates.
Taken as whole, however, the evidence regarding social trust and health is less than compelling: associations are inconsistent and appear to be confined to particular countries, particularly the United States. A recent cross-national study found that measures of social capital were only weakly and inconsistently associated with cause-specific mortality and that greater distrust was actually associated with lower mortality from coronary heart disease.23 In contrast, associations of some country-level variables with health outcomes were as we would expect given our knowledge of the determinants of health. For example, the percentage of the government made up by women—an indicator of empowerment—was strongly inversely related to infant and child mortality rates and to the prevalence of low birthweight.23
Even where associations have been observed between measures of social capital and population health, it is by no means clear that these associations are causal. At the individual level, it is very difficult to isolate the effects of factors such as income, education, occupation, and control, and it is even more difficult to do so with factors defined at the community level.42 In general, communities that have high levels of participation and trust may be healthier, but it is by no means established that this association is causal. Some advocates of the social capital hypothesis acknowledge the possibility of other interpretations of the income inequality findings,32,43,44 but to date there has been little research that would enable us to distinguish between these competing interpretations.
That social capital is an important determinant of population health and health differentials is a hypothesis that needs to be explored and tested against competing hypotheses, not a ready-made explanation that can simply be “verified” in isolation. It is not sufficient simply to show that social capital is associated with mortality rates, while adjusting for an incomplete set of confounders such as income alone.32 If social capital is to be a major focus of health and social policy then it is necessary to show that levels and changes of social capital explain population mortality patterns better than other competing theories.
THE PSYCHOSOCIAL INTERPRETATION
When it is claimed that social capital is causally associated with population health, it is not clear what the etiological pathways are considered to be. In a recent review, Macinko and Starfield45 document the diverse ways in which “social capital” has been operationalized, as variables that can be computed only at the community level (e.g., effectiveness of local government, crime levels, numbers of demonstrations or strikes) and as aggregates of individual data (e.g., the proportion of respondents reporting low levels of trust in their neighbors or government, or the percentage of individuals involved in community groups).
Social capital can be—and has been—defined broadly to include virtually all socioeconomic aspects of society,46 particularly by proponents of the hypothesis that social capital is an important determinant of population health.47,48 To link these broad social factors to health, several possible causal mechanisms have been proposed, including the influence of social cohesion on health-related behaviors, differential procurement of social services, and variations in individuals’ access to life opportunities and material resources (e.g., health care, education) that are consequent on greater inequality.47,48 However, a narrower psychosocial definition of the mechanisms linking social capital and health has been the most influential.5
The psychosocial interpretation proposes that socioeconomic differences affect health through perceptions of place in the social hierarchy.32 Thus, the growing gap between rich and poor has led to declining levels of social cohesion or “trust.” Wilkinson has argued that perceived low position in the social hierarchy produces negative emotions such as shame and distrust, which are translated into poor health through psycho-neuro-endocrine mechanisms as well as through stressinduced behaviors such as smoking.4,5 At the same time, these negative emotions are translated into antisocial behavior and reduced participation in community organizations.
Wilkinson has argued for the psychosocial interpretation as the best explanation for the associations between income inequality and mortality in some wealthy countries.4 This argument has in part been based on animal experiments49,50 that are of questionable applicability in human populations—as some of the animal experimenters themselves acknowledge.51 However, a major argument for the psychosocial interpretation has been that “a shift in emphasis from absolute to relative standards indicates a fall in the importance of the direct physical effect of material circumstances relative to psychosocial influences.”4(p168)
In fact, little evidence has been given for this assertion. It appears to be based on the assumption that in wealthy societies the poor have enough for the daily necessities of life, since there are countries that have the same average level of per capita income as that of the poor in rich countries, but where average levels of health are considerably better than the health of the poor in rich countries. The health problems of the poor therefore cannot be due to material conditions and must therefore be due to psychosocial factors. However, a given level of income may be sufficient for daily life in a developing country but quite inadequate in a wealthy country in which access to a telephone, a television, a car, and a job may be necessary to participate in daily life and to have access to good health care.
A given income—even when corrected for purchasing parity across countries—has different consequences in societies with different degrees of inequality. For example, in cities like London, where there are relatively large numbers of wealthy people who can support very high property prices, even people with incomes that, on an international scale, appear high cannot afford decent accommodation. The fact that such competition is local (the number of wealthy individuals in London will not influence house prices in Naples) is commensurate with the finding that inequalities in health according to income are seen within countries, but not across countries.
A life-course perspective is important when considering a second major argument for the psychosocial perspective. This is the suggestion that since the gradient in health outcomes is continuous across the socioeconomic spectrum it cannot be due to absolute material standards. Thus, with respect to the Whitehall study of British civil servants, it has been argued that the “gradient in mortality among civil servants who are not poor argues for the importance of psychosocial factors linked to position in the hierarchy.”52(p1127) However, this argument ignores the earlier life experience of these civil servants. The top-grade civil servants will almost all have come from privileged backgrounds, while the lower-grade (but still middle-class) civil servants will in many cases have come from poorer backgrounds. Indeed, the top-grade civil servants are considerably taller and have a considerably lower risk of mortality due to stomach cancer than the lower-grade civil servants, suggesting that their childhood circumstances were more favorable.53 Many studies have demonstrated that deprived circumstances in childhood increase the risk of poor health outcomes in adulthood, independent of later-life social circumstances.3,54 Thus, when lifetime social circumstances are taken into consideration, the gradient is not mysterious and need not be attributed to (somewhat mystical) psychosocial influences.
RISK FACTOR OR OUTCOME?
Levels of income inequality, social capital, and health in a community may all be consequences of macrolevel social and economic processes that influence health across the life course. When this dependency is not seen, then the health associations of income inequality and social capital will not be seen. It is hardly surprising that an increasingly individualistic free market–oriented society, in which job security is diminished, benefits have been cut, and the social security safety net is increasingly fragile, produces both reduced levels of trust and community participation and increased inequalities in income and health. New Zealand, for example, has large socioeconomic inequalities and invests relatively little in education and other forms of human and social capital.55 If social capital (and psychosocial consequences of position in a hierarchy) were important direct determinants of health, it would be expected that overall health levels should have deteriorated in recent years in New Zealand. They have not. This is consistent with life-course notions, since the lifetime experiences of successive cohorts in New Zealand certainly improved across the 20th century, in line with their improving health status.
This interpretation of recent developments in New Zealand is consistent with the main alternative explanations for socioeconomic differences in health. Neomaterialist explanations argue that interpretations should start with the structural and material causes of inequalities rather than just with perceptions of inequality. Lynch et al. present the tongue-in-cheek metaphor of airline travel and the effects on well-being of traveling in economy class.11 Under a psychosocial interpretation, these health effects might be due to the feelings of resentment, and consequent loss of social capital, engendered when economy-class passengers walk past the first-class seats on leaving the plane (or perhaps the differing levels of trust in the airline experienced by economy- and first-class passengers). A neomaterialist interpretation would emphasize the cramped and uncomfortable seats in economy, the consequent inability of passengers to sleep, and the fact that improvements in economy class are often resisted by those who travel in first class. Although it is important not to push the analogy too far, it does make the point that we should start by examining the material, institutional, and political factors that are major determinants both of community levels of social capital and of health inequalities. In this framework, psychosocial mechanisms may also play a role, but as just one of a number of sets of potential pathways between the macrolevel forces and health.
WHY IS “SOCIAL CAPITAL” FASHIONABLE?
Despite the relatively weak nature of the evidence connecting social capital to population health, the concept has received considerable publicity, and in some instances enthusiastic support and advocacy, in recent years.
At first glance, the concept of social capital seems to have a lot in its favor. It combines the economic concept of “capital” with social concepts such as “trust” and “fairness.” Thus “social capital” takes its place alongside “economic capital” and “human capital” as something fundamental to the smooth functioning of society and economic growth. When the importance of social factors is presented in economic terminology, these factors are made more acceptable to the currently dominant political and economic orthodoxy.
In fact, the concept of “social capital” is largely a repackaging of old ideas such as “community capacity,” “empowerment,” and “social support.”12,33,46 The concept has thus revitalized a field of research that had produced relatively weak and inconsistent findings with major problems of interpretation as to whether the observed associations were causal or were due to reverse causality (ill health reduces an individual’s or community’s social networks) or confounding (low levels of social networks are associated with ill health but the association, rather than being causal, is due to other socioeconomic factors that influence both phenomena). Similar considerations apply to the conceptualizing of social capital in other fields. Thus it has been suggested that both social capital and the supposed economic and social benefits of social capital are outcomes of political processes that underlie them both, rather than being causally linked.33
A second possible reason for the concept’s recent popularity is that the term “social capital” is flavored with an economic essence46 in which the consideration of social factors is justified as a means to the end of economic growth (for those with a market-driven ideology) as well as an end in itself (for those with a more communitarian ideology).56 Thus, it appears to represent a “third way,” in which the community forms the missing link between macrolevel economic policies and individual-level behaviors. In practice, the term has been widely embraced across the political spectrum by different interest groups who have interpreted it according to their own agendas. In particular, it has been used to depoliticize issues of social and economic development.33
BOWLING ALONE OR BLOWING ALONG?
Finally, it is instructive to examine how the concept of social capital has colonized health discourse and the ways in which health researchers have influenced the social capital theorists. One of the most influential social capital theorists has certainly been Robert Putnam, whose 1993 book Making Democracy Work34 is considered seminal. A later article and then book, engagingly titled Bowling Alone35,36—with the lone bowler standing as the symbol of the victim of declining social capital—has had much influence on academics, social policy analysts, and politicians.57 How has Putnam’s interest in health developed? In Making Democracy Work he explicitly states that health should not be considered an outcome of social capital: “[W]e must be careful not to give governments credit (or blame) for matters beyond their control. In the language of policy analysis, we want to measure ‘outputs’ rather than ‘outcomes’—health care rather than mortality rates. . . . Health depends on factors like diet and lifestyle that are beyond the control of any democratic government.”34(p65–66)
However, Putnam’s work was eagerly taken up by health researchers, and only 7 years after excluding health as an outcome Putnam claims that “[o]f all the domains in which I have traced the consequences of social capital, in none is the importance of social connectedness so well established as in the case of health and well-being”; that “bowling alone represents one of the nation’s most serious public health challenges”; that social capital is as well-established and as important as smoking as a cause of ill health, and that these findings are heartening because “it’s easier to join a group than to lose weight, exercise regularly and quit smoking.”36(p326–331) These are strong and certain claims for someone who previously thought social capital should not be studied as a cause of health outcomes. They are also seriously worrying conclusions if the last quote is taken seriously by people responsible for health policy (or by people who decide not to quit smoking because they have joined the Rotary Club).
Clearly, social capital theorists are successful social entrepreneurs, know a bandwagon when they see one, and know when it is time to change horses. It is not just in the health field that Putnam seems to have been influenced by his followers to change his conclusions about his work. In Making Democracy Work34 it is clear that historical-path dependence—in which forces set in train at one particular time are relatively autonomous and do not change rapidly with changing circumstances, and thus have long-term effects—is taken to be of considerable importance, while in later work Putnam seems to suggest that rapid social change could yield rapid results.33
Putnam is not an epidemiologist, and we cannot expect him to realize that much of what he says with respect to health makes no epidemiological sense. We might hope that his enthusiasm would be restrained by health researchers; however, health researchers have also been too willing to see gold where it does not exist. Thus, remarkably, when Lochner et al. showed a very weak effect of income inequality on mortality (by quintile, low to high income inequality, relative risks of death were 1.00, 1.08, 1.10, 1.11, and 1.12) and a very strong effect of family income (relative risks 1.00, 1.52, 2.14, 2.69), they focused their discussion on the tiny effects of income inequality—which they oversell and which may well be residual effects of other variables—being as yet more of “[t]he evidence linking income inequality to both population and individual health outcomes [that] continues to grow.”58(p390)
DOWNPLAYING SOCIAL CAPITAL
Is there any harm in embracing a concept that has such wide appeal and that seems to suggest useful interventions that we can all feel good about? Almost everyone is in favor of encouraging community development and participation in community organizations. If this not only is good for health but may also be good for economic growth, then what is the problem? Surely interventions that increase community levels of social capital must be good for health, and at least cannot do any harm, so are the social capital and neomaterialist explanations not on the same side, in that they both stress the importance of socioeconomic factors, even if they have different interpretations of the evidence?
Well, maybe, but we know that research that focuses on individual behaviors without considering the wider social context can too easily result in blaming the victim and producing interventions that can be ineffective or even harmful.16,59 It would be accepted by most proponents of the social capital hypothesis that simply urging individuals not to smoke tobacco is ineffective, because individual smoking behavior is largely socially determined. Analogously, it is important to acknowledge the macrolevel economic policies that strongly influence levels of social capital in a particular community.33 Otherwise, intervening in communities to increase their levels of social capital may be as ineffective, or as damaging, as intervening to encourage individuals to change their lifestyles. Usually such an approach doesn’t work, creates resentment, overloads community resources, and “blames the victim.” Thus, as Lynch et al. have noted, “there has been little discussion of the possibility that focusing on what materially and politically disenfranchised communities can do for themselves may be akin to victim blaming at the community level.”11(p1201)
A further issue is that increases in social capital for some sections of the community may represent decreases in social capital for others. In the US context, it has been argued that levels of social capital may be high in the National Rifle Association or the Mafia, but this may not be good for public health.12 Similarly, Putnam recently remarked on the increases in social capital occurring during wartime, with respect to the effects in the United States of the so-called war against terrorism,60 but this increase in social capital in one country is certainly not beneficial to the health of infants and children in Afghanistan and Iraq.
It should also be noted that, even within a particular community or demographic group, increased community involvement may not necessarily be good for health.61 The modern move to the cities and away from traditional communities has occurred not only for economic reasons but has often also involved a break from stifling social networks that reinforce traditional values, both positive and negative. Strong social networks can be coercive and sources of strain as well as support.11,61 Of course, as Sen notes, “if a traditional way of life has to be sacrificed to escape grinding poverty or minuscule longevity . . . then it is the people directly involved who must have the opportunity to participate in deciding what should be chosen.”9(p31) The point is that it is possible to overromanticize traditional community values and that many people choose, and should have the right to choose, to escape from traditional social networks that are harmful to their health.
Finally, the vagueness of the concept of social capital makes it widely acceptable but open to widely varying interpretations, and it offers little in the way of effective interventions. The danger is that this vague, popular concept diverts attention from the macrolevel economic and social policies that set the bounds within which communities and individuals live.33 There is no great mystery as to why socioeconomic and health inequalities have increased in countries such as New Zealand in the last 20 years.62,63 Health researchers should consider the health effects of macrolevel policies and should not study community-level factors (such as social capital) or individual-level factors (such as lifestyle) out of context. To take these macrolevel economic policies as a given and then study only factors that may have a marginal effect on health is unscientific and leads to social policy that is at best ineffective and at worst harmful to the health of individuals, communities, and populations.
Acknowledgments
The Centre for Public Health Research receives funding from the Health Research Council of New Zealand.
We wish to thank Tony Blakely, Brian Easton, Tony Gattrell, Ichiro Kawachi, and Andrew Sporle for their comments on the draft of this commentary.
Peer Reviewed
References
- 1.Townsend P, Davidson N. Inequalities in Health: The Black Report. Harmondsworth, England: Penguin; 1982.
- 2.Lynch J, Kaplan G. Socioeconomic position. In: Berkman LF, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press; 2000:13–35.
- 3.Davey Smith G, Gunnell D, Ben-Shlomo Y. Life-course approaches to socio-economic differentials in cause-specific adult mortality. In: Leon D, Walt G, eds. Poverty, Inequality and Health. Oxford, England: Oxford University Press; 2000:88–124.
- 4.Wilkinson RG. Income distribution and life expectancy. BMJ. 1992;304:165–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilkinson RG. Unhealthy Societies: The Afflictions of Inequality. London, England: Routledge; 1996.
- 6.Kennedy BP, Kawachi I, Prothrow-Stith D. Income distribution and mortality: cross-sectional ecological study of the Robin Hood index in the United States. BMJ. 1996;312:1004–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaplan GA, Pamuk ER, Lynch JW, et al. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. BMJ. 1996;312:999–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sen A. Levels of Poverty: Policy and Change. Washington, DC: World Bank; 1980. World Bank Staff Working Paper No. 401.
- 9.Sen A. Development as Freedom. New York, NY: Oxford University Press, 1999.
- 10.Kawachi I, Kennedy BP. Income inequality and health: pathways and mechanisms. Health Services Res. 1999;34:215–227. [PMC free article] [PubMed] [Google Scholar]
- 11.Lynch JW, Davey Smith G, Kaplan GA, House JS. Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. BMJ. 2000;320:1200–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lynch J, Due P, Muntaner C, Davey Smith G. Social capital—is it a good investment strategy for public health? J Epidemiol Community Health. 2000;54:404–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blane D, Bartley M, Davey Smith G. Disease aetiology and materialistic explanations of socio-economic mortality differentials. Eur J Public Health. 1997; 7: 385–391. [Google Scholar]
- 14.Marmot M, Wilkinson RG. Psychosocial and material pathways in the relation between income and health: a response to Lynch et al. BMJ. 2001;322:1233–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davey Smith G. Income inequality and mortality: why are they related? Income inequality goes hand in hand with underinvestment in human resources. BMJ. 1996;312:987–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pearce N. Traditional epidemiology, modern epidemiology, and public health. Am J Public Health. 1996;86:678–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodgers GB. Income and inequality as determinants of mortality: an international cross-section analysis [reprinted in Int J Epidemiol.2002;31:533–538]. Popul Stud. 1979;33:343–351. [DOI] [PubMed] [Google Scholar]
- 18.Wilkinson R. Liberty, fraternity, equality. Int J Epidemiol. 2002;31:538–543. [DOI] [PubMed] [Google Scholar]
- 19.Easton B. What has happened in New Zealand to income distribution and poverty levels? In: Shaver S, Saunders P, eds. Social Policy for the 21st Century: Justice and Responsibility. Proceedings of the National Social Policy Conference, Sydney, 21–23 July, 1999. Sydney, New South Wales, Australia: University of New South Wales; 1999. Social Policy Research Centre (SPRC) Reports and Proceedings no. 142.
- 20.Saunders P. Do inequalities in income cause inequalities in health? In: Crampton P, Howden-Chapman P, eds. Socioeconomic Inequalities and Health. Wellington, New Zealand: Victoria University; 1997:9–36.
- 21.Leon DA, Chenet L, Shkolnikov VM, et al. Huge variation in Russian mortality rates 1984–94: artefact, alcohol, or what? Lancet. 1997;350:383–388. [DOI] [PubMed] [Google Scholar]
- 22.Shkolnikov V, McKee M, Leon DA. Changes in life expectancy in Russia in the mid-1990s. Lancet. 2001;357:917–921. [DOI] [PubMed] [Google Scholar]
- 23.Lynch J, Davey Smith G, Hillemeier M, Shaw M, Raghunathan T, Kaplan G. Income inequality, the psychosocial environment, and health: comparisons of wealthy nations. Lancet. 2001;358:194–200. [DOI] [PubMed] [Google Scholar]
- 24.Deaton A. Relative deprivation, inequality, and mortality. National Bureau of Economic Research Working Paper No. W8099. January 2001. Available at: http://papers.nber.org/papers/W8099. Accessed November 4, 2002.
- 25.Deaton A. The convoluted story of international studies of inequality and health. Int J Epidemiol. 2002;31:546–549. [DOI] [PubMed] [Google Scholar]
- 26.Davey Smith G, Hart C, Hole D, et al. Education and occupational social class: which is the more important indicator of mortality risk? J Epidemiol Community Health. 1998;52:153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Muller A. Education, income inequality and mortality: a multiple regression analysis. BMJ. 2002;324:23–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osler M, Prescott E, Gronbaek M, Christensen U, Due P, Engholm G. Income inequality, individual income, and mortality in Danish adults: analysis of pooled data from two cohort studies. BMJ. 2002;324:13–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shibuya K, Hashimoto H, Yano E. Individual income, income distribution, and self-rated health in Japan: cross sectional analysis of nationally representative sample. BMJ. 2002;324:16–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mackenback JP. Income inequality and population health. BMJ. 2002;324:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lynch J, Davey Smith G. Income inequality and health: the end of the story? Int J Epidemiol. 2002;31:549–551. [DOI] [PubMed] [Google Scholar]
- 32.Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87:1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harriss J. Depoliticizing Development: The World Bank and Social Capital. New Delhi, India: Leftword Books; 2001.
- 34.Putnam RD. Making Democracy Work. Princeton, NJ: Princeton University Press; 1993.
- 35.Putnam RD. Bowling alone: America’s declining social capital. J Democracy. 1995;6:65–78. [Google Scholar]
- 36.Putnam RD. Bowling Alone. New York, NY: Simon & Schuster; 2000.
- 37.Bourdieu P. The forms of capital. In: Richardson JG, ed. Handbook of Theory and Research for the Sociology of Education. New York, NY: Greenwood Press; 1986.
- 38.Coleman JS. Social capital in the creation of human capital. Am J Sociology. 1988;94:S95–S120. [Google Scholar]
- 39.Baron S, Field J, Schuller T, eds. Social Capital: Critical Perspectives. Oxford, England: Oxford University Press; 2000.
- 40.Woolcock M, Narayan D. Social capital: implications for development theory, research and policy. World Bank Res Observer. 2000;15:225–249. [Google Scholar]
- 41.Foley MW, Edwards B. Is it time to disinvest in social capital? J Public Policy. 1999;19:141–173. [Google Scholar]
- 42.Blakeley T, Woodward A. Ecological effects in multi-level studies. J Epidemiol Community Health. 2000;54:367–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kawachi I, Kennedy BP. Income distribution, social capital, and mortality. In: Crampton P, Howden-Chapman P, eds. Socioeconomic Inequalities and Health. Wellington, New Zealand: Victoria University; 1997.
- 44.Kawachi I, Kennedy BP. The Health of Nations: Why Inequality Is Harmful to Your Health. New York, NY: New Press; 2002.
- 45.Macinko J, Starfield B. The utility of social capital in research on health determinants. Milbank Q. 2001;79:387–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Leeder S, Dominello A. Social capital and its relevance to health and family policy. Aust N Z J Public Health. 1999;23:424–429. [DOI] [PubMed] [Google Scholar]
- 47.Kawachi I, Kennedy BP. Income inequality and health: pathways and mechanisms. Health Serv Res. 1999;34:215–277. [PMC free article] [PubMed] [Google Scholar]
- 48.Kawachi I, Berkman L. Social cohesion, social capital and health. In: Berkman LF, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press; 2000:174–190.
- 49.Sapolsky R, Alberts S, Altmann J. Hypercortisolism associated with social subordinance or social isolation among wild baboons. Arch Gen Psychiatry. 1997;54:1137–1143. [DOI] [PubMed] [Google Scholar]
- 50.Shively CA, Clarkson TB. Social status and coronary artery atherosclerosis in female monkeys. Arterioscler Thromb. 1994;14:721–726. [DOI] [PubMed] [Google Scholar]
- 51.Sapolsky RM. Hormonal correlates of personality and social contexts: from non-human to human primates. In: Panter–Brick C, Worthman CM, eds. Hormones, Health and Behavior. New York, NY: Cambridge University Press; 1999:18–46.
- 52.Marmot M, Bobak M. International comparators and poverty and health in Europe. BMJ. 2000;321:1124–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Davey Smith G, Ben-Shlomo Y, Lynch J. Life course approaches to inequalities in coronary heart disease risk. In: Stansfeld SA, Marmot MG, eds. Stress and the Heart. London, England: BMJ Books; 2002.
- 54.Davey Smith G, McCarron P, Okasha M, McEwen J. Social circumstances in childhood and cardiovascular disease mortality: prospective observational study. J Epidemiol Community Health. 2001;55:340–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Howden-Chapman P, Blakeley T, Blaiklock AJ, Kiro C. Closing the health gap. N Z Med J. 2000;113:301–302. [PubMed] [Google Scholar]
- 56.Labonte R. Social capital and community development: practitioner emptor. Aust N Z J Public Health. 1999;23:430–433. [DOI] [PubMed] [Google Scholar]
- 57.Muntaner C, Lynch J. Social capital, class, gender and race conflict, and population health: an essay review of Bowling Alone’s implications for social epidemiology. Int J Epidemiol. 2002;31:261–267. [Google Scholar]
- 58.Lochner K, Pamuk E, Makuc D, Kennedy BP, Kawachi I. State-level income inequality and individual mortality risk: a prospective, multilevel study. Am J Public Health. 2001;91:385–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McKinlay JB. The promotion of health through planned sociopolitical change: challenges for research and policy. Soc Sci Med. 1993;36:109–117. [DOI] [PubMed] [Google Scholar]
- 60.Putnam R. A better society in a time of war. New York Times. 19October2001.
- 61.Kunitz S. Disease and Social Diversity. New York, NY: Oxford University Press; 1994.
- 62.Shaw M, Dorling D, Gordon D, Davey Smith G. The Widening Gap: Health Inequalities and Policy in Britain. Bristol, England: Policy Press; 1999.
- 63.Pearce N. Economic policy and health in the year of the family. N Z Med J. 1994;107:379–81. [PubMed] [Google Scholar]


