Abstract
Differences in health across ethnic groups have been documented in the United States and the United Kingdom. The extent to which socioeconomic inequalities underlie such differences remains contested, with many instead focusing on cultural or genetic explanations. In both the United States and the United Kingdom, data limitations have greatly hampered investigations of ethnic inequalities in health. Perhaps foremost of these is the inadequate measurement of ethnicity, but also important is the lack of good data on socioeconomic position, particularly data that address life-course issues. Other elements of social disadvantage, particularly experiences of racism, are also neglected.
The author reviews existing evidence and presents new evidence to suggest that social and economic inequalities, underpinned by racism, are fundamental causes of ethnic inequalities in health.
Differences in health across ethnic groups, in terms of both morbidity and mortality, have been repeatedly documented in both the United States1–9 and the United Kingdom.10–16 In the United States, non-Hispanic Blacks and Native Americans are reported to have higher rates of mortality than do non-Hispanic Whites, though these decrease at older ages, while Hispanic people and Asian/Pacific Islanders have lower rates of mortality than non-Hispanic Whites. This suggests considerable heterogeneity in experience across ethnic/racial groups, with some minority groups doing well, others doing badly, and the differences possibly varying across the life course. In the United Kingdom, although mortality data are not available by ethnic group, the data on immigrant mortality rates and morbidity again suggest heterogeneity of experience across minority groups. For most outcomes, Bangladeshi and Pakistani people report the poorest health, followed by Caribbean people and then Indian people, with Chinese and White people having the best health.
Although there is now substantial data describing differences across ethnic groups, the factors underlying such differences, in particular the role that socioeconomic inequalities may play, remain contested. While in 1845 Engels attributed the poor health and mortality record of Irish people living in England to their poor social circumstances,17 and in 1916 Trask concluded that lower death rates among Whites than Blacks in the United States reflected more favorable social circumstances rather than any inherent differences,18 the role that socioeconomic position may play remains the subject of considerable debate. Some claim that socioeconomic inequalities make a minimal or no contribution to ethnic inequalities in health,19 others suggest that even if they do contribute, the cultural and genetic elements of ethnicity must also play a role,20 and others argue that ethnic inequalities in health are predominantly determined by socioeconomic inequalities.21,22 Given the growing empirical and theoretical sophistication of work on ethnic inequalities in health, it is worrying that crude explanations based on cultural stereotypes and claims of genetic difference persist,23–25 despite a lack of concrete evidence, more than 100 years of research exposing the limitations of the assumptions underlying such explanations,26 and growing evidence that the obvious social and economic inequalities faced by ethnic minority groups are likely to be a fundamental explanation.5,7,15,27–29
In the United Kingdom there has, of course, been a long tradition of investigating socioeconomic inequalities in health. However, in the main this work has not been drawn upon by those investigating ethnic inequalities in health, perhaps as a consequence of Marmot and colleagues’ now classic study of immigrant mortality rates.10 Published shortly after the Black Report had firmly placed inequalities in health on the research agenda,30 this study used a combination of British census and death certificate data to explore the relationship between country of birth and mortality rates. A central finding was that there was no relationship between occupational class and mortality for immigrant groups, even though there was a clear relationship for those born in the United Kingdom. These findings led to the conclusion that differences in socioeconomic position could not explain the higher mortality rates found in some migrant groups in the United Kingdom.10 It was not until 1997 that socioeconomic position reappeared in published national data exploring the relationship between ethnicity and health in the United Kingdom.12,13 But again, conclusions drawn from analysis of immigrant mortality data did not appear to support a socioeconomic explanation,12 although those on morbidity did.13
In the United States, there is also a long tradition of investigating ethnic/racial disparities in health; indeed, and in contrast with the situation in the United Kingdom, in recent decades there has been greater interest in health differences according to “race” than in socioeconomic differentials in health. This is partly due to the limited data on socioeconomic position available in routine US health statistics and the use of race as a surrogate for poverty in many analyses.1 Implicit in this approach is the mistaken assumption that ethnic minority groups in the United States are uniformly disadvantaged and therefore that socioeconomic differentials in health status within ethnic minority groups do not need to be considered. Indeed, until recently there have been few examinations of the socioeconomic stratification of health within ethnic minority groups in the United States.3,8,31 On the other hand, the contribution of socioeconomic factors to, in particular, Black–White health differentials in the United States has been investigated in many studies.2,3,7,32,33 These studies have, however, often been limited by small sample sizes or a reliance on administrative data in which information on factors other than ethnicity and socioeconomic position was not available.
In fact, in both the United States and the United Kingdom, data limitations have greatly hampered investigations of ethnic inequalities in health and how they might be structured by social and economic disadvantages, particularly as obvious data limitations are often ignored by investigators. Perhaps the main limitation is the inadequate measurement of ethnicity in many studies, with the heterogeneity of ethnic groups ignored, observer-assigned ethnicity used instead of self-reported ethnicity, and surrogates such as country of birth used instead of ethnic origin. Also important is the lack of good, or any, data on current socioeconomic position in health studies, let alone data that can deal with changes over the life course and other elements of social disadvantage, such as inequalities related to geography and experiences of racial discrimination and harassment.34
This article illustrates the impact of some of these limitations on how data are interpreted and suggests that social and economic inequalities are fundamental causes of ethnic inequalities in health. It also suggests that an adequate understanding of racism is fundamental to understanding ethnic inequalities in health.
SOCIOECONOMIC PATTERNS WITHIN ETHNIC GROUPS
It is now reasonably clear that a socioeconomic patterning of health is present within ethnic groups in industrialized countries. Analysis of the US Multiple Risk Factor Intervention Trial (MRFIT) data7 showed that all-cause mortality rates over its 16-year follow-up period had a very clear relationship to mean income in the area of residence of respondents for both Black and White men (individual socioeconomic data were not included in the study, so income data from the 1980 US Census were used to determine median family income of White and Black households in the area of residence of the individual). Mortality rates increased with decreasing income, resulting in a twofold difference in mortality rates between those in the top annual income band ($27 500 or higher) and those in the bottom annual income band (less than $10 000) for both Black and White men.7
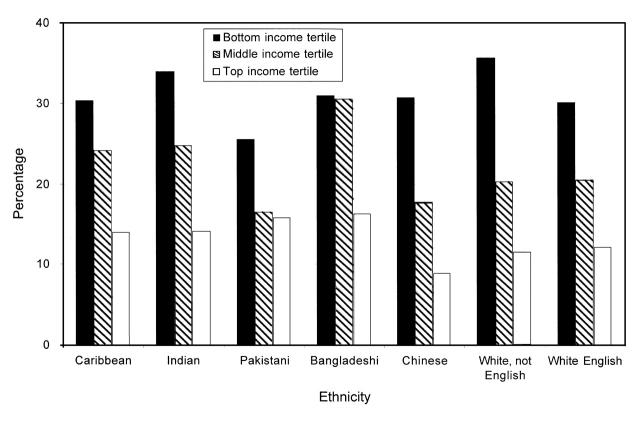
Figure 1 ▶ reports a new analysis of data from the 1999 Health Survey for England.16 (The Health Survey for England is an annual survey commissioned by the UK Department of Health. Interviews are administered to a nationally representative sample identified through a stratified sampling design, which is usually followed by a biomedical assessment. In 1999, the Health Survey for England focused on ethnic minority people.) It shows rates of reporting fair or bad general health for each of the ethnic groups included in the study (in response to a question asking respondents to rate their health as very good, good, fair, bad, or very bad) by household income (equivalized to account for variations in household size and banded into tertiles). As with the US MRFIT all-cause mortality data, there is a clear relationship between reported general health and income for each ethnic group.
FIGURE 1.
—Ethnic differences in reported fair or bad general health by household income: 1999 Health Survey for England.
Important here is that both sets of data point to heterogeneity within broad ethnic groupings. It is misleading, for example, to consider that Black Americans are uniformly disadvantaged in terms of their health; those in better socioeconomic positions have better health. There is nothing inevitable, or inherent, in the link between being Black American or Bangladeshi, for example, and a greater risk of mortality and morbidity.
SOCIOECONOMIC PATTERNING OF HEALTH ACROSS ETHNIC GROUPS
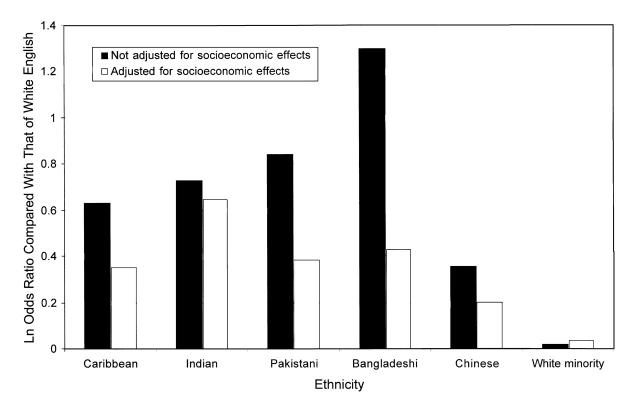
If socioeconomic position is related to health within groups, it seems probable that inequalities in socioeconomic position might be related to ethnic inequalities in health. Figure 2 ▶ explores the impact of socioeconomic factors on ethnic differences in reporting fair or bad general health across a range of ethnic groups in the United Kingdom; as in Figure 1 ▶, a new analysis of data from the 1999 Health Survey for England is presented. Once adjustments had been simultaneously made for a variety of socioeconomic indicators (income, housing tenure, economic activity), there is a clear and large reduction in odds ratio for most ethnic minority groups (to give an accurate visual impression of the size of the change in odds, the natural logarithm of the odds ratio compared with that of White English people is used); exceptions are the White minority (predominately Irish) group (which has an odds close to 1) and the Indian group (for whom the reduction in odds ratio is small). Similarly, analysis of the US MRFIT data showed that standardizing for mean household income in area of residence reduced the relative risk for all-cause mortality of Black compared with White men from 1.47 to 1.19; that is, about two thirds of the elevated mortality risk among Black men was statistically explained by this income measure.7 Conversely, adjusting the Black–White mortality differential for a number of medical risk factors (diastolic blood pressure, serum cholesterol, cigarette smoking, existing diabetes, and prior hospitalization for coronary heart disease) only decreased the relative risk from 1.47 to 1.40.7 This demonstrates that socioeconomic position—as indexed by income of area of residence—is a considerably more important determinant of Black–White differentials in mortality in the United States than biological markers of risk and behavioral factors, such as cigarette smoking or diet.
FIGURE 2.
—Impact of socioeconomic effects on ethnic differences in the reporting of fair or bad general health: 1999 Health Survey for England.
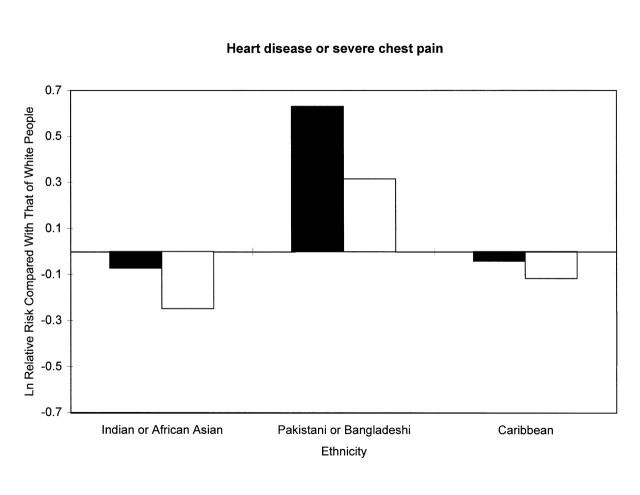
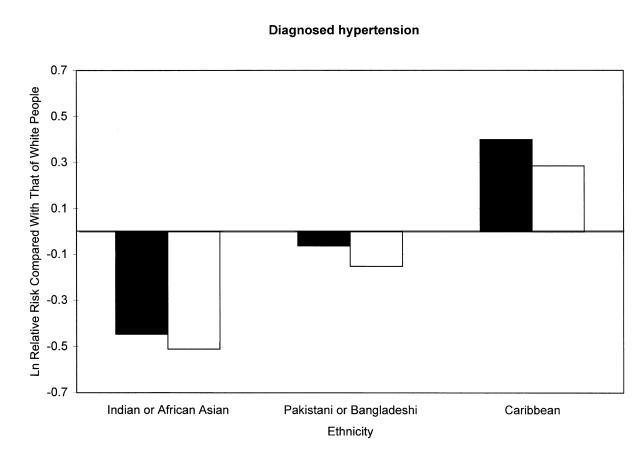
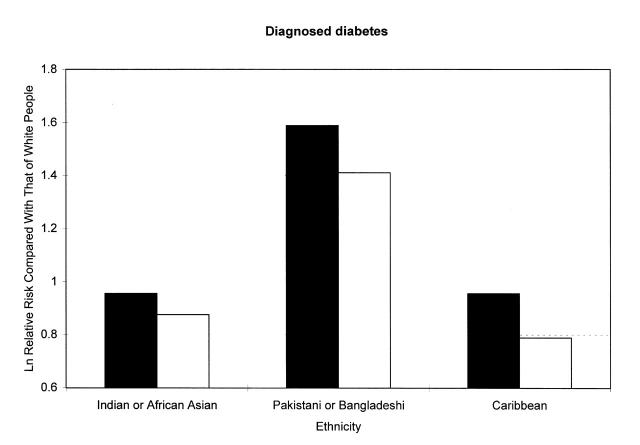
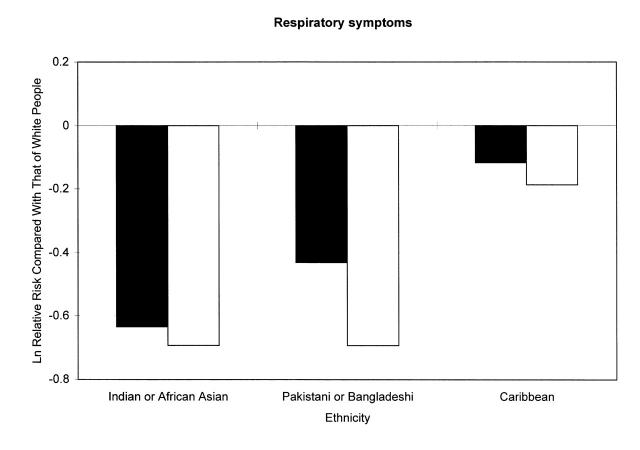
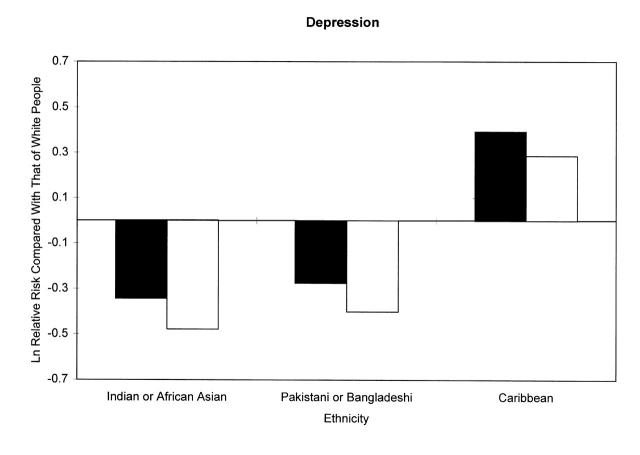
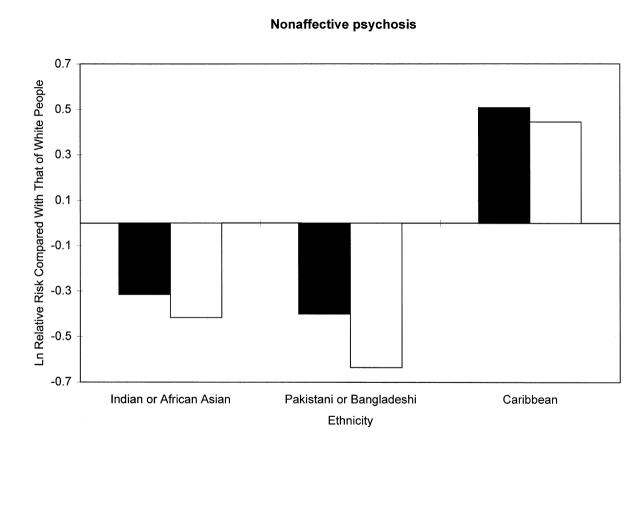
Additional evidence of the importance of socioeconomic inequality is provided by Figure 3 ▶, which explores the contribution of socioeconomic effects to ethnic inequalities in health for 3 broad ethnic minority groups and 6 different health outcomes. (Data are from the UK Fourth National Survey of Ethnic Minorities, a representative survey of the main ethnic minority groups living in Britain, together with a comparison White sample.35 Topics covered included economic position, education, housing, health, ethnic identity, and experiences of racial harassment and discrimination.) Figure 3 ▶ uses the natural logarithm of the relative risk statistic to show how risk of ill health among ethnic minority respondents compared with White respondents changes once socioeconomic position is partially adjusted for use of an indicator of standard of living.15,36 In the figure, a risk equivalent to that for Whites is represented by 0 on the y-axis; a figure above 0 represents a greater risk while a figure below 0 represents a smaller risk. In all cases, the risk for each ethnic minority group compared with Whites is reduced once the socioeconomic control has been applied.
FIGURE 3.
—Impact of standard of living on ethnic inequalities in health: UK Fourth National Survey of Ethnic Minorities.
Overall, then, the impression is that across ethnic groups, across countries, and across outcomes, socioeconomic factors contribute to ethnic inequalities in health. However, these data also raise the possibility that socioeconomic inequalities cannot fully explain ethnic inequalities in health. For most groups and for most outcomes, differences remain once the adjustment for the socioeconomic indicator has been made. It is important to recognize here that the process of standardizing for socioeconomic position when making comparisons across groups, particularly ethnic groups, is not so straightforward. As Kaufman and colleagues point out,37,38 the process of standardization is effectively an attempt to deal with the nonrandom nature of samples used in cross-sectional population studies. Controlling for relevant “extraneous” explanatory factors introduces the appearance of randomization. But this assumes that all necessary factors are accounted for by the measures available, and that particular measures do not contain any residual confounding. Evidence from the Fourth National Survey of Ethnic Minorities clearly illustrates the fallacy in the latter point. In that survey, analysis of ethnic differences in income within class groups showed that within each class group, ethnic minority people had a smaller income than White people.13 Indeed, for the poorest group—Pakistani and Bangladeshi people—differences were twofold and equivalent in size to the difference between the top and bottom class groups in the White population. A similar pattern existed for other indicators of socioeconomic position in the Fourth National Survey of Ethnic Minorities, and similar findings have been reported in the United States.28,39 For example, Oliver and Shapiro report that within occupational groups, White people have higher incomes than Black people; among those below the poverty line, Black people are more likely to remain in this situation than White people; and within income strata, Black people have considerably lower wealth levels than White people and are less likely to be home owners.40
The implication of this is clear; using either single or crude indicators of socioeconomic position is of little use for “controlling out” the impact of socioeconomic position. Within any given level of a particular socioeconomic measure, the social circumstances of ethnic minority people in the United Kingdom and the United States are less favorable than those of White people. This leads to 2 related problems with approaches that attempt to adjust for socioeconomic effects when making comparisons across ethnic groups. First, if socioeconomic position is simply regarded as a confounding factor that needs to be controlled out to reveal the “true” relationship between ethnicity and health, data will be presented and interpreted once controls have been applied. This will result in the impact of socioeconomic factors becoming obscured, and their explanatory role in determining the health of ethnic minority people will be lost. The second problem is that the presentation of “standardized” data allows the problems with such data13,36–38 to be ignored, leaving both the author and reader to assume that all that is left is an “ethnic/race” effect, be that cultural or genetic.
Nevertheless, if these cautions are considered, there are some benefits in attempting to control for socioeconomic effects. In particular, if controlling for socioeconomic effects alters the pattern of ethnic inequalities in health, despite the limitations of the indicators used, we can conclude that at least some of the differences we have uncovered are a result of a socioeconomic effect. Figures 2 and 3 ▶ ▶ have suggested that differences in socioeconomic position make a key contribution to ethnic inequalities in health, particularly if we take seriously cautions on the difficulties of making effective adjustments for socioeconomic position.13,36–38 It is also worth emphasizing that the analyses shown here simply reflect current socioeconomic position; data on the life course and on other forms of social disadvantage were not included and are almost never available in existing studies of ethnic inequalities in health.
AGE, THE LIFE COURSE, AND MIGRATION
There is growing evidence that socioeconomic conditions across the life course can influence current health.41 This could occur in 2 ways. First, an early “exposure,” perhaps prenatal42 or in early childhood, might set an adverse biological process in train. For example, low birthweight, which is strongly influenced by adverse material circumstances acting over the lifetime of the mother, is associated with high rates of diabetes, coronary heart disease, respiratory disease, and hypertension in adult life. Similarly, short stature, influenced by nutrition in early life, is related to an increased risk of respiratory and cardiovascular mortality.41 Second, the impact of socioeconomic disadvantage on health might accumulate across the life course, a process that has been referred to as “weathering” with respect to the health of Black women in the United States.43
Evidence from the Fourth National Survey of Ethnic Minorities suggests that ethnic inequalities in health in the United Kingdom increase with age, with relatively small differences at younger ages and larger differences emerging from the mid-30s onwards.15 Variations in ethnic inequalities in health across the life course are also apparent in US data, but these take the opposite form, with an apparent narrowing of differences at old ages (there has been much discussion of possible “cross-over” effects for Black–White differences and how far these might be an artifact of the data).44,45 The interpretation of the contrasting UK and US patterning of ethnic inequalities in health with age is not straightforward, but such data do point to the need for sophisticated approaches to the explanation of ethnic inequality that takes account of life-course issues. In particular, we need to place ethnic inequalities in health within a wide social context. For example, the increasing ethnic inequalities in health with age in the United Kingdom could reflect a number of coexisting explanations, including accumulation of risks over the life course and the long-term consequences of exposure to hazards in early life. In the UK context, the cross-sectional pattern of increasing differences in risk over age could also reflect differences between first- and second-generation migrants, since older people are first-generation migrants and younger people second-generation migrants. This final point is a reminder of the need to be aware of a number of potential effects related to migration.
Entry into a migrant group will be related to both health and human capital, potentially leading to a healthy migrant effect.10
The childhood experiences of firstgeneration migrants will be very different from those of the second generation; insofar as these lead to long-term adverse health outcomes or to pathways that lead to an accumulation of social and health disadvantage, differences in health across generations might be expected.
The experience of migration itself will occur alongside social and economic upheavals, which might have a direct impact on health.
Return migration might have a significant impact on the apparent relationship between age and ethnic inequalities in health, with entry into a return migrant group being related to both health and economic capital.
The contemporary social and economic experiences of first- and second-generation migrants might be quite different, with the second generation more likely to do well economically and to have less traditional ethnic identities.46
IMPACT OF RACIAL HARASSMENT AND DISCRIMINATION ON HEALTH
Experiences of and awareness of racism appear to be central to the lives of ethnic minority people, and there is growing evidence that these contribute to ethnic inequalities in health. Eighty percent of Black respondents in a US study reported experiencing racial discrimination at some time in their lives.27 Findings from the UK Fourth National Survey of Ethnic Minorities suggested widespread experiences of racial harassment and discrimination among ethnic minority people in the United Kingdom: more than 1 in 8 respondents reported having experienced at least one incident of harassment over the preceding year47; among ethnic minority respondents, there was a widespread belief that employers discriminated against ethnic minority job applicants and widespread experience of such discrimination48; among White people, 1 in 5 said that they were racially prejudiced against Caribbean people and 1 in 4 said they were racially prejudiced against Asian people.47 Indeed, qualitative investigations of experiences of racial harassment and discrimination in the United Kingdom have found that for many people experiences of interpersonal racism are a part of everyday life, that the way they lead their lives is constrained by fear of racial harassment, and that being made to feel different is routine and expected.49,50
Experiences of racial harassment and discrimination appear to be related to health in the few studies that have been conducted. US studies have shown a relationship between self-reported experiences of racial harassment and a range of health outcomes, including hypertension, psychological distress, poorer self-rated health, and days spent unwell in bed; they have also found that differences in rates of hypertension between Black and White respondents were substantially reduced by taking into account reported experiences of, and responses to, racial harassment.5,27,51,52 In the United Kingdom, analyses of the Fourth National Survey of Ethnic Minorities also suggested a relationship between experiences of racial harassment, perceptions of racial discrimination, and a range of health outcomes across ethnic groups.29,53 Table 1 ▶ presents a logistic regression model drawn from these analyses. It shows that reporting experiences of racial harassment and perceiving that employers discriminate against ethnic minority people are independently related to the likelihood of reporting fair or poor health, and that this relationship is independent of socioeconomic effects as indexed by occupational class. This may represent 3 dimensions of social and economic inequality operating simultaneously: economic disadvantage (as measured by occupational class); a sense of being a member of a devalued, low-status group (British employers discriminate); and the personal insult and stress of being a victim of racial harassment.
TABLE 1.
—Racial Harassment, Racial Discrimination, and Risk of Fair or Poor Health: UK Fourth National Survey of Ethnic Minorities
| Fair or Poor Healtha | ||
| Odds Ratiob | 95% Confidence Interval | |
| Experience of racial harassment | ||
| No attack | 1.00 | … |
| Verbal abuse | 1.54 | 1.07, 2.21 |
| Physical attack | 2.07 | 1.14, 3.76 |
| Perception of discrimination | ||
| Fewer than half of employers discriminate | 1.00 | … |
| Most employers discriminate | 1.39 | 1.10, 1.76 |
| Occupational class | ||
| Nonmanual | 1.00 | … |
| Manual | 1.44 | 1.07, 1.94 |
| No full-time worker in the household | 2.42 | 1.82, 3.22 |
aAll ethnic minority groups.
bAdjusted for gender and age.
CONCLUSION
In both the United States and the United Kingdom, there remain ongoing problems with the data available to explore ethnic inequalities in health. Data often do not contain sufficiently detailed information on the ethnicity of respondents to reflect heterogeneity across ethnic groups and heterogeneity within broadly defined ethnic groups. Socioeconomic data are either not collected at all or are collected at very crude levels that are plainly inadequate for drawing comparisons across ethnic groups. Those that are collected invariably reflect current position rather than risks across the life course, and they do not include other dimensions of social inequality, such as experiences of racial harassment and discrimination and geographically based inequalities.
Nevertheless, a large body of convincing evidence now supports the possibility that ethnic inequalities in health are largely a consequence of socioeconomic differentials. This applies in both the United States and the United Kingdom, across a range of ethnic minority groups and outcomes. There is also a growing body of evidence from both countries suggesting that experiences of racial harassment and discrimination, and perceptions of living in a discriminatory society, contribute to ethnic inequalities in health. These findings, however, need to be placed within a wider explanatory framework. There are 2 routes, not mutually exclusive, that can be followed.
First, these findings could be investigated in terms of how they relate to the individual embodiment of social risks. How do such markers of social inequality relate to psychological and biological markers of stress, and how does this translate into disease outcomes? Here, the emphasis is on the causal pathways linking “exposures” to social and economic inequality with disease outcomes. Importantly, the processes involved might vary across ethnic groups, given differences in social context and suggested genetic variations across ethnic groups. For example, from an epidemiological perspective it might be fruitful to explore how social inequality translates into hypertension-related diseases for Black American people in the United States and Black Caribbean people in the United Kingdom but into cardiovascular disease for Pakistani and Bangladeshi people in the United Kingdom.
However, such an approach avoids more fundamental explanations for the health, economic, and social inequalities related to ethnicity. Second, therefore, it is important to consider the centrality of racism to any attempt to explain ethnic inequalities in health. Not only are personal experiences of racism and harassment likely to influence health, but racism as a social force will play a central role in structuring the social and economic disadvantage faced by ethnic minority groups. The socioeconomic differences between ethnic groups should not be considered as somehow autonomous (which is a danger of an approach that attempts to examine the extent to which socioeconomic differentials “explain” ethnic differentials in health). As Oliver and Shapiro demonstrate,40 the socioeconomic disadvantage of Black people in the United States is the outcome of a long history of institutional racism and discrimination that has produced the current levels of disadvantage. Similarly, while the postwar migration of ethnic minority people into the United Kingdom was driven by a shortage of labor, this process and the socioeconomic disadvantage faced by ethnic minority migrants was, and continues to be, structured by a racism that has its roots in colonial history.54,55
It is worth carefully considering the motives for undertaking work on inequalities in health. These motives seem to be related to competing desires to expose the extent and consequences of wider social inequalities and to uncover etiologic processes, and I have argued elsewhere that this focus on etiologic processes has great potential for racializing inequalities in health.56 For studies of inequalities in health to contribute to our understanding of etiology, we need a tight focus on the pathways that lead from social and economic disadvantage to poor health, particularly if we are to meet the requirement that social causes of inequalities in health must be biologically plausible. There is no reason why such pathways should be identical for different health outcomes or for different dimensions of social and economic inequality. However, such a focus on pathways produces an exclusive concern with inequalities in health as an adverse outcome, and how the complex pathways leading to this outcome can be understood and broken. The root cause, wider social inequalities, becomes obscured from view. The policy implications of this are clear: the more difficult and dramatic interventions to address social inequalities can continue to be avoided and public health can focus on improving our understanding of pathways and designing interventions along them. Inequalities in health become a problem requiring technical interventions tailored to individual diseases and individual circumstances; they become a problem for individuals rather than a reflection of social malaise. Williams and colleagues’ comments in this regard are worth citing:
There is a temptation to focus on identified risk factors as the focal point for intervention efforts. In contrast, we indicate that the macrosocial factors and racism are the basic causes of racial differences in health. The risk factors and resources are the surface causes, the current intervening mechanisms. These may change, but as long as the basic causes remain operative, the modification of surface causes alone will only lead to the emergence of new intervening mechanisms to maintain the same outcome.28(p36)
However, understanding how the macrosocial factors indicated by Williams and colleagues operate and designing appropriate policy interventions are by no means straightforward. Certainly, there is a need to recognize the overriding importance of national and historical context on the “making” of ethnic groups, how this is related to economic processes and inequities in economic position, and how this influences the lives of ethnic minority and migrant populations and the disadvantages that they face. Racism can be considered to be fundamentally involved in the structuring of economic, social, and health opportunities for ethnic minority people. At an institutional level, it is clear that discrimination influences the economic opportunities that people have, as well as the quality of health and social services that they receive. In addition, historically racism has fundamentally structured the construction of ethnic minority groups and patterns of migration at both an international level (when, why, and where to) and a national level (which locations, which industries). For example, Fenton,57 building on Eriksen’s work,58 has distinguished 5 types of ethnic-making or migration situations:
Urban minorities, who are often migrant worker populations;
Proto-nations or ethnonational groups, which are peoples who maintain that they are nations and claim some form of self-governance;
Ethnic groups in plural societies, which are the descendants of populations who have typically migrated as coerced, voluntary, or semivoluntary workers;
Indigenous minorities, those dispossessed by colonial settlement;
Postslavery minorities, the descendants of (African) people formerly enslaved in the New World.
While this typology might not be comprehensive, it does point to the different contexts within which ethnicity or race becomes mobilized to form distinct groupings. Implicit is that the differing processes listed will lead to different forms of racialization, of subsequent disadvantage, and to different historical trajectories for the groups concerned. Understanding the process and the context within which it occurs should aid in understanding disadvantage and how it might develop. Understanding how they are related to future trajectories for ethnic minority groups (across generations and cohorts) and individuals (over time) is important to any understanding of ethnic difference, including ethnic inequalities in health, and appropriate policy responses.
Acknowledgments
The author acknowledges the support of NHS Executive London.
The views expressed are those of the author and do not necessarily reflect those of National Health Service (NHS) Executive London.
Peer Reviewed
References
- 1.Health Status of the Disadvantaged: Chart Book 1990. Washington, DC: Dept of Health and Human Services; 1990.
- 2.Rogers R. Living and dying in the USA: sociodemographic determinants of death among blacks and whites. Demography. 1992;29:287–303. [PubMed] [Google Scholar]
- 3.Sorlie P, Rogot E, Anderson R, Johnson NJ, Backlund E. Black-white mortality differences by family income. Lancet. 1992;340:346–350. [DOI] [PubMed] [Google Scholar]
- 4.Rogot E, Sorlie PD, Johnson NJ, Schmitt C. A Mortality Study of 1.3 Million Persons by Demographic, Social and Economic Factors: 1979–1985. Follow-Up, US National Longitudinal Mortality Study. Washington, DC: National Institutes of Health; 1993.
- 5.Krieger N, Rowley DL, Herman AA, Avery B, Philips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. Am J Prev Med. 1993;9(suppl):82–122. [PubMed] [Google Scholar]
- 6.Sorlie PD, Backlund E, Keller J. US mortality by economic, demographic and social characteristics: the National Longitudinal Mortality Study. Am J Public Health. 1995;85:949–956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davey Smith G, Neaton JD, Wentworth D, Stamler R, Stamler J. Mortality differences between black and white men in the USA: contribution of income and other risk factors among men screened for the MRFIT. Lancet. 1998;351:934–939. [DOI] [PubMed] [Google Scholar]
- 8.Pamuk E, Makuc D, Heck K, Reuben C, Lochner K. Socioeconomic Status and Health Chartbook. Health, United States, 1998. Hyattsville, Md: National Center for Health Statistics; 1998.
- 9.Williams DR. Racial variations in adult health status: patterns, paradoxes and prospects. In: Smelser NJ, Wilson WJ, Mitchell F, eds. America Becoming: Racial Trends and Their Consequences. Washington, DC: National Academy Press; 2001:371–410.
- 10.Marmot MG, Adelstein AM, Bulusu L, Office of Population Censuses and Surveys. Immigrant Mortality in England and Wales 1970–78: Causes of Death by Country of Birth. London, England: Her Majesty’s Stationery Office;1984.
- 11.Rudat K. Black and Minority Ethnic Groups in England: Health and Lifestyles. London, England: Health Education Authority; 1994.
- 12.Harding S, Maxwell R. Differences in the mortality of migrants. In: Drever F, Whitehead M, eds. Health Inequalities: Decennial Supplement Series DS No. 15. London, England: The Stationery Office; 1997:108–121.
- 13.Nazroo JY. The Health of Britain’s Ethnic Minorities: Findings From a National Survey. London, England: Policy Studies Institute; 1997.
- 14.Nazroo JY. Ethnicity and Mental Health: Findings From a National Community Survey. London, England: Policy Studies Institute; 1997.
- 15.Nazroo JY. Ethnicity, Class and Health. London, England: Policy Studies Institute; 2001.
- 16.Erens B, Primatesta P, Prior G. Health Survey for England 1999: The Health of Minority Ethnic Groups. London, England: The Stationary Office; 2001.
- 17.Engels F. The Condition of the Working Class in England. Harmondsworth, England: Penguin; 1987.
- 18.Trask JW. The significance of the mortality rates of the coloured population of the United States. Am J Public Health. 1916;6:254–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wild S, McKeigue P. Cross sectional analysis of mortality by country of birth in England and Wales. BMJ. 1997;314:705–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smaje C. The ethnic patterning of health: new directions for theory and research. Sociol Health Illness. 1996;18:139–171. [Google Scholar]
- 21.Navarro V. Race or class versus race and class: mortality differentials in the United States. Lancet. 1990;336:1238–1240. [DOI] [PubMed] [Google Scholar]
- 22.Sheldon TA, Parker H. Race and ethnicity in health research. J Public Health Med. 1992;14:104–110. [PubMed] [Google Scholar]
- 23.Soni Raleigh V, Balarajan R. Suicide and self-burning among Indians and West Indians in England and Wales. Br J Psychiatry. 1992;161:365–368. [DOI] [PubMed] [Google Scholar]
- 24.Gupta S, de Belder A, O’Hughes L. Avoiding premature coronary deaths in Asians in Britain: spend now on prevention or pay later for treatment. BMJ. 1995;311:1035–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stewart JA, Dundas R, Howard RA, Rudd AG, Woolfe CDA. Ethnic differences in incidence of stroke: prospective study with stroke register. BMJ. 1999;318:967–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bhopal R. Is research into ethnicity and health racist, unsound, or important science? BMJ. 1997;314:1751–1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. Am J Public Health. 1996;86:1370–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Williams DR, Lavizzo-Mourey R, Warren RC. The concept of race and health status in America. Public Health Rep. 1994;109:26–41. [PMC free article] [PubMed] [Google Scholar]
- 29.Karlsen S, Nazroo JY. Relation between racial discrimination, social class, and health among ethnic minority groups. Am J Public Health. 2002;92:624–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Townsend P, Davidson N. Inequalities in Health (the Black Report). Middlesex, England: Penguin; 1982.
- 31.Davey Smith G, Wentworth D, Neaton JD, Stamler R, Stamler J. Socioeconomic differentials in mortality risk among men screened for the Multiple Risk Factor Intervention Trial, II: black men. Am J Public Health. 1996;86:497–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sterling T, Rosenbaum W, Weinkam J. Income, race and mortality. J Natl Med Soc Assoc. 1993;85:906–911. [PMC free article] [PubMed] [Google Scholar]
- 33.Rogers RG, Hummer RA, Nam CB, Peters K. Demographic, socioeconomic, and behavioral factors affecting ethnic mortality by cause. Soc Forces. 1996;74:1419–1438. [Google Scholar]
- 34.Williams DR. Racial/ethnic variations in women’s health: the social embeddedness of health. Am J Public Health. 2002;92:588–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Modood T, Berthoud R, Lakey J, et al. Ethnic Minorities in Britain: Diversity and Disadvantage. London, England: Policy Studies Institute; 1997.
- 36.Nazroo JY. Genetic, cultural or socio-economic vulnerability? Explaining ethnic inequalities in health. Sociol Health Illness. 1998;20:710–730. [Google Scholar]
- 37.Kauffman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8:621–628. [PubMed] [Google Scholar]
- 38.Kauffman JS, Long AE, Liao Y, Cooper RS, McGee DL. The relation between income and mortality in US blacks and whites. Epidemiology. 1998;9:147–155. [PubMed] [Google Scholar]
- 39.Lillie-Blanton M, Laveist T. Race/ethnicity, the social environment, and health. Soc Sci Med. 1996;43:83–91. [DOI] [PubMed] [Google Scholar]
- 40.Oliver ML, Shapiro TM. Black Wealth/White Wealth: A New Perspective on Racial Inequality. New York, NY: Routledge; 1995.
- 41.Kuh D, Ben-Shlomo Y. A Life Course Approach to Chronic Disease Epidemiology. Oxford, England: Oxford University Press; 1997.
- 42.Barker D. The foetal and infant origins of inequalities in health in Britain. J Public Health Med. 1991;13:64–68. [PubMed] [Google Scholar]
- 43.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis. 1992;2:207–221. [PubMed] [Google Scholar]
- 44.Kestenbaum B. A description of the extreme age population based on improved Medicare enrollment data. Demography. 1992;29:565–580. [PubMed] [Google Scholar]
- 45.Nam CB. Another look at mortality crossovers. Soc Biol. 1995;42:133–142. [DOI] [PubMed] [Google Scholar]
- 46.Karlsen S, Nazroo JY. Identity and structure: rethinking ethnic inequalities in health. In: Graham H, ed. Understanding Health Inequalities. Buckingham, England: Open University Press; 2000:38–57.
- 47.Virdee S. Racial harassment. In: Modood T, Berthoud R, Lakey J, et al, eds. Ethnic Minorities in Britain: Diversity and Disadvantage. London, England: Policy Studies Institute; 1997:259–289.
- 48.Modood T. Employment. In: Modood T, Berthoud R, Lakey J, et al. Ethnic Minorities in Britain: Diversity and Disadvantage. London, England: Policy Studies Institute; 1997:83–149.
- 49.Virdee S. Racial Violence and Harassment. London, England: Policy Studies Institute; 1995.
- 50.Chahal K, Julienne L. “We Can’t All Be White!”: Racist Victimisation in the UK. London, England: York Publishing Services; 1999.
- 51.Krieger N. Discrimination and health. In: Berkman L, Kawachi I, eds. Social Epidemiology. Oxford, England: Oxford University Press; 2000:36–75.
- 52.James SA, Strogatz DS, Wing SB, Ramsey DL. Socioeconomic status, John Henryism and hypertension in blacks and whites. Am J Epidemiol. 1987;126:664–673. [DOI] [PubMed] [Google Scholar]
- 53.Karlsen S, Nazroo JY. Agency and structure: the impact of ethnic identity and racism on the health of ethnic minority people. Sociol Health Illness. 2002;24:1–20. [Google Scholar]
- 54.Miles R. Racism and Migrant Labour. London, England: Routledge and Kegan Paul; 1982.
- 55.Gilroy P. There Ain’t No Black in the Union Jack: The Cultural Politics of Race and Nation. London, England: Hutchinson; 1987.
- 56.Nazroo JY. The racialisation of ethnic inequalities in health. In: Dorling D, Simpson L, eds. Statistics in Society: The Arithmetic of Politics. London, England: Arnold; 1998:215–222.
- 57.Fenton S. Ethnicity: Racism, Class and Culture. Basingstoke, England: MacMillan Press Ltd; 1999.
- 58.Eriksen TH. Ethnicity and Nationalism: Anthropological Perspectives. London, England: Pluto Press; 1993.