Abstract
The authors’ 1990 article “Producing Health, Consuming Health Care” presented a conceptual framework for synthesizing a rapidly growing body of findings on the nonmedical determinants of health. The article received a very positive response, and here the authors reflect on what lessons might be learned from that response about the style or content of effective interdisciplinary communication.
Much substantive knowledge has been accumulated since 1990, and a number of different frameworks have been developed before and since. The authors situate theirs within this literature and consider how they might have modified it if they “knew then what they know now.” They ask what impact this article, and the much broader stream of research on the determinants of health, has had on public policy?
“PRODUCING HEALTH, Consuming Health Care” (PHCHC), published in Social Science and Medicine in 1990,1 has, we believe, received more attention than any other single article either of us has ever written. More than a decade later, the first question is still “Why?” What was it about the content or the style of that article, or about the intellectual context into which it emerged, that generated such a response? Are there lessons to be learned about effective communication, particularly across disciplines, or were we just lucky in our timing and in the fit between what people were looking for and what we happened to stumble upon?
But that was then, and this is now. Research on the socioeconomic determinants of health has long historical roots, and by 1990 this had already become a lively and extensive field. Since then it has truly exploded and shows little sign of topping out. Powerful stimulants to this work, in earlier years, were political or moral concerns about large inequalities in health within or across populations. These concerns remain very much alive, but it is our impression that the question of why some people are healthy and others are not has become a demanding intellectual challenge in its own right, apart from any implications the answers might have for social policy. Much has been learned, even if much less has been acted upon (and, to be fair, the appropriate policy actions implicit in research findings are often far from clear).
Thus, a second natural question for a retrospective begins with the following: If we knew then what we know now . . . ? How might we, in hindsight, have written the article differently, in structure, content, or emphasis? And just as important, what would we not have changed? What, in our inevitably biased opinion, did we get basically (and importantly) right?
“ ‘But what good came of it at last?’ quoth little Peterkin” (in Robert Southey’s poem After Blenheim). Testimonials, citations, and republications are all very gratifying and may advance an academic career. But how is the world different now, if at all, because PHCHC was published? This is a very demanding and humbling question for anyone working in the so-called social sciences; we may justly envy the real scientists who can often answer such a question very specifically, if very incompletely.
Moreover, if focused on this single article, the question is obviously wrongly posed. PHCHC was simply one early product of the much broader enterprise that was the Program in Population Health of the Canadian Institute for Advanced Research (CIAR), and that in turn was only one component of the still much larger collection of researchers, communicators, and policymakers who were wrestling with the problems of both understanding the determinants of health and acting upon them. PHCHC happened to find itself riding on top of this very large stream of work. But because it did receive such attention (and if it is thought worthy of a retrospective, res ipse loquitur), it may serve as a lens through which to examine the real question: What has been the impact of our advancing collective understanding of population health?
The primary reason for the article’s success, we suspect, is that it was rooted in ignorance. (Orwell was right.) Its authors, longtime students of health care systems, had recently become members of a new and unique cross-disciplinary research program—the CIAR Program in Population Health—with very broad but ill-defined goals. In this context, we were trying to absorb an extraordinary range of information about patterns and correlates of variations in health status. As we were acutely aware, we possessed essentially no prior intellectual framework for understanding these observations.
This program, however, provided an unusual opportunity, in effect a requirement, for intensive interdisciplinary communication. One could not fall back on explanations of health inequalities offered by discipline-specific “theories” (usually just conventions and habits of thought) in a working environment where these theories were not generally shared (or even necessarily understood) and might well be rejected (quite firmly) by those with a different disciplinary perspective. Participants had to develop a mutual understanding and a common language with which to describe and integrate the different pieces of the overall puzzle that emerged from different disciplines or simply from common observation.
This context enforced an inferential, inductive approach—here is a mass of data, how might one explain it? As a forgotten source put it, “data unite, theories divide.” Of particular importance were the “2 × 4s,” anomalies that attract one’s attention forcefully (like hitting a mule over the head with a 2 × 4). These were wellaccepted observations on variations in health status, statistical or otherwise, that were anomalous, difficult, or impossible to explain in terms of simple, monocausal ideas (e.g., medical care, lifestyle “choices,” poverty) about the determinants of health. Conversely, discussions of the proper definition of health were more or less explicitly banned, in that they were likely to absorb considerable time and effort without yielding any useful result. Logically, it might seem that a discussion of the determinants of health should begin with a definition of the entity discussed, but it turns out that this is not so.
No definition appears in PHCHC. What does appear is a continuum of possible definitions ranging from the simplest—alive or dead—to the broadest possible, the “sum of all good things” offered in the classic definition of the World Health Organization. The “right” choice is determined instrumentally, by what one is trying to do. We found that, for most of our purposes, mortality was a good choice.
The article thus addressed primarily systematic variations in mortality, as representing widely available and unambiguous, though clearly incomplete, measures of health about which there could be little or no disagreement. On the other hand, the range of possible determinants of health status, narrowly defined, was taken very broadly; indeed, the whole purpose of the article was to assemble a causal framework that would be capable of integrating, or at least representing, the diversity of determinants found in various disciplinary literatures and in common experience: a very narrow definition of health, a very broad range of possible determinants.
The diversity of disciplinary backgrounds in the CIAR program led naturally to a style of working that could be summed up as “Everybody here is ignorant; nobody here is stupid.” The diversity of specializations meant that each participant was relatively ignorant about all of the other disciplines around the table, but not stupid: we were fortunate in recruiting some rather good talent. It follows that if a participant is not understood by the group, the onus is on that individual, not (as in the typical academic setting) on those who do not understand. Brilliance is no help to a cross-disciplinary enterprise if it cannot be communicated.
Thus, when we came to write an article for an external audience, we were drawing upon an array of information that had already been translated for the intelligent and scientifically inclined nonspecialist by the members of the internal audience. The process of synthesis could proceed with confidence, because the specialists in that internal audience could (and did) stand behind the article, checking its contents from a variety of perspectives. If the article sold well, it was, we think, because most of the “marketing” had already been done through the enthusiastic yet properly skeptical discussions within the CIAR Program in Population Health itself. We had only to transcribe the translation and synthesis that had emerged from the interaction among the participants.
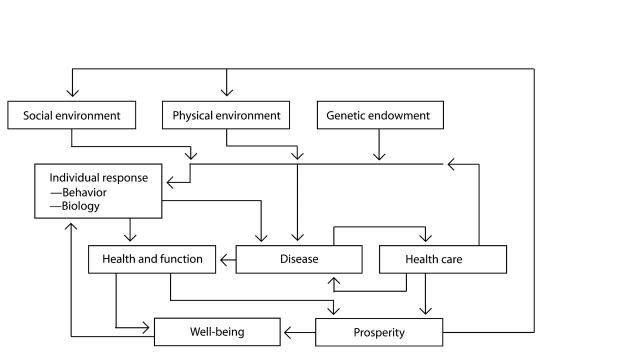
The “line-and-box” diagram that summed up the state of our understanding in PHCHC (Figure 1 ▶) thus evolved, as described in the article itself, from a process of setting up categories and linkages to account for all of the various types of evidence that we were hearing or reading about. It was driven by what we needed to make sense of what we found; the boxes were not defined a priori. In addition (drawing on the pooled competencies of the program members), the article went into a fair degree of literature-based detail as to the nature of the observations that motivated inclusion of the different boxes. This too, we suspect, added to its impact.
FIGURE 1—
Conceptual Framework for Patterns of Determinants of Health.1
The relationship between the health care system and the health of a population was established as the core of the model, the foundation building block, not because we believed that this was necessarily the most important contributor to population health but because we believed that those who make health policy and fund health care systems, and the populations who support them, act as if they believe this. We asked ourselves what model of the determinants of health would have to be in their minds to explain the policy choices that we see around us. Then we went on to augment this structure to take account of other evidence or beliefs as to the determinants of health, starting with the additional factors identified a quarter century ago in A New Perspective on the Health of Canadians.2
THERE ARE NINE AND SIXTY WAYS . . .
The resulting framework is only one among a number that have been developed by students of population health. We did not attempt a review of existing frameworks in PHCHC. Recently, however, VanLeeuwen and colleagues3 reviewed the evolution of models of human health, concluding with their own, which strongly emphasizes the biophysical as well as the socioeconomic environment. They identified the early models of Blum,4 Morris,5 and Travis,6 which they labeled “holistic,” “socio-ecological,” and “wellness,” respectively. These models included the important concept of health as “a dynamic equilibrium and balance between the host, agent, and environment” and introduced the role of “personal behavior factors,”3(p241) paralleling the “lifestyle” field described by Lalonde.2 In each model, however, VanLeeuwen et al. found significant limitations.
Perhaps better known are the “mandala of health” framework of Hancock and Perkins7 and the framework for health promotion that emerged from the World Health Organization’s Ottawa Charter for Health Promotion8 and its accompanying Canadian document Achieving Health for All.9 The mandala framework included a comprehensive set of influences on health (personal behaviors, sick care system, human biology, physical environment, psychosocioeconomic environment, work, and lifestyle). Its most important feature, however, was recognition of the existence of myriad simultaneous interactions among influences occurring within and between 3 levels of a nested hierarchy involving the family, the community and human-made environment, and the culture and biosphere, in that order of proximity. Hancock10 later supplemented this model of individual health with one that integrated sustainable development and the health of communities.
The Ottawa charter and the Epp framework9 did not focus directly on the determinants of health in the way that the mandala or PHCHC did, although the same categories of determinants implicitly underpinned them. Instead, they identified several health challenges (e.g., reducing inequalities) and suggested mechanisms and strategies for addressing them. Five key strategies together composed a systems approach to achieving health for all citizens: building healthy public policy, creating supportive environments, strengthening community action, developing personal skills, and reorienting health services.
Since the publication of PHCHC, several other useful categorizations of influences on health or frameworks have appeared and continue to appear.3,11–15 Moreover, researchers are increasingly focusing on subframeworks to explore and explain in much richer detail specific pieces of the puzzle of the determinants of population health. For example, Patrick and Wickizer16 proposed a subframework for studying community and health, while Amick and Lavis17 offered one for labor market experiences and health. Marmot18 presented models that help to explain the role of psychosocial and biological pathways linking socioeconomic status to cardiovascular disease. Sapolsky19 and Kaplan and Manuck20 offered models on the linkage from social hierarchy to health among nonhuman primates that are highly suggestive for humans.
Subframeworks were what we had envisioned as being required once one entered the “doorway” of one of our boxes21,22 but would have been well beyond the scope of our article, let alone our abilities. Numerous subframeworks for specific health determinants or population groups can be found in several recent population health books.23–26
Taken as a group, most of the conceptual frameworks of the past 2 decades (including PHCHC) have 3 important common features. First, they recognize the importance of context and the capacity of social, economic, cultural, and physical environments to modify the relationship between health and individual characteristics. Second, they acknowledge the complexity of the interactions among the many determinants of health, even if they do not and cannot unravel them all. Third, they place the activities (and resource demands) of health care systems in a more balanced perspective, in that health care is shifted from center stage and attention is focused not on how to make sick people well but on why they are sick in the first place.
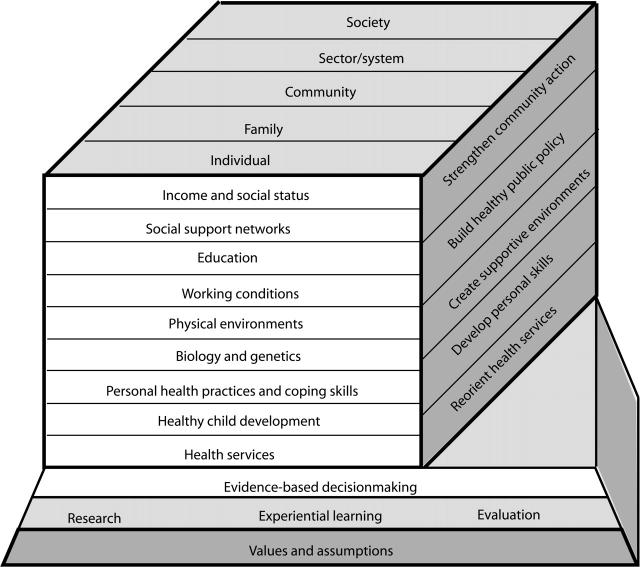
The Hamilton and Bhatti12 population health promotion model, however, warrants special attention for its attempt to integrate population health research with health promotion activities. Although the 2 fields overlap and are, in our view, very complementary, the emergence of population health has at times been a source of tension for the health promotion community.27 Hamilton and Bhatti set out to reduce that tension.
We present in Figure 2 ▶ an adaptation of the cube that embodies their integrated framework. The front face identifies the categories of determinants taken from population health; in their language, On what should we take action? On the side face, they take from health promotion the key strategies for acting on knowledge about determinants; in their language, How should we take action? On the top face, they use the levels at which action can occur—in their language, With whom should we act?—that are recognized in both health promotion and population health frameworks.
FIGURE 2—
Population Health Promotion Model.12
This seems to us to be a useful and appropriate integration and to accord well with the definition of health promotion provided in Nutbeam’s28 glossary: “the process of enabling individuals and communities to increase control over the determinants of health and thereby improve their health.” Interestingly, mention of determinants is commonly omitted from documents and articles on health promotion, and the definition is reduced to “the process of enabling people to increase control over and to improve their health.”13,29 The omission of determinants from the shortened definition unfortunately may hinder understanding of the complementarity of population health and health promotion illustrated in Hamilton and Bhatti’s cube.
IF WE KNEW THEN . . .
The multiplication of frameworks and subframeworks in the decade and more since the PHCHC framework was first laid out reflects the dramatic subsequent expansion of knowledge as well as of the number of analysts struggling to integrate that knowledge in a compact and comprehensible form (without doing too much violence to the inherent complexity). So, if we knew then what we or others know now, would we ourselves have written the article very differently? Probably not.
To begin with, however, we must admit that although the article was fairly extensively referenced, there were egregious exceptions. We should have given more acknowledgment to earlier work that pointed to the linkage from social environment through individual psychology to health status, such as that of Antonovsky,30,31 for example, or Cassel32 or, for that matter, Selye himself.33 We can only offer Samuel Johnson’s excuse for such oversights: “Sirs, it was pure ignorance.”
For the simplicity of the framework, however, we offer no apology. The complexity of the determinants of health has become more and more apparent. Rather than a simple, linear system of relationships—much less a single causal factor—health depends upon everything, all the time. But the boxes were never thought of as representing homogeneous entities; as noted earlier, they were more like doorways, each of which opened onto its own world of complexity. They would be useful if they partitioned that complexity in an intuitively plausible way, if the entities and interactions relevant to health within a given box or category were more dense, or more similar and more readily grasped as a group, than the interactions between boxes.
As an example of where we got this wrong, we followed what was then general understanding in treating genetic endowment as prior and exogenous, a box off on its own at the edge of the model. Granted, in utero insults can induce congenital defects that will certainly affect future health and function, but the individual genome was thought of as not only fixed at the moment of conception but unambiguous in its implications for health: genetic destiny.
This is now hopelessly old-fashioned. Research is making it increasingly clear that whatever the initial genetic endowment, the expression of that endowment will depend upon interactions with both the physical and, particularly, the social environment. There should be lines of causality moving into the genetic box, as well as out of it, or else tapping into the side of the line coming from the genetic box, and realization of the strength of that connection continues to grow rapidly.
This connection, however, should not lead one to conflate the genetic box with either the social or the physical environment. The measurement, methods of study, and potential interventions of the determinants included in these 3 boxes seem quite distinct, and it would be confusing rather than enlightening to combine them. In any case, the spirit of the gene–environment interaction is picked up in something we did get right, the combination of behavior and biology in a single box.
That combination represented an important insight, though hardly an original one. The stresses and supports of the environment, physical and especially social, can drive one to drink or induce a variety of other beneficial or harmful behavioral responses. They can also induce various biological responses that may be effective or damaging ways of responding to stress. To treat biological and behavioral responses as qualitatively different, as would be implied by situating them in separate boxes, would set up a form of “free will vs determinism” dichotomy. This can lead to the “just say no” school of health promotion, in which choosing healthy or unhealthy “lifestyles” is akin to choosing chocolate or vanilla ice-cream. Such a decontextualized view of human behavior provides an excuse for inaction—preaching instead of programs—and can readily be twisted into futile victim-blaming. (Most of those who consider themselves “health promoters” have a much more subtle understanding of human behavior.)
Research is showing increasingly clearly that behavior patterns have biological correlates. Social environments become embedded in individual biology, as well as in behavioral patterns. Perhaps the clearest examples of this “biological embedding” in human populations have been shown in the divergent health experiences, over the past 35 years, of populations in the “West” and in the former Soviet Union and its satellites.34,35 Experimental work has revealed biological differences in stress responses between “Eastern” and “Western” populations that can have arisen only from differences in social environments. Systematic differences have not, however, been found in the usual behavioral suspects: smoking, blood lipids, and hypertension.36,37
There is now an extensive array of immunological and endocrinological research, including extraordinary findings from the study of various nonhuman primates, that is beginning to fill in the biological pathways from social experience through individual responses to health status outcomes. This is all “through the doorway” of the biological/behavioral box; if PHCHC were being written now, one might add some of the leading references. Evans38 briefly surveyed some of this material. It all fits in beautifully.
We also think that we fit in the health care system appropriately in the overall framework. Some clinicians and advocates of the expansion of health care systems have interpreted the focus on nonmedical determinants of health as a revival of “medical nihilism” and a justification for containment or reduction of expenditures on health care. And indeed we did point out that a good deal of clinical activity is known to be unnecessary or unnecessarily expensive—a fact well-cited in the medical literature but nonetheless a very sensitive point for clinicians. To the extent that health is associated with economic well-being, wasteful clinical practices may pose a double threat to health. However, clinical medicine is clearly identified in the framework as being of central importance in responding to the situation of those who have already become ill or injured. There is also some evidence39 that a strong primary care network that exploits the potential for a broad range of preventive interventions and coordinates the care of those with multiple comorbidities can have a measurable influence on the health of the populations served. But impassioned and sometimes intemperate defenses of the role of medicine have occasionally risked denial of the obvious: that there are many other factors in play as well particularly in influencing the incidence of illness or injury. Clinical interventions are often decisive in the life of an individual, but to argue that the level and sophistication of such interventions, much less differences in total health care expenditures, can explain why some populations are healthier than others is simply to fly in the face of the evidence.
In any case, it would quite simply be ridiculous to suggest that the flattening of health expenditure trends in both Canada and the United States from 1992 to 1997 resulted from the instant and massive uptake of a set of “new” ideas about population health. The fiscal condition of the Canadian federal and provincial governments and American corporations provides a perfectly adequate explanation. And the finance ministries and corporate boardrooms that engineered the financial squeeze on health care appear, in fact, to be the areas of policy generation least penetrated by these ideas (see subsequent discussion).
A factor that is wholly missing from PHCHC is the role of time. The framework betrays the disciplinary origins of its creators, rooted in the static equilibrium models of most of economic theory. The various determinants of health must have their effects in real time, some cumulatively, some with long lags, some at a particular stage in the life of the organism, some combined in a particular sequence. By now it is generally understood that the effects of social environments—similar to aspects of the physical environment—operate over the life course, and research designs are increasingly focusing on longitudinal data sets that can be linked to form a picture of the whole trajectory.
We did know that time was important, and said so. But (as far as we can now remember) just how important, and in how many different ways, was not then clear to us. In the light of subsequent analysis and findings, however, we still have no idea how or whether one could construct an extended framework that would adequately represent the complex web of dynamic processes through which the various determinants of health have their effects. The answer might reside in more advanced, computer-based representational technologies; certainly our pencil-and-paper, line-and-box diagram approach was a long way behind the technological frontier even then. On the other hand, most of the people in the potential audience are also well behind the technological frontier at any point in time. Had we been technologically more competent, we might have produced a much more sophisticated representation with much less impact. “Keep it simple, stupid!”
Anyway, if we knew then what we know now, we would still use lines and boxes, because we ourselves do not actually know any more now than we did then about advanced representational techniques. But there is no question that the interaction of determinants over the life trajectory is central to understanding their effects, and research designs and data sources must correspond to this reality. PHCHC recognized but did not address this issue; probably it could not have done so.
This leaves one major area in which we certainly would try to rewrite PHCHC and (somehow) restructure Figure 1 ▶. The treatment of income or wealth as both a contributor to and a consequence of health status is not at all adequate in light of current knowledge. The nature of the rewrite, however, would be very much a matter of dates. Research findings on this relationship have shifted dramatically over the past decade, and new data that may change the picture yet again are emerging as this piece is written.
Our thinking then was much influenced by the work of McKeown,40 who by a process of elimination concluded that the major declines in mortality from infectious diseases observed in 19th-century England were attributable to a general increase in living standards and corresponding improvement in nutrition and host resistance. Medical advances came on the scene far too late to explain these trends. Credit is usually given primarily to public sanitary measures, but McKeown argued that these measures could not have caused the dramatic decline in tuberculosis mortality because the disease is not waterborne. We also had in front of us the spectacular increase in the health status of the Japanese population, rising in parallel with the country’s spectacular rate of economic growth, and we speculated about the possible connections.
These considerations, combined with the well-known correlation at the individual level between health and wealth, led us to insert a direct link between prosperity and health. We took it for granted that this meant an equiproportionate rise in all incomes—the rising tide lifting all boats—rather than simply an increase in the average driven by large increases for the wealthy and stagnation or decline for the general population. But we were clear, from the work of Marmot and his colleagues,41,42 that the “wealth–health” link represented much more than the obvious effects of poverty and material deprivation. The existence of a socioeconomic gradient in health status, running across the entire income spectrum, is an extremely important observation—perhaps the most important single fact—for our understanding of the determinants of health.43 It is all too easy, in focusing on the very real physical and moral implications of poverty, to be blinded to the reality that other factors are influencing the health of a much larger proportion of the population. This we knew.
A simple link from income to health, however, invites misinterpretation as support for policies of economic growth über alles. Why waste resources on public health, medical care, or social programs more generally? Maximize the rate of economic growth, by whatever means possible, and you will maximize the rate of increase in health as well. This crude conception, which we do not and never did share, casually ignores crucial questions as to how increases in wealth are shared and how they are spent. Unfortunately, it also feeds into the policy agenda of narrowly based but powerful and strategically placed interest groups.
In any case subsequent reevaluation of McKeown’s work in light of better historical data indicates that while he was right about the minimal influence of medical care in earlier decades, he was wrong to dismiss the impact of sanitary measures.44–46 Increased private consumption and expanded public health initiatives may both follow from increased national income, but public initiatives offer more potential for health improvement.
The relationship between health and income distribution has attracted particularly intense research interest in the more than a decade since PHCHC was written, focusing on a core idea in the work of Richard Wilkinson.47–49 Comparing health status measures for a group of countries with measures of their inequality of income distribution, he found a positive correlation between inequality and mortality, suggesting that highly unequal societies are less healthy overall. His findings attracted considerable attention for their intrinsic intellectual interest as well as their political significance, but they were also criticized on the basis of selective choice of countries and particularly of inequality measures, as well as noncomparable data sources.50 In 1996, however, 2 major articles involving the use of US cross-state data appeared strongly to confirm Wilkinson’s thesis.51,52 A later comparison of American metropolitan areas showed the same pattern.53 Had we been writing PHCHC in the late 1990s, this “big idea” would have been a centerpiece.
But not today. Ross et al.54 reported results obtained from pooling data on income inequality and mortality from American states and Canadian provinces, as well as metropolitan areas in both countries. The Canadian data strengthened the relationship posited by Wilkinson for North America as a whole; they showed lower rates of both mortality and income inequality and fit neatly into the overall scatterplot. When examined in isolation, however, they showed no such relationship within Canada itself. Nor were Wilkinson’s earlier findings replicated across a larger set of Organisation for Economic Cooperation and Development countries.55,56 And in an editorial accompanying a set of country-specific studies published in the British Medical Journal at the beginning of 2002, Mackenbach57 concluded that “the evidence for a correlation between income inequality and the health of the population is slowly dissipating, with supporting evidence reduced almost entirely to (still inconclusive) analyses in the United States.”57(p2)
Even in the United States, the strength and, in fact, the existence of the inequality–ill health relation are still in question; some analysts have argued that other characteristics of American states, such as the percentage of the population that is Black, are more powerful predictors of health than income inequality per se. Several studies appear to show that the most powerful predictor of health status at the individual level is income, pure and simple, with little or no role for either relative income status or measures of inequality.
On the other hand, while this article was being written in June 2002, Nancy Ross and James Dunn presented as yet unpublished data at a CIAR conference in Victoria, British Columbia, showing that while the crossregional relation between income inequality and mortality in Australia and Sweden appeared to be very similar to that in Canada, a comparison of cities in the United Kingdom was more similar to the US findings. In addition, Wilkinson58 has argued persuasively that the frequently observed relationship between individual income and health is in fact picking up important aspects of the social context. The entire issue is still very much in flux.
All of this makes it difficult to know what we should say, knowing what we know now (or do not), about the linkage between health and wealth. The rapidly advancing knowledge about the biological pathways through which the determinants of health operate over the life course is impossible to square with a simple-minded story such as “more money buys more health.” And yet that seems to be the best that the econometricians can come up with.
We think the most plausible view to this point is that the relationship between income and health, or between inequality and health, depends very much on the social and cultural environment in which income differences are experienced. The framework evolved by Sapolsky19 from studies of hierarchy conducted with olive baboons may be the most relevant; according to this framework, the impact of hierarchical position on health depends upon the stability of that hierarchy and the intensity with which differences in position are experienced, modulated by the social supports available to differently placed individuals and by the sensitivity or resilience of individual personalities. American society is characterized by a steep (but somewhat unstable) hierarchical structure defined by wealth, in which individuals experience intensely their differences in position.
It may be that the correlation between economic inequality and mortality does not cross the Canadian border because Canada (as is the case with most other developed societies) provides many more public programs and regulatory structures: high-quality public health care and education, minimum wages and unemployment insurance, greater labor rights. These elements serve to buffer individuals against the vulnerabilities associated with low income and make their life chances (and those of their children) less hostage to their economic circumstances. Canada is far from generous by European standards, but also is quite different from the United States, and the data show that these differences matter.
A RESPONSE TO PETERKIN
In the conclusion of PHCHC, we noted that the test of our framework would be whether others found it useful as a set of categories for assembling data, approximating complex causal patterns, and illuminating policy choices and trade-offs. In short, would it be used? It seems appropriate, therefore, to close with some reflections on the reception accorded PHCHC and, more important, on the impact over the past decade or so of the work of the many individuals and groups who have been advancing and disseminating knowledge about the determinants of population health.
Our article was in general well received by academics, and we have naturally been gratified by the numerous citations and several republications in book collections. (There have of course been critics.59,60 Hayes and Dunn27 provide summaries of the main lines of criticism in their review of the evolution of population health in Canada.) It seems to have aged relatively well, although, as noted earlier, significant updates and revisions are necessary at this point. Perhaps most important, it has contributed to and helped to stimulate the revival and popularization of interest in nonmedical determinants of the health of populations.
There is one exception among academic audiences; population health ideas have had minimal impact on economists. We do not think this is entirely surprising. The discipline of economics is not fertile ground for population health ideas; the “preanalytic cognitive acts” (in Schumpeter’s phrase) of its practitioners presuppose a world of autonomous individuals, stripped of social context and even of biological content, whose behavior is restricted to conscious, selfregarding rational choices. Environments get short shrift in economic theory; even families, if recognized at all, are simply economically motivated associations. The “representative agents” popular with economic theorists leave no heterogeneity to explain. If health gradients occur, they must be either selection effects or the outcomes of “free” and deliberate choices.
However, we have been surprised by the number of people—individual researchers, students, public health officials, and those working in other specific organizations, associations, or community contexts, often with few resources—who have contacted us to say that they have found the article helpful. Most have indicated that what they found most useful was having “the big picture” in one place, warts and all, and being connected through one article to research bases from several disciplines. Some have said that our work and the similar work of others had given legitimacy to their own local efforts to travel the same road. And, of course, everyone had suggestions for how to redraw the causal arrows!
PHCHC is only one small piece in the accumulating work produced by those in the fields of social epidemiology, public health, health promotion, and population health (to name only a few) who seek to understand better the broad range of determinants of health and use this knowledge to change health and social policies to improve health. Where does this collective enterprise now stand? Our brief assessment is that it is making steady progress, perhaps even gaining momentum on several fronts, but that its impact on policy has been slow to materialize.
It appears to be penetrating academic institutions in Canada, the United States, and the United Kingdom, as evidenced by the creation of research centers and institutes and the restructuring of academic departments at many major universities.61 Often, the phrase “population health” is included in their names. Although in some instances this may be cosmetic, an effort to cash in on the current popularity of the label, most often it signals a genuine intellectual commitment of both personnel and financial resources to the study of health determinants.
It also appears to be penetrating research funding organizations and at least some statistical agencies.61 In Canada, for example, the Institute of Population and Public Health is one of 13 institutes in the newly formed Canadian Institutes of Health Research, and a population health perspective has been made a “horizontally” cross-cutting concern of all 13. Another federally funded organization, the Canadian Population Health Initiative, and some provincial research granting agencies also have earmarked funds for population health research and research transfer activities. In addition, a “determinants of health” perspective has stimulated and informed the design of at least 2 new Canadian longitudinal databases, the National Population Health Survey and the National Longitudinal Survey of Children and Youth. The Canadian Institute for Health Information, the national agency with primary responsibility for assembling health data, now produces (and disseminates widely) extensive information on the health of the Canadian population and its determinants, as well as on the health care system. In other countries, similar trends are occurring via different institutional frameworks.
In the case of governments and policymakers, the story is more complex and less encouraging. The determinants of health perspective seems to have penetrated large parts of the Canadian public bureaucracies; Lavis et al.,62 in a recent survey of Canadian federal and provincial policy advisors in finance, labor, social services, and health ministries, found broad awareness of and interest in population health ideas. The clear outliers, however, were finance officials (almost entirely economists), who were to a person unaware of the major source documents in population health. They were much less supportive of the position that health determinants should be considered in all major government initiatives, much less aware of research on the impact of specific nonmedical determinants of health, and much less likely to support investments in policy action or further research related to nonmedical determinants. We suspect that surveys undertaken in other countries would show similar results.
Policy rhetoric on health inequalities, at least in Canada and the United Kingdom, frequently expresses these concepts; occasionally they are carried as far as institutional restructuring or actual policy statements. In Canada, several provincial ministries of health have established Population Health units or branches. The federal department of health, Health Canada, has made Population Health one of its “business lines” and created a population health “template” and Web site at http://www.hcsc.gc.ca/hppb/phdd/approach. It is difficult, however, to find examples of significant shifts in policy direction, carried through to implementation, that could be attributed to the creation, synthesis, and dissemination of knowledge about the (nonmedical) determinants of health, though the National Children’s Agenda in Canada may offer 1 example.
The explanation for this limited impact has, we think, 2 components. First, if the central financing ministries do not “get it,” they will be neither sensitive to the powerful impact of macro-economic policies in setting the social environment of individuals and communities nor supportive of initiatives in other ministries for which they must provide the necessary funding. It is notable that in the United Kingdom, Canada, and the United States fiscal policies over the last 15 years have been focused on restricting public spending and increasing income inequality through tax changes favoring those with higher incomes. On current evidence one might expect these policies to be actively harmful to population health. (The UK government does appear to have changed this stance in the last year.)
Second, however, to the extent that finance ministries are aware of health issues, their concern is with the health care system. Health care absorbs a very large share of public resources in every modern society and, unless tightly constrained, is capable of expanding that share without limit. Aaron Wildavsky63(p109) summarized this observation 25 years ago as the Law of Medical Money: “costs will increase to the level of available funds . . . that level must be limited to keep costs down.” The constituency for expansion is large, highly organized, extremely powerful, and backed by broad public support. Redirecting some of these resources to action on the nonmedical determinants of health might have the potential to yield overall better health at lower costs, but all of these costs are simultaneously someone’s income. Redirecting resources means redirecting those incomes. Worse, most students of population health cannot confidently answer with precision the question “Well, where would you put the money?” Health care advocates have a thousand answers, very precise, very confident, and with methods for demonstrating outcomes that are well worked out and rigorous if not necessarily followed.
This imbalance of forces is illustrated by the health policies of the Blair government in the United Kingdom, as expressed in From Vision to Reality.64 Opening with a ringing declaration of the government’s unshakable determination to reduce inequalities in health, it documents large new financial commitments for the health care system: the National Health Service. These commitments may be all to the good and seem to have broad public support, but the evidence is that they are unlikely to reduce health inequalities.65,66 A variety of other policies, some specific and small, others perhaps more significant but vague, are also put forward, but the financial muscle is all behind health care.38 The United Kingdom has, of course, the longest tradition of any country of outstanding research on, and strong policy concern with, the nonmedical determinants of health.
It is still early, in policy time, for the “determinants of health movement,” if it may be called such. The increasingly rapid accretion of knowledge, associated with dramatic increases in research funding, personnel, and quantity and quality of data, may reduce the degrees of freedom for policy inaction. It may increasingly force those concerned with financing health care to look “upstream,” while those responsible for other aspects of social and especially economic policy have to look “downstream” for health consequences.
If this is to happen, however, research on the determinants of health will probably have to go beyond extending our knowledge of correlates and pathways and focus much more on identifying specific social and fiscal policies and demonstrating their impact (or lack of it) on health.61,67 Current policies are unlikely to change in the absence of a clear agenda—literally, “what is to be done”—whose health benefits are beyond question. Can researchers in population health generate such an agenda? And even if they can, how far will policymakers be willing (or able) to go in accepting it? There are other reasons why things do not happen, reasons that will not disappear in the light of advancing knowledge alone. Well-defined, though narrowly based, economic interests will be threatened by any serious efforts to act on the nonmedical determinants of health. Lavis et al.62 remind us of this reality, quoting the eminent American philosopher Homer Simpson: “Just because I don’t care doesn’t mean I don’t understand.”
Acknowledgments
We thank John Lavis for helpful comments on an earlier version of this article.
Both authors contributed original ideas to the initial outline for this article. R. G. Evans wrote the initial draft of the first and third sections; G. L. Stoddart wrote the initial draft of the second and fourth sections. Subsequent revision and editing were done jointly.
Peer Reviewed
References
- 1.Evans RG, Stoddart GL. Producing health, consuming health care. Soc Sci Med. 1990;31:1347–1363. [DOI] [PubMed] [Google Scholar]
- 2.Lalonde M. A New Perspective on the Health of Canadians. Ottawa, Ontario, Canada: Information Canada; 1974.
- 3.VanLeeuwen JA, Waltner-Toews D, Abernathy T, et al. Evolving models of human health toward an ecosystem context. Ecosystem Health. 1999;5:239–254. [Google Scholar]
- 4.Blum HL. Planning for Health: Developmental Application of Social Change Theory. New York, NY: Human Sciences Press; 1974. .
- 5.Morris JN. Uses of Epidemiology. New York, NY: Churchill Livingstone Inc; 1975. .
- 6.Travis JW. Wellness for Helping Professionals. 3rd ed. Mill Valley, Calif: Wellness Associates; 1977. .
- 7.Hancock T, Perkins F. The mandala of health: a conceptual model and teaching tool. Health Educ. 1985;24:8–10. [Google Scholar]
- 8.The Ottawa Charter for Health Promotion. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 1986. .
- 9.Epp J. Achieving Health for All: A Framework for Health Promotion. Ottawa, Ontario, Canada: Health and Welfare Canada; 1986.
- 10.Hancock T. Health, human development and the community ecosystem: three ecological models. Health Promotion Int. 1993;8:41–46. [Google Scholar]
- 11.Strategies for Population Health: Investing in the Health of Canadians. Ottawa, Ontario, Canada: Federal, Provincial and Territorial Advisory Committee on Population Health; 1994.
- 12.Hamilton N, Bhatti T. Population Health Promotion: An Integrated Model of Population Health and Health Promotion. Ottawa, Ontario, Canada: Health Promotion Development Division, Health Canada; 1996.
- 13.Health 21—The Health for All Policy for the WHO European Region: 21 Targets for the 21st Century. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 1998.
- 14.Starfield B, Shi L. Determinants of health: testing of a conceptual model. In: Adler NE, Marmot M, McEwen BS, Stewart J, eds. Socioeconomic Status and Health in Industrial Nations: Social, Psychological, and Biological Pathways. New York, NY: New York Academy of Sciences; 1999:344–346. [DOI] [PubMed]
- 15.Healthy People 2010. Washington, DC: US Dept of Health and Human Services; 2000.
- 16.Patrick DL, Wickizer TM. Community and health. In: Amick BC, Levine S, Tarlov AR, Walsh DC, eds. Society and Health. New York, NY: Oxford University Press Inc; 1995:46–92.
- 17.Amick BC, Lavis JN. Labour markets and health: a framework and set of applications. In: Tarlov AR, St. Peter RF, eds. The Society and Population Health Reader. Vol. 2. New York, NY: New Press; 2000:178–210.
- 18.Marmot M. Multilevel approaches to understanding social determinants. In: Berkman LF, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press Inc; 2000:349–367.
- 19.Sapolsky RM. Hormonal correlates of personality and social contexts: from non-human to human primates. In: Panter-Brick C, Worthington CM, eds. Hormones, Health and Behaviour. New York, NY: Cambridge University Press; 1999:18–47.
- 20.Kaplan JR, Manuck SB. Status, stress, and atherosclerosis: the role of environment and individual behavior. Ann N Y Acad Sci. 1999;896:145–161. [DOI] [PubMed] [Google Scholar]
- 21.Stoddart GL. The Challenge of Producing Health in Modern Economies. Toronto, Ontario, Canada: Canadian Institute for Advanced Research; 1995. Program in Population Health working paper 46.
- 22.Stoddart GL. Toward an understanding of the determinants of health—together. In: Feather J, Sproat B, eds. Population Health Promotion: Bringing Our Visions Together. Saskatoon, Saskatchewan, Canada: Prairie Region Health Promotion Research Centre; 1996:11–26.
- 23.Amick BC, Levine S, Tarlov AR, Walsh DC, eds. Society and Health. New York, NY: Oxford University Press Inc; 1995. .
- 24.Adler NE, Marmot M, McEwen BS, Stewart J, eds. Socioeconomic Status and Health in Industrial Nations: Social, Psychological, and Biological Pathways. New York, NY: New York Academy of Sciences; 1999. [PubMed]
- 25.Marmot M, Wilkinson RG, eds. Social Determinants of Health. New York, NY: Oxford University Press Inc; 1999.
- 26.Berkman LF, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press Inc; 2000.
- 27.Hayes MV, Dunn JR. Population Health in Canada: A Systematic Review. Ottawa, Ontario, Canada: Canadian Policy Research Networks Inc; 1998.
- 28.Nutbeam D. Health promotion glossary. Health Promotion. 1986;1:113–127. [DOI] [PubMed] [Google Scholar]
- 29.Health promotion: what is it? Health Canada Health Policy Res Bull. 2002;1:5–7. [Google Scholar]
- 30.Antonovsky A. Social class, life expectancy and overall mortality. Milbank Q. 1967;45:31–73. [PubMed] [Google Scholar]
- 31.Antonovsky A. Health, Stress and Coping. San Francisco, Calif: Jossey-Bass; 1979.
- 32.Cassel J. The contribution of the social environment to host resistance. Am J Epidemiol. 1976;104:107–123. [DOI] [PubMed] [Google Scholar]
- 33.Selye H. The Stress of Life. Rev. ed. New York: McGraw-Hill Book Co; 1976.
- 34.Bobak M, Marmot M. East-west health divide and potential explanations. In: Hertzman C, Kelly S, Bobak M, eds. East-West Life Expectancy Gap in Europe: Environmental and Non-Environmental Determinants. Dordrecht, the Netherlands: Kluwer Academic; 1996:17–44.
- 35.Cornia GA, Paniccia R. The transition mortality crisis: evidence, interpretation and policy responses. In: Cornia GA, Paniccia R, eds. The Mortality Crisis in Transitional Economies. New York, NY: Oxford University Press Inc; 2000:3–37.
- 36.Kristenson M. The LiVicordia Study. Linkoping, Sweden: Linkoping University Dept of Health and Environment; 1998. Medical dissertation 547.
- 37.Kristenson M, Orth-Gomer K, Kuchinskiene Z, et al. Attenuated cortisol response to a standardised stress test in Lithuanian vs. Swedish men: the LiVicordia Study. Int J Behav Med. 1998;5:17–30. [DOI] [PubMed] [Google Scholar]
- 38.Evans RG. Interpreting and Addressing Inequalities in Health: From Black to Acheson to Blair to . . . ? London, England: Office of Health Economics; 2002.
- 39.Starfield B, Shi L. Policy relevant determinants of health: an international perspective. Health Policy. 2002;60:201–218. [DOI] [PubMed] [Google Scholar]
- 40.McKeown T. The Role of Medicine: Dream, Mirage or Nemesis? 2nd ed. Oxford, England: Basil Blackwell; 1979.
- 41.Marmot MG, Rose GA, Shipley MJ, Hamilton PJS. Employment grade and coronary heart disease in British civil cervants. J Epidemiol Community Health. 1978;32:244–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marmot MG. Social inequalities in mortality: the social environment. In: Wilkinson RG, ed. Class and Health: Research and Longitudinal Data. London, England: Tavistock; 1986:21–33.
- 43.Evans RG, Barer ML, Marmor TR. Why Are Some People Healthy and Others Not? New York, NY: Aldine de Gruyter; 1994.
- 44.Szreter S. The importance of social intervention in Britain’s mortality decline c. 1850–1914: a reinterpretation of the role of public health. Soc Hist Med. 1988;1:1–37. [Google Scholar]
- 45.Szreter S. The McKeown thesis. J Health Serv Res Policy. 2000;5:119–120. [Google Scholar]
- 46.Szreter S. Rethinking McKeown: the relationship between public health and social change. Am J Public Health. 2002;92:722–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilkinson RG. Income distribution and life expectancy. BMJ. 1992;304:165–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wilkinson RG. The epidemiological transition: from material scarcity to social disadvantage? Daedalus. 1994;123:61–78. [PubMed] [Google Scholar]
- 49.Wilkinson RG. Unhealthy Societies: The Afflictions of Inequality. London, England: Routledge; 1996.
- 50.Judge K. Income distribution and life expectancy: a critical appraisal. BMJ. 1995;311:1282–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kaplan GA, Pamuk ER, Lynch JW, et al. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. BMJ. 1996;312:999–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kennedy BP, Kawachi I, Prothrow-Stith D. Income distribution and mortality: cross sectional ecological study of the Robin Hood index in the United States. BMJ. 1996;312:1004–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lynch JW, Kaplan GA, Pamuk ER, et al. Income inequality and mortality in metropolitan areas in the United States. Am J Public Health. 1998;88:1074–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ross NA, Wolfson MC, Dunn JR, et al. Relation between income inequality and mortality in Canada and in the United States: cross sectional assessment using census data and vital statistics. BMJ. 2000;320:898–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lynch JW, Davey Smith G, Hillemeier M, et al. Income inequality, the psycho-social environment, and health: comparisons of wealthy nations. Lancet. 2001;358:194–200. [DOI] [PubMed] [Google Scholar]
- 56.Judge K, Paterson L. Poverty, Income Inequality and Health. Wellington, New Zealand: Government of New Zealand; 2001. . Treasury working paper 1/29.
- 57.Mackenbach JP. Income inequality and population health. BMJ. 2002;324:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wilkinson RG. Commentary: liberty, fraternity, equality. Int J Epidemiol. 2002;31:538–543. [DOI] [PubMed] [Google Scholar]
- 59.Labonte R. Population health and health promotion: what do they have to say to each other? Can J Public Health. 1995;86:165–168. [PubMed] [Google Scholar]
- 60.Poland B, Coburn D, Robertson A, et al. Wealth, equity and health care: a critique of a “population health” perspective on the determinants of health. Soc Sci Med. 1998;46:785–798. [DOI] [PubMed] [Google Scholar]
- 61.Lavis JN. Ideas at the margin or marginalized ideas? Nonmedical determinants of health in Canada. Health Aff. 2002;21:107–112. [DOI] [PubMed] [Google Scholar]
- 62.Lavis JN, Ross SE, Stoddart GL, et al. Do Canadian civil servants care about the health of populations? Am J Public Health. In press. [DOI] [PMC free article] [PubMed]
- 63.Wildavsky A. Doing better and feeling worse: the political pathology of health policy. Daedalus. 1977;106:105–124. [PubMed] [Google Scholar]
- 64.From Vision to Reality. London, England: United Kingdom Dept of Health; 2001. .
- 65.Black D, Morris J, Smith C, Townsend P. Inequalities in Health: Report of a Research Working Group. London, England: United Kingdom Dept of Health and Social Security; 1980. .
- 66.Wilkins R, Ng E, Berthelot J-M. Trends in Mortality by Income in Urban Canada From 1971 to 1996. Washington, DC: Population Association of America; 2001. .
- 67.Horton R. Commentary: what the UK government is (not) doing about health inequalities. Lancet. 2002;360:186. [DOI] [PubMed] [Google Scholar]