Abstract
Population health is a relatively new term that has not yet been precisely defined. Is it a concept of health or a field of study of health determinants?
We propose that the definition be “the health outcomes of a group of individuals, including the distribution of such outcomes within the group,” and we argue that the field of population health includes health outcomes, patterns of health determinants, and policies and interventions that link these two.
We present a rationale for this definition and note its differentiation from public health, health promotion, and social epidemiology. We invite critiques and discussion that may lead to some consensus on this emerging concept.
ALTHOUGH THE TERM “population health” has been much more commonly used in Canada than in the United States, a precise definition has not been agreed upon even in Canada, where the concept it denotes has gained some prominence. Probably the most influential contribution to the development of the population health approach is Evans, Barer, and Marmor’s Why Are Some People Healthy and Others Not? The Determinants of Health of Populations,1 which grew out of the work of the Population Health Program of the Canadian Institute for Advanced Research. No concise definition of the term appears in this volume, although its authors state the concept’s “linking thread [to be] the common focus on trying to understand the determinants of health of populations.”1(p29)
The idea that population health is a field of study or a research approach focused on determinants seems to have evolved from this work. Early discussions at the Canadian Institute for Advanced Research also considered the definition and measurement of health and the processes of health policymaking, but the dominant emphasis evolved to the determinants themselves, particularly the nonmedical determinants. John Frank, the scientific director of the recently created Canadian Institute of Population and Public Health, has similarly called population health “a newer research strategy for understanding the health of populations.”2 T. K. Young’s recent book Population Health also tends in this direction; he states that in Canada and the United Kingdom in the 1990s, the term has taken on the connotation of a “conceptual framework for thinking about why some populations are healthier than others as well as the policy development, research agenda, and resource allocation that flow from this framework.”3(p4)
However, Young also indicates that in the past, the term has been used as a “less cumbersome substitute for the health of populations,” which is of course its literal meaning. Evans and Stoddart, while supporting an emphasis on “understanding of the determinants of population health,” have also stated, however, that “different concepts [of health] are neither right or wrong, they simply have different purposes and applications. . . . [W]hatever the level of definition of health being employed, however, it is important to distinguish this from the question of the determinants of that definition of health.”1(p28) The Health Promotion and Programs Branch of Health Canada has recently stated that “the overall goal of a population health approach is to maintain and improve the health of the entire population and to reduce inequalities in health between population groups.”4(p1) They indicate that one guiding principle of a population health approach is “an increased focus on health outcomes (as opposed to inputs, processes, and products) and on determining the degree of change that can actually be attributed to our work.”(p11)
Dunn and Hayes, quoting the definition of the Canadian Federal/Provincial/Territorial Advisory Committee on Population Health, write that “population health refers to the health of a population as measured by health status indicators and as influenced by social, economic, and physical environments, personal health practices, individual capacity and coping skills, human biology, early childhood development, and health services. As an approach, population health focuses on interrelated conditions and factors that influence the health of populations over the life course, identifies systematic variations in their patterns of occurrence, and applies the resulting knowledge to develop and implement policies and actions to improve the health and well being of those populations.”5(p57) Kindig has suggested a similarly broad definition: population health is “the aggregate health outcome of health adjusted life expectancy (quantity and quality) of a group of individuals, in an economic framework that balances the relative marginal returns from the multiple determinants of health.”6(p47) This definition proposes a specific unit of measure of population health and also includes consideration of the relative cost-effectiveness of resource allocation to multiple determinants.
Recently, even in the United States, the term is being more widely used, but often without clarification of its meaning and definition. While this development might be seen as a useful movement in a new and positive direction, increased use without precision of meaning could threaten to render the term more confusing than helpful, as may already be the case with “community health” or “quality of medical care.” For this reason, we propose a definition that may have a more precise meaning for policymakers and academics alike; our purpose is to stimulate active critiques and debate that may lead to further clarification and uniformity of use.
DEFINITION AND CONCEPT
As indicated above, the primary tension or confusion at present seems to be between defining population health as a field of study of health determinants or as a concept of health. The Group Health Community Foundation has recently stated that “some observers see population health as a new term that highlights the influential role of social and economic forces in combination with biological and environmental factors, that shape the health of entire populations . . . others interpret population health primarily as a goal—a goal of achieving measurable improvements in the health of a defined population.”7(p7)
We think that there are 3 general possibilities: population health (a) is only concerned with the independent variables (the multiple determinants), (b) is only concerned with the dependent variables (health outcomes), or (c) is concerned with both the definition and measurement of health outcomes and the roles of determinants. While none of the three is normatively correct or incorrect, we believe that the latter is more appropriate, primarily because the concept and measurement of health and health outcomes focuses attention and research effort on the impact of each determinant and their interactions on some appropriate outcome. It also allows one to consider health inequality and inequity and the distribution of health across subpopulations, as well as the ethical and value considerations underpinning these issues.8
While the original Evans and Stoddart “field model” did not discuss a population health concept in these terms, the idea is implicit in the evolution of the dependent variable from “health care” to “health and function” to “well being.”1(pp33–53) The Institute of Medicine has given serious attention to measuring population health, thereby encouraging some kind of summary measure that includes mortality and health-related quality of life.9
Given these considerations, we propose that population health as a concept of health be defined as “the health outcomes of a group of individuals, including the distribution of such outcomes within the group.” These populations are often geographic regions, such as nations or communities, but they can also be other groups, such as employees, ethnic groups, disabled persons, or prisoners. Such populations are of relevance to policymakers. In addition, many determinants of health, such as medical care systems, the social environment, and the physical environment, have their biological impact on individuals in part at a population level.
Defining population health this way requires some measure(s) of health outcomes of populations, including their distribution throughout the population. We chose the broader term “health outcomes” rather than the more narrow term “health status”; we believe the latter refers to health at a point in time rather than over a period of years. We do not believe that there is any one definitive measure, but we argue that the development and validation of such measures for different purposes is a critical task for the field of population health research.
Our definition does imply the necessity of one or more broad summary measures capable of being a dependent variable for the spectrum of all determinants (generally including length of life and health-related quality and function of those life years), along with a family of other submeasures for different policy and research purposes. For example, the Health Utilities Index is being used in the Canadian National Population Health Survey,10 Years of Healthy Life have been used in Healthy People 2000,11 and the EuroQuol has been recently added to the Medical Expenditure Panel Survey.12
We support the idea that a hallmark of the field of population health is significant attention to the multiple determinants of such health outcomes, however measured. These determinants include medical care, public health interventions, aspects of the social environment (income, education, employment, social support, culture) and of the physical environment (urban design, clean air and water), genetics, and individual behavior. We note with caution that such a list of categories can lead to a view that they operate independently; population health research is fundamentally concerned about the interactions between them, and we prefer to refer to “patterns” of determinants.
Population health researchers tend to use a set of methods and approaches that have the following important characteristics: examination of systematic differences in outcomes across populations, complexity of interactions among determinants, biological pathways linking determinants to population health outcomes, and the influence of different determinants over time and throughout the life cycle.13–15
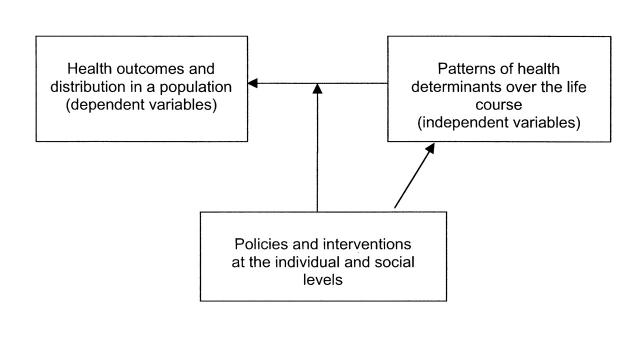
In our view, a population health perspective also requires attention to the resource allocation issues involved in linking determinants to outcomes. Part of the study of population health involves the estimation of the cross-sectoral cost-effectiveness of different types and combinations of investments for producing health.16 Because improvement in population health requires the attention and actions of multiple actors (legislators, managers, providers, and individuals), the field of population health needs to pay careful attention to the knowledge transfer and academic-practice partnerships that are required for positive change to occur.17,18Figure 1 ▶ shows how we view the field of population health. The field investigates each of the components shown in the figure, but particularly their interactions.
FIGURE 1—
A schematic definition of the field of population health.
CRITIQUES
We expect and welcome critiques of the definition presented here. As noted above, one critique will be that the tasks of defining and measuring concepts of health are large enough to constitute a subject of their own, rather than being combined with the study of determinants of health. We have already given our rationale for including them in population health as a field of study, but we would add that the need for accountability argues strongly for the inclusion of outcome and distributional considerations if a population health approach is to be useful in guiding policymaking regarding resource allocation across determinants and sectors. Without such a framework, advocacy and financial incentives for individual determinants can proceed independently of their impact, as some would argue is now the case for some medical care expenditures in the United States.
A second critique is that such a definition and concept is so broad that it includes everything and is therefore not useful to guide either research or policy. We understand this concern but do not agree with it. We believe that a guiding synthesis is essential for considering both the relative impacts of the pattern of determinants and their interactions. Integration of knowledge about health and its multiple determinants seldom occurs. Policy managers typically have responsibility for a single sector; advocacy groups typically have an interest in only one disease or determinant. No one in the public or private sectors currently has responsibility for overall health improvement. We suggest that the importance of a population health perspective is that it forces review of health outcomes in a population across determinants. For population health research, specific investigations into a single determinant, outcome measure, or policy intervention are relevant, and may even be critical in some cases, but they must be recognized as only a part and not the whole.
Those in public health or health promotion may legitimately feel that population health is simply a renaming of what has been their work or legacy. Hamilton and Bhatti have attempted to show the complementarity and overlap between population health and health promotion,19 building on the Canadian Achieving Health for All Framework for Health Promotion20 and the World Health Organization Ottawa Charter on Health Promotion.21 Frank has indicated that historic concepts of public health were similarly broad, until the biomedical paradigm became dominant. Those who define public health as the “health of the public” would not disagree with the definition of population health proposed here; in the words of Frank, the “shift in thinking entailed in population health should be a small one for public health workers . . . in fact it is not so much a shift as a return to our historical roots encompassing all the primary determinants of health in human populations.”22(p163)
However, much of public health activity, in the United States at least, does not have such a broad mandate even in the “assurance” functions, since major determinants such as medical care, education, and income remain outside of public health authority and responsibility, and current resources do not even allow adequate attention to traditional and emerging public health functions. Similarly, we believe that the emerging prominence of social epidemiology is a very important development for population health but does not have the breadth, or imply all of the multiple interactions and pathways, of the definition proposed here for population health.
CONCLUSION
We believe that the time has come for a clarification of the meaning and scope of the term “population health.” We have offered a clarification of the term that combines the definition and measurement of health outcomes and their distribution, the patterns of determinants that influence such outcomes, and the policies that influence the optimal balance of determinants. We welcome discussion and debate regarding these suggestions as a way of moving toward some consensus on this important and emergent concept.
Acknowledgments
D. Kindig was funded in part by the Robert Wood Johnson Health and Society Scholars Planning Grant to the Department of Population Health Sciences at the University of Wisconsin Madison School of Medicine.
We acknowledge the helpful comments of John Mullahy, Stephanie Robert, Donn D’Alessio, John Lavis, and many members of the Robert Wood Johnson Foundation Health and Society Scholars Planning Group.
Both authors contributed equally to the planning and writing of this article.
Peer Reviewed
References
- 1.Evans R, Barer M, Marmor T. Why Are Some People Healthy and Others Not? The Determinants of Health of Populations. New York, NY: Aldine de Gruyter; 1994.
- 2.Frank J. Canada Institute of Population and Public Health. Message from: Dr John Frank, scientific director, Institute of Population and Public Health. Available at: http://www.cihr-irsc.gc.ca/institutes/ipph/about_ipph/ipph_message_director_e.shtml. Accessed December 23, 2002.
- 3.Young TK. Population Health: Concepts and Methods. New York, NY: Oxford University Press; 1998.
- 4.Health Canada. Taking Action on Population Health. Ottawa, Ontario: Health Canada; 1998.
- 5.Dunn JR, Hayes MV. Toward a lexicon of population health. Can J Public Health. 1999;90(suppl 1):S7–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kindig DA. Purchasing Population Health: Paying for Results. Ann Arbor: University of Michigan Press; 1997.
- 7.Kreuter M, Lezin N. Improving Everyone’s Quality of Life: A Primer on Population Health. Atlanta, Ga: Group Health Community Foundation; 2001.
- 8.Williams A. Conceptual and empirical issues in the efficiency-equity trade-off in the provision of health care or, if we are going to get a fair innings, someone will need to keep the score! In: Maynard AJ, ed. Being Reasonable About the Economics of Health. Cheltenham, England: Edward Elgar; 1997:322–349.
- 9.Summarizing Population Health Directions for the Development and Application of Population Metrics. Washington, DC: Institute of Medicine, Division of Health Care Services; 1998. [PubMed]
- 10.Wall R, Foster R. Beyond life expectancy. Health Policy Res Bull. 2002;1:32–33. [Google Scholar]
- 11.Erickson P, Wilson R, Shannon I. Years of Healthy Life. Bethesda, Md: National Center for Health Statistics; 1995. Statistics note no. 7.
- 12.Gold MR, Muenning P. Measure-dependent variation in burden of disease estimates. Med Care. 2002;40:260–266. [DOI] [PubMed] [Google Scholar]
- 13.Berkman L, Kawachi I. Social Epidemiology. New York, NY: Oxford University Press; 2000.
- 14.Keating DP, Hertzman C. Developmental Health and the Wealth of Nations: Social, Biological, and Educational Dynamics. New York, NY: Guilford Press; 1999.
- 15.Adler N, Marmot M, McEwen B, Stewart J. Socioeconomic status and health in industrial nations: social, psychological, and biological pathways. Ann N Y Acad Sci. 1999;896. [PubMed]
- 16.Drummond M, Stoddart G. Assessment of health producing measures across different sectors. Health Policy. 1995;33:219–231. [DOI] [PubMed] [Google Scholar]
- 17.Lavis JN, Ross SE, Hurley JE, et al. Examining the role of health services research in public policy making. Milbank Q. 2002;80:125–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lomas J. Using “linkage and exchange” to move research into policy at a Canadian foundation. Health Aff. 2000;19(3):236–240. [DOI] [PubMed] [Google Scholar]
- 19.Hamilton N, Bhatti T. Population Health Promotion: An Integrated Model of Population Health and Health Promotion. Ottawa, Ontario: Health Promotion Development Division; February1996.
- 20.Epp J. Achieving Health for All: A Framework for Health Promotion. Ottawa, Ontario: Health and Welfare Canada; 1986.
- 21.World Health Organization (WHO). Ottawa Charter on Health Promotion. Copenhagen, Denmark: WHO Regional Office for Europe; 1986.
- 22.Frank JW. Why “population health”? Can J Public Health. 1995;86:162–164. [PubMed] [Google Scholar]