Congenital syphilis can be prevented by testing pregnant women with a serological test developed by Wassermann in 1906 and by treating seropositive women with penicillin, discovered by Fleming in 1928.1,2 Unfortunately, more than 70 years later, congenital syphilis is still a leading cause of perinatal death in many developing countries.3–11
Before 1996, syphilis screening for pregnant women in Haiti’s Artibonite region was done by drawing blood at community dispensaries, transporting the blood to a central laboratory, returning test results to the dispensary, and then treating seropositive women at a follow-up visit. Unfortunately, this centralized prenatal screening strategy failed, and rates of congenital syphilis in the Artibonite region in 1995 were 550 cases per 100 000 live births.9 A decentralized prenatal screening strategy was implemented in 1996.
METHODS
Hospital Albert Schweitzer (HAS) is a nongovernmental organization that serves 250 000 people in Haiti’s rural Artibonite region with community health workers, dispensaries, and a central hospital.12,13 The hospital district is divided into 14 rural zones, each served by a dispensary. Dispensaries are small structures with no running water, no electricity, and outdoor latrines, and many are inaccessible by motor vehicle.
According to HAS and national health surveillance data,14–17 there were 6000 live births in the Artibonite region in 1995, with a 1.7% annual increase in live births in subsequent years. Approximately 80% of pregnant women in the region attend prenatal services at an HAS-affiliated dispensary, and more than 90% deliver at home unattended by medical personnel. Seroprevalence studies conducted in 1996 and 2000 in the Artibonite demonstrated constant rates of syphilis seroreactivity in pregnant women of approximately 6%.9,18,19
In 1996, prenatal syphilis screening was decentralized. A laboratory for performing rapid plasma reagin (RPR) tests (Becton Dickinson, Sparks, Md) was installed in each dispensary. No building construction was necessary. Solar-generated electricity was stored in 6-V batteries and inverted to alternating current for a centrifuge and rotator. Reagents were stored in a propane-powered refrigerator. Personnel from the local community were trained to perform qualitative RPR testing. No new staff was hired, and staff members were not paid extra for performing tests. The cost per dispensary for installation and training was approximately US $3000.
After decentralization, pregnant women attending an HAS-affiliated dispensary for their first prenatal visit had blood drawn during the visit and sera were tested on site. Women whose RPR reactions were positive received same-day treatment with penicillin administered intramuscularly, were given appointments for subsequent doses, were encouraged to notify sexual partners, and were given an appointment for their baby to receive care after delivery.20
In 1996 each of the laboratories was evaluated by an independent laboratory technician using a structured evaluation tool. All sera collected on the day of evaluation were returned to the central laboratory and tested again. RPR-reactive samples were confirmed with fluorescent treponemal antibody testing (Becton Dickinson). For evaluation of clinical practice, charts of women with a reactive RPR test during a 1-month period at 6 dispensaries were reviewed to ensure that women received same-day treatment with penicillin.
At HAS, diagnosis of congenital syphilis is made on the basis of clinical criteria, serology, and radiology. For all years reported, we used the case definition of the US Centers for Disease Control and Prevention (CDC).21 (Updated case definitions can also be found at http://www.cdc.gov/epo/dphsi/casedef.) A list of all suspected cases was made by cross-referencing logs of pediatric admission and discharge diagnoses and laboratory records of RPR testing. Charts of all suspected cases were reviewed. The current protocol was approved by the HAS institutional review board.
RESULTS
Dispensary Laboratories
Between 1996 and 1999, laboratories were installed and personnel trained in 12 of the 14 HAS dispensaries. Laboratories were not installed in 2 dispensaries because of poor cooperation of dispensary staff. An independent laboratory consultant visited each of the laboratories in 1996 and observed that staff members were following manufacturer’s procedures for RPR testing. As part of this evaluation, 649 serum specimens were repeat-tested at the central laboratory. The sensitivity of the RPR tests performed at the dispensary laboratories compared with those performed at the reference laboratory was 41/41 (95% confidence interval [CI] = 91%, 100%) and the specificity was 606/608 (95% CI = 99%, 100%). In a review of clinical practice in 1995, before decentralization, 14 (41%) of 34 pregnant women who tested RPR positive received no penicillin treatment. In 2000, 50 (100%) of 50 women who tested RPR positive received at least one dose of penicillin (P < .001).
Rates of Congenital Syphilis
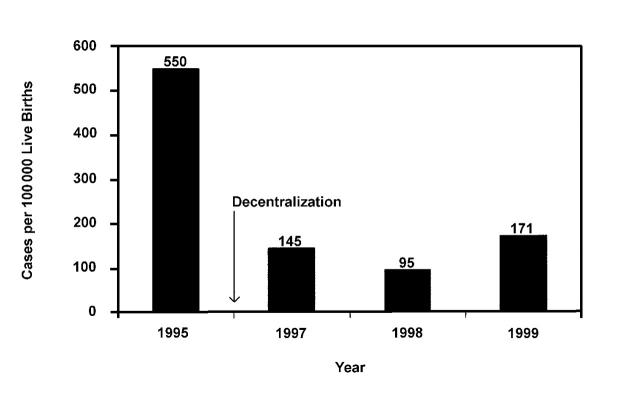
During the study period, the total number of children seen in the HAS outpatient clinic increased from approximately 5000 in 1995 to 8300 in 1999. The total number of children admitted to the HAS inpatient ward increased from 1046 in 1995 to 1114 in 1999. In 1995, the year before decentralization, 33 cases of congenital syphilis were detected, for a rate of 550 cases per 100 000 live births. After decentralization, the number of cases of congenital syphilis decreased to 9 cases in 1997, for a rate of 145 cases per 100 000 live births; to 6 cases in 1998, for a rate of 95 cases per 100 000 live births; and to 11 cases in 1999, for a rate of 171 cases per 100 000 live births. On average, the rate of congenital syphilis in the 3 years after the intervention was 137 cases per 100 000 live births, a 75% decrease from 1995 (preintervention) rates (P < .001; Figure 1 ▶).
FIGURE 1—
Cases of congenital syphilis per 100 000 live births in Haiti’s Artibonite region in the year before decentralization of prenatal screening (1995) and the 3 years after decentralization (1997–1999).
DISCUSSION
Congenital syphilis should be targeted for elimination.22 There is a simple, inexpensive, and sensitive screening test for pregnant women, and penicillin is highly effective in preventing mother-to-child transmission.
Previous studies in developing countries have shown that centralized screening for syphilis in pregnant women is ineffective and that decentralization can dramatically improve the screening process.23–26 Our study shows that a decentralization strategy is feasible in a remote rural area with very limited infrastructure. We believe that if RPR testing can be implemented in the difficult environment of rural Haiti, then it can be implemented in most settings.
We documented a 75% decrease in congenital syphilis rates in the Artibonite region after screening was decentralized. We believe that the efficiency of same-day RPR testing and treatment was critical to the success of this intervention. Improved access to testing may also explain the decrease; however, we do not have data on the proportion of pregnant women who received RPR testing before and after decentralization and cannot state with certainty that access improved. Rates of syphilis in pregnant women were constant during the study period. There were no changes in referrals, in admission procedures, or in fees that would have prevented children from coming to the hospital, and the total number of visits and admissions to HAS increased during the course of the intervention. We do not believe that a variable unrelated to decentralization could explain this sudden drop in congenital syphilis rates. However, as this was an observational study of decentralization, and not a controlled study, we cannot exclude the possibility that another variable may explain the drop.
The rate of congenital syphilis in the 3 years following decentralization, 137 cases per 100 000 live births, was significantly lower than before but still unacceptably high. At present, the decentralized prenatal syphilis screening program continues, and community education is ongoing to encourage all women to seek prenatal care. HAS staff investigate every new case of congenital syphilis in an attempt to identify problems and improve the screening process. The goal is to bring Wasserman and Fleming’s discoveries to the poorest of the poor and to finally eliminate congenital syphilis from the Artibonite region.
Acknowledgments
This project was funded in part by the US Agency for International Development, the Bill and Melinda Gates Foundation, and grant TW00002 from the US Public Health Service.
The authors acknowledge the hard work and dedication of the HAS dispensary staff.
Human Participant Protection
The review of service activities was approved by the Hospital Albert Schweitzer ethics committee.
D. W. Fitzgerald and F. Behets participated in study design, data analysis, and writing of this brief. J. Preval, L. Schulwolf, V. Bommi, and P. Chaillet contributed to data collection, data analysis, and writing.
References
- 1.Dennie CC. A History of Syphilis. Springfield, Ill: Charles C Thomas Press; 1962.
- 2.Tramont EC. Treponema pallidum (syphilis). In: Mandell GL, Bennett JE, Dolin R, eds. Principles and Practice of Infectious Diseases. New York, NY: Churchill Livingstone; 2000:2474–2490.
- 3.Naeye RL, Tafari N, Marboe CC, Judge DM. Causes of perinatal mortality in an African city. Bull World Health Organ. 1977;55:63–65. [PMC free article] [PubMed] [Google Scholar]
- 4.Watts TE, Larsen SA, Brown ST. A case-control study of stillbirths at a teaching hospital in Zambia, 1979–80: serological investigations for selected infectious agents. Bull World Health Organ. 1984;62:803–808. [PMC free article] [PubMed] [Google Scholar]
- 5.Ali Z. Resurgence of congenital syphilis in Trinidad. J Trop Pediatr. 1990;36:104–108. [DOI] [PubMed] [Google Scholar]
- 6.Aiken CG. The causes of perinatal mortality in Bulawayo, Zimbabwe. Cent Afr J Med. 1992;38:263–280. [PubMed] [Google Scholar]
- 7.McDermott J, Steketee R, Larsen S, Wirima J. Syphilis-associated perinatal and infant mortality in rural Malawi. Bull World Health Organ. 1993;71:773–780. [PMC free article] [PubMed] [Google Scholar]
- 8.Ashley D, Greenwood R, McCaw-Binns A, Thomas P, Golding J. Medical conditions present during pregnancy and risk of perinatal death in Jamaica. Paediatr Perinat Epidemiol. 1994; 8(suppl 1):66–85. [DOI] [PubMed] [Google Scholar]
- 9.Fitzgerald DW, Behets F, Lucet C, Roberfroid D. The prevalence, burden, and control of syphilis in Haiti’s rural Artibonite region. Int J Infect Dis. 1998;2:127–131. [DOI] [PubMed] [Google Scholar]
- 10.Mercon de Vargas PR. Avoidable infant and perinatal deaths? Lancet. 2000;356(suppl):s13. [DOI] [PubMed] [Google Scholar]
- 11.Radolf JD, Sanchez PJ, Schulz KF, Murphy FK. Congenital syphilis. In: Holmes KK, Mardh P, Sparling PF, et al., eds. Sexually Transmitted Diseases. New York, NY: McGraw-Hill; 1999:1168–1170.
- 12.Paris B. Song of Haiti: The lives of Dr. Larimer and Gwen Mellon at the Albert Schweitzer Hospital of Deschapelles. New York, NY: Public Affairs; 2000:63–324.
- 13.Berggren WL, Ewbank DC, Berggren GG. Reduction of mortality in rural Haiti through a primary-health-care program. N Engl J Med. 1981;304:1324–1330. [DOI] [PubMed] [Google Scholar]
- 14.World Population Data Sheet. Washington, DC: Population Reference Bureau; 2000:1–12.
- 15.Hospital Albert Schweitzer. Reproductive Health Survey of the Artibonite Valley, 1996. Port au Prince, Haiti: Management Sciences for Health; 1997:1–20.
- 16.Cayemittes M, Rival A, Lerebours G, Barrere B. Survey on Mortality, Morbidity and Utilization of Services (EMMUS-II) 1994/95. Port au Prince, Haiti: Centre Des Enfants Haitiennes and USAID; 1996:15.
- 17.Division du recensement et des enquetes nationals. Recensement general de la population et du logement: resultat pour le department de l’Artibonite 1990. Port au Prince, Haiti: Institut Haitien de Statistique et d’Informatique; 1995.
- 18.Fitzgerald DW, Behets F, Caliendo A, et al. Economic hardship and sexually transmitted diseases in Haiti’s Artibonite Valley. Am J Trop Med Hyg. 2000;62:496–501. [DOI] [PubMed] [Google Scholar]
- 19.Institut Haitien de l’ Enfance, Centres GHESKIO. Etude de sero-surveillance par methode sentinelle de la prevalence du VIH, de la syphilis, et de l’hepatite B chez les femmes enceintes en Haiti 1999–2000. Port au Prince, Haiti: Pan American Health Organization; 2001:21.
- 20.American Academy of Pediatrics. Syphilis. In: Peter G, ed. 1997 Red Book: Report of the Committee on Infectious Diseases. 24th ed. Elk Grove Village, IL: American Academy of Pediatrics; 1997:504–515.
- 21.Centers for Disease Control. Case definitions for public health surveillance. MMWR Morb Mortal Wkly Rep. 1990:39(RR-13);1–43. [PubMed] [Google Scholar]
- 22.Elimination of congenital syphilis. Bull Pan Am Health Organ. 1995;29:364–368. [PubMed] [Google Scholar]
- 23.Hira SK, Bhat GJ, Chikamata DM, et al. Syphilis intervention in pregnancy: Zambian demonstration project. Genitourin Med. 1990;66:159–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Temmerman M, Mohamed Ali F, Fransen L. Syphilis prevention in pregnancy: an opportunity to improve reproductive and child health in Kenya. Health Policy Plann. 1993;8:122–127. [Google Scholar]
- 25.Jenniskens F, Obwaka E, Kirisuah S, et al. Syphilis control in pregnancy: decentralization of screening facilities to primary care level, a demonstration project in Nairobi, Kenya. Int J Gynaecol Obstet. 1995; 48(suppl): S121 – S128. [DOI] [PubMed] [Google Scholar]
- 26.Behets FM, Brathwaite A, Bennett L, Douglas K, Dallabetta G, Figueroa JP. The decentralization of syphilis screening for improved care in Jamaican public clinics. Am J Public Health. 1997; 87:1019–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]