Abstract
Objectives. We compared trends in prevalence rates of preventable cardiovascular- and diabetes-related hospitalizations between African Americans and members of other major US racial/ethnic groups.
Methods. Standardized rates for 1991 to 1998 were derived from hospital and US census data for California.
Results. African Americans had significantly higher hospitalization rates in 1991, and discrepancies in rates continued to widen through 1998. Overall male and female rates were approximately 3 times higher for angina, 7 times higher for hypertension, between 7 and 8 times higher for congestive heart failure, and 10 times higher for diabetes.
Conclusions. Widening disparities in cardiovascular- and diabetes-related health conditions were observed in this study, possibly owing to racial inequalities in provision of effective primary care.
There is a time for everything,
and a season for every activity under heaven.Ecclesiastes 3:1
The relevant health literature is replete with empirical information documenting the disproportionate burden of adverse health outcomes and inequalities in health care experienced by African Americans.1 The existence of these health-related disparities has been well known for years, but there have been limited efforts to understand the complex causal pathways associated with adverse health and quality of care outcomes.2 Little governmental attention and few public resources have been allocated for concerted intervention efforts to ameliorate such disparities until recently.
Two separate but related national health policy initiatives implemented in 1998—the Consumer Protection and Quality in the Health Care Industry Initiative and the Race and Ethnic Health Disparities Initiative—were designed to fundamentally improve overall quality of care and health status among people of color. The Consumer Protection and Quality in the Health Care Industry Initiative was implemented, in part, in response to a groundswell of consumer complaints about deterioration in the general quality of health care associated with the financial and organizational restructuring of the health care industry that occurred in the early 1990s.3
The Race and Ethnic Health Disparities Initiative grew out of former President Clinton’s National Initiative on Race and became a contemporaneous effort to raise public awareness regarding the ongoing prevalence of racial and ethnic discrepancies in health, with an ambitious goal of reducing differentials by 2010.4 Specific goals were incorporated into the nation’s health objectives for the 21st century.5 Achieving improvements in health through reducing rates of cardiovascular disease and diabetes were objectives articulated for African Americans. The first wave of public funds was allocated in 1999 to the Centers for Disease Control and Prevention for targeted community-based intervention efforts.6
Reducing current levels of disparities between African Americans and other racial/ethnic groups over a 10-year period of time is a daunting and—some may argue—unrealistic task. This point is particularly salient for African Americans in light of the endemic and complex nature of competing social constraints stemming from slavery, such as poverty, discrimination, and adverse health coping behaviors, that have historically and collectively contributed to a continuation of differentials in health. Despite these and other obstacles, it is important to establish benchmarks on which to measure success toward achieving health policy goals for this population. More essential perhaps is the need to elucidate pathways that may be associated with the underlying causes of disparity, including racial/ethnic differentials in quality of care for the management of chronic health conditions. A better understanding of this and other potential associations is needed to effectively target intervention efforts designed to ameliorate health status disparities.
Evaluation of potentially avoidable hospitalizations for certain chronic conditions has been identified as a useful and economically efficient measurement tool for monitoring inequalities in distribution of access to quality primary care.7–11 Angina, congestive heart failure (CHF), diabetes, and hypertension are chronic conditions that are frequently used as relevant markers in evaluations of potentially preventable hospitalizations,7–11 because they can often be managed successfully in an ambulatory care setting with appropriate and timely primary care, thereby limiting the need for hospitalization. In addition to providing information on access and quality of care, this type of analysis can be integrated as a proxy measure to assess health status differentials.
Published reports on this topic provide valuable information regarding disparities in terms of preventable hospitalizations; however, limited empirical information is available on African Americans. Pappas et al., for instance, reported that African Americans generally experience higher rates of preventable hospitalizations than Whites, but they did not describe how these rates differ by sex, nor did they compare rates between other major racial/ethnic groups in the United States.10 Other published reports are based on temporal observations and do not provide insight concerning secular trends.7,9 To the best of our knowledge, published information is also not available on patterns of such hospitalizations during the 1990s, a period in which a systematic restructuring of the health care delivery system resulted in an increased emphasis on primary outpatient managed care.12
In the present study, we examined secular trends in estimated prevalence rates of hospitalization for angina, CHF, diabetes, and hypertension among African American men and women and among men and women from 3 other major racial/ethnic groups in the United States between 1991 and 1998. Our goal was to provide new insights concerning the probable association between primary care inequality and racial/ethnic disparities with regard to chronic health, as well as concomitant implications for intervention. Our findings are also intended to provide meaningful benchmarks for policymakers in measuring advancements in Healthy People 2010 health policy objectives concerning reductions in rates of cardiovascular disease and diabetes among African Americans.5
METHODS
Data Source
We analyzed 8 years (1991–1998) of discharge data archived in California’s hospital database9,13; calendar year 1998 was the most recent year in which complete data were available at the time this investigation was conducted. We included in our analyses African American, Asian, White, and Hispanic patients aged 21 to 64 years who were discharged with a principal diagnosis of angina, CHF, diabetes, or hypertension. These diagnoses were based on relevant codes contained in the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM).14 The corresponding labels for the selected diagnostic codes have been described in detail elsewhere.7–10
We excluded patients 65 years or older, because this group has high comorbidity rates7; we also excluded individuals readmitted during the study period, those with pregnancyrelated conditions, and those who died before discharge. Pertinent patient information included the following: self-identified race/ethnicity, sex, age at discharge, year of admission, and type of insurance coverage (self-pay, free care, public Medi-Cal, BlueCross BlueShield, or health maintenance organization).
Data Analysis
We calculated secular trends in hospitalization prevalence rates per 10 000 population, along with 99% confidence intervals, after standardizing rates on the basis of 1990 US census data and subsequent 1991 to 1998 population estimates for California (stratified by sex, age, and race/ethnicity). We presumed that our denominator census data were free of sampling error. Numerators were the aggregate numbers of discharges, by sex and race/ethnicity, among patients aged 21 to 64 years diagnosed with one of the conditions examined.
Sex-specific Poisson regression analyses were used to compare changes in hospitalization rates over time between African Americans and members of the other racial/ethnic groups examined. Adjustments were made for age and type of insurance coverage as potential confounders.15 A first-order Race/Ethnicity × Time interaction term was included to assess differences in changes over time. The level of significance was set at P < .01. Data are presented broken down by sex, emphasizing racial/ethnic differentials between African Americans and the other groups.
RESULTS
Differences in Changes Over Time
Tables 1 ▶ and 2 ▶ present information on number of hospitalizations, relative rates, and mean overall rates per 10 000 population, by race/ethnicity, among men and women, respectively. In general, throughout the 8-year study period, higher rates of hospitalization were observed among African American men for each of the conditions examined (Table 1 ▶). The exception to this pattern was the 3-year period from 1991 through 1993, during which rates of hospitalization for angina were relatively similar between African American and White men. Significant secular improvements occurred thereafter in both racial/ethnic groups. However, as illustrated in Figure 1 ▶, similarities began to diverge in 1994, with steeper secular declines occurring for White men.
TABLE 1—
Secular Trends in Standardized Crude Admission Rates and Mean Admission Rates Associated With Potentially Preventable Hospitalizations for Diabetes- and Cardiovascular-Related Chronic Conditions, by Race/Ethnicity, Among Men Aged 21–64 Years: California, 1991–1998
| Angina | CHF | Diabetes | Hypertension | |||||
| Race/Ethnicity and Year | No. | Rate | No. | Rate | No. | Rate | No. | Rate |
| African American | ||||||||
| 1991 | 891 | 17.7 | 798 | 15.2 | 824 | 16.4 | 435 | 5.1 |
| 1992 | 926 | 17.8 | 930 | 17.9 | 903 | 17.4 | 425 | 5.0 |
| 1993 | 881 | 16.8 | 949 | 18.1 | 923 | 17.6 | 384 | 5.2 |
| 1994 | 622 | 11.4 | 951 | 17.4 | 1004 | 18.4 | 384 | 5.4 |
| 1995 | 656 | 11.8 | 1428 | 25.8 | 1082 | 19.5 | 404 | 5.9 |
| 1996 | 628 | 10.9 | 1299 | 22.6 | 1006 | 17.5 | 411 | 5.4 |
| 1997 | 524 | 9.0 | 1264 | 21.6 | 981 | 16.8 | 424 | 5.5 |
| 1998 | 509 | 8.6 | 1398 | 23.7 | 1064 | 18.0 | 446 | 5.3 |
| Meana: 1991–1998 (99% CI) | 12.8 (9.2, 16.4) | 19.7 (16.9, 22.2) | 17.0 (16.8, 18.0) | 5.3 (5.1, 5.6) | ||||
| Asian | ||||||||
| 1991 | 633 | 7.8 | 194 | 2.9 | 157 | 1.9 | 82 | 1.0 |
| 1992 | 620 | 7.2 | 201 | 3.2 | 162 | 1.9 | 60 | 0.7 |
| 1993 | 602 | 6.8 | 237 | 3.3 | 154 | 1.8 | 64 | 0.7 |
| 1994 | 381 | 4.2 | 250 | 3.2 | 160 | 1.8 | 65 | 0.7 |
| 1995 | 267 | 2.8 | 292 | 4.6 | 161 | 1.7 | 77 | 0.8 |
| 1996 | 260 | 2.7 | 291 | 3.9 | 175 | 1.8 | 84 | 0.9 |
| 1997 | 252 | 2.4 | 345 | 4.0 | 198 | 1.9 | 82 | 0.8 |
| 1998 | 213 | 2.0 | 380 | 4.2 | 206 | 1.9 | 74 | 0.7 |
| Meana: 1991–1998 (99% CI) | 4.5 (2.3, 6.8) | 3.5 (3.1, 3.9) | 1.8 (1.7, 1.9) | 0.8 (0.7, 0.9) | ||||
| White | ||||||||
| 1991 | 9 596 | 17.4 | 2390 | 4.3 | 2210 | 4.0 | 435 | 0.8 |
| 1992 | 9 511 | 17.0 | 2344 | 4.2 | 2250 | 4.0 | 425 | 0.8 |
| 1993 | 8 633 | 15.5 | 2606 | 4.7 | 2133 | 3.8 | 384 | 0.7 |
| 1994 | 4 939 | 8.9 | 2448 | 4.4 | 2135 | 3.8 | 384 | 0.7 |
| 1995 | 2 968 | 5.4 | 3243 | 5.9 | 2354 | 4.3 | 404 | 0.7 |
| 1996 | 2 818 | 5.1 | 2866 | 5.2 | 2169 | 3.9 | 411 | 0.7 |
| 1997 | 2 467 | 4.4 | 2902 | 5.2 | 2292 | 4.1 | 424 | 0.8 |
| 1998 | 2 070 | 3.7 | 3236 | 5.8 | 2292 | 4.3 | 446 | 0.8 |
| Meana: 1991–1998 (99% CI) | 9.6 (4.1, 15.1) | 4.8 (4.3, 5.3) | 3.9 (3.7, 4.1) | 0.7 (0.7, 0.8) | ||||
| Hispanic | ||||||||
| 1991 | 1 315 | 7.2 | 529 | 2.9 | 1164 | 6.4 | 194 | 1.1 |
| 1992 | 1 522 | 7.9 | 608 | 3.2 | 1289 | 6.7 | 184 | 1.0 |
| 1993 | 1 433 | 7.3 | 643 | 3.3 | 1267 | 6.4 | 192 | 1.0 |
| 1994 | 987 | 4.8 | 654 | 3.2 | 1306 | 6.3 | 193 | 0.9 |
| 1995 | 790 | 3.6 | 1006 | 4.6 | 1506 | 6.8 | 182 | 0.8 |
| 1996 | 779 | 3.4 | 884 | 3.9 | 1560 | 6.8 | 221 | 1.0 |
| 1997 | 637 | 2.7 | 957 | 4.0 | 1552 | 6.5 | 245 | 1.0 |
| 1998 | 559 | 2.3 | 1014 | 4.2 | 1681 | 7.0 | 230 | 1.0 |
| Meana: 1991–1998 (99% CI) | 4.8 (2.7, 6.9) | 3.5 (3.1, 3.9) | 6.6 (6.4, 6.8) | 1.0 (0.9, 1.1) | ||||
| Overall | ||||||||
| 1991 | 12 435 | 14.3 | 3881 | 4.5 | 4355 | 5.0 | 967 | 1.1 |
| 1992 | 12 579 | 14.1 | 4083 | 4.6 | 4604 | 5.2 | 930 | 1.0 |
| 1993 | 11 549 | 12.9 | 4435 | 5.0 | 4477 | 5.0 | 915 | 1.0 |
| 1994 | 6 929 | 7.6 | 4303 | 4.7 | 4605 | 5.1 | 935 | 1.0 |
| 1995 | 4 681 | 5.1 | 5969 | 6.5 | 5103 | 5.5 | 988 | 1.1 |
| 1996 | 4 485 | 4.8 | 5340 | 5.7 | 4910 | 5.2 | 1028 | 1.1 |
| 1997 | 3 880 | 4.1 | 5468 | 5.7 | 5023 | 5.3 | 1072 | 1.1 |
| 1998 | 3 351 | 3.5 | 6028 | 6.2 | 5351 | 5.5 | 1065 | 1.1 |
| Meana: 1991–1998 (99% CI) | 8.3 (4.0, 12.6) | 5.4 (4.7, 6.1) | 5.2 (5.0, 5.4) | 1.1 (1.0, 1.1) | ||||
Note. Selected conditions (and related ICD-9-CM hospital discharge rubric codes) were as follows: angina (413.0, 413.1, 413.9 [excluding 411.1, unstable and preinfarction angina]), congestive heart failure (428, 402.01, 402.11, 402.91), diabetes (250.0, 250.1, 250.2, 250.3, 251.0), and hypertension (401, 401.0, 401.1, 401.9, 402.0, 402.1). The African American and White groups reflect self-identified Black and White non-Hispanic race/ethnicity, respectively; the Hispanic group reflects self-identified “other”/Hispanic race/ethnicity. Data were derived from pooled computerized 1991–1998 calendar year hospital discharge data, 1990 US census data, and 1991–1998 population estimates for California. Hospital admission rates were standardized (per 10 000) by sex, and according to age and race/ethnicity, on the basis of census data. CHF = congestive heart failure; CI = confidence interval.
aMean rate per 10 000.
TABLE 2—
Secular Trends in Standardized Crude Admission Rates and Mean Admission Rates Associated With Potentially Preventable Hospitalizations for Diabetes- and Cardiovascular-Related Chronic Conditions, by Race/Ethnicity, Among Women Aged 21–64 Years: California, 1991–1998
| Angina | CHF | Diabetes | Hypertension | |||||
| Race/Ethnicity and Year | No. | Rate | No. | Rate | No. | Rate | No. | Rate |
| African American | ||||||||
| 1991 | 1043 | 15.7 | 909 | 13.7 | 809 | 12.2 | 366 | 5.5 |
| 1992 | 971 | 14.3 | 966 | 14.2 | 792 | 11.7 | 353 | 5.2 |
| 1993 | 960 | 14.1 | 1063 | 15.6 | 817 | 12.0 | 361 | 5.3 |
| 1994 | 763 | 11.1 | 979 | 14.2 | 786 | 11.4 | 392 | 5.7 |
| 1995 | 736 | 10.4 | 1459 | 20.7 | 885 | 12.5 | 436 | 6.2 |
| 1996 | 717 | 10.0 | 1377 | 19.2 | 887 | 12.4 | 442 | 6.2 |
| 1997 | 605 | 8.3 | 1264 | 17.4 | 904 | 12.5 | 427 | 5.9 |
| 1998 | 525 | 7.2 | 1425 | 19.5 | 891 | 12.2 | 470 | 6.4 |
| Meana: 1991–1998 (99% CI) | 11.2 (8.3, 14.1) | 16.3 (14.2, 18.3) | 11.9 (11.3, 12.4) | 5.7 (5.3, 6.1) | ||||
| Asian | ||||||||
| 1991 | 339 | 3.6 | 189 | 2.0 | 128 | 1.4 | 66 | 0.7 |
| 1992 | 391 | 3.9 | 182 | 1.8 | 127 | 1.3 | 84 | 0.8 |
| 1993 | 374 | 3.7 | 215 | 2.1 | 111 | 1.1 | 89 | 0.9 |
| 1994 | 306 | 2.9 | 175 | 1.7 | 138 | 1.3 | 87 | 0.8 |
| 1995 | 226 | 2.0 | 250 | 2.2 | 137 | 1.2 | 87 | 0.8 |
| 1996 | 232 | 2.0 | 212 | 1.9 | 143 | 1.2 | 112 | 1.0 |
| 1997 | 190 | 1.6 | 259 | 2.2 | 134 | 1.1 | 129 | 1.1 |
| 1998 | 185 | 1.5 | 285 | 2.3 | 147 | 1.2 | 122 | 1.0 |
| Meana: 1991–1998 (99% CI) | 2.6 (1.7, 3.6) | 2.0 (1.8, 2.2) | 1.2 (1.1, 1.3) | 0.9 (0.7, 1.0) | ||||
| White | ||||||||
| 1991 | 4560 | 7.2 | 1728 | 2.7 | 2015 | 3.2 | 442 | 0.7 |
| 1992 | 4654 | 7.3 | 1645 | 2.6 | 1994 | 3.1 | 427 | 0.7 |
| 1993 | 4183 | 6.6 | 1822 | 2.9 | 1876 | 3.0 | 470 | 0.7 |
| 1994 | 2896 | 4.6 | 1852 | 2.9 | 1812 | 2.9 | 427 | 0.7 |
| 1995 | 2122 | 3.4 | 2265 | 3.6 | 1903 | 3.0 | 404 | 0.6 |
| 1996 | 1950 | 3.1 | 1994 | 3.2 | 1886 | 3.0 | 443 | 0.7 |
| 1997 | 1795 | 2.8 | 2094 | 3.3 | 1836 | 2.9 | 454 | 0.7 |
| 1998 | 1558 | 2.5 | 2134 | 3.4 | 1853 | 2.9 | 443 | 0.7 |
| Meana: 1991–1998 (99% CI) | 4.6 (2.7, 6.5) | 3.0 (2.7, 3.2) | 2.9 (2.8, 3.1) | 0.7 (0.66, 0.72) | ||||
| Hispanic | ||||||||
| 1991 | 1179 | 5.7 | 590 | 2.9 | 957 | 4.6 | 175 | 0.8 |
| 1992 | 1258 | 5.8 | 647 | 3.0 | 1007 | 4.7 | 227 | 1.1 |
| 1993 | 1177 | 5.4 | 690 | 3.1 | 901 | 4.1 | 237 | 1.1 |
| 1994 | 1045 | 4.6 | 756 | 3.3 | 1103 | 4.9 | 246 | 1.1 |
| 1995 | 842 | 3.5 | 888 | 3.7 | 1045 | 4.3 | 281 | 1.2 |
| 1996 | 832 | 3.4 | 899 | 3.6 | 1161 | 4.7 | 276 | 1.1 |
| 1997 | 778 | 3.0 | 850 | 3.3 | 1194 | 4.7 | 313 | 1.2 |
| 1998 | 629 | 2.4 | 921 | 3.5 | 1198 | 4.6 | 336 | 1.3 |
| Meana: 1991–1998 (99% CI) | 4.8 (2.7, 6.9) | 3.2 (3.0, 3.4) | 4.5 (4.2, 4.8) | 1.1 (1.0, 1.2) | ||||
| Overall | ||||||||
| 1991 | 7121 | 7.1 | 3416 | 3.4 | 3909 | 3.9 | 1049 | 1.0 |
| 1992 | 7274 | 7.1 | 3440 | 3.4 | 3920 | 3.8 | 1091 | 1.1 |
| 1993 | 6694 | 6.6 | 3790 | 3.7 | 3705 | 3.6 | 1157 | 1.1 |
| 1994 | 5010 | 4.9 | 3762 | 3.7 | 3839 | 3.7 | 1152 | 1.1 |
| 1995 | 3926 | 3.7 | 4862 | 4.6 | 3970 | 3.8 | 1208 | 1.1 |
| 1996 | 3731 | 3.5 | 4482 | 4.2 | 4077 | 3.8 | 1273 | 1.2 |
| 1997 | 3368 | 3.1 | 4467 | 4.1 | 4068 | 3.8 | 1323 | 1.2 |
| 1998 | 2937 | 2.7 | 4765 | 4.4 | 4089 | 3.7 | 1371 | 1.3 |
| Meana: 1991–1998 (99% CI) | 4.8 (3.1, 6.5) | 3.9 (3.5, 4.4) | 3.8 (3.7, 3.9) | 1.1 (1.1, 1.2) | ||||
Note. Selected conditions (and related ICD-9-CM hospital discharge rubric codes) were as follows: angina (413.0, 413.1, 413.9 [excluding 411.1, unstable and preinfarction angina]), congestive heart failure (428, 402.01, 402.11, 402.91), diabetes (250.0, 250.1, 250.2, 250.3, 251.0), and hypertension (401, 401.0, 401.1, 401.9, 402.0, 402.1). The African American and White groups reflect self-identified Black and White non-Hispanic race/ethnicity, respectively; the Hispanic group reflects self-identified “other”/Hispanic race/ethnicity. Data were derived from pooled computerized 1991–1998 calendar year hospital discharge data, 1990 US census data, and 1991–1998 population estimates for California. Hospital admission rates were standardized (per 10 000) by sex, and according to age and race/ethnicity, on the basis of census data. CHF = congestive heart failure; CI = confidence interval.
aMean rate per 10 000.
FIGURE 1—
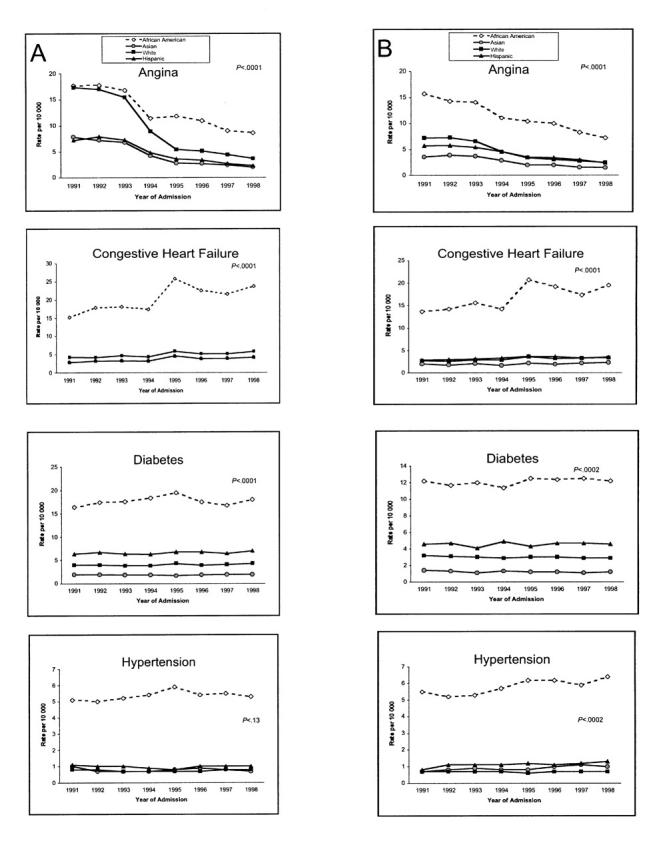
Secular trends in standardized crude admission rates associated with potentially preventable hospitalizations among men (a) and women (b) aged 21–64 years for selected diabetes- and cardiovascular-related chronic conditions, by race/ethnicity: California, 1991–1998.
Note. The P value reflects the significance level associated with the main effect variable of time, derived from separate sex-specific, age-adjusted Poisson regression models for each of the 4 conditions.
Overall rates of hospitalization for CHF and diabetes increased significantly from 1991 through 1998 regardless of race/ethnicity, with no significant changes occurring in the pattern of admission with respect to hypertension (Figure 1 ▶). However, markedly higher and persistent rates of hospitalization for CHF, diabetes, and hypertension were observed in African American men. In 1991, the rate of hospitalization for CHF was 15.2 per 10 000 among African American men, as compared with lower respective rates of 2.9, 4.3, and 2.9 among Asian, White, and Hispanic men. The proportional change over time was greater among African Americans: 23.7 per 10 000 in 1998, as compared with 4.2, 5.8, and 4.2 per 10 000 among Asians, Whites, and Hispanics, respectively. Similar magnitudes of disparity were observed for diabetes and hypertension.
There were also wide variations in mean aggregate rates of hospitalization for each of the selected conditions, with higher mean admission rates observed among African American men (Table 1 ▶). Mean admission rates for diabetes were 17.0 per 10 000 among African American men and 1.8, 3.9, and 6.6 per 10 000 among Asian, White, and Hispanic men, respectively. Wide discrepancies were present in the pattern of hospitalizations for hypertension as well, with 5.3 mean admissions per 10 000 among African American men and mean rates of 0.8, 0.7, and 1.0 per 10 000 among Asian, White, and Hispanic men, respectively.
The data displayed in Table 2 ▶ reveal similar patterns among African American women. However, unlike the case for African American and White men, African American women had a substantially higher rate of hospitalization for angina in 1991 than White women (15.7 vs 7.2 per 10 000). Figure 1B ▶ shows a pattern of significant overall secular decreases in the pattern of admissions for angina along with concurrent increases for CHF, diabetes, and hypertension. Higher rates and wider racial/ethnic disparities were present in African American women, regardless of direction. Similar race/ethnicity differentials existed in patterns of mean admission rates.
Crude Overall Rate Ratios and Adjusted Poisson Regression Results
Standardized overall crude rate ratios are presented in Table 3 ▶, along with respective P values derived from the adjusted sexspecific Poisson regression models. In general, a greater degree of disparity was observed between Asians and African Americans with regard to diabetes. Hospitalization rates were almost 10 times higher among African American men and women than among Asian men and women. A lesser (but significant) degree of disparity was observed between Whites and African Americans for angina-related hospitalizations. In comparison with White men and women, African American men and women experienced threefold higher rates of hospitalization for this condition.
TABLE 3—
Crude Overall Rate Ratios (RRs), by Race/Ethnicity and Time, Associated With Potentially Preventable Hospitalizations (per 10 000) Among Men and Women Aged 21–64 Years for Selected Chronic Conditions: California, 1991–1998
| Angina | CHF | Diabetes | Hypertension | |||||||||
| RR | 99% CI | P | RR | 99% CI | P | RR | 99% CI | P | RR | 99% CI | P | |
| Men | ||||||||||||
| African American vs | ||||||||||||
| Asian | 3.2 | 2.6, 4.0 | <.0001 | 7.0 | 5.8, 8.3 | <.0001 | 9.6 | 8.1, 12.0 | <.0001 | 6.8 | 4.9, 9.6 | <.0001 |
| Caucasian | 1.6 | 1.3, 2.1 | <.0001 | 4.1 | 3.5, 4.6 | <.0001 | 4.4 | 3.8, 4.9 | <.0001 | 7.1 | 6.1, 8.9 | <.0001 |
| Hispanic | 2.9 | 2.3, 3.4 | <.0001 | 5.6 | 4.8, 6.6 | <.0001 | 2.7 | 2.1, 3.2 | <.0001 | 5.4 | 4.3, 6.9 | <.0001 |
| Time (1991–1998) | 0.15 | 0.14, 0.16 | <.0001 | 1.38 | 1.32, 1.45 | <.0001 | 1.12 | 1.07, 1.18 | <.0001 | 1.06 | 0.96, 1.17 | .13 |
| Race/Ethnicity × Time: African American vs | ||||||||||||
| Asian | . . . | . . . | <.0001 | . . . | . . . | .28 | . . . | . . . | .19 | . . . | . . . | .09 |
| Caucasian | . . . | . . . | <.0001 | . . . | . . . | .28 | . . . | . . . | .30 | . . . | . . . | .09 |
| Hispanic | . . . | . . . | <.0001 | . . . | . . . | <.0001 | . . . | . . . | .08 | . . . | . . . | .08 |
| Women | ||||||||||||
| African American vs | ||||||||||||
| Asian | 4.4 | 3.9, 5.0 | <.0001 | 8.2 | 7.3, 9.1 | <.0001 | 9.9 | 9.0, 10.8 | <.0001 | 6.7 | 5.8, 7.5 | <.0001 |
| Caucasian | 2.6 | 2.2, 3.0 | <.0001 | 5.5 | 5.1, 5.8 | <.0001 | 4.0 | 3.9, 4.2 | <.0001 | 8.3 | 7.7, 9.0 | <.0001 |
| Hispanic | 2.7 | 2.5, 2.9 | <.0001 | 5.1 | 4.7, 5.5 | <.0001 | 2.6 | 2.5, 2.8 | <.0001 | 5.1 | 4.6, 5.9 | <.0001 |
| Time (1991–1998) | 0.26 | 0.25, 0.28 | <.0001 | 1.20 | 1.14, 1.26 | <.0001 | 0.93 | 0.88, 0.98 | <.0002 | 1.14 | 1.04, 1.26 | <.0002 |
| Race/Ethnicity × Time: African American vs | ||||||||||||
| Asian | . . . | . . . | .0002 | . . . | . . . | <.02 | . . . | . . . | .003 | . . . | . . . | .006 |
| Caucasian | . . . | . . . | <.0001 | . . . | . . . | <.009 | . . . | . . . | .18 | . . . | . . . | .34 |
| Hispanic | . . . | . . . | .02 | . . . | . . . | <.006 | . . . | . . . | .80 | . . . | . . . | .15 |
Note. Selected conditions (and related ICD-9-CM hospital discharge rubric codes) were as follows: angina (413.0, 413.1, 413.9 [excluding 411.1, unstable and preinfarction angina]), congestive heart failure (428, 402.01, 402.11, 402.91), diabetes (250.0, 250.1, 250.2, 250.3, 251.0), and hypertension (401, 401.0, 401.1, 401.9, 402.0, 402.1). The African American and White groups reflect self-identified Black and White non-Hispanic race/ethnicity, respectively; the Hispanic group reflects self-identified “other”/Hispanic race/ethnicity. Results were derived from 4 separate sex-specific Poisson regression models. Each model included the following coding scheme. The outcome variable was rate of admission, and the independent variables were race/ethnicity (African American, Asian, White, Hispanic, with African American as the comparison group), and year of admission (1991–1998). Covariates included age (21–44 years, 45–64 years) and type of health insurance coverage (public Medi-Cal, private BlueCross BlueShield, private health maintenance organization, self-pay, free care). All models included first-order Race/Ethnicity × Time interaction terms. The level of significance was set at P ≤ .01. Data were derived from pooled computerized 1991–1998 calendar year hospital discharge data, 1990 US census data, and 1991–1998 population estimates for California. Hospital admission rates were standardized (per 10 000) by sex, and according to age and race/ethnicity, on the basis of census data. CHF = congestive heart failure; CI = confidence interval.
Analysis of the interaction between race/ethnicity and time revealed that significant changes in rates of hospitalization occurred over time between African American men and women and men and women in the other racial/ethnic groups. In the case of some conditions—for example, diabetes and hypertension—wide racial/ethnic differentials persisted over the entire 8-year study period, resulting in a lack of statistical changes in magnitude.
DISCUSSION
Our results reveal that, during the 1990s, there were significant secular disparities between African Americans and the other major US racial/ethnic groups with regard to potentially preventable cardiovascular- and diabetes-related chronic conditions. Disparities widened over time and remained after adjustments had been made for age and health insurance status. Degrees of variation relative to other groups were similar among African American men and African American women.
General overall patterns revealed significant secular declines in rates of hospitalization for angina among male and female members of all of the racial/ethnic groups examined; however, slopes were less steep for African American men and women. Particularly striking was the degree of variation in patterns of hospitalization for CHF, diabetes, and hypertension. Asian, White, and Hispanic men and women had relatively low rates of hospitalization for each of these conditions in 1991, whereas rates among African American men and women were disproportionately higher.
For instance, the rate of hospitalization for diabetes among African American men was approximately 5 times higher than that observed for Asian men and 4 times higher than that of both White and Hispanic men, and African American women exhibited a ninefold higher rate of diabetes hospitalizations than Asian women and an approximately fourfold higher rate than White and Hispanic women. Similar differentials were observed for the other conditions examined, with widening racial/ethnic disparities continuing over time through 1998. Indeed, with the exception of angina among White men during the initial 3-year period of the study, rates of hospitalization for the conditions assessed remained low in the other racial/ethnic groups throughout the entire study period (Figure 1 ▶).
These findings suggest that the health status of African Americans may have worsened over the past decade. The increasing rates of hospitalization may also reflect concomitant patterns in the general incidence of cases of each of the selected study conditions, as exemplified in the secular trend for CHF.16 However, this is unlikely to explain the substantial racial/ethnic differentials during the same time period for conditions such as hypertension and diabetes. Our findings, although based on individuals hospitalized in California, may nevertheless portend broader national patterns.
The present results suggest that inequalities in the provision of quality primary care may have had an impact on African Americans with chronic cardiovascular- and diabetesrelated conditions. This aspect of our findings is particularly notable given the concurrent events that took place during the study period, including rapid advances in medical technologies and pharmacological interventions and a shift from inpatient treatment to an increased emphasis on primary care physicians as “gatekeepers” in outpatient managed care.11
Other studies have documented discrepancies in rates of preventable hospitalizations based on various sociodemographic characteristics, including income, type of health insurance coverage, and geographic location.7–10 Few researchers, however, have reported differences according to race/ethnicity. The findings generated from our study provide new information on additional dimensions of health status and quality of care among African Americans. These results, however, should be interpreted with caution before extrapolation beyond this context.
LIMITATIONS
Angina, CHF, and diabetes are chronic conditions in which ambulatory care is not expected to completely prevent the need for occasional hospitalization. Indeed, the clinical nature of each of these conditions will undoubtedly necessitate periodic hospitalizations as a result of episodes of acute exacerbation. However, one would not expect this to be the case among individuals with hypertension, because the onset of malignant hypertension or accelerated hypertension should be rare among patients receiving quality medical care. Thus, our findings may indicate the need for interventions beyond routine outpatient care to stabilize exacerbations of angina, CHF, and diabetes. Further research, however, is needed to better elucidate potential factors associated with the profound degree of variation in rates of admission revealed here between African Americans and those in the other racial/ethnic groups.
African Americans have disproportionately higher rates of clinical and behavioral risk factors attributable to angina, CHF, diabetes, and hypertension,17 and these conditions occur more frequently among African Americans than among members of other racial/ethnic groups. Therefore, increased rates of hospitalization may be associated with higher prevalence rates of single and multiple risk factors that contribute to a greater likelihood of inpatient care. Although plausible, risk factor prevalence would not completely explain all of the variance associated with our observation of secular increases and widening disparities in hospitalization rates.
Studies have shown that African Americans are less likely than members of other racial groups to be exposed to quality medical interventions.18 The present findings may be related to clinical and behavioral differences between various racial/ethnic groups; they may also be an indication of adverse health outcomes stemming from differences between groups in the provision and availability of effective primary care case management.
Other potential contributing factors may include lower medication compliance rates and lower socioeconomic status, both of which have been shown to be more prevalent among African Americans than among members of other groups.19,20 Data limitations precluded assessment of medication compliance. We did, however, evaluate type of health care insurance coverage as an alternative measure for socioeconomic status. Findings revealed a significant independent relationship between rates of hospitalization and type of coverage among both men and women. Individuals with publicly funded coverage had higher hospitalization rates than those with privately funded coverage; however, there was no interaction effect with race/ethnicity to suggest that higher hospitalization rates among African Americans were due to type of health insurance coverage. Finally, we are aware that our findings may not be generalizable beyond the state of California; however, we would expect similar results in other regions of the country with similar racial/ethnic compositions.
CONCLUSIONS
Despite the limitations just described, observational evaluation of trends in potentially preventable hospitalizations may be an economically efficient and useful method in which to monitor secular changes in health status and access to quality primary care across racial/ethnic groups. Our results reveal significant inequalities in the distribution of hospitalizations among African Americans residing in California during the last decade of the 20th century for conditions that potentially could be managed in ambulatory care health care settings. These findings may have broader national implications.
Our results also reveal the presence of wide disparities in rates of hospitalization for cardiovascular- and diabetes-related conditions in 1998, the year in which the Race and Ethnic Health Disparities Initiative was implemented.4 This information provides useful benchmark indicators for policymakers to measure success in achieving Healthy People 2010 national health policy objectives concerning reductions in cardiovascular disease and diabetes among African Americans.5 It also perhaps implies the need for the development of specific policy instruments (e.g., economic disincentives) designed to alter and improve current provider behavior. New policy instruments and tools are also needed to ensure equal access to quality health care.3
Reports of inferior health and health care among African Americans have persisted over time, with limited efforts made to intervene or understand potential causal factors. Well-established behavioral risk factors such as obesity and cigarette smoking are disproportionately prevalent in African Americans.17 However, other less established risk factors may also influence health status differentials. Our findings suggest that inequality in the provision of effective primary care for certain chronic conditions may be associated with health disparities in African Americans. More research is needed to elucidate other similar associations.
Health policy initiatives implemented during the last decade of the 20th century focused belated attention to—and, subsequently, resources on—reversing ongoing negative health trends. The development of tailored policy interventions designed to influence the behavior of primary care providers regarding quality of care in the management of chronic conditions may yield tangible improvements in the health status of African Americans and other disproportionately affected race/ethnic groups. Policymakers have established a national goal of reducing cardiovascular disease and diabetes health disparities by 2010. A subsequent long-term goal should be developed that articulates not only continued reductions in, but the eventual elimination of, racial/ethnic disparities in health and health care. Policy interventions aimed at health care providers have the potential to achieve such goals.
Acknowledgments
This work was supported by a scientist development award and a grant-in-aid from the National American Health Association to Sharon K. Davis.
We would like to thank Rebecca Din, MD, PhD, and Judy Hughes, MS, for their thoughtful insights on earlier versions of this article, as well as Candice Hall-Wilcox and Pat Abramson for preparation of tables and graphs.
Human Participant Protection
Ethical clearance for this research was obtained from the institutional review board of the Morehouse School of Medicine.
S. K. Davis conceptualized the study and its design and assisted with interpretation of the findings. Y. Liu conducted the statistical analysis and provided assistance in the study design and interpretation of the findings. G. H. Gibbons provided assistance in interpreting the clinical significance of the research findings.
Peer Reviewed
References
- 1.Cooper R. Health and social status of US blacks. Ann Epidemiol. 1993;3:137–144. [DOI] [PubMed] [Google Scholar]
- 2.Ford R, Cooper RS. Implications of race/ethnicity for health and health care use. Health Serv Res. 1995;301:237–252. [Google Scholar]
- 3.Quality First: Better Health Care for All Americans. Washington, DC: President’s Advisory Commission on Consumer Protection and Quality in the Health Care Industry; 1998.
- 4.Satcher D. The initiative to eliminate racial and ethnic health disparities is moving forward. Public Health Rep. 1999;14:283–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Healthy People 2010. Washington, DC: US Dept of Health and Human Services; 2000.
- 6.Davis SK, Liu Y, Troutman A. Baseline disparities in preventable cardiovascular hospitalizations among African American men and women in Atlanta’s Empowerment Zone: benchmarks for CDC’s REACH 2010 objectives. Paper presented at: 129th Annual Meeting of the American Public Health Association, 21–25October2001, Atlanta, Ga.
- 7.Weissman JS, Gatsonis C, Epstein AM. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. JAMA. 1992;268:2388–2394. [PubMed] [Google Scholar]
- 8.Billings J, Zeitel L, Lukomnik J, Carey T, Blank A, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff. 1993;12:162–173. [DOI] [PubMed] [Google Scholar]
- 9.Bindman AB, Grumback K, Osmond D, et al. Preventable hospitalization and access to health care. JAMA. 1995;274:304–311. [PubMed] [Google Scholar]
- 10.Pappas G, Hadden WC, Kozak LJ, Fisher GF. Potentially avoidable hospitalizations: inequalities in rates between US socioeconomic groups. Am J Public Health. 1997;87:811–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Preventable Hospitalizations in Massachusetts. Boston, Mass: Division of Health Care Finance and Policy; 1998. Publication 18232-62-1000-04/98-DHCFP-C.R.
- 12.Epstein AM. Changes in the delivery of care under comprehensive health care reform. N Engl J Med. 1993;329:1672–1676. [DOI] [PubMed] [Google Scholar]
- 13.California Hospital Discharge 1991–1998 Data. Sacramento, Calif: Office of Statewide Health Planning and Development; 1999.
- 14.International Classification of Diseases, 9th Revision, Clinical Modification. Los Angeles, Calif: Practice Management Information Corp; 1993.
- 15.Thall PF. Mixed Poisson likelihood regression models for longitudinal interval count data. Biometrics. 1998;44:197–209. [PubMed] [Google Scholar]
- 16.Morbidity and Mortality: 2000 Chartbook on Cardiovascular, Lung, and Blood Diseases. Washington, DC: US Dept of Health and Human Services; 2000.
- 17.Health, United States, 1998 With Socioeconomic Status and Health Chartbook. Hyattsville, Md: National Center for Health Statistics; 1998.
- 18.Morehouse Medical Treatment and Effectiveness Center. A Synthesis of the Literature: Racial and Ethnic Differences in Access to Medical Care. Menlo Park, Calif: Henry J Kaiser Family Foundation; 2000.
- 19.Shea S, Misra D, Ehrlich MH, Field L, Francis CK. Predisposing factors for severe, uncontrolled hypertension in an inner-city minority population. N Engl J Med. 1992;327:776–781. [DOI] [PubMed] [Google Scholar]
- 20.Report of the Working Group on Research in Coronary Heart Disease in Blacks. Bethesda, Md: National Institutes of Health; 1994.


