Abstract
Objectives. We investigated socioeconomic disparities in injury hospitalization rates and severity-adjusted mortality for pediatric trauma.
Methods. We used 10 years of pediatric trauma data from Sacramento County, Calif, to compare trauma hospitalization rates, trauma mechanism and severity, and standardized hospital mortality across socioeconomic strata (median household income, proportion of households in poverty, insurance).
Results. Children from lower–socioeconomic status (SES) communities had higher injury hospitalization and mortality rates, and presented more frequently with more lethal mechanisms of injury (pedestrian, firearm), but did not have higher severity-adjusted mortality.
Conclusions. Higher injury mortality rates among children of lower SES in Sacramento County are explained by a higher incidence of trauma and more fatal mechanisms of injury, not by greater injury severity or poorer inpatient care.
Injury rates and injury mortality rates among children are well known to be associated with socioeconomic factors. Several studies have documented increased rates of injury and injury mortality among children who are from racial and/or ethnic minority groups,1 who lack medical insurance,2 who reside in lowincome communities,3–7 and whose mothers have fewer years of education.8,9
Although the majority of this research supports an association between markers of poverty and high injury and injury mortality rates, some investigators have questioned the etiology and significance of these relationships.10,11 Several factors potentially contribute to the higher injury mortality rates among children from low-income communities; these include the overall incidence of injury, the average severity of injury, and severity-adjusted mortality (i.e., the observed mortality compared with the expected mortality, where expected mortality is dependent on injury severity). Little is known about how much each of these factors contributes to the observed socioeconomic disparities in injury mortality rates among children.
Our primary aims in this study were to investigate the relationship between the socioeconomic status (SES) of pediatric trauma patients and the severity of their injuries on presentation to the emergency department (ED) and their severity-adjusted (i.e., standardized) hospital mortality. Specifically, using population-based data, we explored whether the trauma hospitalization rate among children from lower-SES neighborhoods is actually higher than that among children from higher-SES neighborhoods, and if so, whether this difference is explained by more frequent minor trauma (low severity of injury), more frequent major trauma (high severity of injury), or both. Secondarily, we investigated whether severity-adjusted trauma mortality is associated with SES. Our hypotheses were that children from communities of lower SES present to a particular regional trauma center with more severe injuries than children from communities of higher SES, and that children from communities of lower SES have higher standardized hospital mortality than children from communities of higher SES.
METHODS
The University of California, Davis, Children’s Medical Center (UCDCMC) is the single designated pediatric trauma center for Sacramento County Emergency Medical Services (EMSC). UCDCMC receives all pediatric trauma cases with the exception of “critical trauma patients”—those without an effective or established airway or those requiring cardiopulmonary resuscitation. These children are transported to the closest available facility and then transferred to the UCDCMC ED once stabilized.
All children admitted to UCDCMC with acute trauma, defined as a bodily injury occurring less than 24 hours before presentation to the ED, are included in a comprehensive trauma registry. The trauma registry includes physiological and laboratory data collected at the time of presentation, as well as demographic and diagnostic data collected at the time of discharge for all trauma patients. For patients transferred to UCDCMC from another facility, the referring hospital’s physiological and laboratory data are entered when available.
All patients in the trauma registry aged 18 years or younger who were admitted to UCDCMC between July 1, 1988, and June 30, 1998, were included in the analyses. Because our analyses were population-based, patients whose primary residence was outside Sacramento County were excluded. Subjects in the database were selected if any of the first 10 International Classification of Diseases, Ninth Revision, Clinical Modification12 (ICDM-9-CM) codes included 800 to 904.9, 910 to 929.9, 950 to 957.9, or 959. This definition omitted late effects (codes 905–909), foreign body injuries (codes 930–939), burns (codes 940–949), and certain early complications of trauma (code 958). Victims of child abuse (code 995.5) were excluded, because these patients are not usually cared for by trauma surgeons and are not routinely included in the trauma registry. Trained medical coders determined the mechanism of injury, and we categorized the codes by applying the recommended framework of the Centers for Disease Control and Prevention for presenting injury mortality data.13
To estimate the SES for patients, we used 3 variables: US Census median household income, US Census proportion of families below the poverty line, and insurance status.14,15 The US Census measures were intended to reflect the patients’ community SES and were obtained by matching 1990 US Census data to the complete home address of the patient. We performed geocoding with Dynamap/ZIP Codes (Geographic Data Technology, Lebanon, NH). We successfully matched home addresses for 94.4% of the patients. For these patients, US Census data were obtained at the census-block level, providing more precise measures of the specific community SES than zip code–level data. For the remaining 5.6% of the patients, for whom we could geocode only zip codes, the data from the median census block within the zip code were used. Insurance status, a proxy for individual SES, was categorized as “Medicaid” (which included patients with Medicaid, pending Medicaid, county-designated medically indigent, and self-pay) and “other” (which included contracted and private insurance). Self-pay patients represented less than 10% of the Medicaid category because of California’s relatively broad eligibility criteria for Medicaid.
We generated trauma hospitalization rate ratios and mortality rate ratios stratified by SES with block-level census estimates for the population of children under 18 years of age. We defined trauma mortality with inpatient data only, without any time restriction. We developed a customized severity-of-injury model for each blunt and penetrating trauma that took into account the following variables: age, Glasgow Coma Scale (GCS) score, systolic blood pressure, and respiratory rate on presentation to the ED. Also, we generated the Injury Severity Score (ISS)16,17 and the individual components of the A Severity Characterization of Trauma (ASCOT)18,19 from the ICDM-9-CM codes with ICDMAP-90 (TriAnalytics Inc, Baltimore, Md). ASCOT utilizes Anatomic Profile components that describe anatomic injury to the head, brain, and spinal cord (AP-A); anatomic injury to the thorax and front of neck (AP-B); and all other serious injuries (AP-C).
We analyzed all potential continuous and ordinal independent variables by use of logit plots and transformed them to generate a log-linear relation with mortality when necessary. Age was “Winsorized”20 above 6 years, because the log-linear relation between mortality and age was present only up to that age; after that point, the relation had an approximate slope of 0. Therefore, all ages older than 6 years were reclassified as age 6 years. Similarly, AP-B was Winsorized above age 4. AP-C was dichotomized as age 3 or younger and over age 3. We used a quadratic transformation of systolic blood pressure because of its parabolic relation with the log odds of survival. We then performed a logistic regression, with statistical significance defined at the level of P < .05. We removed variables not associated with mortality in the multivariate analyses (P > .50) from the final logistic regression.
To evaluate the association between SES and the mortality rate of pediatric trauma patients, we individually forced each of the following measures of SES into the final logistic regression: median household income (continuous variable), proportion of households below the poverty level (continuous variable), and insurance status (nominal variable). We compared standardized mortality ratios (SMRs—observed mortality rate divided by predicted mortality rate) across SES strata by applying the standard z score.21 We estimated that a sample size of 4090 would be sufficient to detect a mortality risk ratio of 1.3 (for patients of lower SES compared with patients of higher SES), assuming 5% overall mortality, a 2-tailed α level of 0.05, a β level of 0.20, and an R2 of 0.5 with other covariates.
RESULTS
From the 10 years of data, there were 5507 children under 18 years of age admitted with a trauma diagnosis specified in our inclusion criteria. Of these, 1582 patients (29%) were excluded because their residential address was outside Sacramento County. Another 15 patients were excluded because of a diagnosis of child abuse, maltreatment, or neglect. Seventy patients (6 deaths) were excluded because of missing vital sign and physiological data. The final sample included 3855 subjects, of whom 131 died (3.4%). The mean age of the children in the sample was 12.6 years, and 67.6% were male. The mean GCS score was 13.8, and the mean ISS was 8.7. The mean of the median household annual income was $30 250, the mean of the proportion of households below the poverty line was 17.6%, and the proportion of patients with Medicaid was 40.9%.
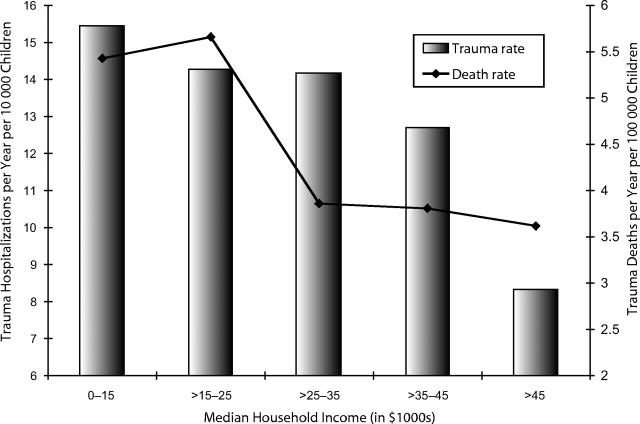
Figure 1 ▶ demonstrates the declining trauma hospitalization rate and trauma mortality rate with increasing median household income. We noted a similar relationship when hospitalization rates and mortality rates were plotted against the proportion of households below the poverty line (data not shown). Table 1 ▶ demonstrates the differences in mechanism of trauma across income categories. Mortality rates varied depending on the mechanism of injury: firearm injuries and pedestrian trauma (children struck by a motor vehicle) were more lethal than assaults and motor vehicle crashes (driver or occupant). There was a higher incidence of trauma hospitalization among children from lower-SES communities for all mechanisms of injury except motor vehicle crashes. Table 1 ▶ also demonstrates the higher incidence of mild or moderately severe injury (defined by ISS) among children from lower-SES communities. The incidence of severe injury (ISS > 18) did not vary systematically across socioeconomic strata.
FIGURE 1—
Trauma hospitalization and death rate by median household income in Sacramento County, 1988–1998.
TABLE 1—
Trauma Admissions Per 10 000 Children Over Age 18 Per Year in Sacramento County, 1988–1998
| Median Annual Household Income ($) | ||||||
| Mechanism of Injury | N (% Deaths) | < 5000 | 15 001–25 000 | 25 001–35 000 | 35 001–45 000 | > 45 000 |
| Assault | 387 (1.6) | 2.3 | 1.5 | 1.6 | 1.1 | 0.36 |
| Pedestrian struck | 743 (4.7) | 3.7 | 3.2 | 2.5 | 2.4 | 1.1 |
| Firearm injury | 457 (9.4) | 2.4 | 2.3 | 1.7 | 1.1 | 0.48 |
| Motor vehicle crash | 1273 (2.4) | 3.6 | 3.8 | 4.6 | 4.7 | 3.9 |
| Other | 995 (1.7) | 2.4 | 2.3 | 1.7 | 1.1 | 0.5 |
| Mild injury (ISS ≤ 4) | 1531 (0.2) | 6.9 | 5.7 | 5.6 | 4.9 | 2.9 |
| Moderate injury (ISS = 5–18) | 1736 (0.9) | 6.9 | 6.4 | 6.1 | 5.9 | 3.9 |
| Severe injury (ISS > 18) | 598 (19.0) | 1.2 | 1.3 | 1.5 | 1.2 | 1.0 |
Note. ISS = Injury Severity Score.
Table 2 ▶ shows the results of the logistic regression survival prediction model. To facilitate comparison with the trauma health services literature, we estimated the model with survival rather than mortality as the outcome variable. Factors associated with an increased probability of survival included older age (up to 6 years), less severe AP-A and AP-C injuries, higher GCS score, and systolic blood pressure at the 80th percentile (a measurement of 142 mm Hg was associated with the highest survival in the quadratic transformation). AP-B injuries were associated with a higher probability of survival after adjustment for other variables. This model had a C statistic of 0.99 and a Hosmer–Lemeshow goodness-of-fit test P value of .69, with no evidence of systematic prediction error across deciles. Adding the 3 SES proxy variables individually to the model only minimally changed the coefficients for demographic and physiological predictors (data not shown). Median household income, percentage below the poverty line, and Medicaid status were not significantly associated with survival; however, patients with Medicaid tended to have lower severity-adjusted survival, with an odds ratio (OR) of 0.56 (95% confidence interval [CI] = 0.31, 1.03).
TABLE 2—
Results of Logistic Regression Predicting Survival Among Pediatric Trauma Patients in Sacramento County, 1988–1998
| Parameter | Estimate (Standard Error) | Odds Ratio (95% Confidence Interval) | P |
| Agea | 0.18 (0.087) | 1.19 (1.00, 1.42)b | .044 |
| AP-A | – 0.45 (0.08) | 0.64 (0.54, 0.74)c | <.001 |
| AP-Bd | 0.32 (0.13) | 1.34 (1.07, 1.78)c | .014 |
| AP-C > 3e | – 1.20 (0.42) | 0.30 (0.13, 0.69)c | .004 |
| Glasgow Coma Scale | 0.37 (0.047) | 1.45 (1.32, 1.59)f | <.001 |
| SBP | 0.08 (0.012) | 1.08 (1.06, 1.11) | <.001 |
| (SBP)2 | – 0.00028 (0.00005) | 1.00 (1.00, 1.00) | <.001 |
| Median household income | 0.009 (0.012) | 1.01 (0.98, 1.03)g | .74 |
| Below poverty line (%) | 0.00089 (0.0012) | 1.00 (0.99, 1.01)h | .46 |
| Insurance | |||
| Other | 1.0 | Reference | . . . |
| Medicaid | – 0.58 (0.31) | 0.56 (0.31, 1.03) | .06 |
Note. AP-A = anatomic injury to the head, brain, and spinal cord; AP-B = anatomic injury to the thorax and front of neck; AP-C = all other serious injuries; SBP = systolic blood pressure. The 3 proxies for socioeconomic status were forced individually into the logistic regression.
aAge is Winsorized at 6 years, meaning that values greater than 6 were reset to 6 because there was no univariate association between age and logit trauma mortality above that age.
bOdds ratio associated with a 1-year change in age.
cOdds ratio associated with a 1-point change in A Severity Characterization of Trauma Anatomic Profile.
dAP-B is Winsorized at 4, meaning that values greater than 4 were reset to 4.
eAP-C is dichotomized as greater than 3 and less than or equal to 3.
fOdds ratio associated with a 1-point change in the Glasgow Coma Scale score.
gOdds ratio associated with a $1000 change in median household income.
hOdds ratio associated with a 1% increase in percentage of households below the poverty line.
Table 3 ▶ demonstrates the mean predicted mortality (i.e., severity of injury) and observed vs predicted mortality rates, stratified by median household income, proportion of households below the poverty level, and insurance status. Overall, there were no statistically significant differences in the mean severity of injury across SES strata when we used all of our measures, although there was a trend toward a higher mean predicted mortality among children from communities with higher median household income. There were also no statistically significant z scores for observed vs predicted mortality rates; however, there were trends toward lower survival among children from communities with a median household income of $15 000 or less per year (z = 1.63; SMR = 1.27 [95% CI = 0.69, 2.14]) and children with Medicaid (z = 1.49; SMR = 1.14 [95% CI = 0.86, 1.47]).
TABLE 3—
Effect of Socioeconomic Status on Observed and Predicted Mortality Rates for Pediatric Trauma Patients in Sacramento County, 1988–1998
| Survivors | Deaths | |||||||
| N | Mean Predicted Mortality | Observed | Predicted | Observed | Predicted | Standardized Mortality Ratioa (95% Confidence Interval) | Z Score | |
| Overall | 3855 | 3.39 | 3724 | 3724 | 131 | 131 | 1.00 | 0 |
| Median household income ($) | ||||||||
| 0–15 000 | 398 | 2.79 | 384 | 387 | 14 | 11 | 1.27 (0.69, 2.14) | 1.63 |
| 15 001–25 000 | 1009 | 3.65 | 969 | 972 | 40 | 37 | 1.08 (0.77, 1.47) | 0.56 |
| 25 001–35 000 | 1099 | 3.11 | 1069 | 1064 | 30 | 35 | 0.86 (0.58, 1.22) | −1.33 |
| 35 001–45 000 | 867 | 3.35 | 841 | 838 | 26 | 29 | 0.89 (0.59, 1.31) | −0.93 |
| > 45 000 | 482 | 4.09 | 461 | 462 | 21 | 20 | 1.05 (0.65, 1.60) | 0.37 |
| Below poverty line (%) | ||||||||
| < 1 | 359 | 3.06 | 348 | 347 | 11 | 12 | 0.92 (0.46, 1.64) | −0.43 |
| 1–20 | 1557 | 3.79 | 1498 | 1496 | 58 | 61 | 0.95 (0.72, 1.23) | −0.66 |
| 21–50 | 1296 | 2.93 | 1258 | 1258 | 38 | 38 | 1.1 (0.70, 1.37) | 0 |
| > 50 | 643 | 3.58 | 620 | 623 | 23 | 20 | 1.15 (0.73, 1.73) | 1.19 |
| Insurance | ||||||||
| Other | 2256 | 3.50 | 2183 | 2177 | 73 | 79 | 0.92 (0.72, 1.12) | −1.26 |
| Medicaid | 1599 | 3.25 | 1541 | 1547 | 58 | 51 | 1.14 (0.86, 1.47) | 1.49 |
aStandardized mortality ratio equals observed number of deaths divided by predicted number of deaths.
DISCUSSION
This population-based analysis supports previous research correlating high pediatric trauma admission and mortality rates with markers of poverty. Our data demonstrate that in Sacramento County, the higher trauma mortality rate among children from lower-SES communities is not due to higher mean injury severity among hospitalized patients. Instead, the higher injury mortality rate among children living in census blocks with low median household income and higher proportions of households below the poverty line reflects a higher overall incidence of trauma requiring hospitalization. And although the mean severity of trauma did not significantly differ among children from communities of differing SES, children from lower-SES communities did have a higher incidence of more lethal mechanisms of injury, such as pedestrian trauma and firearm injuries.
In the logistic regression analysis, the 3 measures of SES were not significantly associated with survival after adjustment for severity of illness, although there was a trend for patients with Medicaid to have lower-than-predicted survival (OR = 0.56; 95% CI = 0.31, 1.03). Also, in our analyses of observed vs predicted mortality (z scores), there were nonstatistically significant trends toward higher standardized mortality rate ratios among children from census blocks where the median household income was less than $15 000 per year and among children with Medicaid. These findings are consistent with previously published data on overall childhood mortality, which documented higher mortality rates with lower median household income22,23 and Medicaid receipt.24
Although socioeconomic disparities in mortality from trauma have been recognized for years, a study by Roberts has shown that these disparities continue to increase despite an overall declining trauma mortality rate.25 In our study, we attempted to better define the factors contributing to this disturbing phenomenon. High trauma mortality rates among children of lower SES may be attributable to several factors, including a higher overall incidence of injury, a higher average severity of injury, and higher severityadjusted mortality. Whereas previous investigations have demonstrated high mortality rates among children living in poverty,10,26–28 this is the first study, to our knowledge, that has systematically analyzed the relative contributions of these factors to the observed differences in mortality rates. The validity of this study is strengthened by its population-based design, its use of a customized physiology-based severity-of-illness measure, and its use of US Census data at the block level as a measure of community SES.
Two previous studies have investigated the association between injury severity and surrogates of SES.2,27 Haas and Goldman found that adult trauma patients without health insurance were more likely to die in a hospital than were patients with insurance, after adjustment for injury severity. Average injury severity was found not to be different between the 2 groups when we used the ISS. Hartzog and colleagues found that children in “poor social situations” were more likely to suffer trauma that was more severe (reflected as a higher median ISS) than were children in better social situations. Unlike our results, these authors’ findings indicated the higher mortality rates among poor children to be attributable to a higher average severity of trauma. To adjust for severity of illness, both of these studies used the ISS, based on ICDM-9-CM codes. The ISS has been shown to lack validity compared with other measures of trauma severity that incorporate physiological variables such as GCS, blood pressure, and respiratory rate.18,29,30
Hospital factors, such as rationing or quality of care, might also contribute to higher injury mortality rates among poor children. For example, children from a lower-SES community may be less likely to receive extraordinary therapies or may be more likely to receive limitations of care or a do-notresuscitate order than children from a higher-SES community. Haas and Goldman found that adult hospitalized patients were less likely to undergo operative procedures following trauma if uninsured or insured with Medicaid.2 Similarly, differences in the medical management of trauma patients may be related to the race and ethnicity of the patient. Although the conflation of SES and race/ethnicity is well documented, we chose not to include race and ethnicity in our analyses, because they are fundamentally a social construct, and not a genetic or physiological risk factor for injury incidence and mortality. We are still unsure of the relative contribution that differences in processes of care make to the differences in mortality rates among lower-SES patients (those who lack insurance, who are racial/ethnic minorities, or who reside in lowincome communities).
This study has several potential limitations. The relationship between SES and hospitalization for mild trauma, such as lacerations and minor fractures, is subject to selection bias, because patients from different socioeconomic strata utilize EDs and urgent care clinics differently. It is possible that some patients with mild trauma were not included in the trauma registry, either because the emergency medical services/trauma system was not utilized or because the attending ED physician did not consult the trauma surgeons. It was our intention, however, to focus on moderate to severe trauma. All children with more than a trivial risk of dying were likely to have been included in the trauma registry.
We were unable to adjust for other important predictors of patient outcomes, such as the time from injury to arrival at the ED. If these predictors differed systematically across socioeconomic strata, we might have underestimated or overestimated differences in predicted mortality (and SMRs) across strata.
Finally, the results of our analyses may not be representative of other counties or trauma care systems. Because we analyzed trauma data from all of Sacramento County, a relatively diverse mix of injuries and patient SES were included. The validity of our conclusions may be limited in trauma centers that treat a primarily urban or suburban population with a less diverse case mix, or in centers where processes of care may differ according to patients’ SES or insurance status.
Our results suggest that socioeconomic disparities in the incidence of the most serious types of injury, such as firearm injuries, assaults, and pedestrian injuries, explain most of the observed disparities in overall injury mortality. There is no evidence that the average severity of injury, among all hospitalized injuries, is inversely associated with SES. Children with Medicaid may be slightly more likely than children with other insurance to die after hospitalization for trauma, but this difference probably results more from patient-level confounders that were omitted (e.g., nutritional status, comorbidities) than from SES differences.
To reduce socioeconomic disparities in pediatric injury mortality, public health interventions should focus more on reducing disparities in the incidence of the most serious types of injuries (i.e., pedestrian, firearm, other assaultive injuries) than on reducing disparities in hospitalization or treatment practices. Future studies should corroborate these findings with population-based data from other settings that include physiological measures of injury severity and patient-level socioeconomic measures.
Acknowledgments
This study was supported, in part, by a grant from the Children’s Miracle Network, Children’s Hospital, University of California, Davis.
Human Participant Protection
The University of California, Davis, human subjects review committee approved this study.
J. P. Marcin planned the study, assisted in data analyses, and wrote the article. Both M. S. Schembri and J. He performed the data analysis and contributed to the writing of the article. P. S. Romano supervised and assisted with study design, data analyses, and writing of the article.
Peer Reviewed
References
- 1.Baker SP. The Injury Fact Book. 2nd ed. New York, NY: Oxford University Press; 1992.
- 2.Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: differences in care and mortality, by insurance status. Am J Public Health. 1994;84:1605–1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Onwuachi-Saunders C, Hawkins DF. Black-white differences in injury. Race or social class? Ann Epidemiol. 1993;3:150–153. [DOI] [PubMed] [Google Scholar]
- 4.Carey V, Vimpani G, Taylor R. Childhood injury mortality in New South Wales: geographical and socio-economic variations. J Paediatr Child Health. 1993;29(2):136–140. [DOI] [PubMed] [Google Scholar]
- 5.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and injury mortality: individual and neighbourhood determinants. J Epidemiol Community Health. 2000;54:517–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faelker T, Pickett W, Brison RJ. Socioeconomic differences in childhood injury: a population based epidemiologic study in Ontario, Canada. Inj Prev. 2000;6(3):203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laing GJ, Logan S. Patterns of unintentional injury in childhood and their relation to socio-economic factors. Public Health. 1999;113(6):291–294. [DOI] [PubMed] [Google Scholar]
- 8.Wicklund K, Moss S, Frost F. Effects of maternal education, age, and parity on fatal infant accidents. Am J Public Health. 1984;74:1150–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scholer SJ, Mitchel EF Jr, Ray WA. Predictors of injury mortality in early childhood. Pediatrics. 1997;100(3 pt 1):342–347. [DOI] [PubMed] [Google Scholar]
- 10.Langley J, Silva P, Williams S. Socio-economic status and childhood injuries. Aust Paediatr J. 1983;19:237–240. [DOI] [PubMed] [Google Scholar]
- 11.Anderson R, Dearwater SR, Olsen T, Aaron DJ, Kriska AM, LaPorte RE. The role of socioeconomic status and injury morbidity risk in adolescents. Arch Pediatr Adolesc Med. 1994;148:245–249. [DOI] [PubMed] [Google Scholar]
- 12.International Classification of Diseases, Ninth Revision, Clinical Modification. Hyattsville, Md: National Center for Health Statistics; 1980. DHHS publication PHS 80-1260.
- 13.Centers for Disease Control and Prevention. Recommended framework for presenting injury mortality data. MMWR Morb Mortal Wkly Rep. 1997;46(RR-14):1–30. [PubMed] [Google Scholar]
- 14.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. [DOI] [PubMed] [Google Scholar]
- 16.Baker SP, O’Neill B. The injury severity score: an update. J Trauma. 1976;16:882–885. [DOI] [PubMed] [Google Scholar]
- 17.Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- 18.Champion HR, Copes WS, Sacco WJ, et al. Improved predictions from a severity characterization of trauma (ASCOT) over Trauma and Injury Severity Score (TRISS): results of an independent evaluation. J Trauma. 1996;40:42–48; discussion 48–49. [DOI] [PubMed] [Google Scholar]
- 19.Champion HR, Copes WS, Sacco WJ, et al. A new characterization of injury severity. J Trauma. 1990;30:539–545; discussion 545–536. [DOI] [PubMed] [Google Scholar]
- 20.Ruppert D. Trimming and Winsorization. In: Kotz S, Johnson NL, Read CB, eds. Encyclopedia of Statistical Sciences. Vol. 9. New York, NY: John Wiley & Sons; 1988:348–353.
- 21.Fleiss JL. Statistical Methods for Rates and Proportions. 2nd ed. New York, NY: John Wiley & Sons; 1981.
- 22.Wise PH, Kotelchuck M, Wilson ML, Mills M. Racial and socioeconomic disparities in childhood mortality in Boston. N Engl J Med. 1985;313:360–366. [DOI] [PubMed] [Google Scholar]
- 23.Mare RD. Socioeconomic effects on child mortality in the United States. Am J Public Health. 1982;72:539–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nersesian WS, Petit MR, Shaper R, Lemieux D, Naor E. Childhood death and poverty: a study of all childhood deaths in Maine, 1976 to 1980. Pediatrics. 1985;75:41–50. [PubMed] [Google Scholar]
- 25.Roberts I, Power C. Does the decline in child injury mortality vary by social class? A comparison of class specific mortality in 1981 and 1991. BMJ. 1996;313(7060):784–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jolly DL, Moller JN, Volkmer RE. The socioeconomic context of child injury in Australia. J Paediatr Child Health. 1993;29:438–444. [DOI] [PubMed] [Google Scholar]
- 27.Hartzog TH, Timerding BL, Alson RL. Pediatric trauma: enabling factors, social situations, and outcome. Acad Emerg Med. 1996;3:213–220. [DOI] [PubMed] [Google Scholar]
- 28.Durkin MS, Davidson LL, Kuhn L, O’Connor P, Barlow B. Low-income neighborhoods and the risk of severe pediatric injury: a small-area analysis in northern Manhattan. Am J Public Health. 1994;84:587–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hannan EL, Mendeloff J, Farrell LS, Cayten CG, Murphy JG. Validation of TRISS and ASCOT using a non-MTOS trauma registry. J Trauma. 1995;38(1):83–88. [DOI] [PubMed] [Google Scholar]
- 30.Baxt WG, Upenieks V. The lack of full correlation between the Injury Severity Score and the resource needs of injured patients. Ann Emerg Med. 1990;19:1396–1400. [DOI] [PubMed] [Google Scholar]