Go to the people. Live among them. Learn from them. Love them. Serve them. Plan with them. Start with what they know. Build on what they have.
This poem by Dr Y. C. Yen, friend of Larimer Mellon, captures the philosophy that guided Dr Mellon’s work in Haiti—“It was what he preached and practiced.”1(p205)
If you stand in the lakou (courtyard) just inside the Hospital Albert Schweitzer (HAS) in Deschapelles, Haiti, you will see a gnarled tree standing guard like an imperious matron. Its leafy headdress is filled with blazingly red-and-gold nesting birds, warbling and “gossiping like women in the market place.”2(p170) No one would guess that this tree, and others like it planted around the hospital, started life as a stick without roots or leaves. In a country where the daily desperate search for firewood has denuded the mountains and the earth in many areas offers as little sustenance as a dried-up breast, the survival of robust trees like this one is noteworthy. Likewise, in the starkly beautiful Artibonite Valley, filled with 300 000 people living in unfathomable poverty and previously without any form of modern health care, the birth, survival, and evolution of HAS has grown into one of the most important stories in international health.
REVERENCE FOR LIFE
Albert Schweitzer (1875–1965) was a philosopher, theologian, and accomplished organist who, at 38 years of age, became a physician. With his wife, a nurse, he established a mission hospital in 1913 in equatorial Lambaréné, Gabon (Africa), and later established a colony to care for individuals with leprosy. Leprosy is a disease that has been associated with fear and stigma since antiquity, a disease that disfigures the face, eyes, skin, and extremities and that, untreated, can be lethal. Schweitzer described his personal philosophy of reverence for life, in which he argued that the ethical man assists all life that he is able to help and refrains from injuring any living thing.3 He received the Nobel Peace Prize in 1952.
In 1947, Larimer Mellon was strongly influenced by Schweitzer’s philosophy and accomplishments and, at 37 years of age, he decided to leave his ranch in Arizona, go to medical school, and devote his life to the establishment of what would become the first modern hospital in Haiti. In 1956, Dr Mellon and his wife, Gwen, a medical technician, opened the newly built HAS in Deschapelles, an isolated rice-producing region 120 km northwest of Port-au-Prince. What was originally envisioned as a “simple rural hospital” took root. With ample funding and highly qualified medical and surgical specialists from the United States and Europe to staff it, the hospital quickly began to attract patients, and professionals who wanted training, from throughout Haiti. The program blossomed and quickly sent out new shoots.
In the early 1960s, in recognition that many of the valley’s public health and societal needs could not be met through hospital-based care, Dr Mellon “hung up his stethoscope and took up a transit [engineering tool for surveying],”1(p196) transferred leadership of the hospital to Gwen, and created a community development program. The program improved community water supplies, introduced better farming techniques, introduced reforestation, assisted with animal husbandry, developed microenterprises to generate income, and helped village groups grow in strength, capabilities, and financial independence.
A community health program was created in 1967, under the direction of Drs Warren and Gretchen Berggren of the Harvard University School of Public Health. Their program became one of the first in a developing country to document clear-cut beneficial effects on infant and child mortality.4 It has since been widely replicated throughout Haiti and used as a model for other developing countries. Initially, emphasis was placed on hospital-based immunization and nutritional programs, in tandem with a household census for the entire population served by the program. Within a decade, however, a continuum of health care reaching throughout the community was created, starting with a home visiting program staffed by health agents (Agentes de Sante); neighborhood-based “rally post sessions” in which health staff provided immunizations, primary health care, and education at gatherings of the community; and a network of dispensaries, health centers, and mobile clinics (for isolated communities), which provided adult care, prenatal care, pediatric care, and family planning.
The community health program now works closely with nearly 300 village midwives (matrones); with community health workers (monitrices) to educate mothers of malnourished children in nutritional techniques and provide breastfeeding education and counseling; with community workers (enqueteurs) to collect census data, register families, and make community maps for a computerized community-based information system; and with 1800 men and women volunteers (animatrices) who receive regular training to detect signs of deteriorating health and provide first aid. Over time, HAS has developed responsibility for the primary health care needs of most of the residents of the Artibonite Valley.
Today, HAS has 122 beds (62 pediatric, 32 surgical, 23 medical, and 5 high-risk maternity). In 2001, there were 10 805 hospital admissions, 51 012 clinic visits, and 2897 surgical procedures at the hospital. The community health program made 95 750 home visits and provided 53 497 adult consultations, 60 293 pediatric consultations, 9237 prenatal visits, and 26 725 family planning visits.5
The combined effects of HAS’s hospital, community health, and community development programs over more than 40 years have resulted in a persistent marked reduction in infant and child mortality in the Artibonite Valley compared with the rest of Haiti.6 The results are a convincing and eloquent validation of the founders’ vision and painstaking investment in a long-term response to the needs of the Artibonite Valley.
CONGENITAL SYPHILIS IN THE ARTIBONITE REGION
Today, the major causes of readily preventable or treatable causes of serious illness and death in the Artibonite Valley are childhood malnutrition, tuberculosis (500 cases per 100 000 population), and HIV infection (3% to 5% of the childbearing women) and other sexually transmitted diseases,7 including congenital syphilis.
In this issue of the Journal, Fitzgerald and colleagues from HAS describe a 75% decrease in the incidence of congenital syphilis over a 3-year period (1997–1999) in response to the decentralization of prenatal syphilis screening at 14 community dispensaries.8 By installing a laboratory in each health dispensary to allow same-day, on-site syphilis testing, HAS reduced the number of pregnant women with positive syphilis tests who went untreated from 41% in 1995, the year before decentralization, to 0% in 2000. At the same time, rates of congenital syphilis fell from 550 cases per 100 000 live births to 137 cases per 100 000. Seroprevalence studies in 1996 and 2000 showed that the rate of syphilis seroreactivity in pregnant women in the area remained constant at 6%, and there is no evidence that access to care changed substantially during this period.
The authors’ conclusion that the decentralization of prenatal syphilis screening resulted in a decreased incidence of congenital syphilis is convincing, and their findings, together with complementary observations made by others,9,10 make a persuasive argument for same-day testing and treatment programs even in rural areas with little infrastructure. As the authors conclude, despite the remarkable progress made by this program, the rate of congenital syphilis remains unacceptably high; further improvement most likely would result from earlier and more frequent prenatal care visits for more women. Similar programs have been shown to increase the acceptance of voluntary HIV testing and counseling11,12 and are a reminder of the central importance of efficient systems of care, particularly when dealing with diseases that may be accompanied by fear, guilt, denial, stigma, or secrecy.
INTERNATIONAL HEALTH IN THE ERA OF AIDS: A NEW EQUATION?
The global HIV/AIDS pandemic provides a compelling rationale to help resource-poor regions of the world, notably sub-Saharan Africa, the Caribbean, Eastern Europe, and Asia, with unacceptably high prevalence and incidence rates of HIV. I have cared for children with HIV/AIDS in Harlem, New York City, since the early 1980s, but remarkably, the pediatric AIDS epidemic is disappearing throughout the United States and other resource-rich countries.13 As a result of this progress—and propelled by a growing belief that it is imperative that we share our health personnel and expertise, along with essential pharmaceuticals and material goods, with resource-poor countries—I have become involved with HAS to develop a program to prevent mother-to-infant transmission of HIV infection and to treat infected individuals. There is good reason to believe that the same strong health care infrastructure that has improved the survival and well-being of children and that allowed Fitzgerald and colleagues to reduce cases of congenital syphilis will also provide the framework for effective family AIDS prevention and treatment programs.
The lack of exposure to international health issues within my own medical training created obstacles to my providing quality health care for newly arrived immigrant children and their families when I first arrived in New York City decades ago. A rotation in international pediatrics during pediatric residency training would be an important step toward improving the quality of community pediatrics in the United States.
The central philosophy of Albert Schweitzer, as envisioned and implemented by Larimer and Gwen Mellon, is alive and well in Haiti. But it would be an important, long overdue, and beneficial evolutionary step in our own health care system if we were able to incorporate a world view into our everyday practices.
Figure .
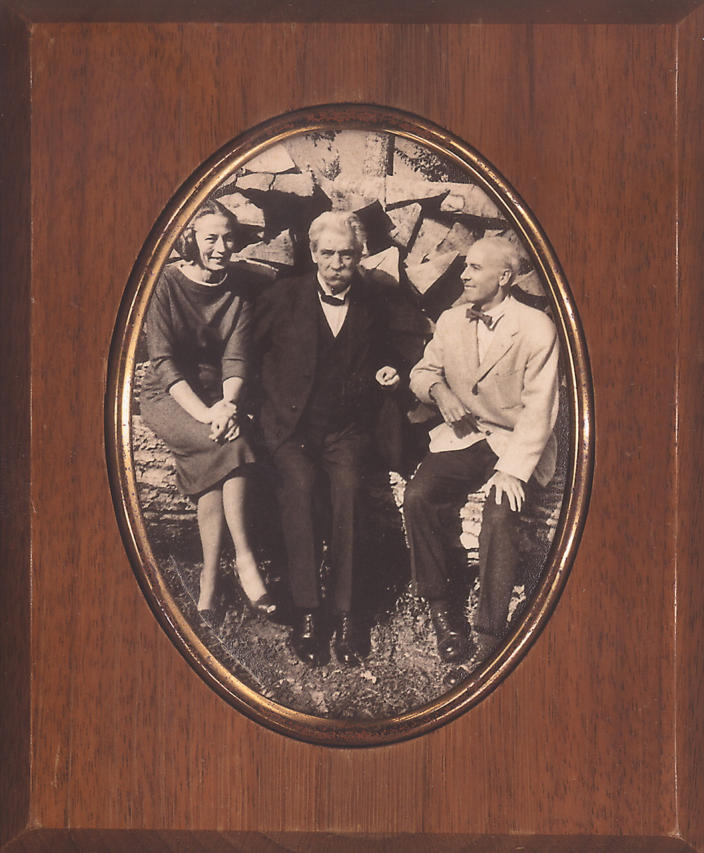
Dr Albert Schweitzer with Gwen and Larimer Mellon in Gunsbach, Germany in the summer of 1950.
References
- 1.Paris B. Song of Haiti: The Lives of Dr. Larimer and Gwen Mellon at the Albert Schweitzer Hospital of Deschapelles. New York, NY: Public Affairs; 2000.
- 2.Mellon GG. My Road to Deschapelles. New York, NY: Continuum; 1998.
- 3.Albert Schweitzer. The Philosophy of Civilization. CT Campion, trans. New York, New York: The MacMillan Company; 1949.
- 4.Berggren WL, Ewbank DC, Berggren GG. Reduction of mortality in rural Haiti through a primary health-care program. N Engl J Med. 1981;304:1324–330. [DOI] [PubMed] [Google Scholar]
- 5.Poised for the Future: Annual Report 2001 Hospital Albert Schweitzer. Sarasota, Fla: Grant Foundation; 2001.
- 6.Perry H, Volk D, Philippe F, Dortonne JR, Berggren G, Berggren W. The long-term impact of a community-based health care program on infant and child mortality: the experience of the Hospital Albert Schweitzer in Haiti. Paper presented at: Annual Meeting of the American Public Health Association;24October2001; Atlanta, Ga.
- 7.Perry H. Description of Haiti, its health, health services, and healthrelated behaviors. Background document to the assessment of HAS programs. Sarasota, Fla: Grant Foundation; 2000.
- 8.Fitzgerald DW, Behets F, Preval J, Schulwolf L, Bommi V, Chaillet P. Decreased congenital syphilis incidence in Haiti’s rural Artibonite region following decentralized prenatal screening. Am J Public Health. 2003;93:444–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel A, Moodley D, Moodley J. An evaluation of on-site testing for syphilis. Trop Doct. 2001;31:79–82. [DOI] [PubMed] [Google Scholar]
- 10.Warner L, Rochat RW, Fichtner RR, Stoll BJ, Nathan L, Toomey KE. Missed opportunities for congenital syphilis prevention in an urban southeastern hospital. Sex Transm Dis. 2001;28:92–98. [DOI] [PubMed] [Google Scholar]
- 11.Downing RG, Otten RA, Marum E, et al. Optimizing the delivery of HIV counseling and testing services: the Uganda experience using rapid HIV antibody test algorithms. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18:384–388. [DOI] [PubMed] [Google Scholar]
- 12.Kassler WJ, Alwano-Edyegu MG, Marum E, Biryahwaho B, Kataaha P, Dillon B. Rapid HIV testing with same-day results: a field trial in Uganda. Int J STD AIDS. 1998;9:134–138. [DOI] [PubMed] [Google Scholar]
- 13.Nicholas SW, Abrams EJ. Boarder babies with AIDS in Harlem: lessons in applied public health. Am J Public Health. 2002;92:163–165. [DOI] [PMC free article] [PubMed] [Google Scholar]


