Abstract
We report on the creation of an integrative medicine clinic within the setting of a medical research and tertiary care hospital.
The clinical audit used a prospective case series of 160 new patients who were followed by telephone interviews over a 6-month period. Patients’ demographic characteristics, presenting symptoms and diagnoses, physician treatment recommendations, extent of understanding and adherence to treatment recommendations, changes in symptom intensity, and progress toward achieving health objectives were recorded. Patients at the clinic showed significant reductions in the severity of symptoms and made significant progress toward achieving their health objectives at the 6-month follow-up.
Thus far, the clinic’s experience suggests that an integrative medicine clinic can face current health care financial challenges and thrive in a conventional medical center.
COMPLEMENTARY AND alternative medicine (CAM) represents a subset of health care practices, one often used by patients but not integral to conventional allopathic medicine.1 CAM therapies encompass a number of diverse health care and medical practices, ranging from dietary and behavioral interventions, vitamins, supplements, and herbs to ancient systems of medicine, such as ayurvedic medicine and traditional Chinese medicine. Integrative medicine describes a clinical philosophy in which the most appropriate CAM, conventional medical treatments, or both are employed to address patients and their diseases from the most holistic, mind–body–spirit perspective possible.
In response to patient demand for integrative medical care at California Pacific Medical Center (CPMC), a 1200-bed, not-for-profit community hospital in San Francisco, the Institute for Health and Healing at CPMC began planning for a Health and Healing Clinic in 1996; the clinic opened in 1998.2,3 Financial startup for the clinic came from a grant from an Institute for Health and Healing patient/ donor, who shared the vision of a multidisciplinary clinic for holistic collaboration between physicians and CAM therapists, and a matching grant from the CPMC Foundation.
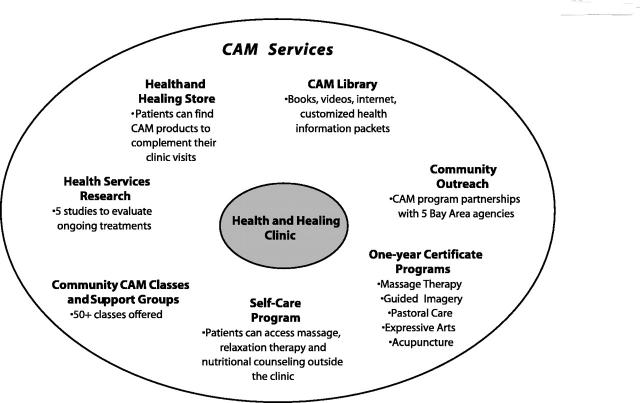
Founding an integrative medicine clinic in a conventional hospital required considerable support by CPMC and careful planning by the Institute for Health and Healing. A task force was formed that included CPMC’s administrative leadership, medical staff, and foundation. An Institute for Health and Healing steering committee worked to define the treatment philosophy; create a calm, supportive, healing environment; recruit personnel; establish policies such as practitioner credentialing, quality, and performance improvement standards; and establish a budget and marketing plan. All physicians at the clinic are board certified and licensed by the state. All CAM practitioners and pastoral care workers are either certified (e.g., massage therapists and nutritionists) or state licensed (e.g., acupuncturists/Chinese medicine practitioners, chaplains, and psychotherapists). The clinic is part of a network of related services, which include a store, library, self-care program, and training program in CAM therapies (Figure 1 ▶).
FIGURE 1—
Complementary and alternative medicine (CAM) services available through the Institute for Health and Healing.
Note. California Pacific Medical Center’s Institute for Health and Healing is a department within a 3-campus community hospital, which is within the 29-hospital Sutter System.
CLINIC FUNDAMENTALS
The clinic’s philosophy is to consider the health of each patient in the broadest, most holistic sense possible. The intention is to address not only the patients’ presenting symptoms but also the underlying causes of the disease, whether it resides at the mental, physical, or spiritual level or a combination of these. The goal of the therapy is to apply relationship-centered care to assist patients in achieving optimal health at all levels. Practitioners at the clinic (box 1), and the Institute for Health and Healing in general, remain committed to this integrated, holistic approach and together offer patients a broad range of CAM therapies and services (box 2).
BOX 1—CLINIC PRACTITIONERS.
4 board-certified physicians
Traditional Chinese medicine practitioner/acupuncturist
Massage, body work, and craniosacral massage therapists
Guided imagery practitioners
Hospital chaplains
Nutritionista
Psychotherapista
Feldenkreis practitioner a
aAdded to the clinic in 2001, after the Clinic Audit Study.
BOX 2—CAM THERAPIES AVAILABLE AT THE CLINIC.
Nutritional and dietary counseling
Dietary supplements and vitamins
Western and Eastern herbs
Acupuncture
Mindfulness meditation training
Interactive guided imagery
Reiki—a Japanese/Tibetan Buddhist-based form of hands-on energy work
A variety of massage therapies
Spiritual care and counseling
Psychotherapy a
Feldenkreis—individual and group sessionsa
aAdded to the clinic in 2001, after the Clinic Audit Study.
The clinic is an integrative medicine specialty referral clinic. It is intended to complement, rather than replace, other medical services, and all patients must retain a primary care physician not associated with the clinic. The clinic uses a fee-for-service payment model, although patients may submit billing forms to their own third-party insurers for reimbursement.
PATIENT CARE
Before the initial visit, patients complete a comprehensive intake questionnaire. The initial intake visit lasts 1.5 hours, during which patients and practitioners explore the fundamental causes of their symptoms and underlying conditions as well as potential treatments. The goal of this comprehensive assessment is to develop an individualized, integrated treatment plan for each patient.
From 1998 to 2002, only physicians conducted these initial visits. In 2002, this physician-based model was changed to allow all clinic practitioners to conduct initial evaluations and initiate treatment plans. Follow-up medical appointments usually last 30 minutes, with 1-hour appointments for guided imagery and spiritual and psychotherapeutic counseling. The entire clinic staff meets once a week for 2 hours to discuss issues related to administration and patient care, including interpractitioner communication, education, and multidisciplinary case conferences.
CLINICAL AUDIT
In order to characterize the patient population and their presenting health conditions, symptoms, and objectives, we carried out a prospective case-series study of all consenting new clinic patients from February 2000 to February 2001. We extracted baseline and follow-up data from patients’ medical charts and via telephone interviews conducted 1, 3, and 6 months after the initial visit. We sought to ascertain (1) who came to the clinic, (2) the types of therapies recommended by clinic physicians, (3) recall and adherence to treatment recommendations, and (4) changes in health outcomes, including symptom severity, functionality, days missed from work or school, and achievement of stated health objectives.
RESULTS
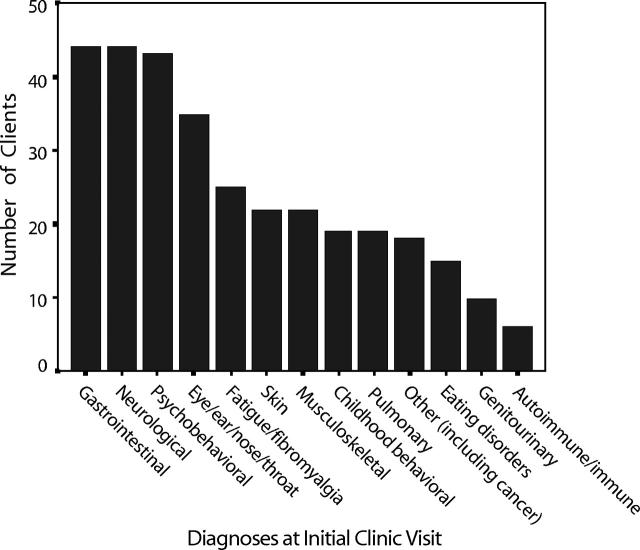
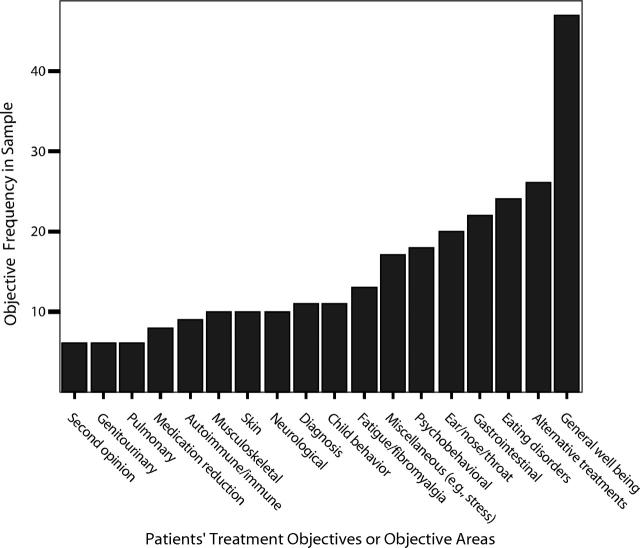
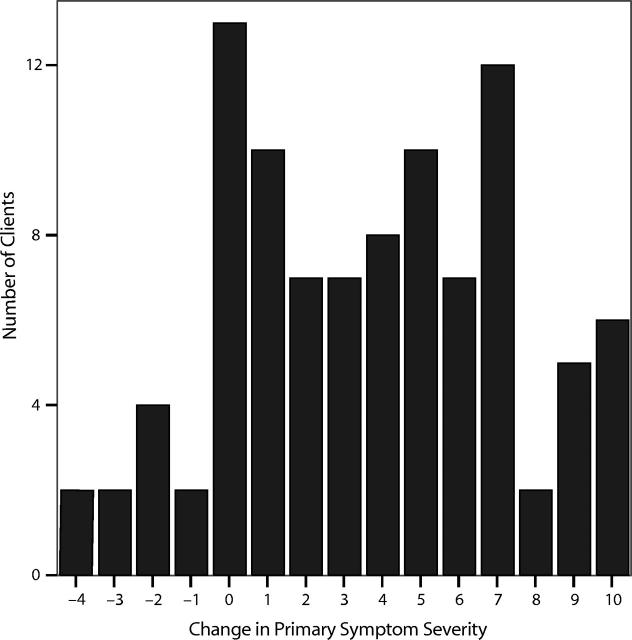
We recruited 160 patients to participate in the study, with 109 patients completing follow-up at 6 months. There were no significant baseline differences in age, sex, education, or initial symptom intensity between those who completed and those did not complete the 6-month interview (χ2 or t test). Patients were referred to the clinic by their physician (24%), family or friend (15%), media or advertising (12%), CPMC employee (12%), other conventional health provider (11%), alternative health care provider (5%), another patient of the clinic (4%), or some other source (17%). The clinic’s population was predominantly college educated, affluent, and White; 68% of patients were female. Patients presented with multiple and varied diagnoses (Figure 2 ▶) and health objectives (Figure 3 ▶) and with symptoms of moderately severe intensity (an average of 7.8 on a 10-point scale; see Figure 4 ▶). Thirty-five percent of the patients visited the clinic only once, 21% visited twice, 11% visited 3 times, and 33% had 4 or more visits in the year following their initial visit.
FIGURE 2—
Diagnoses of patients at initial visit to the Health and Healing Clinic (by organ system).
FIGURE 3—
Patients’ reasons for coming to the Health and Healing Clinic.
FIGURE 4—
Change in the severity of patients’ primary symptoms from their initial visit to the Health and Healing Clinic to 6-month follow-up.
Note. Changes are based on a scale of –10 to +10, with positive scores indicating improvement, negative scores worsening, and zero no change in symptoms.
Self-reported symptom intensity significantly decreased from 7.6 at the initial visit to 4.1 after 6 months (46%) (t 96 = 9.8, P < .001; 2-tailed test). Symptom intensity increased in 11% of the patients and remained unchanged in 13% (the modal response). At 6 months, the patients’ average rating of “achieving their treatment objective” was 5.4 points, with –10 representing getting much worse and 10 representing complete achievement. The modal response was “no change,” representing 22% of patients.
Physicians made an average of 9.4 treatment recommendations per patient—50% were for substances to take, such as dietary supplements, vitamins, herbs, homeopathic remedies, or a combination of these; 16% were for self-care, such as exercise or meditation; 13% were referrals to other therapists; 12% were dietary; and 9% were for further diagnostic testing. After 1 month, patients recalled 56% of all treatment recommendations correctly without prompting and 20% after receiving a general prompt (i.e., they were asked if they had been given “something to take”). Patients adhered very well ( ≥ 90% of the time) to 48% of the recommendations, but they did not adhere at all (≤ 10% of the time) to 42% of the recommendations.
KEY FINDINGS.
A CAM integrative clinic can exist in a major medical center. It is a partnership that can work despite the financial challenges in medical care.
Clients report substantial improvement in their symptom intensity and progress in achieving their health objectives, although, without a controlled study, this cannot be attributed to the care they received.
The clinic is seeking ways to better support each client’s ongoing change process to reinforce progress and healing.
DISCUSSION
Most patients at the clinic presented complex medical problems, often involving multiple organ systems and associated with moderate to severe symptom intensity that had not been resolved with conventional medical treatment. Patients reported substantial improvement in their symptoms and achievement of their health objectives at 6-month follow-up. Since this was not a controlled study, it was not possible to determine which, if any, aspects of care at the clinic may have contributed to this improvement.
Integrative medicine treatment plans typically contained multiple recommendations, incorporating a wide variety of lifestyle modifications and CAM therapies. Despite this complexity, patients recalled almost 76% of the treatment recommendations after 1 month, either without being prompted or with only a general prompt. Patients tended to follow the treatment recommendations either completely (48%) or not at all (42%). Complex cases often require long-term treatment with holistic and challenging healing at the mental, physical, or spiritual level. Given that patients visited the clinic relatively few times, it is difficult to determine whether further follow-up would increase adherence to treatment and lead to greater reductions in symptom intensity, the achievement of health objectives, or both. Cost, especially with the fee-for-service model used at the clinic, and ongoing patient education and support for major lifestyle changes remain significant barriers to long-term treatment. In response to these concerns, the clinic has available a donated patient assistance fund that allows sliding-scale fees based on financial need. In addition, in 2002, the clinic began offering group appointments, both general and disease specific (e.g., cardiovascular illness and physical rehabilitation), in which patients can work together in a facilitated and ongoing manner to support and sustain desired changes in their level of health.
Figure .
Above: The first labyrinth at a major medical center, established in 1997 by the Institute for Health and Healing (modeled after Grace Cathedral in San Francisco and Chartres Cathedral in Chartres, France).
Acknowledgments
Human Participant Protection
Before patient recruitment began, this study was approved by the California Pacific Medical Center’s institutional review board (February 2000).
L. Scherwitz designed the study (with M. Cantwell) and directed all aspects of the study, including data analysis, interpretation, and writing the report. W. Stewart provided access to the clinic, allocated resources for staff, and helped to write the report. P. McHenry worked on the administrative and research assistant aspects, including preparation of the protocol and consent forms, data entry, table preparation, training of the interviewers, and interviewing patients. C. Wood was involved in developing methods of procedure for data collection, editing, reducing the data for analysis, and some data analysis. L. Robertson conducted the literature review, edited the report, and prepared graphs and photographs. M. Cantwell provided medical insights, created the database, and edited the report.
Peer Reviewed
References
- 1.Lewith G, Jonas W, Walah H, eds. Clinical Research in Complementary Therapies: Principles, Problems and Solutions. London, England: Harcourt Publishers Ltd; 2002.
- 2.Stewart WB, Faass N. Hospital-based integrative medicine: The Institute for Health and Healing. In: Faass N, ed. Integrating Complementary Medicine Into Health Systems. Gaithersburg, Md: Aspen Publications; 2001:406–412.
- 3.Stewart WB. The Institute for Health and Healing: Contributing to the evolution of contemporary medicine. San Francisco Med. June/July 2000:18–20.