In response to growing complaints and safety concerns,1–4 most states and the federal government have now enacted legislation to guarantee a more reasonable postpartum length of stay.5 The Ohio law required health maintenance organizations, health insurers, public employers, and the state’s Medicaid program to provide a minimum of 48 hours of inpatient care following a normal vaginal delivery and a minimum of 96 hours of inpatient care following a cesarean delivery. This study examined, in a single region in southwestern Ohio, whether the state legislative mandate was applied in a manner that equally affected decisions made for Medicaid and commercially insured infants and their families.
METHODS
The study population consisted of 30 035 healthy, full-term, single-birth infants born in 1 of 10 hospitals in southwestern Ohio between April 1, 1996, and December 31, 1998, and discharged to home. Patients were stratified by insurance type; 25 747 had commercial insurance, and 4288 had Medicaid coverage. Self-pay patients were excluded.
Changes over time in the proportions of newborns with a “short-stay” delivery were examined for commercially insured infants and those with Medicaid coverage by reviewing a regional database of hospital discharge information. Short stay was defined as discharge within 1 day following a vaginal delivery or 2 days following a cesarean delivery.6
Three time periods were analyzed to examine the effect of the legislation: (1) the baseline period (April 1, 1996, to July 18, 1996) immediately before the law was signed by the governor, (2) the immediate postlegislative period (July 19, 1996, to October 17, 1997) between the signing of the law and 1 year after the law went into effect, and (3) the late postlegislative period (October 18, 1997, to December 31, 1998).
The association between length of stay and insurance status was tested with χ2 tests of proportions and multivariate logistic regression models.7 Each of the 3 periods was modeled separately. The dependent variable in these analyses was a binary variable indicating whether the patient had a short stay. To determine differences in time trend between discharge practices for Medicaid and those for commercial insurance, a variable for interaction between insurance status and the time variable was included in the logistic regression model. Odds ratios (ORs) and relative risks are reported. All statistical analyses were performed with PC-SAS software (Release 8.1; SAS Institute Inc, Cary, NC).
RESULTS
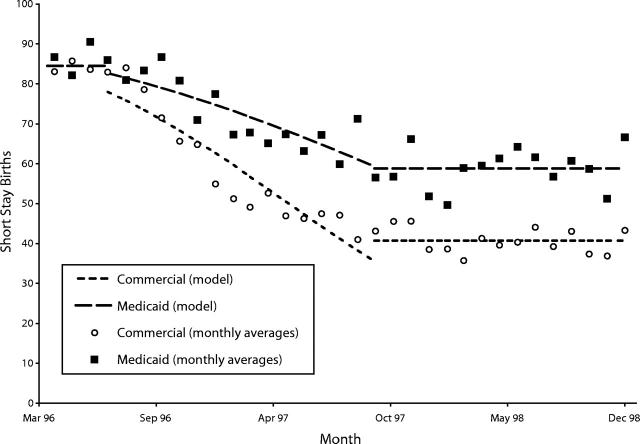
Figure 1 ▶ shows the changing trend in short stays for newborns over the course of the study. Before the law was signed by the governor, the probability of having a short stay (Table 1 ▶) was not significantly different for patients with Medicaid and patients with commercial insurance. In addition, the trends over time during this period were not statistically significant for either group.
FIGURE 1—
Trend in the proportion of patients discharged with a short stay (discharge within 1 day of a vaginal delivery or within 2 days of a cesarean delivery).
TABLE 1—
Results for the 3 Time Periods
| Baseline Period April 1, 1996–July 18, 1996 | Immediate Postlegislative Period July 19, 1996–October 17, 1997 | Late Postlegislative Period October 18, 1997–December 31, 1998 | ||||
| Medicaid | Commercial Insurance | Medicaid | Commercial Insurance | Medicaid | Commercial Insurance | |
| n | 409 | 2528 | 1860 | 11 562 | 2023 | 11 653 |
| Short stay, % | 87.0 | 84.1 | 71.3 | 57.0 | 58.8 | 40.7 |
| Relative risk (Medicaid/commercial) | 1.03 | 1.06 (beginning) | 1.44 | |||
| 1.67 (end) | ||||||
| Odds ratio (Medicaid/commercial) | 1.27 | 1.34 (beginning) | 2.07 | |||
| 2.65 (end) | ||||||
| 95% confidence limits | 0.93, 1.72 | 1.05, 1.72 (beginning) | 1.89, 2.28 | |||
| 2.16, 3.24 (end) | ||||||
| Change in the odds of a short stay during the period, % per month | +12.9 | −1.0 | −7.6 | −11.7 | +1.2 | −0.8 |
| 95% confidence limits | −17.6, 50.9 | −10.6, 9.6 | −9.9, –5.3 | −12.5, –10.9 | −0.9, 3.4 | −1.6, 0.1 |
Note. Commercial insurance included BlueCross BlueShield, commercial health maintenance organization nonsenior plans, and all other commercial insurance plans. Medicaid coverage included fee-for-service and health maintenance organization plans. April 1, 1996–July 18, 1996 = the baseline period immediately before the law was signed by the governor; July 19, 1996–October 17, 1997 = the immediate postlegislative period between the signing of the law and 1 year after the law went into effect; October 18, 1997–December 31, 1998 = the late postlegislative period.
During the immediate postlegislative period, the odds of a short stay decreased 85% (an average of 11.7% per month) for commercially insured newborns but only 70% (an average of 7.6% per month) for newborns with Medicaid. The odds ratio trend comparing Medicaid short stay with commercial short stay was statistically significant over the 15 months (OR = 1.974; confidence limits = 1.019, 1.074). The relative risk of having a short stay among Medicaid patients, relative to commercially insured patients, increased from 1.06 to 1.67 from the beginning to the end of this period.
The proportion of newborns discharged following a short stay stabilized during the late postlegislative period. The time trends during this period were not statistically significant for either group. However, the difference between the groups in the proportion of infants discharged following a short stay was significant. Thus, Medicaid patients during this period had a 44% greater probability of having a short stay as commercially insured patients.
DISCUSSION
The effect of the law guaranteeing a minimum newborn length of stay varied for commercially insured and Medicaid infants in this region of southwestern Ohio. In the immediate postlegislative period, newborns with Medicaid coverage were significantly more likely to be discharged early than were those with commercial insurance. As late as 2 years after the law went into effect, Medicaid patients still had twice the odds of being discharged early.
It is unclear whether the Medicaid mothers left early, unaware of the legislative mandate allowing them to remain longer, or whether the commercially insured mothers, being more educated, were better positioned to take advantage of the new legislation. Breastfeeding rates traditionally have been low in the Medicaid population,8–11 and physicians may have felt more comfortable with early discharge for mothers who did not intend to breastfeed. Also, the establishment of early discharge programs linked with aggressive home visit support for Medicaid patients in this region before passage of the state legislation12 may have prompted application of the law in a more tailored approach. Our study was limited to a single geographic region. Whether the outcomes reported are related to local environmental and practice factors or can be generalized to other states where similar legislation has been enacted remains to be seen.
Acknowledgments
Human Participant Protection
The institutional review board of Cincinnati Children’s Hospital Medical Center determined that informed consent was not required for this study.
U. R. Kotagal made substantial contributions to the study conception and design, the acquisition of the data, the analysis and interpretation of the data, the drafting of the brief, the critical revision of the brief, and supervision and provided statistical expertise. P. J. Schoettker made substantial contributions to the analysis and interpretation of the data, the drafting of the brief, the critical revision of the brief, and supervision. H. D. Atherton and R. W. Hornung made substantial contributions to the analysis and interpretation of the data and provided statistical expertise.
Peer Reviewed
References
- 1.Catz C, Hanson KW, Simpson L, Yaffe SJ. Summary of workshop: early discharge and neonatal hyperbilirubinemia. Pediatrics. 1995;96:743–745. [PubMed] [Google Scholar]
- 2.Maisels MJ, Newborn TB. Kernicterus in otherwise healthy breast-fed term newborns. Pediatrics. 1995;96:730–733. [PubMed] [Google Scholar]
- 3.Seidman DS, Stevenson DK, Ergaz Z, Gale R. Hospital readmission due to neonatal hyperbilirubinemia. Pediatrics. 1995;96:727–729. [PubMed] [Google Scholar]
- 4.Cooper WO, Atherton HD, Kahana M, Kotagal UR. Increased incidence of severe breastfeeding malnutrition and hypernatremia in a metropolitan area. Pediatrics. 1995;96:957–960. [PubMed] [Google Scholar]
- 5.Declercq E, Simmes D. The politics of “drive-through deliveries”: putting early postpartum discharge on the legislative agenda. Milbank Q. 1997;75:175–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kotagal UR, Atherton HD, Eshett R, Schoettker PJ, Perlstein PH. Safety of early discharge for Medicaid newborns. JAMA. 1999;282:1150–1156. [DOI] [PubMed] [Google Scholar]
- 7.Col NF, McLaughlin TJ, Soumerai SB, et al. The impact of clinical trials on the use of medications for acute myocardial infarction: results of a community-based study. Arch Intern Med. 1996;156:54–60. [PubMed] [Google Scholar]
- 8.Kramer MS. Poverty, WIC, and promotion of breast-feeding. Pediatrics. 1991;87:399–400. [PubMed] [Google Scholar]
- 9.Ryan AS, Rush D, Krieger FW, Lewandowski GE. Recent declines in breast-feeding in the United States, 1984 through 1989. Pediatrics. 1991;88:719–727. [PubMed] [Google Scholar]
- 10.Beck LF, Morrow B, Lipscomb LE, et al. Prevalence of selected maternal behaviors and experiences, Pregnancy Risk Assessment Monitoring System (PRAMS), 1999. MMWR Surveill Summ. 2002;51:1–27. [PubMed] [Google Scholar]
- 11.Colley Gilbert BJ, Johnson CH, Morrow B, Gaffield ME, Ahluwalia I. Prevalence of selected maternal and infant characteristics, Pregnancy Risk Assessment Monitoring System (PRAMS), 1997. MMWR CDC Surveill Summ. 1999;48:1–37. [PubMed] [Google Scholar]
- 12.Cooper WO, Kotagal UR, Atherton HD, et al. Use of health care services by inner-city infants in an early discharge program. Pediatrics. 1996;98:686–691. [PubMed] [Google Scholar]