Abstract
Objectives. We describe the intervention tested in EXPLORE, an HIV prevention trial aimed at men who have sex with men (MSM), and test the empirical basis of the individually tailored intervention.
Methods. Data on participants’ self-efficacy, communication skills, social norms, and enjoyment of unprotected anal intercourse were examined in relation to sexual risk. Combinations of these factors, together with alcohol use and noninjection drug use, were also examined.
Results. The individual factors examined were associated with sexual risk behavior. The cohort was shown to be heterogeneous in regard to the presence of combinations of these risk-related factors.
Conclusions. Baseline data from the EXPLORE study support the efficacy of the individually tailored intervention used.
Evidence indicates that HIV incidence rates are rising among men who have sex with men (MSM),1–3 that prevalence rates remain high in large urban areas,4–7 that sexually transmitted disease rates among MSM have risen,8–10 and that the prevalence of sexual risk behaviors, specifically unprotected anal intercourse, has increased.11 A recent meta-analysis of HIV interventions designed for MSM revealed that behavioral interventions tested to date have reduced the number of episodes of unprotected intercourse but that effects have waned over time and have not been consistent across studies.12 Among the factors contributing to the success of interventions are the use of interventions of longer duration and a focus on interpersonal skills related to reducing risk behavior, including the ability to communicate and discuss risk status and possession of the skills necessary to negotiate safer behaviors.
Research has associated individual, interpersonal, and situational factors with sexual risk taking among MSM and has thus offered potential targets for intervention. These factors include greater pleasure in or enjoyment of risk-related sexual behavior, negative mood states, communication difficulties, social norms encouraging misperceptions of risk and risk taking, use of alcohol or recreational drugs, and life events and environments that are catalysts for risk taking.13,14
Elsewhere in this issue, Koblin et al.15 describe the demographics and prevalence of HIV-related risk behavior in a large, multicity, multiethnic cohort of MSM enrolled in EXPLORE, a randomized clinical trial designed to evaluate the impact on HIV incidence rates of a 10-session, individually delivered cognitive–behavioral intervention followed by quarterly maintenance sessions. Here, using baseline data from the EXPLORE cohort, we test the empirical foundation of the intervention’s design: both the salience of the factors targeted by the intervention as correlates of self-reported risk and the need to individualize delivery of the intervention because of the heterogeneous clustering of factors among at-risk men.
THE EXPLORE INTERVENTION
The EXPLORE behavioral intervention assumes that different core factors are associated with risk among different MSM and that interventions need to be tailored to address the factors most pertinent to a given individual. The intervention addresses these factors by integrating the approaches of (1) motivational interviewing,16–19 which addresses behavior change in areas in which individuals may be ambivalent; (2) the information–motivation–behavior model,20–22 as a means of supporting training in the use of specific skills (e.g., communicating one’s intentions to use a condom in different interpersonal contexts); and (3) social learning theory,23 which focuses on the normative components of behavioral change.
The first 3 EXPLORE sessions were designed to establish rapport between the counselor and the individual in the context of identifying those factors most salient to unsafe sex and those most important for effective self-protective behavior. Using factors relevant to the individual, counselors selected pertinent modules for subsequent sessions (Table 1 ▶) from 6 domains drawn from the literature: (1) individual perception of risk behavior as examined through guided exploration of participants’ sexual episodes; (2) attitudes and skills that facilitate or impair clear communication of risk limits; (3) beliefs about serostatus and its role in choosing whether to practice safer sex; (4) the role of substance use in promoting personal risk behavior; (5) aspects of partners, events, and places that are associated with risky behavior; and (6) planning for ongoing adherence to personal safety plans adopted in EXPLORE sessions.
TABLE 1—
EXPLORE Counseling Modules: Core Theme and Session Focus
| Module | Core Theme | Session Focus | |
| Module 1 | Being HIV negative and participating in EXPLORE | Participants state why they want to stay HIV negative; desire to remain negative is made explicit | |
| Mixed feelings about sex and risk are examined and normalized, beginning the focus on ambivalence16,18,19 | |||
| Modules 2 and 3 | Risk: What’s acceptable to me? | Knowledge of risk factors for infection is assessed | |
| Crossing acceptable risk limits | Personal relevance of risk reduction guidelines is examined through recent sexual episode narratives; individual attitudes regarding “acceptable” risk | ||
| Discussion regarding pleasure of unprotected sex.25,26 | |||
| Modules 4 and 5 | Sexual communication: HIV status, spoken and unspoken messages | Attitudes and skills that facilitate or impair clear communication of risk limits27; communication about serostatus; the role of being part of a couple that employs risk limits or negotiated safety arrangements28–31 | |
| Module 6 | Sex, drinking, and drugs | Impact of substance use on risk behavior32,33 | |
| Modules 7, 8, 9 | Places and events as triggers Feelings and thoughts as triggers Partners as triggers |
How personal, social, and environmental factors may trigger risky sex or preventive behavior Examination and skills training to manage risk when presented with |
|
| Module 10 and maintenance | Planning for maintenance Staying HIV negative |
Planning for ongoing adherence to personal safety plans, including training for relapse prevention41–43; applying lessons from modules to changing life situations |
Although this approach tailors selection of emphases and approaches to the individual, all modules used during the intervention were structured in accordance with guidelines provided in a detailed counseling manual.24 The aim of the present study was to provide empirical validation for this individualized approach by examining the homogeneity or heterogeneity observed among the EXPLORE cohort in terms of the distribution of the factors under study and the association of these factors with self-reported risk behaviors.
METHODS
Study Population and Procedures
Details regarding study recruitment, baseline visits, data collection and management, and study monitoring are described by Koblin et al.15
Data Collection
Using audio computer-assisted selfinterviewing (ACASI) technology, participants completed 22 items, scored on a 6-point Likert scale (strongly disagree to strongly agree), that measured self-efficacy regarding risk reduction, communication skills, and social norms about safer sex. Three items focusing on enjoyment of specific risk behaviors were prefaced with the following: “Please indicate how much you enjoy or think you enjoy doing the following activities with a man. Please answer for each sexual activity whether you have done it or not.” These 3 items were as follows: (1) “You have insertive anal sex with your partner and you don’t use a condom”; (2) “You have receptive anal sex with your partner and he does not use a condom”; and (3) “You have oral sex with your partner and you don’t use a condom.” Responses were scored on a 4-point Likert scale (dislike very much, dislike, enjoy, enjoy very much). ACASI was also used in collecting alcohol and drug use data and information on sexual risk behaviors.15
Statistical Analysis
The purpose of the analysis was to investigate the homogeneity or heterogeneity of domains associated with the intervention targets and their association with unsafe sexual practices. We first examined the distribution of the measures of self-efficacy for adopting safer sexual behaviors, communication skills, social norms about safer sex, and enjoyment of risk-related behaviors. Second, we assessed the distribution of combinations of these factors, and of alcohol and drug use. Finally, we evaluated the relationships of these factors, both separately and in combination, with sexual risk behaviors reported during the 6 months preceding baseline.
An exploratory factor analysis of the 22 items verified the presence of 3 factors in the baseline data: self-efficacy, communication skills, and social norms. These factors consisted of 9, 6, and 5 items, respectively. We constructed factor-based scales using the additive quantities of the scores for each item (based on the 1–6 scoring) and rescaled scores as 0 to 100, with lower scores reflecting lower self-efficacy, poorer communication skills, and weaker perceptions that social norms favor safer sex. Factor scores were dichotomized at 50, the midpoint of the range; scores below 50 represented disagreement with items reflecting safer behaviors.
In a similar fashion, we dichotomized enjoyment of risk-related behavior by combining the responses enjoy somewhat and enjoy very much and the responses dislike somewhat and dislike very much. To examine combinations of these factors, we coded each participant in terms of whether he had a low score (50 or less) on the factors, whether he enjoyed unprotected receptive anal sex (the riskiest behavior), whether he reported heavy alcohol use (defined as consumption of 4 or more drinks per day or 6 or more drinks per occasion), and whether he reported any noninjection drug use.
We used z-score statistics to evaluate the relationships between the factors and specific sexual risk behaviors. We compared the percentages of participants who reported enjoying (defined as “enjoy/enjoy very much”) each of the 3 risk behaviors, using z-score statistics. Finally, using logistic regression, we examined the associations between a summary variable of high-risk sex and combinations of the factors in conjunction with heavy alcohol use and noninjection drug use. High-risk sex was defined as receptive or insertive anal sex with an HIV-positive partner or a partner of unknown serostatus without use of condoms. The estimated regression coefficients produced were used to obtain the odds ratio associated with each combination.
RESULTS
One third of the cohort (Table 2 ▶) reported low communication skills, twice the percentage that reported low self-efficacy or weak social norms. Seventy-five percent of the participants reported enjoying insertive anal sex with their partner without using a condom, whereas 53% and 52% reported enjoyment of receptive and oral sex without using a condom, respectively.
TABLE 2—
Distributions of Factors: Self-Efficacy, Communication Skills, Safer Sex Norms, and Enjoyment of Unsafe Sex: EXPLORE, 1999–2001
| Factor | No. (%) |
| Self-efficacy for safer sex score | |
| 0–25 | 117 (2.8) |
| 26–50 | 522 (12.5) |
| 51–75 | 1467 (35.2) |
| 76–100 | 2063 (49.5) |
| Communication skills score | |
| 0–25 | 292 (7.3) |
| 26–50 | 1095 (27.2) |
| 51–75 | 1296 (32.2) |
| 76–100 | 1342 (33.3) |
| Safer sex norms score | |
| 0–25 | 138 (3.4) |
| 26–50 | 588 (14.4) |
| 51–75 | 1652 (40.4) |
| 76–100 | 1710 (41.8) |
| Enjoyment of unprotected insertive anal sex | |
| Dislike | 1055 (24.8) |
| Enjoy | 3194 (75.2) |
| Enjoyment of unprotected receptive anal sex | |
| Dislike | 1986 (47) |
| Enjoy | 2239 (53) |
| Enjoyment of unprotected oral sex | |
| Dislike | 2048 (48.1) |
| Enjoy | 2209 (51.9) |
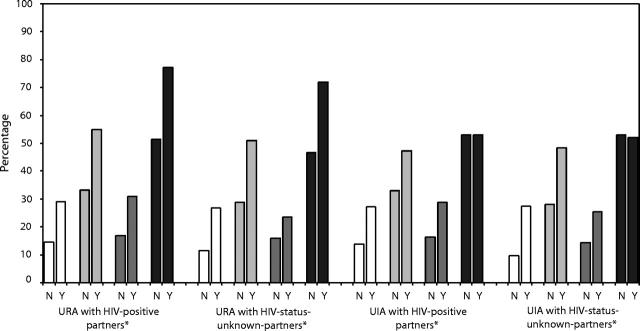
The 3 factor scores and enjoyment of unprotected receptive anal sex were associated with sexual risk behaviors (Figure 1 ▶). Men reporting sexual risk behaviors were significantly more likely than men not reporting such behaviors to have low scores (50 or less) on the safer sex self-efficacy measure (P < .0001). Participants reporting unprotected anal sex (either receptive or insertive sex with partners of unknown or positive serostatus) were more likely to have low scores on the communication factor than were those who did not report such behavior (P < .0001). Men reporting unprotected anal sex were also more likely than those who did not report unprotected anal sex to have low scores on the social norms factor (P < .0001).
FIGURE 1—
Percentages of men with low scores for self-efficacy for safer sex (white bars), communication skills (light gray bars), social norms (dark gray bars), and enjoyment of unprotected receptive anal sex (black bars), by sexual risk behaviors at baseline visit: EXPLORE, 1999–2001.
Note. N = no report of risk behavior 6 months before baseline; Y = report of risk behavior 6 months before baseline; URA = unprotected receptive anal sex; UIA = unprotected insertive anal sex.
*P < .0001.
Finally, 72% of the men reporting that they had engaged in unprotected receptive anal sex with a partner of unknown HIV status also reported enjoyment of unprotected receptive sex, compared with 47% of the men who did not report this risky behavior (P < .0001). Likewise, 77% of men reporting unprotected receptive anal sex with an HIV-positive partner also reported enjoyment of risk-related behavior, compared with 51% of those who did not report unprotected receptive anal sex with an HIV-positive partner (P < .0001).
Table 3 ▶ displays the 15 most prevalent distributions for combinations of factor scores and enjoyment scores and heavy alcohol use and noninjection drug use. The 2 largest subgroups (16% each) reported only noninjection drug use and only enjoyment of riskrelated behavior. The third largest subgroup endorsed none of the factors. The majority of the study population (57%) exhibited combinations of factors, such as enjoyment of risk-related behavior, low communication skills, and use of noninjection drugs (7%). In all, 62 combinations of risk were observed out of a possible 64, indicating that in this cohort of MSM, there was considerable heterogeneity in terms of combinations of risk-related factors.
TABLE 3—
Combinations of Risk-Related Factors, Heavy Alcohol Use, and Noninjection Drug Use and Their Association With Risky Sexual Behaviors: EXPLORE, 1999–2001
| Self-Efficacya | CommunicationSkillsa | Social Normsa | Enjoy URAa | HeavyAlcohol Usea | Noninjection Drug Usea | No. (%) | Estimated Odds Ratio for Risky Sex (95% Confidence Interval) |
| No | No | No | No | No | Yes | 604 (16.1) | 1.7 (1.5, 2.0) |
| No | No | No | Yes | No | Yes | 599 (15.9) | 2.0 (1.6, 2.4) |
| No | No | No | No | No | No | 413 (11.0) | Reference |
| No | No | No | Yes | No | No | 290 (7.7) | 1.1 (1.0, 1.3) |
| No | Yes | No | Yes | No | Yes | 256 (6.8) | 4.2 (3.3, 5.3) |
| No | Yes | No | No | No | Yes | 156 (4.2) | 3.7 (3.0, 4.5) |
| Yes | Yes | No | Yes | No | Yes | 108 (2.9) | 10.2 (7.6, 13.7) |
| No | Yes | No | Yes | No | No | 105 (2.8) | 2.4 (2.0, 2.9) |
| No | Yes | No | No | No | No | 89 (2.4) | 2.1 (1.8, 2.4) |
| No | No | Yes | Yes | No | Yes | 80 (2.1) | 3.1 (2.3, 4.0) |
| No | No | No | No | Yes | Yes | 76 (2.0) | 1.9 (1.5, 2.5) |
| Yes | Yes | Yes | Yes | No | Yes | 74 (2.0) | 15.8 (11.5, 21.8) |
| No | No | Yes | No | No | Yes | 62 (1.6) | 2.7 (2.1, 3.4) |
| No | Yes | Yes | Yes | No | Yes | 57 (1.5) | 6.5 (4.8, 8.7) |
| No | No | No | Yes | Yes | Yes | 51 (1.4) | 2.2 (1.6, 2.9) |
| All other combinationsb | 739 (19.7) |
Note. Risky sex was defined as unprotected receptive or insertive anal sex with HIV-positive partners or partners of unknown status.
aSelf-efficacy, communication skills, and social norms: yes = ≤ 50; no = > 50. Enjoy URA (unprotected receptive anal sex): yes = enjoy very much or enjoy; no = dislike or dislike very much. Heavy alcohol use: yes = ≥ 4 drinks per day or ≥ 6 drinks per occasion. Noninjection drug use: yes = any report of at least 1 type of noninjection drug.
bOf the total 62 combinations, 47 were classified as “other.” All “other” combinations had frequencies less than 1.3%.
Logistic regression analyses of these data showed that different combinations of riskrelated factors were associated with varying levels of selfreported sexual risk behaviors (Table 3 ▶). For example, those who exhibited the most prevalent pattern, involving only noninjection drug use, had an odds ratio (relative to those who reported none of the risk factors) of engaging in risky sex of 1.7 (95% confidence interval [CI] = 1.5, 2.0). Conversely, the 12th most prevalent subgroup (2% of the cohort), whose members endorsed all of the factors examined, including enjoyment of unprotected receptive anal sex and noninjection drug use, had an odds ratio of 15.8 (95% CI = 11.5, 21.8) for risky sex. The next most risky subgroup (3% of the cohort), with the same profile except for the social norm factor, had an odds ratio of 10.2 (95% CI = 7.6, 13.7). The highest odds ratio observed was 17.3 (95% CI = 12.0, 25.0), for the 28th most prevalent subgroup. Members of this subgroup endorsed all of the study factors associated with risk along with enjoyment of unprotected receptive anal sex, noninjection drug use, and heavy alcohol intake. The estimated odds ratios for all of the remaining 47 combinations of the risk factors (data not shown) were greater than the odds ratio for the reference group (i.e., 1.0).
DISCUSSION
EXPLORE baseline data reveal considerable heterogeneity in the study cohort of MSM in terms of the distribution of cognitive–behavioral factors that influence sexual risk taking and heavy alcohol use and noninjection drug use. The 2 most prevalent patterns accounted for only one third of the cohort. These factors also were significantly associated with self-reported risk behaviors among the cohort members. Our findings support an individualized approach to behavioral risk reduction counseling in which the specific targets are those most salient to an individual’s unique profile.
One of the most common factors reported, by 75% of cohort members, was enjoyment of unprotected anal sex. This factor presents a potential barrier to behavior change motivation, which supports use of approaches such as motivational interviewing that are designed specifically for populations not strongly motivated to change.16–19 In EXPLORE, motivational interviewing is used to identify ambivalence toward reducing risk behavior, with a counseling focus on enhancing intrinsic motivation for change by articulating reasons for and costs and benefits of change.
Weak communication skills were another prevalent factor, exhibited by 35% of the cohort and appearing in 7 of the top 15 most prevalent risk combinations. For some participants, communication difficulties appeared in combination with alcohol and drug use; for others, such difficulties appeared in combination with a low selfefficacy for adopting safer behaviors. To succeed in lowering risks among MSM presenting with these risk combinations, interventions need to incorporate strategies that provide information and behavioral skill building; an example of such a strategy is the information–motivation–behavior model20–22 used in EXPLORE to teach specific skills in different contexts.
The third most prevalent factor combination comprised 11% of the cohort. Individuals exhibiting this combination, used as the reference group in the logistic regression analysis, endorsed none of the factors thought to be associated with risk behavior and reported neither heavy alcohol use nor noninjection drug use. All of the other combinations had odds ratios greater than 1, suggesting that participants in the reference group were less likely than the majority of the cohort to be engaging in high-risk behaviors at the time of enrollment.
Longitudinal studies11,13 show, however, that risk behaviors among MSM can increase over time. Even among men showing low risk at baseline, it can be expected that some will increase their risk behavior over the duration of a trial. Individually tailored counseling approaches similar to that taken in EXPLORE allow counselors to reinforce current safer sex practices among these individuals while helping them anticipate changes in life circumstances and relationships that could be associated with increases in risk. For example, when a monogamous relationship is at risk of ending, counselors would rely on the information–motivation–behavior model20–22 to provide training in communication skills regarding serostatus and on motivational interviewing16–19 to address ambivalence about using alcohol or noninjection drugs, which might assist individuals in managing depressed mood but increase their likelihood of risky behaviors.
The EXPLORE baseline data support the relevance to at-risk MSM of the factors targeted by the study’s counseling methods and the content of the behavioral intervention. In addition, the heterogeneity with which these factors were shown to be distributed among the cohort members reinforces the importance of a tailored approach in which structured modules are selected and implemented in a manner consistent with individuals’ unique characteristics which predispose them to engage in risk behavior.
Acknowledgments
Support for this study was provided by the National Institute of Allergy and Infectious Diseases through the HIV Prevention Trials Network (grant 5 U01 AI46749-03 to Family Health International, with a subcontract to Abt Associates Inc; grant U01 AI48016 to the New York Blood Center; grant U01 AI47981-04 to the University of Washington; grant U01 AI48040 to the Fenway Community Health Center; and grant U01 AI47995 to the San Francisco Department of Public Health).
The members of the EXPLORE Study Team are as follows: Fenway Community Health Center: Felipe Agredano, Rodrigo Barahona, Keith Bell, Christine Borges, Manual Burnias, Mark Cayabayab, Dan Church, Allison Cohn, Yvonne Colon, Janet Dargon, Nancy DeSousa, Judy Erdman, Josh Gagne, Eliza Goodhue, Juan Jimenez, William Johnson, Wilfred Labiosa, Ana Lara, Darren LeBlanc, Vin Longo, Marc Manseau, Marshall Miller, Matthew Mimiaga, Elie Mohns, Arnel Montenegro, David Pantalone, Oscar Patino, Tracey Rogers, Edual Ruiz, Liz Salomon, Julio Silva, Laura van der Leeden, Rodney VanDerwarker, and Curt Weber. Howard Brown Community Health Center: Althea Batticks, Jason Bird, Liz Bradshaw, Robert Brown, Tom Buckingham, Toni Buckingham, Kelly Carson, Irene Chubinsky, Scott Clark, Scott Cook, Jeff Eichholz, Erica Gaffold, Sanford Gaylord, Mark Hartfield, David Henry, Brent Hope, Dale Gluth, Shane Gosselink, Jenny Hopwood, Laura Hosto, Jennifer Howard, D. J. Jacques, Heather Jandura, Susan Killelea, Andy Knight, Simone Koehlinger, Melissa Kohnke, Felicity LaBoy, Han Lee, Kandis Martin, Nicole Martin, Michele McGrady, Cheron McNeal, Denise Miles, Gino Moore, Michael Munn, Jose Narvaez, Aisha Nawab, Arlette Oblaza, Kevin O’Keefe, Liz Perez, Elisse Pertiller, Kelly Picketts, Borris Powell, Chris Powers, Bart Ramey, Ingrid Rodriguez, Laurez Rutledge, Porfirio Sanchez, Michael Saven, Chris Schmidt, Mark Schulze, Jim Skinner, David Snyder, Al Sorrese, Justin St. Andre, Gerry Taranzo, Ted Taylor, Sonia Torres, Kristin Vanfossan, Gregory Victorianne, and Erik Wetz. Denver Public Health: Misty Aas, Ramon Armendariz, Chloe Bailey, Brian Bost, Julie Caine, David Cline, Stuart Cooper, Kent Curtis, Beth Deyo, John Douglas, Michael Furhman, Rene Gonzalez, Jeff Hiller, Paul Huber, Sharon Huber, Ken Miller, Philip Osteen, Laurie Peter, Doug Robinson, Dave Ward, Tim Wright, and Andrew Yale. New York Blood Center: Anne Aldrich, Louise Austin, Lynne Bartell, Jane Bensel, Roberta Bernet, Damian Bird, Adam Bonilla, Carolyn Booher, Michael Camacho, Bradley Clark, Kent Curtis, Nikki Englert, Tonya Flores, George Gates, Corinne Geller, Octavio Gonzalez, Denise Goodman, Krista Goodman, Joshua Hinson, Sean Lawrence, Thomas Lee, Jay Loeffel, Angelo Luna, Larry Metzger, Carolle Morris, Patrick O’Quinn, Eric Ortiz, Ofiji Parris, Alfredo Perez, Terrence Precord, Alberto Rodriguez, Jason Santiago, Craig Siulinski, Leah Strock, Paul Teixeira, Eric Torres, Francesca Valenti, Curt Weber, Avery White, and Jess Zimmerman. University of Washington: Scott Britt, Fransing Daisy, Aline Dang, Tennessee Dickenson, Niles Eaton, Terry Elliott, Raymond Evans, Paul Farley, Mark Fleming, George Froehle, Jerome Galea, Hal Garcia-Smith, Patrick Gonzalez, Bruce Gooding, Krista Goodman, Justin Haines, Keifa Herzog, Rick Hieb, Eric Hildebrandt, Damon Jameson, E. J. Janson, Thom Kelty, Bill Krutch, Erin Lennon, Matt Leidholm, Alfredo Lopez, Paul Louey, Matt Meko, Jenny Melmed, Dany-Paul Mucha, Shelley Ozscuro, Joe Picciano, Jim Price, Monica Rayne, Alex Rodriguez, Barbara Steele, Nancy Stoaks, Jason Stucky, Matthew Swank, Stephen Tabet, Jeff Thompson, Dennis I. Torres, John Torres, Patrick Tschumper, Paul B. Verano, Ken Wheeler, and Robert Yoon. San Francisco Department of Public Health: Jonas Abella, Mike Ahern, Ari Bacharat, Alba Barreto, Christopher Boyden-DeShazer, Susan Buchbinder, Jesse Brooks, Meredith Broome, Tony Buckman, David Colbert, Emily Cole, Joao De Sales, Alfonso Diaz, Michael Edgar, Beth Faraguna, Paige Fratesi, Vincent Fuqua, Reggie Gage, Anjali Garg, Dale Gluth, Ted Guggenheim, Gavin Hall, Thomas Knoble, Rachel Langdon, Irene Lee, Jennifer Lessard, Nicole Lightburn, Tim Matheson, Corvette Moore, Mario Moreno, Paul O’Malley, Jennifer Owen, Jesus Perez, Robin Rifkin, Chris Rubino, Mateo Rutherford, Jennifer Sarche, Georgia Schreiber, Rob Schwarz, Craig Siulinski, John Stryker, Jason Tomasian, Jim Touchstone, Seth Watkins, Sarah Wheeler, Belinda Van, and Allison Zerbe. Abt Associates: Dana Benet, Samuel Bozeman, Maria Madison, and Sean McKee. Center for AIDS Prevention Studies: Kevin Filocamo, Cliff Leonardi, Matthew Troy, and Scott Stumbo. Statistical Center for HIV/AIDS Research and Prevention: Neil Albright, Geetha Beauchamp, Rana Bonnice, Lynette Browne, Claire Chapdu, Maya Covarrubias, Martina Deseyve, Lynda Emel, Alice Fisher, Eileen Hess, Sarah Holte, MaryAnn Klotz, Wolfe Maykut, Peter McDonnell, Barbara Metch, Geoff Minerbo, Lisa Ondrejcek, Jennifer Schille, Steve Self, and Al Williams.
Human Participant Protection
This study was approved by the institutional review boards of all institutions involved. Written informed consent was obtained from all participants.
Note. The content of this article does not necessarily reflect the views or policies of the National Institute of Allergy and Infectious Diseases or the HIV Prevention Trials Network, nor does mention of trade names, commercial products, or organizations imply endorsement by the US government.
Contributors
M. A. Chesney, B. A. Koblin, and T. J. Coates conceived the study and oversaw all aspects of its implementation. P. J. Barresi was a leader in the development of the EXPLORE intervention. M. J. Husnik and Y. Huang performed the data analyses. B. A. Koblin, C. L. Celum, G. Colfax, K. Mayer, D. McKirnan, and F. N. Judson supervised all aspects of study implementation at the individual research sites. All of the authors helped to conceptualize ideas, interpret findings, and review drafts of the article.
Peer Reviewed
References
- 1.Response to the Updated Estimates of HIV Infection in San Francisco. San Francisco, Calif: San Francisco Dept of Public Health and AIDS Research Institute, University of California, San Francisco; 2000.
- 2.Kellogg T, McFarland W, Katz M. Recent increases in HIV seroconversion among repeat anonymous testers in San Francisco [letter]. AIDS. 1999;13:2303–2304. [DOI] [PubMed] [Google Scholar]
- 3.Dukers NH, Spaargaren J, Geskus RB, et al. HIV incidence on the increase among homosexual men attending an Amsterdam sexually transmitted disease clinic: using a novel approach for detecting recent infections. AIDS. 2002;16:F19–F24. [DOI] [PubMed] [Google Scholar]
- 4.Catania JA, Osmond D, Stall RD, et al. The continuing HIV epidemic among men who have sex with men. Am J Public Health. 2001;91:907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koblin BA, Torian LV, Guilin V, Ren L, MacKellar DA, Valleroy LA. High prevalence of HIV infection among young men who have sex with men in New York City. AIDS. 2000;14:1793–1800. [DOI] [PubMed] [Google Scholar]
- 6.Valleroy LA, MacKellar DA, Karon JM, et al. HIV prevalence and associated risks in young men who have sex with men. JAMA. 2000;284:198–204. [DOI] [PubMed] [Google Scholar]
- 7.Wolitski R, Valdiserri R, Denning P, Levine W. Are we headed for a resurgence of the HIV epidemic among men who have sex with men? Am J Public Health. 2001;91:883–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams LA, Klausner JD, Whittington WL, Handsfield HH, Celum C, Holmes KK. Elimination and reintroduction of primary and secondary syphilis. Am J Public Health. 1999;89:1093–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fox K, del Rio C, Holmes K, et al. Gonorrhea in the HIV era: a reversal in trends among men who have sex with men. Am J Public Health. 2001;91:959–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Outbreak of syphilis among men who have sex with men—Southern California, 2000. MMWR Morb Mortal Wkly Rep. 2001;50:117–120. [PubMed] [Google Scholar]
- 11.Ekstrand ML, Stall RD, Paul JP, Osmond DH, Coates TJ. Gay men report high rates of unprotected anal sex with partners of unknown or discordant HIV status. AIDS. 1999;13:1525–1533. [DOI] [PubMed] [Google Scholar]
- 12.Johnson WD, Hedges LV, Ramirez G, et al. HIV prevention research for men who have sex with men: a systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2002;30(suppl 1):S118–S129. [PubMed] [Google Scholar]
- 13.Stall RD, Hays RB, Waldo CR, Ekstrand M, McFarland W. The gay ’90s: a review of research in the 1990s on sexual behavior and HIV risk among men who have sex with men. AIDS. 2000;14(suppl 3):S101–S114. [PubMed] [Google Scholar]
- 14.Strathdee SA, Hogg RS, Martindale SL, et al. Determinants of sexual risk-taking among young HIVnegative gay and bisexual men. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;19:61–66. [DOI] [PubMed] [Google Scholar]
- 15.Koblin BA, Chesney MA, Husnik MJ, et al. High-risk behaviors among men who have sex with men in 6 US cities: baseline data from the EXPLORE Study. Am J Public Health. 2003;93:926–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller WR. Motivational interviewing: research, practice, and puzzles. Addict Behav. 1996;21:835–842. [DOI] [PubMed] [Google Scholar]
- 17.Miller WR. Motivational Enhancement Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals With Alcohol Abuse and Dependence. Rockville, Md: National Institute on Alcohol Abuse and Alcoholism; 1995.
- 18.Miller WR, Rollnick S. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York, NY: Guilford Press; 1991.
- 19.Rollnick S, Miller WR. What is motivational interviewing? Behav Cognitive Psychother. 1995;23:325–334. [Google Scholar]
- 20.Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychol. 1996;15:114–123. [DOI] [PubMed] [Google Scholar]
- 21.Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychol. 1994;13:238–250. [DOI] [PubMed] [Google Scholar]
- 22.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–474. [DOI] [PubMed] [Google Scholar]
- 23.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986.
- 24.Chesney M, Barresi P, Leonardi C, Filocamo K, Coates TJ. Project EXPLORE Manual. San Francisco, Calif: Center for AIDS Prevention Studies; 1998.
- 25.Kelly JA, Kalichman SC. Reinforcement value of unsafe sex as a predictor of condom use and continued HIV/AIDS risk behavior among gay and bisexual men. Health Psychol. 1998;17:328–335. [DOI] [PubMed] [Google Scholar]
- 26.Rader M, Marks G, Mansergh G, et al. Preferences about the characteristics of future HIV prevention products among men who have sex with men. AIDS Educ Prev. 2001;13:149–159. [DOI] [PubMed] [Google Scholar]
- 27.Molitor F, Facer M, Ruiz JD. Safer sex communication and unsafe sexual behavior among young men who have sex with men in California. Arch Sex Behav. 1999;28:335–343. [DOI] [PubMed] [Google Scholar]
- 28.Crawford JM, Rodden P, Kippax S, Van de Ven P. Negotiated safety and other agreements between men in relationships: risk practice redefined. Int J STD AIDS. 2001;12:164–170. [DOI] [PubMed] [Google Scholar]
- 29.Davidovich U, de Wit JB, Stroebe W. Assessing sexual risk behaviour of young gay men in primary relationships: the incorporation of negotiated safety and negotiated safety compliance. AIDS. 2000;14:701–706. [DOI] [PubMed] [Google Scholar]
- 30.Elford J, Bolding G, Maguire M, Sherr L. Sexual risk behaviour among gay men in a relationship. AIDS. 1999;13:1407–1411. [DOI] [PubMed] [Google Scholar]
- 31.Hoff CC, Coates TJ, Barrett DC, Collette L, Ekstrand M. Differences between gay men in primary relationships and single men: implications for prevention. AIDS Educ Prev. 1996;8:546–559. [PubMed] [Google Scholar]
- 32.Hospers HJ, Kok G. Determinants of safe and risk-taking sexual behavior among gay men: a review. AIDS Educ Prev. 1995;7:74–96. [PubMed] [Google Scholar]
- 33.Van de Ven P, Campbell D, Kippax S, et al. Gay men who engage repeatedly in unprotected anal intercourse with casual partners: the Sydney Men and Sexual Health Study. Int J STD AIDS. 1998;9:336–340. [DOI] [PubMed] [Google Scholar]
- 34.Binson D, Woods WJ, Pollack L, et al. Differential HIV risk in bathhouses and public cruising areas. Am J Public Health. 2001;91:1482–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Wit JB, de Vroome EM, Sandfort TG, van Griensven GJ. Homosexual encounters in different venues. Int J STD AIDS. 1997;8:130–134. [DOI] [PubMed] [Google Scholar]
- 36.Somlai AM, Kalichman SC, Bagnall A. HIV risk behaviour among men who have sex with men in public sex environments: an ecological evaluation. AIDS Care. 2001;13:503–514. [DOI] [PubMed] [Google Scholar]
- 37.Colfax GN, Mansergh G, Guzman R, et al. Drug use and sexual risk behavior among gay and bisexual men who attend circuit parties: a venue-based comparison. J Acquir Immune Defic Syndr. 2001;28:373–379. [DOI] [PubMed] [Google Scholar]
- 38.Paul JP, Catania J, Pollack L, Stall R. Understanding childhood sexual abuse as a predictor of sexual risk-taking among men who have sex with men: the Urban Men’s Health Study. Child Abuse Negl. 2001;25:557–584. [DOI] [PubMed] [Google Scholar]
- 39.Martin JI, Knox J. Loneliness and sexual risk behavior in gay men. Psychol Rep. 1997;81:815–825. [DOI] [PubMed] [Google Scholar]
- 40.Martin JI, Knox J. Self-esteem instability and its implications for HIV prevention among gay men. Health Soc Work. 1997;22:264–273. [DOI] [PubMed] [Google Scholar]
- 41.Roffman RA, Stephen RS, Curtin L, et al. Relapse prevention as an interventive model for HIV risk reduction in gay and bisexual men. AIDS Educ Prev. 1998;10:1–18. [PubMed] [Google Scholar]
- 42.de Wit JBF, van Griensven GJP. Time from safer to unsafe sexual behaviour among homosexual men. AIDS. 1994;8:123–126. [DOI] [PubMed] [Google Scholar]
- 43.Brownell KD, Marlatt GA, Lichtenstein E, Wilson GT. Understanding and preventing relapse. Am Psychol. 1986;41:765–782. [DOI] [PubMed] [Google Scholar]