Abstract
Objectives. We measured the effect of Hurricane Floyd on Medicaid enrollment and health services use in the most severely affected counties of North Carolina.
Methods. We used differences-in-differences models on balanced panels of Medicaid claims and enrollment data.
Results. Overall spending per enrollee showed little short-term effect but demonstrated a moderate increase 1 year after the storm. We found very modest short-term increases in Medicaid enrollment, a small long-term decrease in enrollment, and large increases in the long-term use of emergency room and outpatient services.
Conclusions. Our findings suggest that hurricane victims experienced substantial changes in patterns of care that endured for much longer than the initial crisis period. These findings can have important implications for the management of disaster relief for this population.
The short-term effect of natural disasters has received considerable attention from the public health community.1–6 Disasters can have devastating economic consequences and a substantial impact on the incidence of disease and injuries.
Natural disasters are shocks to both the supply and demand of health services. On the supply side, natural disasters can profoundly affect the delivery of services; facilities may experience diminished staff levels and capacity because of damaged buildings and supplies. Supply-side shocks reduce service availability, an effect mitigated somewhat as temporary services become available. For example, Alson and colleagues examined services provided by a temporary field hospital after Hurricane Andrew7 and found that most services provided were not storm related but were routine medical services.
Demand-side shocks from natural disasters can either increase or decrease demand for care; short- and long-term effects may be different. Disasters can increase disease and injury incidence and acute levels of distress,8–10 thereby increasing service demand. Disasters can reduce demand as the costs of travel to facilities increase; time costs generally increase owing to competing needs such as home reconstruction, and the provision of substitute low-cost services increases.
The long-term effects of natural disasters on the use of medical services are not easily determined or well studied. One of the few extant reports examined changes in health care use resulting from the 1968 floods in Bristol, England11; it found significantly more hospital use during the year after the floods by residents with flooded houses than by those in the control group. Abrahams and colleagues found that after an Australian flood, the percentage of persons consulting their physician 3 or more times during the year following the flood was significantly higher than in a matched control group.12
We report here on the impact of a natural disaster, Hurricane Floyd, which affected North Carolina and other US states. We determine the effect of the hurricane and flooding on Medicaid enrollment and use of health services among Medicaid enrollees in the most severely affected North Carolina counties. Specifically, we (1) assess the impact of Hurricane Floyd on Medicaid enrollment, (2) determine its impact on the use of health services by Medicaid enrollees, and (3) examine trends in use in the weeks, months, and year after the hurricane.
HURRICANE FLOYD
Hurricane Floyd hit eastern North Carolina on September 15, 1999, dropping almost 20 inches of rain in certain areas. The flooding was the worst natural disaster ever to hit North Carolina.13 Fifty-one lives were lost.14 Within 48 hours of the hurricane’s arrival, 250 roads were closed15 and 50 000 people were housed in 235 shelters.16 More than 67 000 homes were damaged and about 8000 homes destroyed.13 Hurricane Floyd caused an estimated $6 billion in damage, and more than 87 500 people registered with the Federal Emergency Management Agency (FEMA).13 FEMA and the Economic Development Administration designated 44 out of 100 North Carolina counties as being substantially affected by the flooding.17
A variety of medical and public health responses during and immediately after the disaster have been documented.17–19 A survey of 18 hospital emergency rooms (ER) in eastern North Carolina found increases in suicide attempts, dog bites, febrile illnesses, basic medical needs, and dermatitis during the first week following the hurricane.17 After the flooding, substitutes for traditional health care services became available, including an emergency pharmaceutical and medical supply hot line set up to distribute donated pharmaceuticals and medical supplies.13
Some research has reported demand-side shocks resulting from Hurricane Floyd. Using a convenience sample of health care users in eastern North Carolina 4 months after the storm, Curry and colleagues found that about 20% of respondents reported worsening health problems and barriers to health care including transportation difficulties and difficulty finding time for clinic visits.20 Little research, however, has examined the impact of disasters on actual use of health services or on enrollment levels in health insurance plans. Furthermore, little has been done to examine the impact of disasters on health care use among vulnerable populations. One might expect, for example, that enrollment in Medicaid, an important part of the medical safety net, would increase during economic crises. Resulting patterns of use are unknown, but they have important implications for disaster relief, particularly for vulnerable populations.
DATA AND METHODS
Data
We used Medicaid claims and enrollment data from the North Carolina Medicaid program for July 1998 through December 2000. Claims data include information on all services reimbursed through the North Carolina Medicaid program. We excluded participants from the State Children’s Health Insurance Program (SCHIP) and the residents of 1 county (unaffected by the hurricane) that uses capitated health maintenance organization (HMO) contracts.
We examined the impact of Hurricane Floyd on inpatient, outpatient, ER, nursing home, and prescription drug use and expenditures. Inpatient, nursing home, and outpatient visits were identified by claim type according to a variable in the claims data. Outpatient visits were identified as unique combinations of enrollee identification number, provider identification number, and date of service, excluding monthly case management fees not tied to use. ER claims were identified through procedure codes or through service category codes; whereas either inpatient or outpatient visits could be ER visits, inpatient and outpatient visits themselves were mutually exclusive. Prescription drugs were not included in outpatient totals. Total expenditures include all of the above categories and others (e.g., home health, dental).
Users of all types of services, a subset of all enrollees, were identified as persons for whom any nonzero amount was paid by Medicaid during the study period.
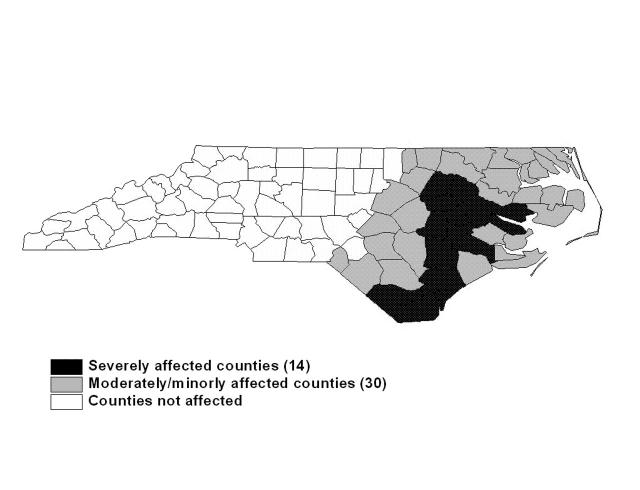
The 100 counties of North Carolina were separated into 3 groups according to FEMA’s assessment of hurricane impact17: severely affected counties (14), moderately or minimally affected counties (30), and the remaining 56 “unaffected” counties (Figure 1 ▶). This classification scheme may imperfectly classify counties. Many counties not classified as severely affected nevertheless suffered considerable damage; 66 total counties were federal disaster areas. In addition, we were unable to identify specific individuals who were directly affected by the storm. Because our control counties are not homogenous in their exposure to the hurricane, results using the combined set of unaffected and moderately affected counties may understate true differences in exposure between those counties severely affected and those completely unaffected. We therefore present a second set of results using only nonaffected counties as controls. Use was tied to the county of enrollee residence, not the county in which services were provided.
FIGURE 1—
Map of North Carolina showing counties that experienced moderate or severe damage from Hurricane Floyd in September 1999.
We aggregated claims files into county-level monthly and weekly files. Monthly county data include the total number of Medicaid enrollees, total medical expenditures, total number of visits or inpatient days reimbursed by Medicaid, and total number of service users. We used monthly data from July 1998 through September 2000, covering the period 14 months before the hurricane to 12 months after. We also used weekly data to examine time trends over a shorter 21-week period from July 4, 1999, to November 27, 1999.
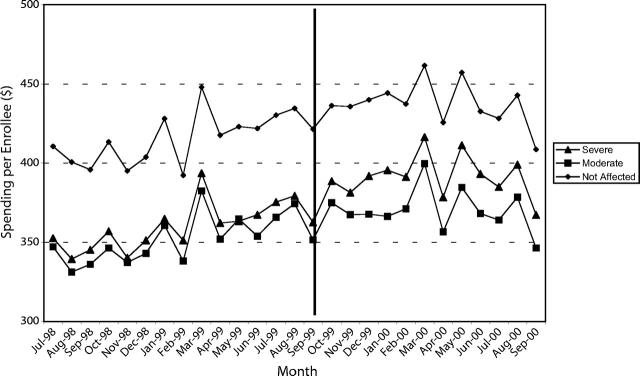
Figure 2 ▶ shows average spending per enrollee for the 3 types of counties. Several points are noteworthy. First, time trends are very similar across county types. Second, severely affected counties are similar to moderately affected counties in average spending before the storm but approach the higher level of spending in the unaffected counties before the storm. This pattern affects our choice of functional form of the time trend in the regression model, discussed below.
FIGURE 2—
Average spending per Medicaid enrollee before and after Hurricane Floyd in severely affected, moderately or minimally affected, and unaffected counties of North Carolina.
Methods
We ran all regression models on dependent variables that reflect use or expenditures per enrollee by means of ordinary least squares regression analysis. Dependent variables and means appear in Table 1 ▶. We used county and time fixed effects to control for effects that were either constant within counties over time or constant within each time period statewide, and we included a separate linear time trend for severely affected counties to control for prestorm trends. Models were weighted either by total county population in 1999 (enrollment models) or by total number of Medicaid enrollees in each county in each time period (all other models). We adjusted standard errors for heteroskedasticity, using a Huber–White correction. The very high R2 indicates that the reported linear models fit the data better than the log-linear models when we used the test proposed by Wooldridge.21
TABLE 1—
Variable Means in Affected and Unaffected North Carolina Counties Before and After Hurricane Floyd
| Monthly Average Before Hurricane | Monthly Average After Hurricane | Change | |||||
| 14 Severely Affected Counties | 85 Control Counties | 14 Severely Affected Counties | 85 Control Counties | 14 Severely Affected Counties, % | 85 Control Counties, % | Percentage Point Difference-in-Difference: Case–Control/Ratio | |
| Medicaid enrolleesa,b | 10 869 (5049) | 8331 (8293) | 11 067 (5126) | 8628 (8550) | 1.8 | 3.6 | −1.7/0.5 |
| Enrollees per capitaa,b | 0.17 (0.039) | 0.14 (0.052) | 0.17 (0.037) | 0.14 (0.052) | 0.0 | 0.0 | 0.0/1.00 |
| Total expenditures per enrollee,a,b $ | 366.81 (36.96) | 407.94 (58.27) | 395.66 (38.27) | 429.78 (60.36) | 7.9 | 5.4 | 2.5/1.46 |
| User/enrollee ratioa,b | 0.52 (0.13) | 0.57 (0.13) | 0.47 (0.028) | 0.49 (0.041) | −9.6 | −14.0 | 4.4/0.69 |
| Emergency room | |||||||
| Expenditures per enrollee,a $ | 9.46 (2.08) | 10.0056 (3.74) | 10.33 (2.30) | 10.71 (3.50) | 9.2 | 7.0 | 2.2/1.31 |
| Expenditures per visit,a $ | 102.44 (18.57) | 99.06 (32.95) | 107.02 (18.09) | 110.01 (34.053) | 4.5 | 11.1 | −6.6/0.41 |
| Visits per enrolleea | 0.095 (0.023) | 0.104 (0.028) | 0.098 (0.021) | 0.010 (.025) | 3.2 | −90.4 | 93.5/–.035 |
| Outpatient | |||||||
| Total expenditures per enrollee,a,b $ | 115.77 (21.0072) | 135.94 (31.15) | 127.17 (22.99) | 144.13 (33.47) | 9.8 | 6.0 | 3.8/1.63 |
| Total expenditures per visit,a,b $ | 70.25 (5.26) | 75.51 (10.71) | 76.71 (5.14) | 79.26 (8.92) | 9.2 | 5.0 | 4.2/1.84 |
| Total visits per enrolleea,b | 1.66 (0.36) | 1.89 (0.43) | 1.66 (0.28) | 1.82 (0.39) | 0.0 | −3.7 | 3.7/0.0 |
| Hospital expenditures per enrollee,a,b $ | 23.53 (5.57) | 26.09 (6.11) | 26.41 (6.69) | 27.95 (11.47) | 12.2 | 7.1 | 5.1/1.72 |
| Hospital expenditures per visit,b $ | 153.46 (19.11) | 154.55 (38.09) | 165.78 (21.94) | 159.60 (57.45) | 8.0 | 3.3 | 4.8/2.42 |
| Hospital visits per enrolleea,b | 0.15 (0.031) | 0.17 (0.041) | 0.16 (0.035) | 0.18 (0.045) | 6.7 | 5.9 | 0.8/1.14 |
| Inpatient expenditures per enrollee, $ | 63.46 (15.15) | 63.55 (21.51) | 63.48 (17.13) | 61.60 (20.06) | 0.0 | −3.1 | 3.1/0.0 |
| Nursing home expenditures per enrollee,a,b $ | 38.75 (19.83) | 52.64 (32.86) | 19.68 (11.85) | 28.93 (25.60) | −49.2 | −45.0 | −4.2/1.09 |
| Prescription drug expenditures per enrollee,a,b $ | 54.72 (10.66) | 60.13 (14.44) | 71.19 (12.97) | 77.53 (15.74) | 30.1 | 28.9 | 1.2/1.04 |
Note. Standard deviations are given in parentheses.
aP < .05 for comparison of 14 flooded counties with 85 nonflooded counties before the hurricane.
bP < .05 for comparison of 14 flooded counties with 85 nonflooded counties after the hurricane.
The variables of interest are the interaction between the indicator variable for the 14 severely affected counties and the relevant time period. Four time periods are reported in the monthly regression table (Table 2 ▶): the first month after the hurricane (October 1999), the first 2 months after the hurricane (October–November 1999), the first 3 months after the hurricane (October–December 1999), and the first year after the hurricane (October 1999–September 2000). Only one Time Period × 14-County Indicator Variable interaction is used in each model. We present the models first with both moderately affected and unaffected counties used as controls and then with only unaffected counties used as controls. We further explore selected results using weekly data (results not reported). Relevant time periods here are not cumulative, as in the monthly tables, but instead are used to show interactions between the 14-county variable and the indicators for the week of the hurricane and the 3 subsequent weeks. The interpretation of the coefficient of the variable of interaction for this table is the change in the relevant dependent variable during the relevant period associated with the hurricane over the level that would have been predicted in its absence. A danger of this approach is that if unrelated events occurred disproportionately during the posthurricane period in these 14 counties, the effects of these events may erroneously be attributed to the hurricane.
TABLE 2—
Estimates of Hurricane Floyd’s Effect on North Carolina Medicaid Enrollment and Use From Regression Models: Monthly Unit Change After Hurricane in 14 Severely Affected Counties in North Carolina
| First Month | First 2 Months | First 3 Months | First Year | |||||
| Measure | Moderately Affected and Unaffected Controls | Unaffected Controls Only | Moderately Affected and Unaffected Controls | Unaffected Controls Only | Moderately Affected and Unaffected Controls | Unaffected Controls Only | Moderately Affected and Unaffected Controls | Unaffected Controls Only |
| Medicaid enrolleesa | 112.39** (45.99) | 136.03*** (49.46) | 81.25** (37.55) | 92.66** (40.55) | 70.97** (33.74) | 68.15* (35.42) | −90.97** (44.97) | −116.76** (46.92) |
| Total expenditures per enrollee | 0.93 (3.80) | 2.54 (4.22) | −1.53 (3.94) | −1.24 (4.83) | −0.093 (3.26) | −0.64 (3.80) | 7.14* (3.70) | 5.28 (4.05) |
| User/enrollee ratio | 0.0071 (0.020) | 0.013 (0.022) | 0.0084 (0.015) | 0.013 (0.016) | 0.0068 (0.012) | 0.010 (0.013) | 0.015 (0.016) | 0.018 (0.017) |
| Emergency room | ||||||||
| Expenditures per enrollee | 0.63** (0.30) | 0.76** (0.30) | 0.51** (0.22) | 0.80*** (0.21) | 0.19 (0.19) | 0.39** (0.19) | 0.79*** (0.27) | 0.69*** (0.26) |
| Expenditures per visit | −2.77 (2.06) | −2.82 (2.13) | −4.98*** (1.58) | −3.66** (1.54) | −3.76** (1.63) | −2.75* (1.62) | −1.00 (2.02) | −4.07** (1.97) |
| Visits per enrollee | 0.0078*** (0.0019) | 0.0095*** (0.0019) | 0.0091*** (0.0016) | 0.0108*** (0.0016) | 0.0056*** (0.0016) | 0.0066*** (0.0017) | 0.0084*** (0.0021) | 0.0103*** (0.0022) |
| Outpatient | ||||||||
| Total expenditures per enrollee | 0.22 (1.15) | −0.15 (1.34) | −1.82 (2.05) | −3.11 (3.13) | −2.00 (1.46) | −2.88 (2.17) | 4.80*** (1.64) | 3.76* (2.07) |
| Total expenditures per visit | −0.084 (1.10) | −0.45 (1.25) | −1.49 (1.24) | −2.16 (1.67) | −1.64* (0.93) | −2.07* (1.21) | 0.11 (1.09) | −0.40 (1.23) |
| Total visits per enrollee | 0.0076 (0.024) | 0.012 (0.027) | 0.016 (0.019) | 0.018 (0.020) | 0.014 (0.016) | 0.014 (0.018) | 0.072*** (0.023) | 0.077*** (0.025) |
| Hospital expenditures per enrollee | 1.83** (0.76) | 1.90** (0.83) | −0.82 (1.94) | −1.63 (3.01) | −0.75 (1.31) | −1.15 (2.03) | 0.49 (0.99) | −0.047 (1.47) |
| Hospital expenditures per visit | 1.52 (3.99) | −0.23 (4.20) | −11.52 (8.70) | −16.61 (13.34) | −9.16 (5.99) | −12.57 (9.07) | −1.13 (4.95) | −5.03 (6.85) |
| Hospital visits per enrollee | 0.0085*** (0.0023) | 0.0108*** (0.0022) | 0.0091*** (0.0017) | 0.0110*** (0.0017) | 0.0060*** (0.0016) | 0.0082*** (0.0016) | 0.0072*** (0.0021) | 0.0090*** (0.0022) |
| Inpatient expenditures per enrollee | 1.56 (4.12) | 3.52 (4.36) | −0.004 (2.85) | 1.20 (3.06) | 3.31 (2.70) | 3.45 (2.80) | 1.13 (3.28) | −0.21 (3.40) |
| Nursing home expenditures per enrollee | 0.76 (3.81) | −1.16 (4.17) | 1.81 (2.79) | 1.46 (2.98) | 0.52 (2.16) | 0.89 (2.29) | −3.04 (2.91) | −3.53 (3.21) |
| Prescription drug expenditures per enrollee | 0.59 (0.80) | 0.85 (0.83) | 0.86 (0.94) | 0.99 (0.97) | 0.67 (0.96) | 0.58 (0.99) | 1.53* (0.92) | 1.65* (0.94) |
Note. Each entry is the coefficient estimate on the interacted 14-county–posthurricane indicator for the relevant time period from a separate differences-in-differences model. The R2s for all models reported are always greater than 0.93. Robust standard errors (in parentheses) are adjusted for heteroskedasticity by use of a Huber-White correction. All models also control for county and time fixed effects and for a separate time trend in severely affected counties.
aWeighted by county population in 1999.
*P < .1; ** P < .05; *** P < .01.
RESULTS
Table 1 ▶ contains the means of monthly variables used in the analyses. Means are presented separately for the severely affected counties and for all other counties, for the periods before and after the hurricane. Service use per enrollee was somewhat higher in the control counties than in affected counties, although some differences disappeared after the hurricane. These differences indicate the need to control for trends in use that began before the hurricane; in all reported regression models, we controlled for these effects by using county-specific indicator variables, monthly fixed effects, and a separate linear time trend for affected counties.
Table 2 ▶ provides coefficient estimates from the fixed effects regressions on monthly data described above. As can be seen from the first row of data, in the first month after the hurricane, an average increase in Medicaid enrollment of 112 persons was observed over what would be predicted had the hurricane not occurred, whereas there was an increased enrollment of 136 persons over trends based on unaffected counties only. In the discussion below, we mention only the effect over the full set of counties when the level of impact is similar and identify discrepancies between the 2 sets of estimates. The 81-person increase predicted in the first 2 months (third column) indicates that the average enrollment increase in the second month was smaller than that in the first month. Although the data on which these models were run constitute the entire population of North Carolina Medicaid enrollees and users (thus making statistical tests of significance less critical than if we had sampled enrollees), conventional measures of statistical significance are reported, since the data may be construed as a sample of the population of Medicaid enrollees across states and time. The last column indicates that during the first year after the hurricane, the 14 counties each experienced an average decrease in enrollment of 91 people per month over what would have been predicted had the hurricane not occurred.
These modest increases (approximately 1%) in Medicaid enrollment during the short-term period of 3 months after the storm, and decreasing Medicaid enrollment in the long run, were somewhat surprising and contrary to our hypothesis. This finding was consistent for elderly and disabled enrollees (not reported). Temporary Assistance for Needy Families (TANF) enrollees, despite the extension of TANF eligibility after the storm, and Medical Assistance for Families enrollees exhibited declines of 2% to 5% in the severely affected counties. Only children enrolled in the Infants and Children program showed significant enrollment increases (4% per month) in the short run.
We investigated enrollment further by examining the role that out-migration may have played. We find no evidence of disproportionate migration from these 14 counties into other North Carolina counties after the hurricane; migration to other states is unobservable in these data. We also examined the percentage of outpatient visits to providers outside enrollees’ county of residence to determine whether out-migration from these counties occurred without an update in the enrollment file. Enrollees would increase their visits to providers out of their county of residence if in fact they had moved out of county and obtained services in their new county of residence. We found no disproportionate increase in out-of-county use. No reasonable monthly estimates of total county population could be obtained, so we cannot rule out a large decrease in the number of residents in these counties after the flooding. If outmigration occurred in the general population, actual Medicaid enrollment rates could have increased. We did find disproportionately higher first-time enrollment (7.3% increase) after the flood than before the flood.
From Table 2 ▶, we see that total expenditures per enrollee show little change during the first 3 months after the storm, but an average spending increase of $7.14 per enrollee each month is observed during the first full year after the storm. The ratio of users of any type of service to total enrollees shows virtually no change in the short or long run, suggesting that the hurricane had negligible impact on total access to services, although the remaining results show that patterns of care changed substantially.
As expected, ER expenditures per enrollee increased immediately after the hurricane by less than a dollar per enrollee (7%), but this rate declined over the first 3 months. One year after the disaster, however, ER expenditures were still $0.80 higher per enrollee (8%) than would be predicted without the hurricane. The second ER row of Table 2 ▶ shows the effect of the hurricane on expenditures per ER visit. Average cost per visit decreased after the hurricane in the 14 counties, probably indicating a shift toward relatively “low-tech” visits (to be expected in response to minor flood-related health conditions) perhaps owing to the substitution of the ER for primary care services. A competing explanation suggests that an increase in ER visits occurred at hospitals with lower costs per visit. At 1 year, average spending per ER visit returned to just $1.00 less than the level experienced in all other counties, but it was $4.07 lower than spending in unaffected counties. There were substantial increases in ER visits per enrollee both during the first 3 months and throughout the first year after the hurricane (6%–10%).
Outpatient expenditures per enrollee remained stable during the months after the hurricane, with a small decline in months 2 and 3. During the first year after the hurricane, there was a $4.80 average monthly increase in spending over what would have been predicted without the storm. Outpatient spending per visit showed a small decline in the short run and very little long-term change, suggesting that the intensity of outpatient visits remained fairly constant. Most surprisingly, virtually no short-term change in the number of outpatient visits per enrollee was seen to result from the storm. This suggests that increased ER use was not owing to the substitution of ER visits for outpatient visits, which would have been the case if physician office and outpatient facility closures reduced outpatient capacity. We did find a small long-term increase (4.3%) in outpatient visits per enrollee.
Hospital outpatient expenditures and visits per enrollee show a pattern similar to that of ER visits, except at a lower magnitude. Hospital outpatient spending per visit shows large declines during the second and third months after the hurricane but little change on average over the first full year. Again, this pattern indicates that although the intensity of initial hospital outpatient visits (measured in dollars) decreased initially, visits became more intensive at some point between 4 and 12 months after the storm; thus, the overall effect was near zero.
Inpatient expenditures per enrollee show moderate but insignificant increases after the hurricane, over both the short and long run. Nursing home expenditures show very little short-term effect but a fairly large long-term decrease. Prescription drug expenditures show constant small increases after the hurricane (1%) that persist in every period reported; only the long-term model shows a significant increase in monthly spending per enrollee ($1.53–$1.65).
Because of the dramatic changes that occurred in these 14 North Carolina counties within a short time, we examined use and costs on a weekly basis to detect changes during early recovery stages (results not reported). Because the major impact of the storm was extensive flooding, we hypothesized that use would initially decrease but then gradually increase as roads opened up and facilities recovered.
Surprisingly, we found virtually no change in ER admissions during the first 4 weeks after the storm. However, consistent with results reported earlier, there was a 4% to 7% increase in ER visits over the first 11 weeks in affected counties.
Inpatient admissions show an initial decrease of 5.2 admissions per 10 000 enrollees (8%) during the week of the storm but otherwise show little response to the storm. Nursing home admissions show small increases, the largest increase (3.4 additional admissions per 1000 enrollees) occurring during the week after the storm, but a moderate long-term increase as well. The numbers of inpatient and nursing home days per enrollee show patterns similar to those of admissions.
Finally, we examined the effect of the hurricane on drug prescriptions financed by Medicaid. We found a large decrease of 4 fewer prescriptions filled per 100 enrollees per month (13%) during the week of the hurricane and significant declines in the following 3 weeks. At 10 weeks after the storm, there remained a significant decrease in the average number of prescriptions filled. Comparison of this decrease with the small increase in prescription drug spending during that same period indicates that filled prescriptions were more expensive than average. This finding could be owing to a decrease in the number of prescriptions filled for older, less expensive medications (perhaps more available through such temporary sources as the Red Cross or donated samples) or to an increase in the length of prescriptions (e.g., a 30-day vs a 15-day supply of medication).
DISCUSSION
Disasters can have profound effects on the use of health services over both the short and long term. These effects may be more pronounced for vulnerable populations who, even during good times, experience access problems. The direction of these effects is not obvious; providers and consumers may experience different consequences.
In this report, we explored the behavior of a large, vulnerable population group, Medicaid enrollees. We sought to learn how Medicaid use changes following a natural catastrophe. We hypothesized that individuals and families previously ineligible for Medicaid would become eligible and initiate enrollment. We expected that flooding and physical dislocation would lead to substantial shocks to both the demand and supply of health care services through increases in injuries, disease outbreaks, psychological trauma, transportation difficulties for providers and patients, and the presence of temporary substitute services. Because the health impact of natural disasters may be broad, we examined use without regard to diagnoses or procedures.6,11
We found a modest impact on use of health services, especially in the short run. Increased Medicaid enrollment did not occur. This non-increase could be an artifact of out-migration from affected counties by the general population, which would affect the interpretation of this finding. We observed substantial short-term increases in emergency care and hospital-based outpatient care. Special hurricane-initiated health services and charity care not represented in Medicaid data may account for some of the lack of service use increase. In addition, the presence of individuals unaffected by the storm but residing in affected counties could dampen the results. Furthermore, because of logistical problems, state agencies may have been unable to implement enrollment initiatives after the hurricane.
Perhaps most significantly, we found that the hurricane had substantial long-term consequences for health care use. The $7.14 increase in total monthly Medicaid expenditures indicates a more than $13.3 million increase in state and federal expenditures resulting from the hurricane in affected counties. Whereas the percentage of enrollees actually using services remained at normal levels, significant increases in ER, outpatient, and pharmacy use were observed 1 year after the storm.
Although data are unavailable on health services not financed through Medicaid, our findings suggest that individuals in hurricane-ravaged counties experienced substantial changes in patterns of care compared with their counterparts in other counties. This result held regardless of whether we compared use in severely affected counties with use in all other counties or only in unaffected counties. Overall, we found that the magnitude of effects increased in almost all models when comparisons were made with the smaller, more homogeneous set of controls.
Flood victims probably acted according to their own “hierarchy of needs”; whereas emergency and hospital outpatient visits increased for acute conditions, other health needs perceived as less urgent may have been given lower priority than, for example, finding shelter. Many health services were inaccessible owing to flooding and the inability of staff and patients to reach facilities. Although we cannot draw conclusions about population health outcomes, results from 1 year after the hurricane indicate moderate increases in health service use among Medicaid enrollees.
Acknowledgments
We gratefully acknowledge the financial support and assistance of the North Carolina Department of Health and Human Services Division of Medical Assistance.
We thank Will Dow, Edward Norton, and the participants of the University of North Carolina’s Seminar on Health Services Research in Low Income Populations and Seminar on Health Services Research for useful comments.
Human Participant Protection
The University of North Carolina School of Public Health institutional review board has exempted this work, owing to the secondary nature of the data used and the lack of personal identifiers.
Note. The staff at the Department of Health Policy and Administration of the University of North Carolina School of Public Health created this report with North Carolina Medicaid data. The Division of Medical Assistance has not reviewed this report and therefore cannot validate the accuracy of the information it contains.
Contributors
M. E. Domino and B. Fried planned the study and wrote the Results section. M. E. Domino oversaw the data management and conducted the econometric analyses. Y. Moon and J. Yoon conducted literature reviews and contributed to the design of the study and the writing of the article. J. Olinick contributed to the design of the study, did all the programming, created the analytic file, and contributed to the writing of the article.
Peer Reviewed
References
- 1.Attia MW. The blizzard of 1996: a pediatric emergency department. Prehosp Emerg Care. 1998;2:285–288. [DOI] [PubMed] [Google Scholar]
- 2.Axelrod C, Killam PP, Gaston MH, Stinson N. Primary healthcare and the Midwest flood disaster. Public Health Rep. 1994;109:601–605. [PMC free article] [PubMed] [Google Scholar]
- 3.Brewer RD, Morris PD, Cole TB. Hurricanerelated emergency department visits in an inland area: an analysis of the public health impact of Hurricane Hugo in North Carolina. Ann Emerg Med. 1994;23:731–736. [DOI] [PubMed] [Google Scholar]
- 4.Noji EK, Toole MJ. The historical development of public health responses to disaster. Disasters. 1997;21:366–376. [DOI] [PubMed] [Google Scholar]
- 5.Pointer JE, Michaelis J, Saunders C, et al. The 1989 Loma Prieta earthquake: impact on hospital patient care. Ann Emerg Med. 1992;21:1228–1233. [DOI] [PubMed] [Google Scholar]
- 6.Salinas C, Salinas C, Kurata J. The effects of the Northridge earthquake on the pattern of emergency department care. Am J Emerg Med. 1998;16:254–256. [DOI] [PubMed] [Google Scholar]
- 7.Alson R, Alexander D, Leonard RB, Stringer LW. Analysis of medical treatment at a field hospital following Hurricane Andrew, 1992. Ann Emerg Med. 1993;22:1721–1728. [DOI] [PubMed] [Google Scholar]
- 8.Campanella N. Infectious disease and natural disasters: the effects of Hurricane Mitch over Villanueva municipal area, Nicaragua. Public Health Rev. 1999;27:311–319. [PubMed] [Google Scholar]
- 9.The Health Effects of Floods: The Easter 1998 Floods in England. London, England: Middlesex University, Flood Hazard Research Centre; 1999.
- 10.Ohl CA, Tapsell S. Flooding and human health. BMJ. 2000;321:1167–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bennet G. Bristol floods 1968: controlled survey of effects on health of local community disaster. Br Med J. 1970;3:454–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abrahams MJ, Price J, Whitlock FA, Williams G. The Brisbane floods, January 1974: their impact on health. Med J Aust. 1976;2:936–939. [DOI] [PubMed] [Google Scholar]
- 13.Floyd by the numbers. North Carolina Redevelopment Center. Available at: http://www.ncredevelopment.org/floydoverview.html. Accessed April 8, 2003.
- 14.FEMA Situation Report #82. Raleigh, NC: Federal Emergency Management Agency; 2000.
- 15.FEMA Situation Report #80. Raleigh, NC: Federal Emergency Management Agency; 2000.
- 16.FEMA Situation Report #8. Raleigh, NC: Federal Emergency Management Agency; 1999.
- 17.Wilson K, Maiolo JR, Whitehead JC, et al. Economic Impact Assessment of Hurricane Floyd for North Carolina. Washington, DC: Economic Development Administration; 2000.
- 18.Franklin JA, Wiese W, Meredith JT, et al. Hurricane Floyd: response of the Pitt County medical community. N C Med J. 2000;61:384–389. [PubMed] [Google Scholar]
- 19.Booker SM. Evaluating Floyd’s effect on health in eastern North Carolina [letter]. Environ Health Perspect. 2000;108:A67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Curry MD, Mansfield CJ, Leonardo KD. Health and social problems of a primary care clinic population after a disaster: the Hurricane Floyd flood. N C Med J. 2000;62:99–102. [PubMed] [Google Scholar]
- 21.Wooldridge JM. Introductory Economics: A Modern Approach. Manson, Ohio: South-Western College Publishing; 2000.