Abstract
Objectives. The authors sought to determine the effects of cold-weather periods on budgets and nutritional outcomes among poor American families.
Methods. The Consumer Expenditure Survey was used to track expenditures on food and home fuels, and the Third National Health and Nutrition Examination Survey was used to track calorie consumption, dietary quality, vitamin deficiencies, and anemia.
Results. Both poor and richer families increased fuel expenditures in response to unusually cold weather. Poor families reduced food expenditures by roughly the same amount as their increase in fuel expenditures, whereas richer families increased food expenditures.
Conclusions. Poor parents and their children spend less on and eat less food during cold-weather budgetary shocks. Existing social programs fail to buffer against these shocks.
In many parts of the United States, winters can impose a financial burden. Newspaper reports suggest that poor families are hardest hit. Such families face difficult decisions about where to place their resources, being forced to choose among heating their homes, feeding themselves, and feeding their children. For example, a 2001 article published in the New York Times1 reported that parents reduce expenditures on utilities to pay for food. One family reported that “we owe $800 on the water bill and $500 for heat.” These tough choices may have a large effect on the nutritional well-being of children. Some of the harm will be tempered if parents can shield their children from nutritional deprivation. The same newspaper article also reported that some poor parents “routinely go without dinner to make sure their . . . children have enough to eat.”
The purpose of this study was to investigate whether poor American families have lower food expenditures and worse nutritional outcomes than richer families during cold-weather periods and to determine the extent to which parents are able to protect their children from these shocks. We used 2 large and nationally representative data sets. The Consumer Expenditure Survey (CEX), administered by the US Bureau of Labor Statistics, includes extensive information regarding household expenditures on food and other items over a long time period. The third National Health and Nutrition Examination Survey (NHANES III) is the gold standard for nationally representative nutritional data.
Actual starvation is rare in the United States, but poor nutritional choices are rampant. American children consume diets that are high in fat, high in sweets, and low in fruit and vegetables.2 Few studies have revealed vitamin intake deficiencies in American children3,4; however, Bhattacharya and Currie2 found high prevalence rates of anemia and of high blood cholesterol and some evidence of serum vitamin deficiencies among American adolescents.
Whereas low serum vitamin levels are clinically difficult to evaluate in the context of a single patient, they are good measures of dietary inadequacy in broad populations. The relationship between micronutrient intake and blood levels of these nutrients is complicated. Because the body can store certain vitamins and minerals for long periods, it is not anomalous to find an individual who has not recently consumed the recommended amount of a particular vitamin and yet does not have a deficiency in that vitamin according to blood tests. For example, it can take between 3 and 6 years for a deficiency in vitamin B12 to become clinically evident.4 Nevertheless, blood tests, when properly interpreted, can provide objective evidence of micronutrient malnutrition.
Although poor diets seldom result in classic vitamin deficiencies related to diseases such as scurvy or pellagra, low vitamin and mineral levels could have long-term health consequences. For example, even mild iron deficiency is associated with fatigue, shortened attention span, decreased work capacity, reduced resistance to infection, and impaired intellectual performance.5
Several recent studies have examined whether poor children consume inadequate diets during the winter. Frank et al.6 reported increases in the percentage of emergency room visits among small-for-age children during winter in a Boston hospital. However, relying on British data, Lawlor et al.7 and Shah and Peacock8 did not find any relation between excess winter mortality and deprivation.
Economists have examined nutritional resource sharing in poor families. Wilde9 and Wilde and Ranney10 examined whether poor families receiving Food Stamp benefits eat less toward the end of a benefit month. They found that adults frequently eat less during the fourth week of a month, whereas children exhibit smooth food consumption patterns throughout the month. These results suggest that the food consumption of poor families is potentially vulnerable to financial strains but that parents in poor families can, to some extent, protect their children from the adverse effects of these strains.
METHODS
Sample and Procedures
To measure patterns of expenditures on food and home fuel, we used data from the 1980 though 1998 versions of the CEX. In this survey, each household reports up to 12 months of expenditure data as well as demographic, geographic, and income information. The CEX collects information from roughly 5000 households each month; our final sample comprised 104 747 households. Survey weights are provided so that the CEX sample is nationally representative within any given month.
We obtained data from the National Oceanic and Atmospheric Administration on mean ground temperatures for each state and each month between 1980 and 1998. We merged these data with the CEX data, using information on each family’s state of residence. With our large sample, we were able to examine differential changes in spending patterns at the household level. However, we were not able to use the CEX to infer consumption patterns of individual household members.
NHANES III, administered by the Centers for Disease Control and Prevention between 1988 and 1994, provides information on nutritional well-being at the individual level. This survey collected data from 33 994 people over 89 locations, using a roving, mobile examination center. NHANES III combines demographic information, data from a standard clinical examination conducted by doctors (including blood tests), and questions about dietary intakes.
Measures
We derived from the CEX data monthly expenditure measures in 4 different categories: food consumed in the home, food consumed outside of the home, clothing, and home fuel. The food consumed in the home measure included expenditures on all meals prepared at home, including picnics. Food consumed outside of the home included expenditures at restaurants, cafes, fast food establishments, and catered affairs; school and boarding house meals; and meals received as pay. Subsidized meals (such as free school breakfasts) are not captured in the CEX measure of food expenditure; we excluded expenditures on alcoholic beverages or tobacco from both measures of food.
The home fuel measure included expenditures on 6 fuels (heating oil, electricity, natural gas, coal, kerosene, and firewood) at primary residences. To account for inflation, we applied the Consumer Price Index deflator so that all expenditures would be measured in constant 1982 to 1984 dollars.
We used 3 conceptually different measures of nutrition on the basis of the NHANES III data: calorie intake, dietary quality, and serum assessments of vitamin and mineral deficiencies. The first 2 measures were based on 24-hour dietary recall information included in NHANES III. In the case of most children younger than 12 years and all children younger than 6 years, parents or guardians supplied dietary information.
On the basis of these responses, NHANES III provides an estimate of total daily calorie intake and a dietary quality measure: the Health Eating Index. The Health Eating Index, which was developed by the US Department of Agriculture, summarizes how closely a diet meets the department’s recommendations.11 Diets that feature fruits, vegetables, meat, and dairy products in the appropriate proportions receive higher Health Eating Index scores, whereas diets that feature high levels of saturated and total fat and cholesterol receive lower scores. Intakes in 10 different categories are measured on a scale of 0 to 10 (with 10 representing a good score) and summed into a total score ranging from 0 to 100. A 2-point score change can reflect, for example, an extra daily serving of vegetables or a 3-percentage-point decrease in the proportion of calories derived from fat.
We used age-specific normal values from standard pediatric and internal medicine textbooks to define inadequate serum levels of vitamins and minerals.12,13 We considered serum levels of vitamins A, C, and E. Because serum iron correlates poorly with inadequate body stores of iron, we used hematocrit and hemoglobin levels to diagnose anemia.
Data Analysis
Because the 2 data sets we examined are structured differently, they required distinct but closely related analyses. In the CEX the unit of observation is the family, whereas in NHANES III the unit of observation is the individual, although family relations are reported. For the CEX, we directly ascertained state of residence; thus, matching temperature data were available for each family during each month of observation. For NHANES III, the only publicly available geographic data were the census region of the respondent (South, West, Midwest, or Northeast) and whether the respondent resided in a large city; thus, we were unable to link temperature information. However, we had data on the month in which the interview was conducted and could infer the season during which the respondent was surveyed.
In the CEX analysis, our strategy was to examine the ways in which expenditures on food, clothing, and home fuel changed in unseasonably cold or warm months. Because changes in expenditures over the course of a year on the part of richer families are presumably not due to resource constraints, we used these families as a comparison group for the poor families.
We constructed a separate multivariate model of log expenditures for each of the 4 expenditure categories. Explanatory variables in these models included temperature, 3 income categories (high-income quartile, middle 2 quartiles, and low-income quartile), and the interaction of temperature with income.
We included dummy variables for each year and each state, effectively “de-trending” expenditures separately for each state. We also included dummy variables for each month to allow for seasonal expenditure patterns. After inclusion of all of these dummy variables, we were left with variations in expenditures due to unseasonably cold and warm months. We emphasize that by including these dummy variables, we were no longer simply comparing outcomes occurring in warm months with those occurring in cold months. Instead, we were comparing specific months—for instance, unusually cold Januarys with average Januarys.
As a sensitivity check, we also estimated similar models (not presented here) with no dummy variables for state, month, or year, and we found similar results. Throughout, we used sample weights in model estimations. Using the estimates from the multivariate models, we predicted expenditure changes resulting from an unseasonable 10°F (5.6°C) drop in temperature for poor and richer families separately. These predictions were nonparametric retransformations of the regression estimates arrived at through use of the Duan smearing technique.14
In our NHANES III analysis, we used a similar strategy, but instead of relying on outcome changes related to temperature changes, we relied on outcome changes across summer and winter. To make these nutritional comparisons, we constructed linear multivariate models for each nutritional outcome, estimating separate models for children and adults. We used the same set of explanatory variables in each model. In addition to the key independent variables (whether a family was poor, whether the interview took place during the winter, and the interaction of these 2 variables), these explanatory variables included age, age squared, and dummy variables indicating the respondent’s region of residence (South, West, Midwest, or Northeast) and whether the respondent lived in an urban area (a census-defined standard metropolitan statistical area), and interactions between these sets of dummy variables.
Using the estimated coefficients derived from the multivariate models, we predicted changes in nutritional outcomes between summer and winter for a reference richer person and a reference poor person. We relied on the multivariate model to assess statistical significance. Again, we used sample weights in all model estimations.
RESULTS
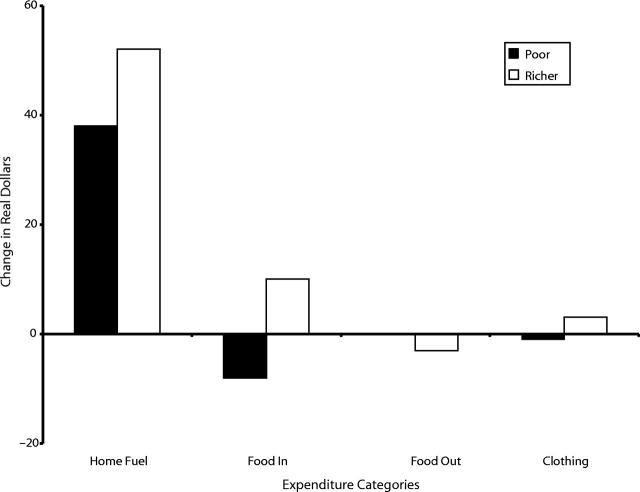
Figure 1 ▶ reports changes in expenditures resulting from a 10°F drop in temperature for the 4 expenditure categories separately for richer and poor families. These predictions were based on the multivariate analysis of the CEX data. In this figure, increases in expenditures during periods of colder temperature are represented with positive bars, whereas decreases are represented with negative bars. All differences between expenditures made by poor and richer families within categories were statistically significant at the .01 α level. As one might expect, expenditures on home fuel increased for both poor and richer families in unusually cold months. Richer families increased their home fuel expenditures more than did poor families ($53 vs $37 per month in 1982–1984 dollars).
FIGURE 1—
Changes in expenditures by category and by income in response to an unseasonable 10°F drop in temperature.
Expenditures on food in the home decreased during cold months among poor families but not among richer families. A 10°F drop in temperature was associated with a $9 per month decrease in such expenditures among poor families, versus an $11 per month increase among richer families. This decrease in food expenditures on the part of poor families was not offset by increased expenditures on food outside the home or on clothing. On the contrary, cold-weather shocks were associated with only small changes in expenditures on clothing and food away from home in both types of families. The difference between richer and poor families in these categories, although statistically significant, was also small.
Poor families spent a larger portion of their income on food than did richer families. Poor families spent 29.5% of their budget on food in the home, as compared to 22.5% among richer families. Expenditures on food outside of the home constituted a much smaller portion of budgets among both poor and richer families (5.3% vs 7.1%). Hence, the net effect of cold-weather months on food expenditures, both in and out of the home, was greatest among the poor.
Home fuel expenditures represented 12.3% of budgets among poor families and 9.7% of budgets among richer families. In effect, the $37 increase in home fuel expenditures observed among poor families during unusually cold months had a greater potential impact on the family budget than did the $53 increase among richer families, because the $37 increase represented a larger share of poor families’ total budgets.
Because the South is typically warmer in the winter than other parts of the country, a winter temperature drop there can have different effects on family budgets than in other parts of the country. Consequently, we also analyzed southern households separately from other households. Southern households did not increase their fuel expenditures in colder months as much as nonsouthern households did (in models with noninteracting region, month, and year dummies), perhaps because winter temperatures are higher in the South.
On the other hand, we found larger increases in fuel expenditures in the South when we focused on unusual changes in temperature (in models with interacting region and month dummies and year dummies), although there were no changes in food expenditures among poor families. That unusual temperature drops can have larger effects on fuel expenditures in the South is not surprising, given that homes there are less likely to have insulation (US Department of Energy recommendations on amount and type of insulation are available at http://www.eren.doe.gov/consumerinfo/energy_savers/insulation.html). We conclude that “heat or eat” choices for the poor are not observable in the South but are observable elsewhere.
Table 1 ▶ reports predicted changes in nutritional outcomes between summer and winter on the basis of our analysis of NHANES III. Because the unit of analysis in NHANES III was the individual, we estimated separate models for children, for adults, and for adults with children. As before, we compared outcomes occurring in poor families with those occurring in richer families.
TABLE 1—
Estimates of Differences in Winter and Summer Nutritional Outcomes
| Poor Familiesa | Richer Familiesb | |||||
| Group and Nutritional Outcome | Summer | Winter | Difference | Summer | Winter | Difference |
| All adults (n =4808) | ||||||
| Dietary qualityc | 59.8 | 60.1 | 0.3 | 64.3 | 64.9 | 0.6 |
| Serum measures | ||||||
| Anemia | 0.081 | 0.097 | 0.016 | 0.076 | 0.091 | 0.015 |
| Low A, C, or E | 0.242 | 0.268 | 0.026 | 0.087 | 0.130 | 0.043* |
| Calories | 1858 | 1711 | −147* | 1847 | 1841 | −6 |
| Adults with children (n = 1994) | ||||||
| Dietary qualityc | 55.3 | 55.4 | 0.1 | 59.9 | 60.8 | 0.9 |
| Serum measures | ||||||
| Anemia | 0.072 | 0.085 | 0.013 | 0.056 | 0.077 | 0.021 |
| Low A, C, or E | 0.191 | 0.251 | 0.061 | 0.027 | 0.093 | 0.067 |
| Calories | 2072 | 1831 | −241* | 1998 | 1973 | −26 |
| Children (n = 3779) | ||||||
| Dietary qualityc | 64.2 | 63.3 | −1.0 | 67.2 | 64.9 | −2.3* |
| Serum measures | ||||||
| Anemia | 0.000 | 0.021 | 0.021 | 0.001 | 0.025 | 0.024 |
| Low A, C, or E | 0.097 | 0.133 | 0.037 | 0.051 | 0.058 | 0.007 |
| Calories | 1807 | 1611 | −197** | 1719 | 1713 | −7 |
Note. These outcomes are based on a regression analysis of third National Health and Nutrition Examination Survey (NHANES III) data in which we estimated separate models for each outcome and age (children and adults). In addition to the key independent variables of income levels and season of interview, the regressions included race/ethnicity dummies, age, age squared, eight region dummies, and a dummy variable for sex. Values were the predicted outcomes for a standardized person (a White female from the urban Northeast); the age of the child was 8 years, and the age of the adult was 35 years. The statistical tests were based on the coefficients of the regression. The only statistically significant difference between adults and children was for richer families in dietary quality.
aPoor families have a poverty–income ratio less than 1.5.
bRicher families have a poverty–income ratio greater than 3.
cDietary quality was measured via the Health Eating Index (on a scale ranging from 0 to 100); see the text for an explanation.
*P < .05; **P < .01.
Poor nutrition was more prevalent among poor families than among richer families. Adults with children and children in poor families exhibited lower levels of dietary quality, higher levels of serum vitamin deficiencies, and lower calorie intakes (in winter only) than did their counterparts in richer families.
The winter resource shift induced statistically significant reductions in caloric intake among both children and adults in poor families. Adults consumed 147 fewer calories during the winter than during the summer (a 7.9% decline), adults with children consumed 241 fewer calories (an 11.6% decline), and poor children consumed 197 fewer calories (a 10.9% decline). Increases in prevalence rates of vitamin deficiencies and anemia were observed during the winter for children and for adults with children, but these increases were not statistically significant.
Children in richer families had worse diets during the winter than during the summer but showed no differences in serum measures. Richer adults (but not richer adults with children) were more likely to have low serum levels of vitamins A, C, and E in the winter but exhibited no changes in dietary quality. Richer adults and children consumed higher-quality diets and were less likely to have serum vitamin deficiencies than their poor counterparts. There were no other statistically significant differences in nutritional outcomes between summer and winter among richer families. Unlike poor families, richer families exhibited no changes in caloric intake. The differences found for richer families do not suggest a “heat or eat” phenomenon, because these families increased their expenditures on food in the winter.
When we used summer–winter differences among richer families as a control category for poor families, statistical tests demonstrated that only winter caloric-intake declines were significantly different between members of poor and richer families (P < .05 for adults, P < .05 for adults with children, and P < .01 for children). Richer and poor families did not differ significantly on any other summer–winter outcomes, including dietary quality changes among children and vitamin deficiencies among adults.
To test the sensitivity of our NHANES III results to smaller changes in temperature, we also conducted analyses comparing outcomes in the spring and fall separately against winter outcomes. Poor adults consumed 118 fewer calories in the winter than in the spring and 97 fewer calories in the winter than in the fall. Poor children consumed 145 fewer calories in the winter than in the spring. Among richer families, adults consumed 236 fewer calories in the winter than in the fall, whereas children’s diets were 2.0 and 2.4 Health Eating Index points worse in the winter than in the fall and spring, respectively. There were no other statistically significant outcomes. This pattern of results is qualitatively similar to the summer–winter results reported in Table 1 ▶.
Finally, we estimated the outcomes described in Table 1 ▶ separately for each census statistical region included in NHANES III. We found no statistically significant differences in NHANES III outcomes in terms of the effect of winter among these regions. Contrary to our findings in the CEX analysis, the South was not shown to differ in a statistically significant way from other regions. However, this result should be interpreted with caution, in that NHANES III sample sizes were too small to definitively answer questions about summer–winter differences between richer and poor families separately for each region.
DISCUSSION
We investigated how well poor American families protect themselves against nutritional risks due to budget shocks resulting from cold weather. We found that poor families reduced their expenditures on food in response to unusually cold weather, whereas richer families did not. Among poor families, we estimated that a monthly temperature that was 10°F colder than normal would result in a reduction in expenditures on food in the home of $11 per month and an increase in fuel expenditures of $37 per month. In poor households, adults and children alike reduced their caloric intake by 10% during the winter months, whereas members of richer families did not reduce their caloric intake during the winter.
It is striking that these nutritional outcomes corresponded so closely with expenditure outcomes. The close correspondence between the CEX and NHANES III results for poor and richer families lends support to our findings.
Our results suggest that poor American families face stark choices in cold weather. In particular, they increase their home fuel expenditures at the cost of expenditures on food and nutritional well-being. Our evidence also suggests that poor parents are only imperfectly able to protect their children from cold-weather resource shocks. Both children and adults reduce their caloric intake during winter months.
Given the importance of food to well-being, it seems likely that families, if they have access to short-term credit or to savings, borrow or dip into savings to pay for high winter fuel needs rather than reduce their food expenditures. Our results indicate that poor families probably do not have access to such resources. Indeed, nearly 25% of American families with incomes below $25 600 (approximately 1.5 times the federal poverty line for a family of 4 in 2000) have neither savings nor checking accounts.15
There are at least 2 alternative explanations for our findings. The first is enrollment by poor children in school meal programs during the school year. This explanation cannot account for the decrease in caloric intake during the winter among children, nor can it explain the decrease in expenditures during “unseasonably” cold months. To investigate this explanation further, we conducted an additional analysis with the CEX data, restricting the sample to families with below-school-aged children only. In this subsample, we found similar declines in food expenditures and increases in home fuel expenditures during cold months (poor families increased their fuel expenditure by $10.40 and reduced their food expenditure by $6.60 in response to an unusually cold month; richer families increased their fuel expenditure by $15.60 but did not reduce their food expenditure). Because below-school-aged children are presumably not enrolled in school lunch programs, these programs cannot explain the observed expenditure patterns.
A second alternative explanation for our results is that nutritious food, such as fresh fruits and vegetables, is cheaper and more readily available in the summer. Such an explanation might account for declining dietary quality in winter months, especially among poor families that cannot afford the expense of high-quality winter diets. However, this explanation is inconsistent with a decline in food expenditures in cold months. A basic economic principle is that expenditures on a product increase with price only as long as demand is relatively unresponsive to price.16 Researchers consistently find that demand for food is relatively unresponsive to price (for a recent US estimate, see van Driel et al.17). Thus, if the price of highquality food rises in the winter, expenditures should also increase. As a consequence, our finding that food expenditures decrease in the winter is inconsistent with this alternative explanation.
Our results should be considered in the context of another public health problem: increasing obesity, especially among the poor (see Popkin and Doak18 and Flegal19 for reviews of national and international trends in obesity; see James et al.20 and Olson21 for discussions of the relationships among poverty, nutrition, and obesity). In this context, it is unclear whether declines in calorie intakes should be seen as an unmitigated disaster, especially in that these declines are not accompanied by changes in dietary quality, serum vitamin deficiency, or anemia rates. However, even if calorie intake declines might be viewed favorably, seasonal cycles in calorie intake, which is what our results imply, may not have the same positive or even desirable health consequences as might caloric restrictions among the obese.
Finally, many social programs are meant to help poor families endure detrimental economic events, including the Food Stamp program, school meal programs, and long-term repayment plans offered by utility companies. Our results suggest that existing social programs are insufficient to buffer poor families from cold-weather shocks to their budgets.
Acknowledgments
We thank the Joint Center for Poverty Research and the Institute for Research on Poverty for financial support of this project.
Seminar participants at the University of Chicago, the University of Wisconsin, the National Bureau of Economic Research at Stanford University, the Midwestern Economics Association, and the Western Economics Association provided helpful feedback and suggestions. We thank Alison Jacknowitz and William Clune for expert research assistance.
Human Participant Protection
The data used for this project are available publicly from the National Center for Health Statistics and the Bureau of Labor Statistics. We obtained ethical clearance for the study from the institutional review board at RAND.
Contributors
All authors participated substantially in generating the ideas expressed in this article and in drafting, revising, and editing the article. J. Bhattacharya and S. Haider did much of the work on the NHANES III data; T. DeLeire and J. Bhattacharya did much of the work on the CEX data. All of the authors participated substantially in interpreting the results of the NHANES III and CEX data analyses.
Peer Reviewed
References
- 1.Becker E. Millions eligible for Food Stamps aren’t applying. New York Times. February 26, 2001:A1.
- 2.Bhattacharya J, Currie J. Youths at nutritional risk: misnourished or malnourished? In: Gruber J, ed. Risky Behavior Among Youths. Chicago, Ill: University of Chicago Press; 2001:483–521.
- 3.Devaney BL, Gordon AR, Burghardt JA. Dietary intakes of students. Am J Clin Nutr. 1995;61(suppl 1):205S–212S. [DOI] [PubMed] [Google Scholar]
- 4.Middleman AB, Emans SJ, Cox J. Nutritional vitamin B12 deficiency and folate deficiency in an adolescent patient presenting with anemia, weight loss, and poor school performance. J Adolesc Health. 1996;19:76–79. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Guidelines for school health programs to promote lifelong healthy eating. MMWR Recomm Rep. 1996;45(RR-9):1–41. [PubMed] [Google Scholar]
- 6.Frank DA, Roos N, Meyers A, et al. Seasonal variation in weight-for-age in a pediatric emergency room. Public Health Rep. 1996;111:366–371. [PMC free article] [PubMed] [Google Scholar]
- 7.Lawlor DA, Harvey D, Dews HG. Investigation of the association between excess winter mortality and socio-economic deprivation. J Public Health Med. 2000;22:176–181. [DOI] [PubMed] [Google Scholar]
- 8.Shah S, Peacock J. Deprivation and excess winter mortality. J Epidemiol Community Health. 1999;53:499–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilde P. A monthly cycle in food use by Food Stamp recipients. Paper presented at: Board of Children, Youth and Families Research Briefing, May 1997, Ithaca, NY.
- 10.Wilde P, Ranney C. A Monthly Cycle in Food Expenditure and Intake by Participants in the US Food Stamp Program. Ithaca, NY: Cornell University, Dept of Agricultural, Resource, and Managerial Economics; 1997. Working paper 97-04.
- 11.Kennedy E, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: design and applications. J Am Diet Assoc. 1995;95:1103–1108. [DOI] [PubMed] [Google Scholar]
- 12.DeAngelis CD, Feigin RD, Warshaw JB, McMillan JA. Oski’s Pediatrics: Principles and Practice. 3rd ed. Philadelphia, Pa: Williams & Wilkins; 1999.
- 13.Wilson JD, Braunwald E, Isselbacher KJ, et al., eds. Harrison’s Principles of Internal Medicine. New York, NY: McGraw-Hill Book Co; 1991.
- 14.Duan N. Smearing estimate: a nonparametric retransformation method. J Am Stat Assoc. 1983;78:605–610. [Google Scholar]
- 15.Hogarth JM, O’Donnell KH. Banking relationships of lower-income families and the governmental trend toward electronic payment. Federal Reserve Bull. July1999:459–470.
- 16.Nicholson W. Microeconomic Theory: Basic Principles and Extensions. New York, NY: Dryden Press; 2000.
- 17.van Driel H, Nadall V, Zeelenberg K. The demand for food in the United States and the Netherlands: a systems approach with the CBS model. J Appl Econometrics. 1997;12:509–523. [Google Scholar]
- 18.Popkin BM, Doak CM. The obesity epidemic is a worldwide phenomenon. Nutr Rev. 1998;56:106–114. [DOI] [PubMed] [Google Scholar]
- 19.Flegal KM. Trends in body weight and overweight in the US population. Nutr Rev. 1996;54:S97–S100. [DOI] [PubMed] [Google Scholar]
- 20.James WP, Nelson M, Ralph A, Leather S. Socioeconomic determinants of health: the contribution of nutrition to inequalities in health. BMJ. 1997;314:1545–1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olson CM. Nutrition and health outcomes associated with food insecurity and hunger. J Nutr. 1999;129(suppl 2):521S–524S. [DOI] [PubMed] [Google Scholar]