The Baby-Friendly Hospital Initiative (BFHI) is based on the Ten Steps to Successful Breast-Feeding, a program which summarize the practices that maternity wards need to adopt to support breastfeeding.1 There are more than 16 000 Baby-Friendly Hospitals throughout the world, and of these, more than 200 are located in Brazil.
Despite the abundance of studies evaluating each of the 10 steps or a combination of them, information on the impact of BFHI on the duration of breastfeeding is limited. Recently, a large randomized controlled trial including 31 hospitals in Belarus showed that an intervention based on BFHI principles increased breastfeeding rates, especially exclusive breastfeeding.2 The present study reproduced these results using a less complex study design.
METHODS
This before-and-after observational study prospectively followed 2 cohorts of babies born at Hospital de Clínicas de Porto Alegre, Brazil, a general university hospital responsible for approximately 4000 births per year. Most of the population served by the hospital comes from a low socioeconomic stratum.
The first cohort was formed of a sample of 187 babies born in 1994. The second cohort included 250 babies born in 1999, 2 years after BFHI implementation. In both cohorts, all babies born after the starting date of the studies were included, provided they fulfilled the criteria of being healthy nontwins, with birthweight of 2500 g or greater, who had initiated breastfeeding, and whose mothers lived in Porto Alegre. Newborns or mothers who presented any health problem that could make breastfeeding more difficult or impossible were excluded from the study (for example, HIV–positive mothers, children with malformations, and children requiring intensive care).
After giving informed consent, mothers were interviewed at the maternity ward and in their homes at the end of the first, second, fourth, and sixth months postpartum. In the 1999 cohort, the second- and fourth-month visits were replaced with telephone interviews whenever possible. Mothers were asked about the usual diet of the children and the time of introduction of any food. Babies receiving only breast milk, with no other liquid or solid, were considered to be receiving exclusive breastfeeding; those receiving breast milk, regardless of supplements, were considered to be receiving breastfeeding.3
The data were analyzed using Epi Info software 6.04b (Centers for Disease Control and Prevention, Atlanta, Ga) and the statistical package SPSS 10.0 for Windows (SPSS Inc, Chicago, Ill). Kaplan–Meyer survival curves of breastfeeding and exclusive breastfeeding were plotted for the 2 cohorts. Cox regression model interaction was used to test the interaction between BFHI implementation and per capita income (lower half vs upper half). The log-rank test was used to calculate the significance level of differences between curves.
The odds for not breastfeeding exclusively at 1 month and discontinuation of any breastfeeding at 4 months among children born before the BFHI, compared with children born after the BFHI, were calculated using Cox regression analysis. The variables included in the model were those whose prevalences differed (P < .2) between the 2 cohorts based on a χ2 test.
RESULTS
In the course of the follow-up of the 1994 and 1999 cohorts, there were losses to the sample of 8.6% and 8.4%, respectively.
Table 1 ▶ shows the characteristics of the 2 cohorts studied. They differed (P < .2) in terms of age and marital status of the mother, sex of the newborn, and per capita family income.
TABLE 1—
Characteristics of the 1994 and 1999 Cohorts Born at Hospital De Clínicas de Porto Alegre, Brazil
| 1994 n = 187, No. (%) | 1999 n = 250, No. (%) | P | |
| Mother’s age ≥ 21 y | 147 (78.6) | 174 (69.6) | .045 |
| Mother’s schooling ≥ 8 y | 91 (48.7) | 126 (50.4) | .729 |
| Per capita income 50% of minimum salary (US $90 per month)a | 158 (84.5) | 174 (73.4) | .008 |
| Mother White | 129 (69.0) | 182 (72.8) | .444 |
| Mother’s first child | 81 (43.3) | 104 (41.6) | .794 |
| Average breastfeeding time of previous children 4 mob | 64 (60.4) | 108 (74.0) | .430 |
| Vaginal birth | 149 (79.7) | 193 (77.2) | .614 |
| Male newborn | 88 (47.1) | 139 (55.6) | .095 |
| Parents legally married | 75 (40.1) | 50 (20.0) | .001 |
| Prenatal care with 5 consultations | 147 (78.6) | 206 (82.4) | .383 |
aThis information was obtained for 237 families in the 1999 study.
bExcluding firstborns (n = 106 in the 1994 cohort and n = 146 in the 1999 cohort).
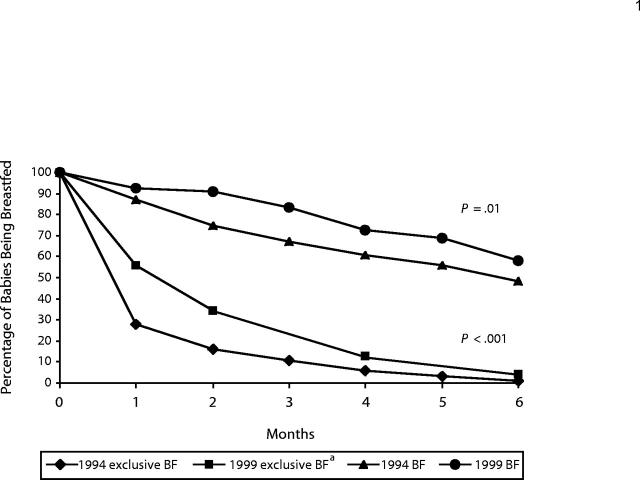
The Kaplan–Meier survival curves of breastfeeding and exclusive breastfeeding presented in Figure 1 ▶ show that those exposed to the BFHI were breastfed significantly longer than those born before the BFHI. The median duration of exclusive breastfeeding was 2 months for children born after the BFHI and 1 month for those born before the BFHI.
FIGURE 1—
Percentage of babies being breastfed and exclusively breastfed: 1994 and 1999.
Note. BF = Breastfeeding.
aData for exclusive breastfeeding not available in the third and fifth months for 1999.
The Cox regression analysis showed that the hazard ratio was 1.66 (95% confidence interval [CI] = 1.40, 1.98) for not breastfeeding exclusively at 1 month and 1.55 (95% CI = 1.16, 2.07) for discontinuation of any breastfeeding at 4 months among children born before the BFHI compared with children born after the BFHI.
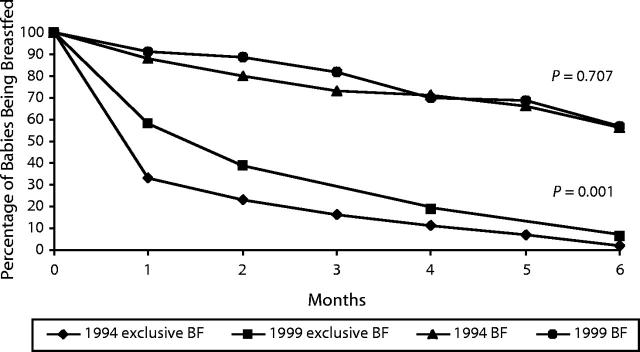
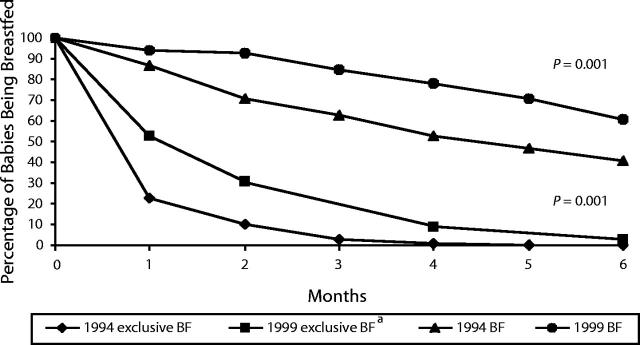
A comparison of the survival curves for breastfeeding according to per capita family income shows that the BFHI was more effective among underprivileged children (interaction term: P = .05). The same was not true for exclusive breastfeeding (interaction term: P = .6) (Figures 1 ▶–3 ▶).
FIGURE 3—
Percentage of babies being breastfed and exclusively breastfed: families with per capita income above median, 1994 and 1999.
Note. BF = Breastfeeding.
DISCUSSION
The present study shows a significant increase in breastfeeding and exclusive breastfeeding rates after BFHI implementation. Of note, the effects of BFHI were stronger in the underprivileged population. The benefits of breast milk are known to be greater in populations at lower socioeconomic levels.4
Despite the occurrence of an increase in breastfeeding rates after BFHI implementation, the frequencies of breastfeeding in the first 6 months of life, especially those of exclusive breastfeeding, are still low. The BFHI in itself appears not to be sufficient to maintain high rates of breastfeeding and exclusive breastfeeding over this period. Interventions made only at 1 moment (such as in the maternity ward) and based solely in hospitals may increase the rates but will have only a short-term effect unless complementary strategies are incorporated.5 Within the BFHI itself, it is possible to obtain more sustainable results through the strengthening of step 10, which seeks the establishment of support groups for mothers who breastfeed after discharge from the maternity ward.
As this study evaluated breastfeeding rates in 2 different periods, it is not possible to conclude that BFHI caused an increase in rates. Because breastfeeding rates in Brazil have gradually increased in the last 20 years, it is possible that a higher national awareness contributed to the increase in rates. Nevertheless, during the time between the 2 cohorts (1994–1999), no other major actions were carried out. Also, a previous study showed that between 1987 and 1994 the rates of breastfeeding in the population under study did not change.6 This reinforces the concept that the BFHI was probably the main factor for the improvement of breastfeeding rates. It is important to mention that Brazil did not experience any substantial change in economics, female employment, or related legislation that could explain the results.
In conclusion, the present study shows a significant increase in breastfeeding rates, especially exclusive breastfeeding, after BFHI implementation. Nonetheless, in order for breastfeeding to become universal, it is necessary to strengthen the BFHI and to develop other interventions aimed at protecting, promoting, and supporting breastfeeding practices.
FIGURE 2—
Percentage of babies being breastfed and exclusively breastfed: families with per capita income below median, 1994 and 1999.
Note. BF = Breastfeeding.
aData for exclusive breastfeeding not available in the third and fifth months for 1999.
Acknowledgments
We are grateful for the financial and editorial support provided by Research Support Fond Hospital de Clínicas de Porto Alegre.
Human Participant Protection
This study was approved by the research and ethics committee of Hospital de Clínicas de Porto Alegre.
Contributors
M. L. G. Braun contributed to the conception and design of the study, collection and analysis of data, and writing of the brief. E. R. J. Giugliani contributed to the conception and design of the study, analysis of data, and writing of the brief. M. E. M. Soares, C. Giugliani, A. P. de Oliveira, and C. M. M. Danelon. contributed to the conception and design of the study and collection of data.
Peer Reviewed
References
- 1.Protecting, Promoting and Supporting Breastfeeding: The Special Role of Maternity Services: A Joint WHO/UNICEF Statement. Geneva, Switzerland: World Health Organization, UNICEP; 1989.
- 2.Kramer MS, Chalmers B, Hodnett ED, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA. 2001;285:413–420. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization, Division of Diarrhoeal and Acute Respiratory Disease Control. Indicators for Assessing Breastfeeding Practices: Report of an Informal Meeting, 11–12 June 1991, Geneva, Switzerland. Geneva: World Health Organization; 1991. WHO/CDD/SER/91.14.
- 4.World Health Organization, Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality. Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: a pooled analysis. Lancet. 2000;355:451–455. [PubMed] [Google Scholar]
- 5.Giugliani ERJ. Increasing Rates of Exclusive Breastfeeding. Technical Consultation on Infant and Child Feeding. Geneva, Switzerland: World Health Organization; 2000.
- 6.Kummer SC, Giugliani ER, Susin LO, et al. Evolution of breastfeeding pattern. Rev Saude Publica. 2000;34:143–148. [DOI] [PubMed] [Google Scholar]