Abstract
Objectives. This study sought to determine whether income inequality, household income, and their interaction are associated with health status.
Methods. Income inequality and area income measures were linked to data on household income and individual characteristics from the 1994 Canadian National Population Health Survey and to data on self-reported health status from the 1994, 1996, and 1998 survey waves.
Results. Income inequality was not associated with health status. Low household income was consistently associated with poor health. The combination of low household income and residence in a metropolitan area with less income inequality was associated with poorer health status than was residence in an area with more income inequality.
Conclusions. Household income, but not income inequality, appears to explain some of the differences in health status among Canadians.
The idea that the distribution of income within a population (i.e., income inequality) could be an important determinant of health has spurred a large and growing research literature.1 Recently, the relationship between income inequality and area-level measures of health status has been called into question.2,3 The early work that reported an inverse relationship between income inequality and life expectancy and a positive relationship between income inequality and mortality across industrialized countries4–7 has been reexamined and its conclusions shown to be a function of sample selection, time period, or data quality.8–10
Research that has examined the relationship between income inequality and area-level measures of health status within countries has generally shown a negative relationship.11–16 Exceptions include 1 study involving Canadian data17 and 2 studies involving American data that controlled for area-level measures of educational attainment or racial concentration.18,19 Controlling for educational attainment and racial concentration may be inappropriate, however, because these area-level attributes could represent pathways through which income inequality affects health.20
Ecological studies have been criticized on both theoretical and methodological grounds.21,22 Most important, the relationship between income inequality and area-level measures of health status can arise from a nonlinear and diminishing relationship between individuals’ income and their health status.23–25 Because area-level data alone cannot fully address this possibility, many researchers have turned to multilevel data.
US studies involving the use of crosssectional designs and multilevel data have consistently revealed a relationship between income inequality and individuals’ health status in regard to a variety of health outcomes at the state or county level26–30 but not at the metropolitan level30; studies conducted in Japan31 and the United Kingdom32 have not revealed such a relationship. Declines in health status may lead to declines in income,33 however, and if such transitions are concentrated geographically, declines in health status could increase income inequality. Studies using cohort designs and multilevel data, which have the potential to account for such sequencing, have produced mixed results when they have examined the relationship between income inequality and individuals’ health status over time in the United States34–38 and have revealed no relationship in Denmark.39
It may be premature, however, to reject the income inequality hypothesis. First, a number of possible reasons have been identified for the mixed results observed in the United States, such as sample selection, differences in income inequality and health measures, misspecification of individuals’ income, and confounder selection.1,3,18 Second, to our knowledge, only 1 study involving the use of a cohort design and multilevel data has been conducted outside the United States.39 Third, even if income inequality does not independently affect health, it may interact with individuals’ income.40
This study extended previous research by examining whether income inequality at the metropolitan level, household income, or the interaction between income inequality and household income is associated with individuals’ health status over a 4-year period in Canada. We examined whether income inequality and average area income are associated with individuals’ health status after control for household income and other relevant confounders and potential pathways. In addition, we examined whether the relationship between income inequality and health status is different among low- and high-income individuals.
We conceptualize income inequality as potentially affecting health status through neomaterialist mechanisms, psychosocial mechanisms, or both.41,42 The neomaterialist explanation hypothesizes that high levels of income inequality could negatively influence health through a systematic underinvestment in and inequity in access to other healthdetermining factors such as education, a clean environment, and health care. The psychosocial explanation hypothesizes that high levels of income inequality could lead to health-damaging reactions such as stress, anxiety, and shame in those who are worse off.
An implication of the neomaterialist mechanism is that Canada’s universal health care system could lessen any relationship between income inequality and health status. The large and growing private health care market (e.g., for noninsured services such as prescription drugs) and regional and socioeconomic inequities in access to health care43,44 suggest that income inequality could still influence health status in Canada through differences among individuals in terms of access to health care.
METHODS
We calculated measures of income inequality and average area income for 53 metropolitan areas with the 1991 Canadian census and linked these measures to individual records from the National Population Health Survey (NPHS).45 The NPHS is a stratified multistage survey that began in 1994 and is repeated every 2 years. It covers household and institutional residents in all provinces and territories, excluding those living in Indian reserves, on Canadian Armed Forces bases, and in some remote regions of Ontario and Quebec. The longitudinal cohort comprises 17 276 randomly selected respondents first interviewed in 1994 or 1995. The follow-up response rate in the second survey (1996–1997) was 90.7% (15 670), and the response rate in the third survey (1998–1999) was 84.6% (14 619) among those who completed the first and second surveys.
Only respondents who completed all 3 waves of the survey were included in the present analysis. Respondents who did not reside in a metropolitan area at baseline (n = 6125) and respondents who moved from their metropolitan area between the 1994 and 1996 surveys (n = 503) were excluded from the analysis; however, respondents who moved from their metropolitan area between the 1996 and 1998 surveys were included. Children and adolescents younger than 18 years (n = 1533) were also excluded, leaving 6456 adults in our study sample.
The dependent variable, self-reported health status, was measured in all 3 surveys. Possible responses were excellent, very good, good, fair, and poor. These responses were coded as a 5-category ordinal variable in which higher numbers represented better health. A second measure of health status, the McMaster Health Utility Index (HUI), was used to test the robustness of the relationship between income inequality and health status. The HUI, which assigns a single value ranging from 0 (death) to 1 (perfect health), is based on 8 dimensions of health: vision, hearing, speech, mobility, dexterity, cognition, emotion, and pain. Details of its construction and validity have been described elsewhere.46
Three independent variables were derived from the 1991 Canadian census. The first was income inequality, defined as the percentage of total household income accruing to the households representing the bottom 50% of the income distribution in a given area; this percentage ranged from 21.59% (most unequal) to 26.55% (most equal). The second variable was average area income, defined as the mean household income in an area; average incomes ranged from $32 700 to $59 500 in 1991 dollars. The third was size of metropolitan population, modeled as a series of 3 dummy variables (50 000–99 999, 100 000–499 999, and more than 500 000).
The main independent variable derived from the NPHS, individual household income, defined as income exclusive of taxes but inclusive of government transfers, was measured at baseline in 1994–1995. This variable, originally an 11-category variable ranging from no income to greater than $80 000, was modeled as a series of 5 dummy variables (less than $10 000, $10 000–$19 999, $20 000–$39 999, $40 000–$59 999, and more than $60 000). This specification balanced the requirement of a minimum sample size in each income dummy-variable category with the potential nonlinear and diminishing relationship between household income and health. Household size was included separately as a deflator for household income.
Building on the neomaterialist and psychosocial explanations for an association between income inequality and health status,41,42 we also derived from the NPHS 4 sets of conceptually related variables that could potentially confound or represent causal pathways in the relationship among income inequality, household income, and health status. These variable sets were demographic characteristics (age, age squared, sex, and marital status), socioeconomic status (highest level of education obtained), health behaviors (smoking status, number of alcoholic drinks consumed in the week before the survey, and level of physical activity), and social networks (social support and social involvement). We conceptualized the demographic variables as confounders. Educational status was viewed primarily as a confounder in the relationship between household income and health and not as a pathway variable in the relationship between income inequality and health in Canadian metropolitan areas, because at the time the surveys were conducted, education-related investments were made at the provincial level. The health behavior and social network variables were viewed primarily as pathway variables (i.e., areas with high levels of income inequality may have fewer parks and recreation facilities and hence lower levels of physical activity and health status).
The associations between the main independent variables (income inequality and average area income measured in 1991 and household income measured in 1994) and the health status variables were analyzed initially as a cross-sectional relationship with health status measured in 1994 and then as a longitudinal relationship with health status measured in 1996 and 1998. In each case, all 3 main independent variables were modeled together. The following variables were added cumulatively to each model: city size, demographics, educational status, health behaviors, and social networks. To control for the potential effect of baseline health status on the income variables (i.e., reverse causality), we also added health status measured in 1994 to the longitudinal models. We created an interaction term by multiplying a dichotomized form of the household income variable (less than $20 000 versus not less than $20 000) by the income inequality variable, allowing us to assess whether the relationship between income inequality and individual health status is different for low- and highincome individuals.
Maximum-likelihood ordered-logit estimation47 was used for all models, with selfreported health status as the dependent variable. The ordered-logit model (also known as the proportional odds model) is conceptually similar to a logistic regression model; however, in the present case, all 5 levels of the health status variable and their logical ordering were used, leading to more efficient estimation (i.e., smaller variance).48 The sign and statistical significance of the resulting coefficients can be interpreted in the same way as the coefficients from linear regression analyses. We calculated the predicted probabilities of a particular level of self-reported health status in 1998 for various levels of income inequality and average area income and for each of the household income dummy variables at the median values of the potential confounders in the fully adjusted model.
We used linear regression for all models in which the HUI was the dependent variable. We used sampling weights to account for the unequal probability of selection into the survey, and we adjusted standard errors and 95% confidence intervals (CIs) to account for the stratified multistage design of the NPHS, with the bootstrap variance estimation technique developed for the survey by Statistics Canada.49
RESULTS
No statistically significant relationship was observed between income inequality and self-reported health status in 1994 (i.e., cross sectionally) (β = 0.007; 95% CI = −0.058, 0.072) or 1996 (i.e., at the 2-year follow-up) (β = 0.009; 95% CI = −0.059, 0.076) before adjustment for potential confounders and pathway variables (Table 1 ▶). A significant positive relationship (i.e., higher income inequality was associated with higher health status) was observed in 1998 (i.e., at the 4-year follow-up) (β = −0.107; 95% CI = −0.174, −0.039) before adjustment for potential confounders and after addition of the demographic, education, and health behavior variables. After incremental adjustment for the social network variables (social support and social involvement), the positive relationship in 1998 weakened (β = −0.080; 95% CI = −0.161, 0.001).
TABLE 1—
Income Inequality and Income-Related Ordered Logit Beta Coefficients With Self-Reported Health Status (SRHS) as the Dependent Variable
| 1994 SRHS β (95% CI) | 1996 SRHS β (95% CI) | 1998 SRHS β (95% CI) | |
| Unadjusted | |||
| Median share of total area income | 0.007 (−0.058, 0.072) | 0.009 (−0.059, 0.076) | −0.107 (−0.174, −0.039) |
| Average area household income | −0.010 (−0.020, −0.001) | −0.006 (−0.017, 0.005) | −0.007 (−0.017, 0.019) |
| Household income, $a | |||
| 40 000–59 999 | −0.368 (−0.524, −0.212) | −0.246 (−0.412, −0.081) | −0.291 (−0.471, −0.112) |
| 20 000–39 999 | −0.762 (−0.919, −0.605) | −0.668 (−0.831, −0.506) | −0.683 (−0.855, −0.511) |
| 10 000–19 999 | −1.120 (−1.312, −0.927) | −0.856 (−1.063, −0.649) | −0.942 (−1.161, −0.724) |
| < 10 000 | −1.235 (−1.531, −0.940) | −1.047 (−1.365, −0.729) | −1.144 (−1.504, −0.785) |
| Sample size | 6186 | 6043 | 5916 |
| Adjusted for city size, household size, demographics,b and educational status | |||
| Median share of total area income | 0.068 (−0.012, 0.149) | 0.003 (−0.079, 0.085) | −0.086 (−0.168, −0.005) |
| Average area household income | −0.020 (−0.031, −0.009) | −0.008 (−0.020, 0.004) | −0.012 (−0.024, −0.003) |
| Household income, $ | |||
| 40 000–59 999 | −0.297 (−0.455, −0.139) | −0.190 (−0.355, −0.024) | −0.251 (−0.434, −0.069) |
| 20 000–39 999 | −0.568 (−0.739, −0.397) | −0.509 (−0.692, −0.327) | −0.547 (−0.731, −0.364) |
| 10 000–19 999 | −0.767 (−0.984, −0.549) | −0.542 (−0.781, −0.303) | −0.655 (−0.900, −0.411) |
| < 10 000 | −1.017 (−1.322, −0.713) | −0.866 (−1.188, −0.545) | −0.990 (−1.378, −0.603) |
| Sample size | 6180 | 6037 | 5911 |
| Adjusted for city size, household size, demographics, educational status, health behaviors,c and social networksd | |||
| Median share of total area income | 0.063 (−0.019, 0.146) | 0.010 (−0.071, 0.091) | −0.080 (−0.161, 0.001) |
| Average area household income | −0.022 (−0.034, −0.010) | −0.010 (−0.023, 0.004) | −0.013 (−0.024, −0.002) |
| Household income, $ | |||
| 40 000–59 999 | −0.274 (−0.443, −0.106) | −0.190 (−0.364, −0.016) | −0.256 (−0.440, −0.071) |
| 20 000–39 999 | −0.506 (−0.688, −0.325) | −0.472 (−0.660, −0.283) | −0.491 (−0.677, −0.305) |
| 10 000–19 999 | −0.686 (−0.918, −0.455) | −0.464 (−0.710, −0.217) | −0.578 (−0.824, −0.332) |
| < 10 000 | −0.910 (−1.243, −0.578) | −0.805 (−1.133, −0.478) | −0.889 (−1.295, −0.484) |
| Sample size | 5869 | 5738 | 5623 |
| Adjusted for city size, household size, demographics, educational status, health behaviors, social networks, and baseline health status | |||
| Median share of total area income | . . . | −0.009 (−0.090, 0.072) | −0.123 (−0.207, −0.040) |
| Average area household income | . . . | −0.001 (−0.015, 0.013) | −0.005 (−0.017, 0.007) |
| Household income, $ | |||
| 40 000–59 999 | . . . | −0.065 (−0.248, 0.118) | −0.143 (−0.332, 0.047) |
| 20 000–39 999 | . . . | −0.220 (−0.420, −0.021) | −0.281 (−0.473, −0.088) |
| 10 000–19 999 | . . . | −0.164 (−0.431, 0.103) | −0.319 (−0.570, −0.067) |
| < 10 000 | . . . | −0.374 (−0.700, −0.049) | −0.472 (−0.859, −0.085) |
| Sample size | . . . | 5738 | 5623 |
Note. Positive coefficients indicate improved health status. CI = confidence interval.
aReference category: household income greater than $60 000.
bIncluding age, age squared, sex, and marital status.
cIncluding smoking status, number of drinks consumed in the week before the survey, and level of physical activity.
dIncluding social support and social involvement.
According to the model adjusted for all potential confounders and pathway variables, an increase in the median share of total area household income from 22.0% to 26.0% in 1991 (i.e., a reduction in income inequality) led to a lower predicted probability of reports of excellent health and very good health in 1998 (differences of 0.048 and 0.029) and a corresponding higher predicted probability of reports of good health, fair health, and poor health (differences of 0.049, 0.023, and 0.006). When we also adjusted for baseline health status, the positive relationship in 1998 increased in magnitude and was again significant (β = −0.123; 95% CI = −0.207, −0.040).
A statistically significant negative relationship (i.e., higher average area income was associated with lower health status) was observed between average area income in 1991 and self-reported health status in 1994 before adjustment for potential confounders and pathway variables (β = −0.010; 95% CI = −0.020, −0.001), and similar relationships were observed in 1994 (β = −0.022; 95% CI = −0.034, −0.010) and 1998 (β = −0.013; 95% CI = −0.024, −0.002), but not in 1996 (β = −0.010; 95% CI = −0.023, 0.004), after adjustment for potential confounders and pathway variables. According to the model adjusting for all potential confounders and pathway variables, an increase in average area income from $35 000 to $55 000 in 1991 led to a lower predicted probability of reports of excellent health and very good health in 1998 (differences of 0.040 and 0.020) and to a higher predicted probability of reports of good health, fair health, and poor health in 1998 (differences of 0.039, 0.017, and 0.004). No statistically significant relationship was observed when baseline health status was added to the longitudinal models.
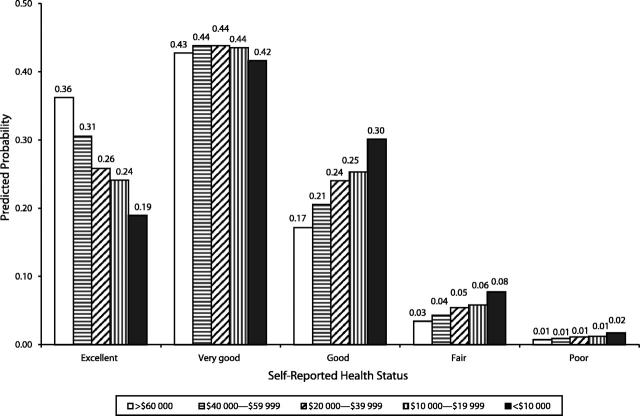
The relationship between household income and self-reported health status was statistically significant for all income categories before and after the addition of all potential confounders and pathway variables. As household income decreased, the probability of reports of lower levels of self-reported health status increased (Figure 1 ▶). According to the model adjusting for all potential confounders and pathway variables and moving from the highest to the lowest income category, the predicted probability of reports of excellent health decreased by 0.173 in 1998, and the predicted probability of reports of good health, fair health, and poor health increased by 0.130, 0.043, and 0.010, respectively, in 1998. When baseline self-reported health status was incrementally added to the longitudinal models, the relationship approximately halved in strength for all income categories, and the second-highest household income category ($40 000–$59 000) became statistically nonsignificant in both outcome years.
FIGURE 1—
Predicted probabilities of various self-reported health states for 5 household income categories, adjusted for all potential confounders: Canada, 1998.
The combination of low household income and residence in a metropolitan area with low levels of income inequality was associated with lower levels of self-reported health status (data not shown). This relationship persisted both cross sectionally and longitudinally and with the addition of all potential confounders and pathway variables. We calculated the predicted probabilities for each level of selfreported health status in 1998 for 4 income inequality and household income combinations in the model that included all potential confounders and pathway variables (Figure 2 ▶). Relative to the combination of high income and residence in a high-income inequality area, the combination of low household income and residence in a low-income inequality area led to predicted proportional declines of 0.22 in reports of excellent health and 0.08 in reports of very good health, along with predicted proportional increases of 0.18, 0.08, and 0.02 in reports of good health, fair health, and poor health, respectively. When baseline self-reported health status was incrementally added, however, this relationship was no longer significant.
FIGURE 2—
Predicted probabilities of various self-reported health states for 4 income inequality and household income combinations, adjusted for all potential confounders: Canada, 1998.
Similar results were observed when the HUI was used as the dependent variable (Table 2 ▶). There were statistically significant positive relationships between income inequality and the HUI in 1996 (β = −0.007; 95% CI = −0.013, −0.001) and 1998 (β = −0.011; 95% CI = −0.020, −0.002), but not in 1994 (β = −0.006; 95% CI = −0.012, 0.000), before the addition of potential confounders and pathway variables. With the addition of all potential confounders and pathway variables, a significant positive relationship was observed only in 1998 (β = −0.010; 95% CI = −0.020, −0.001). A statistically significant negative relationship was observed between average area income and the HUI in 1994 (β = −0.001; 95% CI = −0.002, −0.000), but not in 1996 (β = −0.001; 95% CI = −0.002, 0.000) or 1998 (β = −0.000; 95% CI = −0.001, 0.001), before the addition of potential confounders and pathway variables. After the addition of all potential confounders and pathway variables, the relationship was significant in 1994 (β = −0.002; 95% CI = −0.003, −0.001) and 1996 (β = −0.002; 95% CI = −0.003, −0.000).
TABLE 2—
Income Inequality and Income-Related Beta Coefficients With McMaster Health Utility Index (HUI) as the Dependent Variable
| 1994 HUI β (95% CI) | 1996 HUI β (95% CI) | 1998 HUI β (95% CI) | |
| Unadjusted | |||
| Median share of total area income | −0.006 (−0.012, 0.000) | −0.007 (−0.013, −0.001) | −0.011 (−0.020, −0.002) |
| Average area household income | −0.001 (−0.002, −0.000) | −0.001 (−0.002, −0.000) | −0.000 (−0.001, 0.001) |
| Household income, $a | |||
| 40 000–59 999 | −0.024 (−0.040, −0.008) | −0.024 (−0.037, −0.010) | −0.015 (−0.030, 0.000) |
| 20 000–39 999 | −0.059 (−0.076, −0.042) | −0.054 (−0.071, −0.037) | −0.051 (−0.068, −0.034) |
| 10 000–19 999 | −0.102 (−0.123, −0.082) | −0.103 (−0.123, −0.082) | −0.112 (−0.133, −0.092) |
| < 10 000 | −0.113 (−0.151, −0.075) | −0.113 (−0.148, −0.078) | −0.120 (−0.157, −0.083) |
| Sample size | 6132 | 6001 | 5887 |
| Adjusted for city size, household size, demographics,b and educational status | |||
| Median share of total area income | 0.002 (−0.006, 0.009) | −0.004 (−0.012, 0.003) | −0.010 (−0.021, 0.001) |
| Average area household income | −0.002 (−0.003, −0.001) | −0.002 (−0.003, −0.000) | −0.001 (−0.002, 0.000) |
| Household income, $ | |||
| 40 000–59 999 | −0.015 (−0.031, −0.001) | −0.014 (−0.026, −0.002) | −0.005 (−0.020, 0.009) |
| 20 000–39 999 | −0.032 (−0.049, −0.014) | −0.027 (−0.043, −0.012) | −0.020 (−0.038, −0.003) |
| 10 000–19 999 | −0.051 (−0.074, −0.029) | −0.056 (−0.078, −0.034) | −0.056 (−0.077, −0.035) |
| < 10 000 | −0.074 (−0.112, −0.035) | −0.081 (−0.114, −0.048) | −0.085 (−0.124, −0.047) |
| Sample size | 6127 | 5995 | 5882 |
| Adjusted for city size, household size, demographics, educational status, health behaviors,c and social networksd | |||
| Median share of total area income | −0.001 (−0.009, 0.007) | −0.004 (−0.011, 0.004) | −0.010 (−0.020, −0.001) |
| Average area household income | −0.002 (−0.003, −0.001) | −0.002 (−0.003, −0.000) | −0.001 (−0.002, 0.000) |
| Household income | |||
| 40 000–59 999 | −0.013 (−0.028, 0.003) | −0.010 (−0.023, 0.002) | 0.001 (−0.013, 0.014) |
| 20 000–39 999 | −0.021 (−0.037, −0.004) | −0.019 (−0.035, −0.004) | −0.015 (−0.031, 0.002) |
| 10 000–19 999 | −0.043 (−0.065, −0.020) | −0.047 (−0.068, −0.027) | −0.050 (−0.069, −0.031) |
| < 10 000 | −0.062 (−0.100, −0.024) | −0.074 (−0.107, −0.040) | −0.080 (−0.112, −0.042) |
| Sample size | 5843 | 5702 | 5596 |
| Adjusted for city size, household size, demographics, educational status, health behaviors, social networks, and baseline health status | |||
| Median share of total area income | . . . | −0.003 (−0.009, 0.003) | −0.010 (−0.019, −0.001) |
| Average area household income | . . . | −0.001 (−0.002, 0.000) | −0.000 (−0.001, 0.001) |
| Household income | |||
| 40 000–59 999 | . . . | −0.004 (−0.014, 0.006) | 0.006 (−0.007, 0.018) |
| 20 000–39 999 | . . . | −0.007 (−0.020, 0.006) | −0.002 (−0.015, 0.012) |
| 10 000–19 999 | . . . | −0.025 (−0.044, −0.006) | −0.030 (−0.048, −0.013) |
| < 10 000 | . . . | −0.043 (−0.069, −0.017) | −0.052 (−0.083, −0.022) |
| Sample size | . . . | 5676 | 5572 |
Note. Positive coefficients indicate improved health status. CI = confidence interval.
aReference category: household income greater than $60 000.
bIncluding age, age squared, sex, and marital status.
cIncluding smoking status, number of drinks consumed in the week before the survey, and level of physical activity.
dIncluding social support and social involvement.
A statistically significant positive relationship was observed for all household income categories, both cross sectionally and longitudinally, before the addition of potential confounders and pathway variables. With the addition of all potential confounders and pathway variables, the relationship disappeared for the upper-middle-income level ($40 000–$59 999) in 1996 (β = −0.010; 95% CI = −0.023, 0.002) and 1998 (β = 0.001; 95% CI = −0.013, 0.014) and for the middle-income level ($20 000–$39 999) in 1998 (β = −0.015; 95% CI = −0.031, 0.002); with the addition of baseline health status, the relationship disappeared for the uppermiddle-income level and the middle-income level in both 1996 and 1998. The combination of low household income and residence in a metropolitan area with low levels of income inequality was associated with lower HUI values only in 1994 (data not shown).
DISCUSSION
We found little evidence that higher income inequality is associated with lower levels of health status in Canada. There was some evidence that the relationship between 1 measure of health status—self-reported health status—and income inequality changed across outcome years. However, it is unclear whether this change reflects a real change over time or whether it is owing to a possible reciprocal influence of health on income inequality. A different approach, such as instrumental variable estimation, would be required to account fully for such reciprocal influences.
We found some evidence that higher income inequality is associated with better health status and that low-income Canadians may be healthier in metropolitan areas with high levels of income inequality than in metropolitan areas with low levels of income inequality. Although metropolitan income inequality tended to be smaller and spanned a narrower range than found in metropolitan areas in the United States, a positive relationship between income inequality and area-level mortality has been observed for metropolitan areas in the United States with the same range as Canadian metropolitan areas. This finding suggests that it is not the lesser degree and narrower range of income inequality that explains the lack of a negative relationship between income inequality and health.50
Household income, on the other hand, was strongly and consistently associated with health status over time, across health measures, after adjustment for potential confounders and pathway variables, and after adjustment for baseline health status. Indeed, apart from health status at baseline, household income was the best predictor of future health status. Some support was found for the hypothesis that the position of an individual’s income relative to the average income in an area may affect his or her health status. This follows from the negative relationship between average area income and health status, which implies that, conditional on a given level of household income, an increase in average area income is associated with lower levels of health status. This relationship did not hold consistently across all years.
Our findings are consistent with the results of a study conducted in Denmark39 that involved the use of a cohort design and multilevel data at the county level and with the results of some34,35,38 (but not all36,37) US studies that involved cohort designs and multilevel data and were conducted at the county, metropolitan, or state level. The finding that higher income inequality may be associated with lower levels of health status, however, has not been reported elsewhere.
If we consider that income inequality is a proxy for underlying conditions that may influence health status, however, perhaps our findings are not surprising. In the absence of direct associations between these conditions and measures of income inequality, it is quite understandable that evidence for a relationship varies across countries.9
Our findings may be understood with reference to the neomaterialist explanation of the association between income inequality and health status, according to which increased income inequality influences health through a systematic underinvestment in factors that can influence health status (e.g., health care, education, income replacement programs, public transportation, public health programs, recreation facilities).41 In Canada, the distribution of many of these factors may be independent of metropolitan-level income inequality. Investments in health care, education, and many income replacement programs are determined at the provincial level with partial funding from the federal government (which ensures equitable levels of funding among provinces through equalization payments made to poorer provinces). Public transportation and public health programs tend to be funded by regions (which correspond closely to metropolitan areas), whereas recreation facilities tend to be funded by cities (which are the constituent units of metropolitan areas).
Paradoxically, more unequal metropolitan areas in Canada may have more tax revenues to invest in these programs, given their greater concentration of high-income households and the higher corporate tax bases in their central cities (e.g., Toronto). Metropolitan areas within the United States, on the other hand, are characterized by a greater degree of municipal fragmentation, less generous social programs, and a greater dependence on local revenues for public investments.51
We are not suggesting that socioeconomic inequalities do not matter in Canada. Indeed, health disparities have been found in Canada in terms of both economic hierarchies and occupational hierarchies,52 and despite 2 decades of research and attention by policymakers, they still persist.53
More research is needed that explores the potential underlying mechanisms that might explain a relationship between income inequality and health. Furthermore, why is such a relationship sometimes observed in the United States but not in Canada or Denmark? In the meantime, the case for undertaking and evaluating approaches to addressing low household income continues to grow stronger. Household income appears to explain some of the differences in health status among Canadians, and the relationship between income and health appears to be robust across countries and time periods.54
Acknowledgments
This project was funded in part by the Canadian Population Health Initiative.
We are grateful to J. M. Berthelot, who provided us with the income and other measures based on the 1991 Canadian census, and to J. R. Dunn, who provided helpful comments on earlier versions of the article.
Human Participant Protection
This study was approved by the health and sciences ethics review committee of the University of Toronto. Participants gave verbal consent at the time of the first survey for their data to be collected and used under the auspices of the Canadian Statistics Act of 1985.
Contributors
C. B. McLeod conceived the study, conducted the data analysis, and wrote the article. J. N. Lavis helped conceive the study, reviewed interim data analysis reports, and helped write the article. C. A. Mustard and G. L. Stoddart helped conceive the study and provided comments on the article.
Peer Reviewed
References
- 1.Wagstaff A, van Doorslaer E. Income inequality and health: what does the literature tell us? Annu Rev Public Health. 2000;21:543–567. [DOI] [PubMed] [Google Scholar]
- 2.Deaton A. Health, Inequality, and Economic Development. Cambridge, Mass: National Bureau of Economic Research; 2001. National Bureau of Economic Research working paper 8318.
- 3.Mackenbach J. Income inequality and population health. BMJ. 2002;324:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rogers G. Income and inequality as determinants of mortality: an international cross-sectional analysis. Popul Stud. 1979;33:343–351. [Google Scholar]
- 5.Wilkinson R. Income distribution and mortality: a “natural experiment.” Sociol Health Illness. 1990;12:391–412. [Google Scholar]
- 6.Wilkinson R. Income distribution and life expectancy. BMJ. 1992;304:165–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wennemo I. Infant mortality, public policy, and inequality: a comparison of eighteen industrialized countries, 1950–1995. Sociol Health Illness. 1993;15:429–446. [Google Scholar]
- 8.Judge K, Mulligan J, Benzeval M. Income inequality and population health. Soc Sci Med. 1998;46:567–579. [DOI] [PubMed] [Google Scholar]
- 9.Lynch J, Davey Smith G, Hillemeier M, Shaw M, Raghunathan T, Kaplan G. Income inequality, the psychosocial environment, and health: comparisons of wealthy nations. Lancet. 2001;358:194–200. [DOI] [PubMed] [Google Scholar]
- 10.Gravelle H, Wildman J, Sutton M. Income, income inequality and health: what can we learn from aggregate data? Soc Sci Med. 2002;54:577–589. [DOI] [PubMed] [Google Scholar]
- 11.Ben-Shlomo Y, White I, Marmot M. Does the variation in the socioeconomic characteristics of an area affect mortality? BMJ. 1996;312:1013–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaplan G, Pamuk E, Lynch J, Cohen R, Balfour J. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. BMJ. 1996;312:999–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy B, Kawachi I, Prothow-Stith D. Income distribution and mortality: cross sectional ecological study of the Robin Hood index in the United States. BMJ. 1996;312:1004–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lynch J, Kaplan G, Pamuk E, et al. Income inequality and mortality in metropolitan areas of the United States. Am J Public Health. 1998;88:1074–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiang T. Economic transition and changing relation between income inequality and mortality in Taiwan: regression analysis. BMJ. 1999;319:1162–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McLaughlin D, Stokes S. Income inequality and mortality in US counties: does racial concentration matter? Am J Public Health. 2002;92:99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ross N, Wolfson M, Dunn J, Berthelot J, Kaplan G, Lynch J. Relation between income inequality and mortality in Canada and in the United States: cross sectional assessment using census data and vital statistics. BMJ. 2000;320:898–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mellor J, Milyo J. Re-examining the evidence of an ecological association between income inequality and health. J Health Polit Policy Law. 2001;26:487–522. [DOI] [PubMed] [Google Scholar]
- 19.Muller A. Education, income inequality, and mortality: a multiple regression analysis. BMJ. 2002;324:23–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kawachi I, Blakely T. When economists and epidemiologists disagree. J Health Polit Policy Law. 2001;26:487–522. [DOI] [PubMed] [Google Scholar]
- 21.Gravelle H. How much of the relation between population mortality and unequal distribution of income is a statistical artefact? BMJ. 1998;316:382–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wildman J. The impact of income inequality on individual and societal health: absolute income, relative income and statistical artifacts. Health Econ. 2000;10:357–361. [DOI] [PubMed] [Google Scholar]
- 23.Wolfson M, Rowe G, Gentleman J, Tomiak M. Career earnings and death: a longitudinal analysis of older Canadian men. J Gerontol. 1993;48:S167–S169. [DOI] [PubMed] [Google Scholar]
- 24.Backlund E, Sorlie P, Johnson N. The shape of the relationship between income and mortality in the United States: evidence from the National Longitudinal Mortality Study. Ann Epidemiol. 1996;6:12–20. [DOI] [PubMed] [Google Scholar]
- 25.Ecob R, Davey Smith G. Income and health: what is the nature of the relationship? Soc Sci Med. 1999;48:693–705. [DOI] [PubMed] [Google Scholar]
- 26.Soobader M, Lennart L. Aggregation and the measurement of income inequality. Soc Sci Med. 1997;48:733. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy B, Kawachi I, Glass R, Prothow-Stith D. Income distribution, socioeconomic status, and self rated health status in the United States: multilevel analysis. BMJ. 1998;317:917–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kahn R, Wise P, Kennedy B, Kawachi I. State income inequality, household income, and maternal mental and physical health: cross sectional national survey. BMJ. 2000;321:1311–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diez-Roux A, Link B, Northridge M. A multi-level analysis of income inequality and cardiovascular disease factors. Soc Sci Med. 2000;50:673–687. [DOI] [PubMed] [Google Scholar]
- 30.Blakely T, Lochner K, Kawachi I. Metropolitan area income inequality and self-rated health—a multi-level study. Soc Sci Med. 2002;54:65–77. [DOI] [PubMed] [Google Scholar]
- 31.Shibuya K, Hashimoto H, Yano E. Individual income, income distribution, and self-rated health in Japan: cross sectional analysis of a nationally representative sample. BMJ. 2002;324:16–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weich S, Lewis G, Jenkins S. Income inequality and the prevalence of common mental disorders in Britain. Br J Psychiatry. 2001;178:222–227. [DOI] [PubMed] [Google Scholar]
- 33.Smith J. Healthy bodies and thick wallets: the dual relationship between health and economic status. J Econ Perspect. 1999;13:145–166. [PMC free article] [PubMed] [Google Scholar]
- 34.Fiscella K, Franks P. Poverty or income inequality as predictor of mortality: longitudinal cohort study. BMJ. 1997;317:1724–1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Daly M, Duncan G, Kaplan GA, Lynch JW. Macro-to-micro links in the relation between income inequality and mortality. Milbank Q. 1998;76:315–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fiscella K, Franks P. Individual income, income inequality, health and mortality: what are the relationships? Health Serv Res. 2000;35:307–318. [PMC free article] [PubMed] [Google Scholar]
- 37.Lochner K, Pamuk E, Makuc D, Kennedy B, Kawachi I. State-level income inequality and individual mortality risk: a prospective multilevel study. Am J Public Health. 2001;91:385–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Strum R, Gresenz C. Relations of income or income inequality and family income to chronic medical conditions and mental health disorders: national survey. BMJ. 2002;324:20–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Osler M, Prescott E, Gronbaek M, Christensen U, Due P, Engholm G. Income inequality, individual income, and mortality in Danish adults: analysis of pooled data from two cohort studies. BMJ. 2002;324:13–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ellison G. Letting the Gini out of the bottle? Challenges facing the relative income hypothesis. Soc Sci Med. 2002;54:561–576. [DOI] [PubMed] [Google Scholar]
- 41.Lynch JW, Kaplan GA. Understanding how inequality in the distribution of income affects health. J Health Psychol. 1997;2:297–314. [DOI] [PubMed] [Google Scholar]
- 42.Lynch JW, Davey Smith G, Kaplan GA, House JS. Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. BMJ. 2000;320:1200–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Birch S, Elyes J, Newbold BK. Equitable access to health care: methodological extensions to the analysis of physician utilization in Canada. Health Econ. 1993;2:87–101. [DOI] [PubMed] [Google Scholar]
- 44.van Doorslaer E, Koolman X, Puffer F. Equity in the use of physician visits in OECD countries: has equal treatment for equal need been achieved? In: Smith P, ed. Measuring Up: Improving the Health System Performance in OECD Countries. Paris, France: Organization for Economic Cooperation and Development; 2002:225–248.
- 45.National Population Health Survey, 1994–1998 Longitudinal File. Ottawa, Ontario, Canada: Statistics Canada; 2000.
- 46.Torrance G, Feeny D, Furlong W, Barr R, Zhang Y, Wang Q. Multiattribute utility function for a comprehensive health status classification system. Med Care. 1996;34:702–722. [DOI] [PubMed] [Google Scholar]
- 47.Stata Statistical Software: Release 7.0. College Station, Tex: Stata Corp; 2000.
- 48.McCullagh P, Nelder, J. Generalized Linear Models. 2nd ed. London, England: Chapman & Hill; 1989.
- 49.Yeo D, Mantel H, Liu T. Bootstrap variance estimation for the National Population Health Survey. In: Proceedings of the Survey Research Methods Section, American Statistical Association. Washington, DC: American Statistical Association; 1999:778–784.
- 50.Ross N, Wolfson M, Berthelot J, Dunn J, Kaplan G, Lynch J. Income inequality and mortality in Canada: authors’ reply. BMJ. 2000;321:1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dunn JR. Are Widening Income Inequalities Making Canada Less Healthy? Toronto, Ontario, Canada: Health Determinants Partnership; 2002.
- 52.Mustard CA, Vermeulen M, Lavis JN. Is position in the occupational hierarchy a determinant of decline in perceived health status? Soc Sci Med. In press. [DOI] [PubMed]
- 53.Lavis JN. Ideas at the margin or marginalized ideas? Nonmedical determinants of health in Canada. Health Aff. 2002;21:107–112. [DOI] [PubMed] [Google Scholar]
- 54.Benzeval M, Judge K. Income and health: the time dimension. Soc Sci Med. 2001;52:1371–1390. [DOI] [PubMed] [Google Scholar]