Abstract
Use of multilevel frameworks and area-based socioeconomic measures (ABSMs) for public health monitoring can potentially overcome the absence of socioeconomic data in most US public health surveillance systems.
To assess whether ABSMs can meaningfully be used for diverse race/ethnicity–gender groups, we geocoded and linked public health surveillance data from Massachusetts and Rhode Island to 1990 block group, tract, and zip code ABSMs. Outcomes comprised death, birth, cancer incidence, tuberculosis, sexually transmitted infections, childhood lead poisoning, and nonfatal weapons-related injuries.
Among White, Black, and Hispanic women and men, measures of economic deprivation (e.g., percentage below poverty) were most sensitive to expected socioeconomic gradients in health, with the most consistent results and maximal geocoding linkage evident for tract-level analyses.
Despite growing interest in social inequalities in health,1–4 routine monitoring of socioeconomic gradients in health in the United States is hampered by a lack of socioeconomic data in most US public health surveillance systems.5,6 Notable exceptions include birth and death certificates, which since 1989 have included data on educational level,7 and also data obtained from specialized surveys, such as the National Health Interview Survey.8 However, surveys are incapable of monitoring important aspects of population health (e.g., cancer incidence, tuberculosis (TB), and childhood lead levels), nor can they readily provide the kinds of routine—and local—data required by health departments, especially on relatively small population subgroups, such as members of diverse racial/ethnic communities.5,9
Reflecting gaps created by unavailable socioeconomic data, the 2002 edition of Health, United States,10 the annual federal publication profiling the health of the nation, lacked socioeconomic data in 85.5% of its 71 tables on “health status and determinants”; virtually all tables, however, were stratified by “sex, race, and Hispanic origin.” Likewise, fully 70% of the 467 US public health objectives for the year 2010 had no socioeconomic targets, given a lack of baseline data.11,12 This absence of economic data from routine public health monitoring—equally evident in state health department publications—obscures socioeconomic gradients in health overall and within diverse race/ethnicity–gender groups, as well as the contribution of economic deprivation to racial/ethnic and gender inequalities in health.5,6,12–14
Fortunately, the methodology of geocoding residential addresses and using area-based socioeconomic measures (ABSMs) is a potential and relatively inexpensive solution to the problem of absent or limited socioeconomic data in US public health surveillance systems.6,12,15,16 In this approach, which draws on multilevel frameworks and area-based measures, both cases (numerators) and the catchment population (denominators) are classified by the socioeconomic characteristics of their residential area, thereby permitting calculation of rates stratified by the ABSMs.
Although this approach has been employed in US health research for over 75 years,17–20 to date there exists no consensus or standard as to which ABSMs, at which level of geography, are best suited for monitoring US socioeconomic inequalities in health.6,12,15,20 Nor, to our knowledge, have any investigations systematically assessed, empirically, whether specified ABSMs perform similarly or differently in diverse race/ethnicity–gender groups. Instead, published research has exhibited a remarkable eclecticism regarding choice of geographic level and types of ABSM used, both single variable and composite.6,12,21 Although such a plurality of measures may be useful for etiologic research, in the case of monitoring, such heterogeneity impedes comparing results across studies, outcomes, and regions and over time.
We accordingly launched the Public Health Disparities Geocoding Project to ascertain which ABSMs, at which geographic level (census block group, census tract, or zip code), would be most apt for monitoring US socioeconomic inequalities in health. To provide a robust evaluation, guided by ecosocial theory,22,23 we designed the study to encompass a wide variety of health outcomes, hypothesizing that some ABSMs and geographic levels might be more sensitive to socioeconomic gradients for some health outcomes than others.
Drawing on 1990 census data and public health surveillance systems of 2 New England states, Massachusetts and Rhode Island, we included 7 types of outcomes: mortality (all cause and cause specific), cancer incidence (all sites and site specific), low birth weight, childhood lead poisoning, sexually transmitted infections, TB, and nonfatal weaponsrelated injuries.24–26 Pertinent a priori considerations, derived in part from Rossi and Gilmartin’s criteria for valid and useful social indicators,27 included (a) external validity (do the measures find gradients in the direction reported in the literature, i.e., positive, negative, or none, and across the full range of the distribution?), (b) robustness (do the measures detect expected gradients across a wide range of outcomes?), (c) completeness (is the measure relatively unaffected by missing data?), and (d) user-friendliness (how easy is the measure to understand and explain?).
Our initial analyses focused on the total population of each state, with results suggesting that public health monitoring might be judiciously augmented by the use of census tract–level measures of economic deprivation, and specifically the measure “percentage of persons below poverty.”24–26 In this investigation, we extend our analyses by examining whether these conclusions hold for diverse race/ethnicity–gender groups.
METHODS
Data Sources: Population and Health Outcomes
As described in our earlier publications,24–26 the study base comprised (a) populations and areas in Massachusetts and Rhode Island enumerated at the 1990 census and (b) health outcomes occurring in the period around the 1990 census. We obtained public health surveillance data from the Massachusetts Department of Public Health and the Rhode Island Department of Health for death, birth, cancer incidence, TB, sexually transmitted infections, childhood lead poisoning (Rhode Island only), and nonfatal weapons-related injuries (Massachusetts only).
Data for death, birth, cancer incidence, and childhood lead poisoning (among children 1 to 5 years old) were analyzed for persons. Data for TB, sexually transmitted infections, and nonfatal weapons-related injuries were analyzed for new cases only, since a given individual could experience the specified outcome more than once during the study period; data for lead poisoning were likewise analyzed only for a child’s first record in the study interval, not repeat follow-up tests. Slightly over 760 000 records were included in our final analytic data sets,24–26 restricted to records for in-state residents with health outcomes occurring during the specified study interval and not missing data on age, gender, or the specified outcome, plus additional restrictions described below. All records were geocoded to the census block group, census tract, and zip code levels by a commercial geocoding firm whose accuracy we validated (96%).28
With regard to outcomes, cause of death was categorized according to International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes and cancer type by standard Surveillance, Epidemiology, and End Results (SEER) site/histology definitions.24,29–34 Mortality outcomes analyzed included premature mortality (< 65 years old) and selected causes of death ranked among the top 5 causes of death in each state within one or more racial/ethnic groups,24 including mortality due to heart disease, neoplasm, diabetes, HIV, and homicide. Incidence of cancer was analyzed for all cancers combined and the 5 leading sites reported nationally34: breast, cervix, colon, lung, and prostate.24
We analyzed births to mothers aged 15 to 55 years; we report results only for singleton births, using the conventional definition of low birthweight as less than 2500 g.25,30,35 For Rhode Island’s mandatory universal childhood lead screening program, blood specimens were obtained 2 ways, at the screening physician’s discretion: venous and capillary/fingerstick.25,36 Because the latter may be subject to contamination (e.g., lead dust on the pricked finger),37 we analyzed the 2 sample types separately and present only the venous results. Following guidelines issued by the Centers for Disease Control and Prevention (CDC) in 1997,37 elevated blood lead levels were defined as 10 g/dL or above.
Cases included in the sexually transmitted infection databases for both states were identified and reported to the state health department because they (a) were symptomatic patients, (b) sought testing because they were concerned about their exposure (i.e., after unsafe sex), (c) received a complete battery of sexually transmitted infection tests as part of seeking confidential HIV testing, (d) were sexual partners of persons identified as cases, or (e) received testing as part of a routine gynecologic examination.26,38,39 Cases in both states’ TB databases were identified and reported to the state health department via designated TB clinics and additional health care providers.40,41 Finally, data on nonfatal weapons-related injury (intentional and unintentional) were obtained from the Massachusetts Department of Public Health’s Weapons-Related Injury Surveillance System, which encompasses all Massachusetts acute care hospital emergency departments.42 Fully 97% of the nonfatal weapons-related injuries were intentional; data on whether the injury was intentional or not were obtained from the respondent, if conscious, and otherwise coded as “unknown.”
The 1990 census, the source of our denominators, used self-report data to classify race/ethnicity in accordance with censusdefined categories pertaining to “race” and Hispanic “ethnicity”; data on age and gender were also obtained by self-report.43 Data on race/ethnicity, gender, and age were reported by the next of kin or recorded by the funeral director for the death data and were abstracted by registry staff from medical records for the cancer data.24,29,30,32,33 For birth certificate data, mother’s race/ethnicity and age were obtained by self-report through use of closed-format questions; for childhood lead poisoning, race/ethnicity, gender, and age of the child were reported by the child’s parent (or adult guardian).25,30,35,36 Data on race/ethnicity, gender, and age for the sexually transmitted infection, TB, and injury cases were obtained by a mixture of self-report and observer report.26,38–42 Notably, the different databases employed different approaches to categorizing racial/ethnic data: some used separate fields for data on “race” and on “Hispanic origin” (or “ancestry”), permitting these data to be cross-classified, while others used only one field for these items.
To maximize the compatibility of racial/ethnic categories employed in the numerators (cases) and denominators (population) and to ensure adequate sample size to conduct meaningful analyses, our investigation thus focused primarily on 3 racial/ethnic groups: White, Black, and Hispanic. In these analyses, the White and Black populations were mutually exclusive and included all persons regardless of census-designated “ethnicity,” while the Hispanic population included persons of all census-designated “races.” According to the 1990 census,44 fully 98% of both the Massachusetts and Rhode Island White populations in 1990 identified themselves as “nonHispanic,” as did 92% of the Massachusetts and 89% of the Rhode Island Black population. Conversely, among the Hispanic population, 43% in Massachusetts and 48% in Rhode Island identified themselves as “White,” 8% and 9% as “Black,” and 47% and 41% as “other race.” Analyses for the American Indian and the Asian and Pacific Islander populations (respectively comprising, combined, 2.5% and 2.2% of the Massachusetts and Rhode Island populations) were limited to premature mortality and low birthweight, as they were the main outcomes with sufficient data to yield interpretable results.
Data Sources: ABSMs
As described in our prior investigations,24–26 we obtained 1990 census data for census tracts and block groups from US Census Bureau Summary Tape File 3A and zip code data from Summary Tape File 3B.43 According to the US Census Bureau, census tracts on average contain 4000 persons and are a “small, relatively permanent statistical subdivision of a county . . . designed to be relatively homogeneous with respect to population characteristics, economic status, and living conditions.45(pG-10,G-11) The census tract’s subdivision, the block group, contains on average 1000 persons and is the smallest geographic census unit for which census socioeconomic data are tabulated.45(pG-6)
Zip codes, in turn, have an average population of 30 000 and are “administrative units established by the United States Postal Service . . . for the most efficient delivery of mail, and therefore generally do not respect political or census statistical area boundaries,” and they can range in size from large areas cutting across states to a single building or company with a high volume of mail.43(pA-13) Moreover, unlike with census tracts and block groups, zip code boundaries may overlap (since “carrier routes for one ZIP Code may intertwine with those of one or more ZIP Codes”),46(p22) and they can be added, eliminated, or have their codes changed or boundaries redefined in nondecennial years.47,48
Three considerations guided our development of ABSMs24–26: (a) a priori conceptual definitions of socioeconomic position (SEP) and social class,6 (b) US and UK evidence emphasizing the detrimental effects of material deprivation on health,1–4,49 and (c) the need for measures that can be meaningfully compared over time and space, so as to permit valid monitoring and contrasts in relation to time period and region.6,24–26,49 Our project generated, at each level of geography for each state, 11 single-variable and 8 composite ABSMs that met these criteria (Appendix 1; available from the first author upon request), which together reflected 6 domains of SEP: occupational class, income, poverty, wealth, education, and crowding, premised on the understanding that social class, as a social relationship, fundamentally drives the distribution of these manifest aspects of SEP6,24–26.
Of note, one ABSM we included differs from the others: the Gini coefficient, which is a measure of within-area socioeconomic inequality rather than a measure of the average socioeconomic level of an area.50 We included this measure because of concerns about its uncritical use—for example, at the block group and census tract level—since realities of economic segregation imply that the Gini coefficient should be employed only for larger aggregations.51
Among the composite variables, 2 were US analogues of the UK Townsend21,49,52 and Carstairs21,49,53 deprivation indices, 1 used the algorithm for the CDC’s Index of Local Economic Resources (developed as a county-level measure),54 and the remainder were created exclusively for our study.24–26 Two of these latter composite variables, SEP1 and SEP2, were intended to mirror the skewed population distribution of socioeconomic resources and simultaneously combined categorical data on poverty, working class, and either wealth or high income. Finally, the “SEP index,” a summed z score akin to the Townsend index, was generated through inputs identified by factor analysis,55,56 as described for our prior analyses.24–26 Cutpoints for both the single-variable and composite categorical ABSMs were based on both their percentile distribution (e.g., quintiles) and a priori considerations (e.g., the federal definition of “poverty areas” as regions where 20% or more of the population is below the US poverty line)57,58 (Appendix 2; available from the first author upon request).
Data Analysis
Our analytic plan involved 4 steps, conducted separately for each race/ethnicity–gender group. In Step 1, we assessed the data distribution, including the extent of missing data. In Step 2, we calculated the relevant age-standardized average annual incidence rate or proportion (for low birthweight and childhood lead poisoning), stratified by each ABSM at each level of geography for each state.59,60 For age standardization, we employed the year 2000 standard million,61 using 5 age groups (birth–14, 15–24, 25–44, 45–64, ≥65 years). The numerators and denominators of the calculated rates and proportions consisted of persons residing in areas identified at the specified level of geography for which data on the specified ABSMs were available. Following standard practice for rates centered around a census,62,63 we set the total number of person-years in the denominator equal to the population in that socioeconomic stratum enumerated in the 1990 census multiplied by the relevant number of years of observation.
In Step 3, we visually inspected and quantified socioeconomic gradients for each outcome, using each ABSM at each geographic level. Following standard US reporting practices,1,5 we computed the incidence rate ratio or odds ratio, as warranted, comparing people living in areas with the least and most resources. We also calculated the relative index of inequality, a measure that takes into account the proportion of the population in each stratum as well as the effect estimate for that stratum, thereby providing a single metric that can be meaningfully compared across diverse socioeconomic measures (whether using categories that emphasize the extremes or yield more equal distributions, e.g., quintiles).64–66 In Step 4, we summarized findings across ABSMs and geographic levels, in relation to our above-mentioned a priori considerations regarding external validity, robustness, completeness, and user-friendliness of each measure. All analyses were conducted in SAS.67
Finally, to consolidate our key findings, we devised a “scaled relative index of inequality plot,” in which we display the relative index of inequality for a given ABSM divided by the median value for all the ABSMs being compared. This plot facilitates determining which ABSMs were likely to detect relative indexes of inequality similar to, higher than, or lower than the median relative index of inequality, for each given outcome, at each geographic level, for each race/ethnicity–gender group. To address concerns pertaining to unreliable data, results for outcomes with less than 5 cases are suppressed, while those for outcomes with either 5 to 20 cases or 20 or more cases, and for which the width of the 95% confidence interval is 2 times or more the value of the relative index of inequality, are separately flagged.
RESULTS
Table 1 ▶ presents data on the study base, defined in terms of both population and areas (block group, census tract, and zip code), as enumerated in the 1990 census for Massachusetts and Rhode Island, which respectively included approximately 6 million and 1 million residents. As shown in Table 2 ▶, about half the White population (both women and men) in both states lived in areas where fewer than 5% of persons lived below the poverty line; by contrast, over half of the Black and Hispanic populations lived in areas where the poverty rate was 20% or more (same for women and men). Similar patterns were evident for the ABSM for low education and, more starkly, the Townsend index, with no notable difference by gender within racial/ethnic groups.
TABLE 1—
Study Population, Public Health Disparities Geocoding Project—Adults, by Race/Ethnicity and Gender, and Areas, by Level of Geography: Massachusetts and Rhode Island, 1990
| Massachusetts | Rhode Island | |||||||
| Total | % | Women | Men | Total | % | Women | Men | |
| Population (1990) | 6016425 | 3129948 | 2886477 | 1003464 | 522114 | 481350 | ||
| White | 5411774 | 89.9 | 2819665 | 2592109 | 919073 | 91.6 | 479800 | 439273 |
| Black | 297006 | 4.9 | 154030 | 142976 | 37986 | 3.8 | 18854 | 19132 |
| Hispanic | 275859 | 4.6 | 141147 | 134712 | 43932 | 4.4 | 21960 | 21972 |
| American Indian | 12585 | 0.2 | 6620 | 5965 | 4267 | 0.4 | 2204 | 2063 |
| Asian/Pacific Islander | 140745 | 2.3 | 70547 | 70198 | 17615 | 1.8 | 8934 | 8681 |
| N | Mean | SD | Range | N | Mean | SD | Range | |
| Areas (1990) | ||||||||
| Block groups | 5603 | 1085.4 | 665.2 | 5–10096 | 897 | 1137.7 | 670.8 | 7–5652 |
| Census tracts | 1331 | 4571.8 | 2080.0 | 18–15411 | 235 | 4325.3 | 1810.9 | 26–9822 |
| Zip codes | 474 | 12719.7 | 12244.1 | 14–65001 | 70 | 14335.2 | 13234.8 | 63–53763 |
TABLE 2—
Distribution of the Population for the Public Health Disparities Geocoding Project, Stratified by Block Group–, Census Tract–, and Zip Code–Level Area-Based Socioeconomic Measures, Race/Ethnicity, and Gender: Massachusetts and Rhode Island, 1990
| Massachusetts | Rhode Island | |||||||||||
| White | Black | Hispanic | White | Black | Hispanic | |||||||
| ABSM | N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | N | (%) |
| Poverty (categorical), % | ||||||||||||
| BG | ||||||||||||
| 0–4.9 | 2 751 888 | (50.9) | 41 027 | (13.8) | 35 870 | (13.0) | 403 507 | (44.0) | 3 439 | (9.1) | 4 318 | (9.9) |
| 5.0–9.9 | 1 363 080 | (25.2) | 42 151 | (14.2) | 35 597 | (12.9) | 277 185 | (30.2) | 5 243 | (13.9) | 6 269 | (14.3) |
| 10.0–19.9 | 838 315 | (15.5) | 70 156 | (23.6) | 55 316 | (20.1) | 138 953 | (15.1) | 6 822 | (18.1) | 6 851 | (15.6) |
| 20–100 | 453 877 | (8.4) | 143 400 | (48.3) | 148 850 | (54.0) | 97 701 | (10.7) | 22 245 | (58.9) | 26 347 | (60.2) |
| CT | ||||||||||||
| 0–4.9 | 2 462 306 | (45.5) | 27 423 | (9.2) | 27 849 | (10.1) | 377 676 | (41.2) | 2 731 | (7.2) | 3 716 | (8.5) |
| 5.0–9.9 | 1 728 663 | (32.0) | 49 493 | (16.7) | 44 797 | (16.2) | 269 275 | (29.3) | 4 993 | (13.2) | 4 807 | (11.0) |
| 10.0–19.9 | 798 485 | (14.8) | 70 404 | (23.7) | 57 020 | (20.7) | 195 495 | (21.3) | 8 915 | (23.6) | 10 861 | (24.8) |
| 20–100 | 418 676 | (7.7) | 149 517 | (50.4) | 146 059 | (53.0) | 75 316 | (8.2) | 21 154 | (56.0) | 24 433 | (55.8) |
| ZC | ||||||||||||
| 0–4.9 | 2 196 407 | (40.6) | 25 233 | (8.5) | 25 420 | (9.2) | 199 126 | (21.7) | 1 128 | (3.0) | 1 457 | (3.3) |
| 5.0–9.9 | 1 784 636 | (33.0) | 45 596 | (15.4) | 49 308 | (17.9) | 461 245 | (50.2) | 8 625 | (22.7) | 7 171 | (16.3) |
| 10.0–19.9 | 1 117 857 | (20.7) | 88 949 | (29.9) | 89 436 | (32.4) | 203 391 | (22.1) | 15 460 | (40.7) | 14 504 | (33.0) |
| 20–100 | 312 867 | (5.8) | 137 228 | (46.2) | 111 695 | (40.5) | 55 311 | (6.0) | 12 773 | (33.6) | 20 800 | (47.3) |
| Low education (categorical), % | ||||||||||||
| BG | ||||||||||||
| 0–14.9 | 2 488 369 | (46.0) | 49 370 | (16.6) | 42 416 | (15.4) | 212 623 | (23.1) | 4 193 | (11.0) | 3 331 | (7.6) |
| 15.0–24.9 | 1 525 764 | (28.2) | 61 190 | (20.6) | 40 161 | (14.6) | 252 207 | (27.4) | 3 180 | (8.4) | 2 479 | (5.6) |
| 25.0–39.9 | 987 678 | (18.3) | 108 873 | (36.7) | 75 912 | (27.5) | 290 457 | (31.6) | 8 644 | (22.8) | 8 278 | (18.8) |
| 40–100 | 409 851 | (7.6) | 77 450 | (26.1) | 117 332 | (42.5) | 163 786 | (17.8) | 21 969 | (57.8) | 29 844 | (67.9) |
| CT | ||||||||||||
| 0–14.9 | 2 261 944 | (41.8) | 42 569 | (14.3) | 36 822 | (13.3) | 142 306 | (15.5) | 3 660 | (9.6) | 2 670 | (6.1) |
| 15.0–24.9 | 1 839 913 | (34.0) | 68 539 | (23.1) | 50 295 | (18.2) | 313 258 | (34.1) | 6 127 | (16.1) | 3 476 | (7.9) |
| 25.0–39.9 | 959 725 | (17.7) | 126 459 | (42.6) | 91 816 | (33.3) | 315 690 | (34.3) | 5 448 | (14.3) | 7 353 | (16.7) |
| 40–100 | 350 080 | (6.5) | 59 316 | (20.0) | 96 888 | (35.1) | 147 819 | (16.1) | 22 751 | (59.9) | 30 433 | (69.3) |
| ZC | ||||||||||||
| 0–14.9 | 2 042 089 | (37.7) | 33 138 | (11.2) | 33 863 | (12.3) | 150 152 | (16.3) | 4 629 | (12.2) | 2 235 | (5.1) |
| 15.0–24.9 | 2 075 209 | (38.3) | 71 227 | (24.0) | 71 401 | (25.9) | 243 270 | (26.5) | 4 598 | (12.1) | 2 568 | (5.8) |
| 25.0–39.9 | 1 020 759 | (18.9) | 157 593 | (53.1) | 108 260 | (39.2) | 368 287 | (40.1) | 11 756 | (30.9) | 12 998 | (29.6) |
| 40–100 | 273 710 | (5.1) | 35 048 | (11.8) | 62 335 | (22.6) | 157 364 | (17.1) | 17 003 | (44.8) | 26 131 | (59.5) |
| Townsend index (categorical) | ||||||||||||
| BG | ||||||||||||
| 1 (most resources) | 1 073 403 | (19.8) | 9 618 | (3.2) | 10 452 | (3.8) | 185 534 | (20.2) | 620 | (1.6) | 1 275 | (2.9) |
| 2 | 1 229 164 | (22.7) | 15 248 | (5.1) | 13 557 | (4.9) | 211 306 | (23.0) | 1 314 | (3.5) | 2 310 | (5.3) |
| 3 | 1 228 922 | (22.7) | 22 595 | (7.6) | 20 240 | (7.3) | 205 142 | (22.4) | 3 596 | (9.5) | 2 914 | (6.7) |
| 4 | 1 093 642 | (20.2) | 48 410 | (16.3) | 44 152 | (16.0) | 176 440 | (19.2) | 5 420 | (14.4) | 6 088 | (13.9) |
| 5 (least resources) | 784 731 | (14.5) | 201 047 | (67.7) | 187 425 | (68.0) | 138 924 | (15.1) | 26 799 | (71.0) | 31 198 | (71.3) |
| CT | ||||||||||||
| 1 (most resources) | 1 242 820 | (23.0) | 11 253 | (3.8) | 12 490 | (4.5) | 209 034 | (22.8) | 960 | (2.5) | 1 888 | (4.3) |
| 2 | 1 322 640 | (24.4) | 15 149 | (5.1) | 15 831 | (5.7) | 212 861 | (23.2) | 1 717 | (4.5) | 2 420 | (5.5) |
| 3 | 1 221 587 | (22.6) | 24 093 | (8.1) | 25 876 | (9.4) | 197 171 | (21.5) | 3 296 | (8.7) | 2 914 | (6.7) |
| 4 | 1041 083 | (19.2) | 55 712 | (18.8) | 55 520 | (20.1) | 188 484 | (20.5) | 6 925 | (18.3) | 6 291 | (14.4) |
| 5 (least resources) | 581 780 | (10.8) | 190 717 | (64.2) | 166 109 | (60.2) | 110 212 | (12.0) | 24 895 | (65.9) | 30 304 | (69.2) |
| ZC | ||||||||||||
| 1 (most resources) | 605 276 | (11.2) | 6 107 | (2.1) | 6 225 | (2.3) | 48 066 | (5.2) | 141 | (0.4) | 230 | (0.5) |
| 2 | 816 954 | (15.1) | 8 368 | (2.8) | 8 328 | (3.0) | 137 223 | (14.9) | 697 | (1.8) | 1 101 | (2.5) |
| 3 | 946 108 | (17.5) | 11 304 | (3.8) | 12 011 | (4.4) | 160 402 | (17.5) | 1 019 | (2.7) | 1 470 | (3.3) |
| 4 | 1 336 631 | (24.7) | 23 974 | (8.1) | 31 806 | (11.5) | 262 883 | (28.6) | 3 313 | (8.7) | 4 155 | (9.5) |
| 5 (least resources) | 1 706 798 | (31.5) | 247 253 | (83.2) | 217 489 | (78.8) | 310 499 | (33.8) | 32 816 | (86.4) | 36 976 | (84.2) |
Note. BG = block group; CT = census tract; ZC = zip code; ABSM = area-based socioeconomic measures.
Table 3 ▶ provides data on the number of cases for each outcome, by race/ethnicity and gender, and the percentage geocoded to the block group, census tract, and zip code level, which displayed little variation by race/ethnicity or gender. Overall, 93.7% of records were geocoded to the block group level, 99.5% to the census tract level, and 99.5% to the zip code level; only 0.6% were not geocoded to any of these 3 levels. All records geocoded to the block group and census tract level were linked to the relevant censusdefined areas. By contrast, at the zip code level, for several outcomes (especially birth, cancer incidence, and TB), often 10% to 15% of cases could not be linked to census zip code areas, because either their zip codes were for nonresidential sites or the zip codes were created or changed after the 1990 census.
TABLE 3—
Number of Cases for the Public Health Disparities Geocoding Project: Percentage Geocoded and Percentage Matched to Census Areas, by Level of Geography and Race/Ethnicity: Massachusetts and Rhode Island , ca. 1990
| % Geocoded and Matched to Census Areasa | ||||||||||||||
| BG Level | CT Level | ZC Level | ||||||||||||
| Mass | RI | Mass | RI | Mass | RI | Not Geocoded | ||||||||
| Total Cases | Mass | RI | ||||||||||||
| Data Source: Population | Mass | RI | Geo + Match | Geo + Match | Geo + Match | Geo + Match | Geo | Geo + Match | Geo | Geo + Match | N | (%) | N | (%) |
| Mortality (Mass, 1989–1991; RI, 1989–1991) | ||||||||||||||
| White women | 77 543 | 13 567 | 93.6 | 89.8 | 99.9 | 94.6 | 99.9 | 96.4 | 94.0 | 92.5 | 116 | (0.1) | 737 | (5.4) |
| White men | 69 994 | 12 682 | 93.8 | 92.2 | 99.8 | 95.8 | 99.9 | 96.5 | 95.3 | 93.5 | 141 | (0.2) | 528 | (4.2) |
| Black women | 2 448 | 372 | 95.8 | 94.1 | 99.8 | 97.0 | 99.8 | 98.1 | 97.0 | 96.8 | 6 | (0.2) | 11 | (3.0) |
| Black men | 3 025 | 501 | 96.4 | 94.4 | 99.6 | 97.2 | 99.6 | 97.3 | 96.4 | 95.6 | 13 | (0.4) | 14 | (2.8) |
| Hispanic women | 682 | 73 | 95.5 | 97.3 | 98.8 | 98.6 | 99.3 | 96.6 | 98.6 | 97.3 | 8 | (1.2) | 1 | (1.4) |
| Hispanic men | 1 150 | 172 | 95.4 | 95.9 | 98.9 | 96.5 | 99.1 | 96.7 | 96.5 | 95.3 | 13 | (1.1) | 6 | (3.5) |
| American Indian women | 31 | 28 | 80.6 | 89.3 | 100.0 | 92.9 | 100.0 | 96.8 | 89.3 | 89.3 | 0 | (0.0) | 2 | (7.1) |
| American Indian men | 67 | 48 | 88.1 | 87.5 | 98.5 | 91.7 | 98.5 | 95.5 | 91.7 | 89.6 | 1 | (1.5) | 4 | (8.3) |
| Asian/Pacific Islander women | 346 | 40 | 95.4 | 97.5 | 98.0 | 100.0 | 98.3 | 96.0 | 100.0 | 97.5 | 7 | (2.0) | 0 | (0.0) |
| Asian/Pacific Islander men | 456 | 44 | 93.9 | 100.0 | 97.1 | 100.0 | 97.1 | 93.6 | 100.0 | 100.0 | 13 | (2.9) | 0 | (0.0) |
| Low birthweight (Mass, 1989–1991; RI, 1987–1993) | ||||||||||||||
| White girls | 92 354 | 36 245 | 94.4 | 96.6 | 100.0 | 99.2 | 100.0 | 91.6 | 99.4 | 97.5 | 0 | (0.0) | 275 | (0.8) |
| White boys | 97 758 | 38 192 | 94.2 | 96.5 | 100.0 | 99.3 | 100.0 | 91.7 | 99.4 | 97.5 | 0 | (0.0) | 271 | (0.7) |
| Black girls | 9 562 | 3 405 | 96.9 | 97.7 | 100.0 | 99.0 | 100.0 | 92.4 | 99.7 | 98.2 | 0 | (0.0) | 33 | (1.0) |
| Black boys | 9 810 | 3 577 | 96.5 | 97.5 | 100.0 | 98.8 | 100.0 | 92.5 | 99.7 | 97.8 | 0 | (0.0) | 44 | (1.2) |
| Hispanic girls | 12 568 | 2 659 | 96.8 | 98.5 | 100.0 | 99.7 | 100.0 | 93.5 | 99.8 | 99.1 | 0 | (0.0) | 8 | (0.3) |
| Hispanic boys | 13 215 | 2 726 | 96.7 | 98.7 | 100.0 | 99.7 | 100.0 | 93.7 | 99.9 | 98.8 | 0 | (0.0) | 9 | (0.3) |
| American Indian girls | 232 | 411 | 92.7 | 94.9 | 100.0 | 98.1 | 100.0 | 94.0 | 98.3 | 98.1 | 0 | (0.0) | 8 | (1.9) |
| American Indian boys | 228 | 388 | 90.8 | 96.6 | 100.0 | 98.7 | 100.0 | 90.8 | 99.0 | 98.2 | 0 | (0.0) | 5 | (1.3) |
| Asian/Pacific Islander girls | 4 455 | 1 458 | 96.5 | 96.8 | 100.0 | 97.9 | 100.0 | 89.5 | 98.7 | 96.9 | 0 | (0.0) | 30 | (2.1) |
| Asian/Pacific Islander boys | 4 842 | 1 541 | 96.7 | 97.0 | 100.0 | 98.4 | 100.0 | 90.6 | 99.1 | 97.5 | 0 | (0.0) | 25 | (1.6) |
| Cancer incidence (Mass, 1988–1992; RI, 1989–1992) | ||||||||||||||
| White women | 79 252 | 9 817 | 92.1 | 91.3 | 100.0 | 99.7 | 100.0 | 89.3 | 99.8 | 99.1 | 7 | (0.0) | 25 | (0.3) |
| White men | 76 209 | 9 486 | 92.0 | 91.6 | 100.0 | 99.8 | 100.0 | 89.6 | 99.8 | 99.0 | 4 | (0.0) | 21 | (0.2) |
| Black women | 2 044 | 211 | 94.7 | 96.2 | 100.0 | 100.0 | 100.0 | 93.6 | 100.0 | 100.0 | 0 | (0.0) | 0 | (0.0) |
| Black men | 2 292 | 192 | 92.8 | 92.7 | 100.0 | 100.0 | 100.0 | 94.9 | 100.0 | 99.0 | 0 | (0.0) | 0 | (0.0) |
| Hispanic women | NA | 62 | 91.9 | 100.0 | 100.0 | 96.8 | 0 | (0.0) | ||||||
| Hispanic men | NA | 67 | 94.0 | 98.5 | 98.5 | 98.5 | 1 | (1.5) | ||||||
| Childhood lead poisoning (RI, 1994–1996) | ||||||||||||||
| White girls | 7 145 | 93.4 | 94.2 | 93.9 | 91.3 | 414 | (5.8) | |||||||
| White boys | 7 550 | 93.5 | 94.7 | 94.5 | 92.2 | 402 | (5.3) | |||||||
| Black girls | 1 032 | 97.3 | 97.9 | 97.9 | 97.9 | 22 | (2.1) | |||||||
| Black boys | 1 056 | 97.7 | 98.3 | 98.0 | 97.3 | 18 | (1.7) | |||||||
| Hispanic girls | 2 571 | 97.7 | 97.9 | 97.8 | 97.7 | 55 | (2.1) | |||||||
| Hispanic boys | 2 578 | 98.1 | 98.3 | 98.3 | 98.2 | 45 | (1.7) | |||||||
| Tuberculosis (Mass, 1993–1998; RI, 1985–1994) | ||||||||||||||
| White women | 284 | 145 | 90.1 | 90.3 | 100.0 | 93.1 | 100.0 | 84.2 | 91.7 | 90.3 | 0 | (0.0) | 10 | (6.9) |
| White men | 490 | 223 | 89.8 | 87.9 | 100.0 | 90.6 | 99.8 | 83.9 | 89.7 | 87.9 | 0 | (0.0) | 21 | (9.4) |
| Black women | 208 | 34 | 90.4 | 100.0 | 100.0 | 100.0 | 100.0 | 88.9 | 100.0 | 97.1 | 0 | (0.0) | 0 | (0.0) |
| Black men | 273 | 58 | 86.4 | 91.4 | 100.0 | 96.6 | 100.0 | 87.9 | 96.6 | 96.6 | 0 | (0.0) | 2 | (3.4) |
| Hispanic women | 93 | 34 | 88.2 | 97.1 | 100.0 | 100.0 | 100.0 | 83.9 | 97.1 | 97.1 | 0 | (0.0) | 0 | (0.0) |
| Hispanic men | 156 | 63 | 85.9 | 90.5 | 100.0 | 95.2 | 100.0 | 73.1 | 93.7 | 93.7 | 0 | (0.0) | 3 | (4.8) |
| Syphilis (Mass, 1994–1998; RI, 1994–1996) | ||||||||||||||
| White women | 128 | 27 | 83.6 | 88.9 | 100.0 | 88.9 | 100.0 | 98.4 | 88.9 | 88.9 | 0 | (0.0) | 3 | (11.1) |
| White men | 198 | 31 | 81.3 | 90.3 | 100.0 | 96.8 | 100.0 | 95.5 | 96.8 | 93.5 | 0 | (0.0) | 1 | (3.2) |
| Black women | 394 | 20 | 87.6 | 60.0 | 100.0 | 90.0 | 100.0 | 98.0 | 90.0 | 85.0 | 0 | (0.0) | 2 | (10.0) |
| Black men | 534 | 51 | 84.3 | 62.7 | 100.0 | 80.4 | 100.0 | 97.2 | 80.4 | 76.5 | 0 | (0.0) | 10 | (19.6) |
| Hispanic women | 313 | 50 | 91.1 | 88.0 | 100.0 | 94.0 | 100.0 | 95.8 | 94.0 | 92.0 | 0 | (0.0) | 3 | (6.0) |
| Hispanic men | 533 | 86 | 74.7 | 67.4 | 100.0 | 81.4 | 100.0 | 97.2 | 81.4 | 80.2 | 0 | (0.0) | 16 | (18.6) |
| Gonorrhea (Mass, 1994–1998; RI, 1994–1996) | ||||||||||||||
| White women | 701 | 259 | 90.3 | 94.6 | 100.0 | 95.4 | 100.0 | 96.9 | 95.4 | 94.2 | 0 | (0.0) | 12 | (4.6) |
| White men | 966 | 177 | 89.2 | 92.1 | 100.0 | 94.4 | 100.0 | 95.9 | 94.4 | 93.2 | 0 | (0.0) | 10 | (5.6) |
| Black women | 991 | 236 | 90.3 | 94.9 | 100.0 | 95.8 | 100.0 | 97.8 | 95.8 | 93.6 | 0 | (0.0) | 10 | (4.2) |
| Black men | 1 211 | 350 | 91.7 | 92.6 | 100.0 | 93.4 | 99.9 | 98.0 | 93.4 | 92.3 | 0 | (0.0) | 23 | (6.6) |
| Hispanic women | 479 | 94 | 90.8 | 92.6 | 100.0 | 93.6 | 100.0 | 97.5 | 92.6 | 92.6 | 0 | (0.0) | 6 | (6.4) |
| Hispanic men | 558 | 108 | 89.6 | 94.4 | 100.0 | 94.4 | 99.8 | 97.0 | 94.4 | 94.4 | 0 | (0.0) | 6 | (5.6) |
| Chlamydia (Mass, 1994–1998; RI, 1994–1996) | ||||||||||||||
| White women | 5 816 | 2 099 | 87.2 | 91.8 | 100.0 | 93.1 | 100.0 | 95.9 | 93.0 | 90.9 | 0 | (0.0) | 144 | (6.9) |
| White men | 734 | 269 | 87.9 | 83.6 | 100.0 | 85.1 | 100.0 | 95.8 | 85.1 | 82.5 | 0 | (0.0) | 40 | (14.9) |
| Black women | 3 104 | 864 | 90.7 | 92.4 | 100.0 | 93.9 | 100.0 | 97.5 | 93.8 | 91.4 | 0 | (0.0) | 53 | (6.1) |
| Black men | 1 062 | 276 | 88.8 | 90.2 | 100.0 | 91.3 | 100.0 | 96.2 | 91.3 | 89.1 | 0 | (0.0) | 24 | (8.7) |
| Hispanic women | 3 892 | 923 | 91.8 | 96.0 | 100.0 | 96.7 | 100.0 | 96.7 | 96.5 | 96.0 | 0 | (0.0) | 30 | (3.3) |
| Hispanic men | 690 | 185 | 84.9 | 93.5 | 100.0 | 95.1 | 100.0 | 95.7 | 95.1 | 94.6 | 0 | (0.0) | 9 | (4.9) |
| Nonfatal weapon-related injury (Mass, 1995–1997) | ||||||||||||||
| White women | 283 | 89.0 | 97.9 | 100.0 | 95.1 | 6 | (2.1) | |||||||
| White men | 1 812 | 87.7 | 96.9 | 100.0 | 93.8 | 57 | (3.1) | |||||||
| Black women | 262 | 87.0 | 97.7 | 100.0 | 95.0 | 6 | (2.3) | |||||||
| Black men | 1 413 | 84.1 | 94.6 | 100.0 | 91.8 | 77 | (5.4) | |||||||
| Hispanic women | 132 | 90.2 | 97.7 | 100.0 | 95.5 | 3 | (2.3) | |||||||
| Hispanic men | 1 091 | 86.8 | 96.4 | 100.0 | 93.8 | 39 | (3.6) | |||||||
Note. BG = block group; CT = census tract; ZC = zip code; NA = not available.
a“Geo + Match” = geocoded and matched to census area; “Geo” = geocoded but not able to be matched to census area.
Table 4 ▶ presents results for premature mortality for the Massachusetts census tract–level ABSMs and offers an illustration of the data we generated for each outcome, at each geographic level, for each ABSM, for each race/ethnicity–gender group, for both states (Appendix 3; available from the first author upon request). For each economic stratum of each ABSM, the table (men only) displays the number of cases, the denominator, the computed age-standardized rate, and the relative index of inequality (summarizing the socioeconomic gradient across all the economic strata); the incidence rate ratio, comparing rates among persons living in areas with the least versus most resources, is available from the first author. Thus, in the case of premature mortality, the median relative index of inequality for the 11 census tract–level ABSMs typically was 2 or higher in every race/ethnicity–gender group, with measures of economic deprivation most frequently detecting the steepest gradients. Among men, reliable estimates of the relative index of inequality ranged from a low of 0.9 (Black men: wealth ABSM) to a high of 3.4 (Asian and Pacific Islander men: poverty ABSM). Among women, reliable estimates of the relative index of inequality ranged from a low of 1.2 (Black women: wealth and working class ABSM) to a high of 3.2 (Asian and Pacific Islander women: Townsend ABSM).
TABLE 4—
Premature Mortality (<65 Years Old, Per 100 000a) Among Men, by Race/Ethnicity, Stratified by Census Tract–Level Area-Based Socioeconomic Measures, Massachusetts, 1989–1991: Public Health Disparities Geocoding Project
| White | Black | Hispanic | Asian/Pacific Islander | American Indian | ||||||||||||||||
| ABSM and Category | Cases | Pop | Rate | RII (95% CI) | Cases | Pop | Rate | RII (95% CI) | Cases | Pop | Rate | RII (95% CI) | Cases | Pop | Rate | RII (95% CI) | Cases | Pop | Rate | RII (95% CI) |
| Working class, % | ||||||||||||||||||||
| 0.0–49.9 | 2 468 | 1 137 351 | 187.7 | 2.1 (2.0, 2.3) | 168 | 38 739 | 475.3 | 1.4 (1.2, 1.6) | 46 | 30 192 | 196.7 | 2.1 (1.7, 2.7) | 51 | 53 667 | 113.0 | 2.4 (1.6, 3.7) | 4 | 1 749 | 211.0 | 1.3 (0.4, 4.4) |
| 50.0–65.9 | 8 660 | 3 227 388 | 255.5 | 451 | 108 090 | 448.8 | 167 | 100 566 | 200.2 | 75 | 76 779 | 116.2 | 11 | 6 639 | 165.9 | |||||
| 66.0–74.9 | 5 901 | 1 837 386 | 311.1 | 705 | 159 258 | 487.8 | 271 | 108 252 | 276.3 | 44 | 38 745 | 140.3 | 10 | 5 316 | 212.0 | |||||
| 75.0–100.0 | 2 569 | 669 279 | 402.1 | 485 | 100 686 | 573.2 | 389 | 155 535 | 329.6 | 55 | 33 732 | 231.0 | 6 | 3 171 | 208.6 | |||||
| Median household income, $ | ||||||||||||||||||||
| > 47 125 | 3 714 | 1 736 397 | 186.9 | 2.6 (2.5, 2.8) | 64 | 24 648 | 262.6 | 2.7 (2.3, 3.2) | 22 | 24 234 | 112.5 | 2.8 (2.2, 3.5) | 41 | 39 291 | 101.9 | 2.7 (1.8, 4.2) | 3 | 2 142 | 129.9 | 7.1 (1.9, 27.2) |
| 39 287–47 124 | 4 299 | 1 663 815 | 242.4 | 108 | 33 093 | 351.7 | 41 | 27 369 | 158.3 | 16 | 28 494 | 69.8 | 0 | 2 772 | 0.0 | |||||
| 33 163–39 286 | 4 359 | 1 466 310 | 286.0 | 216 | 64 140 | 363.8 | 73 | 43 749 | 195.0 | 47 | 36 156 | 173.3 | 8 | 3 081 | 230.2 | |||||
| 26 472–33 162 | 3 913 | 1 183 224 | 328.1 | 516 | 120 399 | 471.4 | 198 | 96 201 | 263.5 | 41 | 42 144 | 124.5 | 5 | 4 311 | 162.2 | |||||
| 4 999–26 471 | 3 313 | 818 049 | 446.0 | 905 | 162 303 | 648.9 | 539 | 202 362 | 333.6 | 80 | 56 775 | 207.1 | 15 | 4 524 | 372.3 | |||||
| Poverty, % | ||||||||||||||||||||
| 0.0–4.9 | 7 563 | 3 203 058 | 212.7 | 2.6 (2.5, 2.8) | 107 | 42 777 | 280.9 | 2.7 (2.2, 3.2) | 52 | 41 931 | 134.6 | 2.8 (2.2, 3.6) | 44 | 54 798 | 84.6 | 3.4 (2.2, 5.2) | 4 | 4 314 | 86.4 | 6.3 (1.7, 22.8) |
| 5.0–9.9 | 6 397 | 2 145 999 | 285.3 | 217 | 69 978 | 342.2 | 100 | 64 854 | 181.2 | 51 | 48 780 | 129.7 | 8 | 5 220 | 166.6 | |||||
| 10.0–19.9 | 3 485 | 983 442 | 356.7 | 422 | 96 048 | 478.2 | 182 | 81 999 | 281.9 | 46 | 38 985 | 149.3 | 7 | 3 318 | 234.3 | |||||
| 20.0–100 | 2 153 | 537 120 | 484.8 | 1063 | 197 895 | 610.6 | 539 | 205 635 | 332.4 | 84 | 60 312 | 211.8 | 12 | 3 978 | 371.7 | |||||
| Gini index | ||||||||||||||||||||
| 0.009–0.348 | 4 019 | 1 708 737 | 227.5 | 1.6 (1.5, 1.7) | 114 | 43 965 | 284.7 | 2.9 (2.5, 3.5) | 35 | 31 692 | 123.8 | 2.6 (2.1, 3.3) | 26 | 26 082 | 111.4 | 2.3 (1.5, 3.6) | 1 | 3 294 | 31.7 | 6.8 (1.8, 25.6) |
| 0.349–0.371 | 4 173 | 1 535 217 | 255.3 | 105 | 40 929 | 288.6 | 62 | 40 221 | 193.9 | 30 | 33 390 | 96.5 | 6 | 2 490 | 244.6 | |||||
| 0.372–0.395 | 4 194 | 1 490 193 | 260.2 | 200 | 51 504 | 413.2 | 114 | 58 449 | 205.3 | 36 | 36 339 | 109.8 | 3 | 3 171 | 115.1 | |||||
| 0.396–0.428 | 4 056 | 1 257 159 | 307.4 | 398 | 96 168 | 469.2 | 222 | 100 536 | 282.7 | 44 | 40 950 | 160.1 | 8 | 4 143 | 211.8 | |||||
| 0.429–0.650 | 3 156 | 876 489 | 347.1 | 992 | 172 017 | 642.6 | 440 | 163 017 | 340.0 | 89 | 66 099 | 182.7 | 13 | 3 732 | 380.4 | |||||
| Wealth, % | ||||||||||||||||||||
| 20.0–100 | 2 046 | 905 262 | 191.5 | 1.9 (1.8, 2.0) | 175 | 30 165 | 623.0 | 0.9 (0.7, 1.2) | 54 | 24 726 | 255.6 | 1.4 (1.0, 2.0) | 52 | 42 669 | 130.4 | 1.1 (0.7, 1.8) | 6 | 1 488 | 392.2 | 0.2 (0.1, 1.0) |
| 10.0–19.9 | 1 440 | 576 903 | 223.8 | 59 | 16 953 | 340.2 | 32 | 17 166 | 233.9 | 14 | 11 277 | 152.0 | 4 | 1 539 | 230.6 | |||||
| 5.0–9.9 | 1 964 | 707 640 | 251.4 | 143 | 33 015 | 455.1 | 28 | 18 831 | 168.7 | 21 | 16 884 | 120.6 | 2 | 1 314 | 109.2 | |||||
| 0.0–4.9 | 1 3 919 | 4 643 028 | 295.5 | 1 366 | 317 397 | 484.6 | 694 | 318 000 | 267.4 | 133 | 126 078 | 138.0 | 14 | 12 243 | 130.2 | |||||
| Crowding, % | ||||||||||||||||||||
| 0.0–4.9 | 17 504 | 6 324 546 | 258.2 | 3.3 (3.0, 3.5) | 640 | 172 611 | 410.6 | 1.6 (1.4, 1.9) | 337 | 176 184 | 219.5 | 1.7 (1.3, 2.1) | 131 | 132 219 | 112.3 | 3.0 (1.9, 4.6) | 22 | 12 753 | 175.1 | 0.9 (0.2, 5.3) |
| 5.0–9.9 | 1 422 | 383 601 | 437.0 | 590 | 115 011 | 579.7 | 258 | 99 579 | 338.7 | 51 | 41 889 | 179.6 | 2 | 2 280 | 72.7 | |||||
| 10.0–19.9 | 572 | 147 078 | 497.3 | 508 | 103 203 | 546.0 | 229 | 99 378 | 295.8 | 25 | 20 700 | 196.1 | 4 | 1 683 | 265.5 | |||||
| 20.0–100 | 100 | 12 570 | 911.8 | 71 | 13 758 | 539.6 | 49 | 18 774 | 294.9 | 18 | 8 052 | 262.3 | 3 | 114 | 1 987.9 | |||||
| Low education, % | ||||||||||||||||||||
| 0.0–14.9 | 6 525 | 2 920 797 | 204.0 | 2.4 (2.3, 2.6) | 202 | 63 957 | 344.1 | 2.3 (2.0, 2.8) | 75 | 53 625 | 187.0 | 2.4 (1.9, 3.0) | 65 | 82 701 | 95.1 | 3.3 (2.1, 5.0) | 11 | 5 739 | 178.7 | 2.8 (0.8, 9.7) |
| 15.0–24.9 | 7 074 | 2 333 658 | 291.9 | 340 | 95 100 | 397.0 | 119 | 73 434 | 172.4 | 60 | 53 778 | 135.4 | 3 | 4 686 | 58.1 | |||||
| 25.0–39.9 | 4 323 | 1 198 464 | 357.9 | 812 | 168 933 | 528.6 | 310 | 129 690 | 294.1 | 57 | 42 762 | 172.6 | 12 | 4 125 | 318.4 | |||||
| 40.0–100 | 1 677 | 422 184 | 402.1 | 455 | 78 759 | 687.7 | 369 | 137 799 | 337.3 | 43 | 23 766 | 241.7 | 5 | 2 340 | 282.5 | |||||
| Townsend index | ||||||||||||||||||||
| −8.123 to −2.797 | 3 554 | 1 609 386 | 190.7 | 2.7 (2,6, 2.9) | 50 | 18 390 | 287.4 | 2.7 (2.3, 3.3) | 27 | 18 618 | 187.7 | 2.7 (2.0, 3.4) | 23 | 27 171 | 80.9 | 3.0 (1.8, 4.6) | 4 | 2 274 | 144.0 | 4.8 (1.3, 17.2) |
| −2.796 to −1.596 | 4 287 | 1 711 941 | 234.2 | 58 | 22 704 | 256.1 | 25 | 22 956 | 123.2 | 22 | 23 496 | 111.2 | 3 | 3 024 | 82.3 | |||||
| −1.595 to −0.051 | 4 368 | 1 521 165 | 273.9 | 99 | 33 333 | 319.5 | 50 | 36 825 | 146.9 | 27 | 26 673 | 112.9 | 6 | 3 579 | 219.8 | |||||
| −0.050 to 2.860 | 4 281 | 1 282 509 | 339.1 | 273 | 78 378 | 427.2 | 178 | 79 506 | 261.6 | 52 | 49 983 | 135.6 | 3 | 3 429 | 95.4 | |||||
| 2.861 to 11.223 | 3 108 | 746 451 | 470.1 | 1 329 | 253 968 | 581.3 | 593 | 236 640 | 319.5 | 101 | 75 600 | 195.9 | 15 | 4 569 | 383.3 | |||||
| CDCILER | ||||||||||||||||||||
| 20–26 | 3 995 | 1 799 544 | 193.5 | 2.4 (2.3, 2.6) | 120 | 33 924 | 387.7 | 2.2 (1.9, 2.6) | 50 | 31 869 | 190.8 | 2.8 (2.2, 3.6) | 47 | 54 429 | 94.5 | 3.4 (2.2, 5.1) | 3 | 2 460 | 100.0 | 4.4 (1.3, 15.5) |
| 16–19 | 3 709 | 1 450 092 | 242.5 | 109 | 32 022 | 359.2 | 27 | 27 087 | 136.2 | 33 | 32 310 | 131.2 | 3 | 2 394 | 100.5 | |||||
| 11–15 | 5515 | 1 839 060 | 289.3 | 163 | 54 567 | 361.0 | 82 | 55 227 | 157.5 | 37 | 42 588 | 100.8 | 6 | 3 330 | 182.9 | |||||
| 6–10 | 3491 | 1 091 622 | 325.3 | 475 | 107 718 | 459.3 | 184 | 76 107 | 283.5 | 36 | 32 700 | 151.1 | 6 | 3 942 | 231.6 | |||||
| 0–5 | 2888 | 691 134 | 437.5 | 942 | 178 542 | 613.4 | 530 | 204 255 | 332.9 | 72 | 40 896 | 246.8 | 13 | 4 749 | 317.9 | |||||
| SEP1b | ||||||||||||||||||||
| 1 (most resources) | 1 991 | 937 200 | 179.5 | 2.4 (2.3, 2.6) | 129 | 27 288 | 500.6 | 1.8 (1.5, 2.1) | 34 | 21 852 | 185.2 | 2.1 (1.7, 2.6) | 39 | 37 794 | 113.9 | 3.0 (2.0, 4.7) | 4 | 1 146 | 308.8 | 1.3 (0.3, 4.5) |
| 2 | 1 373 | 524 109 | 235.4 | 86 | 16 938 | 516.6 | 27 | 12 294 | 325.4 | 11 | 10 965 | 114.9 | 6 | 1 656 | 412.4 | |||||
| 3 | 438 | 198 441 | 220.2 | 26 | 11 160 | 263.1 | 8 | 7 710 | 189.1 | 9 | 14 691 | 89.7 | 0 | 579 | 0.0 | |||||
| 4 | 12 353 | 4 318 989 | 273.7 | 518 | 151 362 | 371.1 | 218 | 127 887 | 189.6 | 84 | 82 077 | 117.1 | 8 | 8 604 | 88.7 | |||||
| 5 | 1 460 | 416 673 | 351.7 | 67 | 14 532 | 581.6 | 68 | 27 045 | 316.8 | 6 | 7 614 | 57.4 | 2 | 1 062 | 217.3 | |||||
| 6 | 697 | 188 562 | 440.2 | 506 | 92 481 | 610.2 | 159 | 60 735 | 310.8 | 22 | 18 114 | 194.4 | 3 | 1 560 | 602.4 | |||||
| 7 (least resources) | 1 051 | 243 006 | 491.6 | 410 | 83 487 | 575.4 | 294 | 120 975 | 325.7 | 49 | 25 521 | 282.2 | 3 | 1 917 | 152.1 | |||||
| SEP index | ||||||||||||||||||||
| −13.768 to −3.265 | 3 264 | 1 523 331 | 184.9 | 2.5 (2.5, 2.7) | 121 | 31 938 | 411.0 | 2.2 (1.8, 2.6) | 35 | 27 054 | 151.2 | 2.8 (2.2, 3.6) | 44 | 47 403 | 100.9 | 3.2 (2.1, 5.0) | 4 | 1 908 | 190.0 | 1.5 (0.4, 5.4) |
| −3.264 to −1.153 | 3 948 | 1 612 971 | 231.6 | 97 | 31 716 | 326.1 | 41 | 27 429 | 226.2 | 21 | 26 148 | 96.2 | 6 | 3 168 | 161.3 | |||||
| −1.152 to 0.396 | 4 641 | 1 571 037 | 284.7 | 157 | 40 029 | 456.5 | 63 | 41 865 | 161.9 | 42 | 40 602 | 120.1 | 5 | 3 381 | 163.6 | |||||
| 0.397 to 3.006 | 4 377 | 1 345 047 | 321.7 | 302 | 90 357 | 365.1 | 136 | 72 450 | 215.5 | 38 | 37 884 | 135.1 | 2 | 3 600 | 90.3 | |||||
| 3.007 to 20.605 | 3 133 | 772 827 | 427.7 | 1 065 | 201 093 | 597.0 | 533 | 209 196 | 325.9 | 75 | 44 724 | 234.2 | 9 | 4 467 | 248.3 | |||||
| Median | 2.4 | 2.2 | 2.6 | 3.0 | 2.8 | |||||||||||||||
Note. RII = relative index of inequality; CI = confidence interval; Pop = population; CDCILER = Centers for Disease Control and Prevention’s Index of Economic Resources; CT = census tract; ABSM = area-based socioeconomic measures. For SEP1 and SEP index, see “Methods” section.
aAge-standardized to the year 2000 standard million.
bSEP1: 1 = any poverty, < 50% working class, ≥10% wealth; 2 = any poverty, 51%–74% working class, ≥10% wealth; 3 = any poverty, < 50% working class, < 10% wealth; 4 = < 20% poverty, 51%–74% working class, < 10% wealth; 5 = ≤20% poverty, ≥75% working class, any wealth; 6 = ≥20% poverty, 51%–74% working class, < 10% wealth; 7 = ≥20% poverty, ≥75% working class, any wealth.
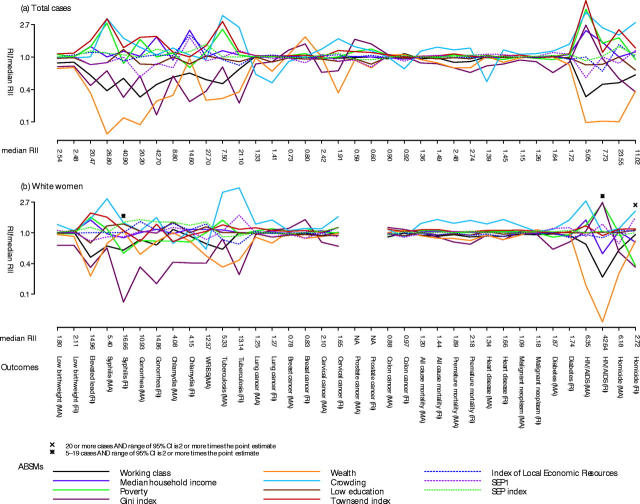
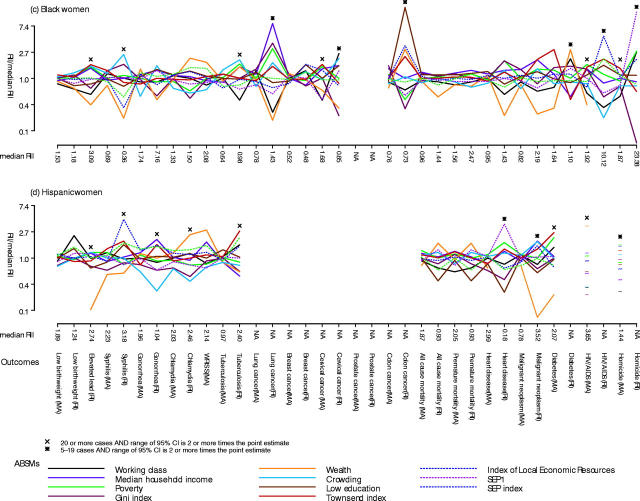
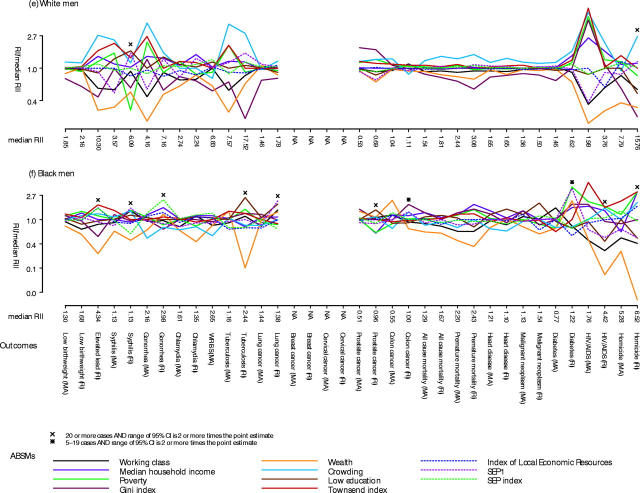
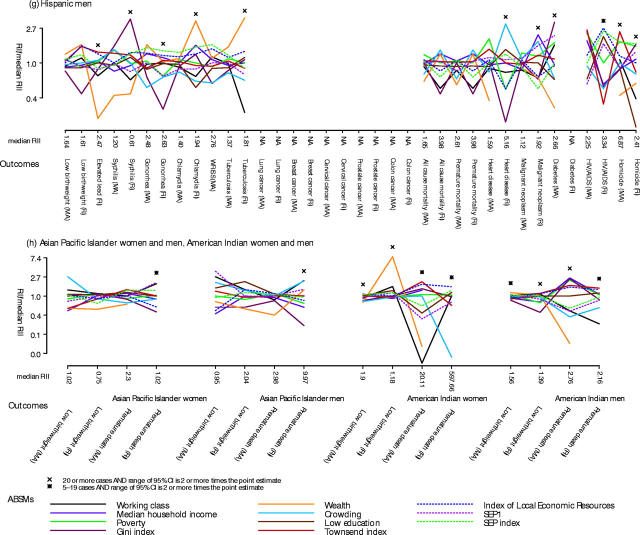
Building on these analyses, Figure 1 ▶ employs the scaled relative index of inequality plot to summarize our findings for the census tract–level ABSMs across all outcomes for the total population and for the different race/ethnicity–gender groups. Four results stand out, which held for analyses at each geographic level (plots at the block group and zip code level available from the first author upon request). First, within both the total population and each race/ethnicity–gender group, the relative index of inequality for most ABSMs was close to the median for virtually all outcomes, suggesting that the impact of socioeconomic position on a given health outcome is robust. Second, measures of economic deprivation—such as the percentage of persons below poverty (the dark green line) and the Townsend index (the bright red line)—were most sensitive to expected socioeconomic gradients in health, with their relative indexes of inequality routinely at or above the median. By contrast, relative indexes of inequality for measures of wealth and income inequality generally fell below the median, and those for measures of education hovered around the median. Third, these patterns were especially evident for HIV mortality, homicide, TB, and sexually transmitted infections, for which much larger (and expected24–26) gradients were detected by ABSMs for economic deprivation compared with other ABSMs. Fourth, for virtually all outcomes, the median relative index of inequality typically was largest for the White population and smallest for the Black population.
FIGURE 1—
Scaled relative index of inequality (RII) plot, with ln (RII/median RII) for the 11 area-based socioeconomic measures (ABSMs) at the census tract level (Massachusetts, ca. 1990) for all health outcomes for (a) total population, (b) White women, (c) Black women, (d) Hispanic women, (e) White men, (f) Black men, (g) Hispanic men, and (h) for low birthweight and premature mortality only for Asian and Pacific Islander and American Indian women and men, from The Public Health Disparities Geocoding Project.
Note. MA = Massachusetts; RI = Rhode Island; WRISS = Weapons-Related Injury Surveillance System. For explanation of SEP1 and SEP index, see “Methods” section.
Two findings, however, differed by geographic level (data not shown; available from the first author upon request). First, in each race/ethnicity–gender group, the block group and census tract median relative indexes of inequality for most outcomes resembled each other (with the block group estimate often slightly larger), whereas the zip code median relative index of inequality variously was larger or smaller than the block group or the census tract median relative index of inequality. Second, as reported previously for the total population,48 in each of the race/ethnicity–gender groups, only zip code–level analyses yielded parameter estimates contrary to what has been reported in the literature (e.g., they detected a positive socioeconomic gradient when most research has reported a negative gradient).
DISCUSSION
Taken together, our results suggest that aptly chosen ABSMs can meaningfully augment US public health surveillance systems to permit routine monitoring of socioeconomic inequalities in health within diverse race/ethnicity–gender groups as well as the total population. Three key findings pertinent to selecting a particular ABSM at a particular level stand out. First, census tract–level analyses yielded the most consistent results with maximal geocoding linkage (i.e., the highest proportion of records both geocoded and linked to census-defined areas). Second, measures of economic deprivation were most sensitive to expected socioeconomic gradients in health. Third, the single-variable measure “percentage of persons below poverty” performed as well as more complex, composite measures of economic deprivation (e.g., the Townsend index). These findings, in conjunction with our a priori criteria pertaining to external validity, robustness, completeness, and user-friendliness, accordingly suggest that the census tract–level measure “percentage of persons below poverty” would be a plausible candidate variable. Also important would be use of a priori categorical cutpoints (including the policy-relevant 20% below poverty57,58) to facilitate meaningful comparisons across time and space.
In evaluating our results, it is important to consider several possible sources of bias and error, as well as issues regarding interpretation and use of ABSMs. First, bias could result if a person’s socioeconomic position were associated with being included in a given public health surveillance system, having an erroneous or ungeocodable address, or living in an area missing ABSM data.6,15 If, for example, these problems occurred more frequently among poorer persons, estimates of socioeconomic gradients would be deflated; if, less plausibly, these problems chiefly affected affluent persons, the estimate would be inflated. In our prior research, however, with the 2 databases containing individual-level socioeconomic data (birth and death), we found no variation by educational level in the proportion of records geocoded at each geographic level.24,25
Second, misclassification of race/ethnicity and differential census undercounts by race/ethnicity and socioeconomic position could also affect parameter estimates.14 In both cases, however, the resultant biases would be operative at each geographic level and thus would not invalidate comparisons of socioeconomic gradients across ABSMs or geographic levels. Moreover, only a tiny proportion of areas (typically under 1%) lacked data on ABSMs and, to minimize geocoding error, we used a geocoding firm whose accuracy we validated.28 Third, from a temporal standpoint, cross-sectional analysis cannot address issues of etiologic period; simultaneity of measurement of ABSMs and health outcomes, however, is appropriate for monitoring, given the goal of quantifying the population burden of ill health in relation to socioeconomic position.24–26
Use of ABSMs nevertheless does raise several concerns. First, associations between ABSMs and health status likely reflect a complex combination of 3 factors: (1) composition (people in poor areas have poor health because poor people, as individuals, have poor health), (2) context (people in poor areas also have poor health because a concentration of poverty creates or exacerbates harmful social interactions), and (3) location of public goods or environmental conditions (poor areas are less likely to have good supermarkets and are more likely to be situated next to industrial plants, thereby harming health of their residents).12,21,68–71
Ascertaining the relative contribution of each of these factors—a task relevant for etiologic research—would necessitate multilevel models with relevant individual-level and area-based data69–72 (i.e., precisely the data that most US public health surveillance systems lack). Germane to compositional effects, however, the handful of US studies comparing effect estimates using area-based and individual-level socioeconomic data in conjunction with individual health data have found effect estimates in the same direction, often with similar magnitude (at the block group and census tract levels, but not the zip code level).15,73–75 Multilevel models, moreover, additionally suggest that, for at least some health outcomes, area- and individual-level socioeconomic factors independently and jointly shape the population distributions of disease.68–72
A second concern pertains to “ecologic fallacy,” which occurs when both the dependent and independent variables are group-level data and confounding is introduced through the grouping process.69,76 This type of aggregation bias, however, is not germane to the method of appending ABSMs to individual records, because individuals constitute the unit of observation for both the dependent variable (health outcomes) and the independent variable (exposure to area-based socioeconomic conditions).15,24–26 Instead, as for any research using areal measures, at issue is whether the areas and contingent areal measures are meaningful entities51,71,77; in the case of monitoring, this translates to whether the areas and ABSMs are apt for characterizing the social contours of the population burden of disease.15,24–26 In the case of census tracts, not only are initial boundaries delineated to demarcate relatively economically homogeneous populations, as previously noted,45(pG-10,G-11) but these administrative areas also affect residents’ lives because they are used by federal, state, and local governments to plan programs and allocate resources—for example, to define “urban empowerment zones,” to designate “medically underserved areas,” and to delimit city neighborhoods served by public health agencies.
A third related concern is whether ABSMs meaningfully measure conditions experienced by all persons residing in the specified area, especially in areas marked by socioeconomic heterogeneity.21,49,71 Indeed, it was this concern which led us to investigate whether use of different geographic areas matters, and whether different patterns are seen for members of diverse race/ethnicity–gender groups. Our principal finding—that census tract and block group ABSMs yield similar parameter estimates, whereas zip code estimates are less consistent—importantly held, however, for both the total population and specified subpopulations. These results are consonant with other studies, especially in the United Kingdom, and support the view that one advantage of ABSMs is that they can be applied equally to all persons, regardless of age, gender, and employment status, thereby avoiding well-known problems associated with occupation- and education-based measures—that is, how to classify people not in the paid-labor force (children, housewives or househusbands, unemployed or retired persons) or who have not yet completed their education (school-age children and young adults).6,15,21,53,78
Concerns about ABSMs and the evidence addressing them thus suggests that while use of ABSMs for public health monitoring requires judicious interpretation, the information gained can usefully offset current gaps in knowledge due to the absence of socioeconomic data in most US public health surveillance systems. With these data, it becomes feasible to monitor socioeconomic gradients within diverse race/ethnicity–gender groups; by extension, the magnitude of race/ethnicity–gender inequality in health within specified economic strata could be assessed—as could the contribution of economic deprivation to racial/ethnic and gender disparities in health.12,15
For example, data in our study provided noteworthy evidence that economic gradients were steepest in the White population and shallowest in the Black population. Far from suggesting that economic inequality is less of a concern for African Americans’ health, these findings chiefly resulted from absolute rates being higher among Black compared with White Americans in areas with the most resources. In addition to underscoring that both absolute and relative rates must be considered when evaluating health disparities,65,79,80 these results emphasize why analyses of racial/ethnic inequalities in health need to take into account economic disparities and, conversely, why analyses of economic inequalities in health need to take into account racial/ethnic disparities.13,14,81
Relevant to future use of ABSMs are 2 additional considerations. The first is that starting with the year 2000 census, zip code–level data are no longer available and databases with only zip codes cannot be linked to census data absent geocoding to some other geographic level for which census data are available.48 Prompting this change were “difficulties in precisely defining the land area covered by each ZIP Code,”82 leading the US Census Bureau to create a new statistical entity built from census blocks: the 5-digit Zip Code Tabulation Area (ZCTA).83 Since ZCTAs and zip codes sharing the same 5-digit code may not necessarily cover the same area,83 zip codes obtained by self-report or from addresses in medical records cannot be assumed to correspond to census-defined ZCTAs.48
Second, regarding the timeliness of census data, pending authorization and funding by Congress, the decennial census long form (source of the socioeconomic data for the ABSMs) is scheduled to be replaced by the annual American Community Survey, which will provide yearly sociodemographic estimates at the national, state, and other geographic levels.84 Data at the census tract level are anticipated to be released starting in 2008, employing annual estimates based on 5-year rolling averages; less certainly, block group–level data may also be released starting in 2009 (C. Richard, senior program analyst, American Community Survey, oral communication, January 8, 2003). Presumably, a similar methodology, employing 5-year rolling averages, could also be used for health data among smaller population subgroups, thereby enabling the routine monitoring of socioeconomic inequalities in health among all race/ethnicity–gender groups, assuming that concerns about validity and consistency of racial/ethnic data across public health data systems could be addressed.14,85
In conclusion, results of our study highlight the importance of multilevel frameworks, including ecosocial theory, for public health research and practice.22,23,68–72,86–89 Tellingly, were data constrained only to the individual level, we would remain without any practical solution for improving routine monitoring of socioeconomic inequalities in the United States, other than continuing to advocate for inclusion of individual-level socioeconomic data in diverse public health surveillance systems. Even if it were possible to overcome resistance to including such measures5,90—let alone ensure use of identical measures across diverse databases to enable meaningful comparison—it would still not be possible to monitor secular trends in socioeconomic inequalities in health, owing to the absence of the individual-level socioeconomic data from previous years. By expanding the levels of analysis to include characteristics of areas in which people reside, it is instead possible to envision—and test—an alternative solution, that of geocoding and using ABSMs. By the same logic, further elaboration of multilevel frameworks and methods is likely to aid efforts to understand and address the persistent problem of social inequalities in health in the United States.22,23,68–72,86–91 One way to begin is by ensuring that the magnitude of these disparities is duly and routinely monitored, rather than hidden from view. We suggest that this can be accomplished by geocoding US public health surveillance systems and using the census tract–level measure “percentage of persons below poverty.”
Acknowledgments
This work was funded by the National Institutes of Health’s National Institute of Child Health and Human Development (1 R01 HD36865–01) and Office of Behavioral and Social Science Research (principal investigator, N. Krieger, PhD).
We thank Dr Daniel Friedman (assistant commissioner, Bureau of Health Statistics, Research and Evaluation, Massachusetts Department of Health) and Dr Jay Buechner (chief, Office of Health Statistics, Rhode Island Department of Health) for facilitating the conduct of this study using data from their respective health departments and for their helpful comments on our manuscript. We likewise thank the following health department staff for their contributions to accessing the study’s data:
Massachusetts Department of Public Health: Alice Mroszczyk, program coordinator for 24A/B/111B Review Committee; Cancer Registry: Dr Susan Gershman, director, Mary Mroszczyk, geocoding/special projects coordinator, and Ann R. MacMillan, data analyst; Registry of Vital Records and Statistics: Elaine Trudeau, registrar of vital records, and Charlene Zion, Public Information Office; Infectious Diseases: Alfred DeMaria, assistant commissioner, Yuren Tang, chief of Surveillance Program, and Sharon Sharnprapai, TB epidemiologist; Weapons-Related Injury Surveillance System: Victoria Vespe Ozonoff, program director, Beth Hume, data manager/analyst, Patrice Cummins, epidemiologist, and Laurie Janelli, site coordinator;
Rhode Island Department of Health: Vital Statistics: Roberta Chevoya, state registrar of vital records; Division of Disease Prevention and Control: Dr John Fulton, associate director, Ted Donnelly, senior public health epidemiologist, and Michael Goscminksi, epidemiologist; Environmental Health Risk Assessment: Susan Feeley, public health epidemiologist; Childhood Lead Poisoning Prevention: Magaly Angeloni, program manager.
Human Participant Protection Use of the data employed in this study was approved by all relevant institutional review boards/human subjects committees at the Harvard School of Public Health, the Massachusetts Department of Public Health, and the Rhode Island Department of Health.
Contributors N. Krieger conceived and designed the study, directed data analysis, and led the writing. J. T. Chen contributed to the study design, led the data analysis, and assisted with manuscript preparation. P. D. Waterman contributed to the study design, secured the data, and assisted with data analysis, interpretation, and manuscript preparation. D. H. Rehkopf assisted with the study and analyses. S. V. Subramanian assisted with the study design and data interpretation. All authors helped to conceptualize ideas, interpret findings, and review drafts of the manuscript.
Peer Reviewed
References
- 1.Health, United States, 1998 With Socioeconomic Status and Health Chartbook. Hyattsville, Md: National Center for Health Statistics; 1998.
- 2.Leon D, Walt G, eds. Poverty, Inequality, and Health: An International Perspective. Oxford, England: Oxford University Press; 2001.
- 3.Marmot M, Wilkinson RG, eds. Social Determinants of Health. Oxford, England: Oxford University Press; 1999.
- 4.Berkman L, Kawachi I, eds. Social Epidemiology. Oxford, England: Oxford University Press; 2000.
- 5.Krieger N, Chen JT, Ebel G. Can we monitor socioeconomic inequalities in health? A survey of US Health Departments’ data collection and reporting practices. Public Health Rep. 1997;112:481–491. [PMC free article] [PubMed] [Google Scholar]
- 6.Krieger N, Williams D, Moss N. Measuring social class in US public health research: concepts, methodologies and guidelines. Annu Rev Public Health. 1997;18:341–378. [DOI] [PubMed] [Google Scholar]
- 7.Tolson GC, Barnes JM, Gay GA, Kowaleski JL. The 1989 revision of the US standard certificates and reports. Vital Health Stat 4. 1991;No. 28. [PubMed]
- 8.National Center for Health Statistics. National Health Interview Survey. Available at: http://www.cdc.gov/nchs/nhis.htm. Accessed January 1, 2003.
- 9.Pollack AM, Rice DP. Monitoring health care in the United States—a challenging task. Public Health Rep. 1997;112:108–113. [PMC free article] [PubMed] [Google Scholar]
- 10.Health, United States 2002 With Chartbook on Trends in the Health of Americans. Hyattsville, Md: National Center for Health Statistics; 2002.
- 11.Healthy People 2010. Conference ed, 2 vol. Washington, DC: US Dept of Health and Human Services; 2000:objective 23–3. Available at: http://www.health.gov/healthypeople. Accessed January 1, 2003.
- 12.Krieger N, Zierler S, Hogan JW, et al. Geocoding and measurement of neighborhood socioeconomic position: a US perspective. In: Kawachi I, Berkman L, eds. Neighborhoods and Health. Oxford, England: Oxford University Press; 2003:147–178.
- 13.Krieger N, Rowley D, Hermann AA, Avery B, Phillips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. Am J Prev Med. 1993;9(suppl):82–122. [PubMed] [Google Scholar]
- 14.Williams DR. Race/ethnicity and socioeconomic status: measurement and methodological issues. Int J Health Serv. 1996;26:483–505. [DOI] [PubMed] [Google Scholar]
- 15.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lynch J, Kaplan G. Socioeconomic position. In: Berkman L, Kawachi I, eds. Social Epidemiology. Oxford, England: Oxford University Press; 2000:13–35.
- 17.Nathan WB. Health Conditions in North Harlem 1923–1927. New York, NY: National Tuberculosis Association; 1932.
- 18.Green HW. The use of census tracts in analyzing the population of a metropolitan community. J Am Stat Assoc. 1933;28:147–153. [Google Scholar]
- 19.Terris M. Relation of economic status to tuberculosis mortality by age and sex. Am J Public Health. 1948;38:1061–1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coulter EJ, Guralnick L. Analysis of vital statistics by census tract. J Am Stat Assoc. 1959;54:730–740. [Google Scholar]
- 21.Carstairs V. Socio-economic factors at areal level and their relationship with health. In: Elliott P, Wakefield J, Best N, Briggs D, eds. Spatial Epidemiology: Methods and Applications. Oxford, England: Oxford University Press; 2000:51–67.
- 22.Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med. 1994;39:887–903. [DOI] [PubMed] [Google Scholar]
- 23.Krieger N. Theories for social epidemiology for the 21st century: an ecosocial perspective. Int J Epidemiol. 2001;30:668–677. [DOI] [PubMed] [Google Scholar]
- 24.Krieger N, Chen JT, Waterman PD, Soobader M-J, Subramanian SV, Carson R. Geocoding and monitoring US socioeconomic inequalities in mortality and cancer incidence: does choice of area-based measure and geographic level matter? The Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156:471–482. [DOI] [PubMed] [Google Scholar]
- 25.Krieger N, Chen JT, Waterman PD, Soobader M-J, Subramanian SV, Carson R. Choosing area-based socioeconomic measures to monitor social inequalities in low birthweight and childhood lead poisoning—The Public Health Disparities Geocoding Project (US). J Epidemiol Community Health. 2003;57:186–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krieger N, Chen JT, Waterman PD, Soobader M-J, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures—The Public Health Disparities Geocoding Project (US). Public Health Rep. 2003;118:240–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rossi RJ, Gilmartin KJ. The Handbook of Social Indicators: Sources, Characteristics, and Analysis. New York, NY: Garland STPM Press; 1980.
- 28.Krieger N, Waterman P, Lemieux K, Zierler S, Hogan JW. On the wrong side of the tracts? Evaluating accuracy of geocoding for public health research. Am J Public Health. 2001;91:1114–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Massachusetts Dept of Public Health, Division of Research and Epidemiology. Massachusetts death data. Available at: http://www.state.ma.us/dph/bhsre/resep/resep.htm. Accessed January 3, 2003.
- 30.Rhode Island Dept of Health. Office of Vital Records. Available at: http://www.health.ri.org/management/vital/home.htm. Accessed January 3, 2003.
- 31.International Classification of Diseases, Ninth Revision, Clinical Modification [computer file]. 6th ed. Washington, DC: Centers for Disease Control and Prevention, Health Care Financing Administration; 2000.
- 32.Massachusetts Dept of Public Health. Massachusetts Cancer Registry. Available at: http://www.state.ma.us/dph/bhsre/mcr/canreg.htm. Accessed January 3, 2003.
- 33.Rhode Island Dept of Health. Cancer Control Program, Rhode Island Cancer Registry. Available at: http://www.health.state.ri.us/disease/cancer/canreg.htm. Accessed January 3, 2003.
- 34.Reis LAG, Eisner MP, Kosary CL, et al., eds. SEER Cancer Statistics Review, 1973–1999. Bethesda, Md: National Cancer Institute; 2002. Available at: http://seer.cancer.gov/csr/1973_1999. Accessed January 1, 2003.
- 35.Massachusetts Dept of Public Health, Division of Research and Epidemiology. Massachusetts birth data. Available at: http://www.state.ma.us/dph/bhsre/resep/resep.htm. Accessed January 3, 2003.
- 36.Rhode Island Dept of Health. Rhode Island Lead Screening Plan (October2000). Available at: http://www.health.state.ri.us/family/lead/screeningplan.pdf. Accessed January 3, 2003.
- 37.Screening Young Children for Lead Poisoning: Guidance for State and Local Public Health Officials. Atlanta, Ga: Public Health Service, Centers for Disease Control and Prevention; 1997.
- 38.Massachusetts Dept of Public Health. 1998. Annual STD Report. Bureau of Communicable Disease Control, Division of Sexually Transmitted Disease Prevention. Available at: http://www.state.ma.us/dph/cdc/std/reports/std98.pdf. Accessed January 1, 2003.
- 39.Rhode Island Dept of Health. Communicable diseases in Rhode Island: diseases spread through sex (sexually transmitted diseases). Available at: http://www.health.state.ri.us/disease/communicable/dis_sex.htm. Accessed January 1, 2003.
- 40.Massachusetts Dept of Public Health. 2000 tuberculosis overview. Bureau of Communicable Disease Control, Division of Tuberculosis Prevention and Control. Available at: http://www.state.ma.us/dph/cdc/tb/tbstat2000.pdf. Accessed January 1, 2003.
- 41.Rhode Island Dept of Health. Tuberculosis. Available at: http://www.healthri.org/disease/communicable/tb.htm. Accessed January 1, 2003.
- 42.Massachusetts Dept of Public Health. Weapon injury data (April2001). Available at: http://www.state.ma.us/dph/bhsre/isp/wrisp/pubs/windata/01wpinjdata.pdf. Accessed January 1, 2003.
- 43.Census of Population and Housing, 1990: Summary Tape File 3 Technical Documentation. Washington, DC: Bureau of the Census; 1991.
- 44.US Bureau of the Census. American Factfinder. Available at: http://factfinder.census.gov. Accessed November 7, 2002.
- 45.Geographical Areas Reference Manual. Washington, DC: US Bureau of the Census; 1994. Available at: http://www.census.gov/geo/www/garm.html. Accessed January 1, 2003.
- 46.US Bureau of Census. Geographics changes for Census 2000 + glossary. Available at: http://www.census.gov/geo/www/tiger/glossary.html. Accessed January 1, 2003.
- 47.Address Information Products Technical Guide. Memphis, Tenn: US Postal Service National Customer Support Center; 2001.
- 48.Krieger N, Waterman P, Chen JT, Soobader M-J, Subramanian SV, Carson R. Zip code caveat: bias due to spatiotemporal mismatches between zip codes and US census–defined areas—The Public Health Disparities Geocoding Project. Am J Public Health. 2002;92:1100–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee P, Murie A, Gordon D. Area Measures of Deprivation: A Study of Current Methods and Best Practices in the Identification of Poor Areas in Great Britain. Birmingham, England: Centre for Urban and Regional Studies, University of Birmingham; 1995.
- 50.Cowell FA. Measuring Inequality. 2nd ed. London: Prentice Hall; 1995. LSE Handbooks in Economics Series.
- 51.Soobader M, LeClere FB. Aggregation and the measurement of income inequality: effects on morbidity. Soc Sci Med. 1999;48:733–744. [DOI] [PubMed] [Google Scholar]
- 52.Townsend P, Phillimore P, Beattie A. Health and Deprivation: Inequality and the North. London, England: Croom Helm; 1988.
- 53.Carstairs V, Morris R. Deprivation and mortality: an alternative to social class? Community Med. 1989;11:210–219. [DOI] [PubMed] [Google Scholar]
- 54.Casper ML, Barnett E, Halverson JA, et al. Women and Heart Disease: An Atlas of Racial and Ethnic Disparities in Mortality. Morgantown: Office for Social Environment and Health Research, West Virginia University; 1999.
- 55.Lawley DN, Maxwell AE. Factor Analysis as a Statistical Method. New York, NY: Macmillan Publishing Co; 1971.
- 56.Bartholomew DJ. Latent Variable Models and Factor Analysis. London, England: Charles Griffin & Co; 1987.
- 57.US Bureau of the Census. Poverty areas. Available at: http://www.census.gov/population/socdemo/statbriefs/povarea.html. Accessed January 1, 2003.
- 58.Jargowsky PA. Poverty and Place: Ghettos, Barrios, and the American City. New York, NY: Russell Sage Foundation; 1997.
- 59.Breslow NE, Day NE, eds. Statistical Methods in Cancer Research, Vol. II: The Design and Analysis of Cohort Studies. Oxford, England: Oxford University Press; 1987:54.
- 60.Rothman KJ, Greenland S. Modern Epidemiology. 2nd ed. Philadelphia, Pa: Lippincott-Raven; 1998:263.
- 61.Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998;37(3). [PubMed]
- 62.Breslow NE, Day NE. Statistical Methods in Cancer Research: Vol. I. The Analysis of Case–Control Studies. Lyon, France: International Agency for Research on Cancer; 1980:47. IARC Scientific Publication 32. [PubMed]
- 63.Boyle P, Parkin DM. Statistical methods for registries. In: Jensen OM, Parkin DM, MacLennan R, et al., eds. Cancer Registration: Principles and Methods. Lyon, France: International Agency for Research on Cancer; 1991:126–158. IARC Scientific Publication 95. [PubMed]
- 64.Pamuk ER. Social class inequality in mortality from 1921 to 1972 in England and Wales. Popul Stud. 1985;39:17–31. [DOI] [PubMed] [Google Scholar]
- 65.Wagstaff A, Paci P, van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33:545–557. [DOI] [PubMed] [Google Scholar]
- 66.Davey Smith G, Hart C, Hole D, et al. Education and occupational social class: which is the more important indicator of mortality risk? J Epidemiol Community Health. 1998;52:153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.SAS/STAT User’s Guide, Version 6. 4th ed, vol 1. Cary, NC: SAS Institute Inc; 1989.
- 68.Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55:125–139. [DOI] [PubMed] [Google Scholar]
- 69.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21:171–192. [DOI] [PubMed] [Google Scholar]
- 70.Jones K, Duncan C. Individuals and their ecologies: analysing the geography of chronic illness within a multilevel modelling framework. Health Place. 1995;1:27–40. [Google Scholar]
- 71.O’Campo P. Invited commentary: advancing theory and methods for multilevel models of residential neighborhoods and health. Am J Epidemiol. 2003;157:9–13. [DOI] [PubMed] [Google Scholar]
- 72.Subramanian SV, Jones K, Duncan C. Multilevel methods for public health research. In: Kawachi I, Berkman L, eds. Neighborhoods and Health. Oxford, England: Oxford University Press; 2003:65–111.
- 73.Krieger N. Women and social class: a methodological study comparing individual, household, and census measures as predictors of black/white differences in reproductive history. J Epidemiol Community Health. 1991;45:35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Geronimus AT, Bound J, Neidert LJ. On the validity of using census geocode data to proxy individual socioeconomic characteristics. J Am Stat Assoc. 1996;91:529–537. [Google Scholar]
- 75.Soobader M, LeClere FB, Hadden W, Maury B. Using aggregate geographic data to proxy individual socioeconomic status: does size matter? Am J Public Health. 2001;91:632–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Alker HR Jr. A typology of ecologic fallacies. In: Doggan M, Rokkan S, eds. Social Ecology. Cambridge, Mass: MIT Press; 1969:69–86.
- 77.Oppenshaw S, Taylor PJ. The modifiable areal unit problem. In: Wrigley N, Bennett RJ, eds. Quantitative Geography. London, England: Routledge & Kegan Paul; 1981:60–69.
- 78.Sorensen A. Women, family, and class. Annu Rev Sociol. 1994;20:27–47. [Google Scholar]
- 79.Lahelma E, Manderbacka K, Rahkonen O, Karisto A. Comparisons of inequalities in health: evidence from national surveys in Finland, Norway and Sweden. Soc Sci Med. 1994;38:517–524. [DOI] [PubMed] [Google Scholar]
- 80.Borrell C, Rue M, Pasarin MI, Benach J, Kunst AE. The measurement of inequalities in health. Gac Sanit. 2000;14(suplemento 3):20–33.11459557 [Google Scholar]
- 81.Krieger N. Does racism harm health? Did child abuse exist before 1962? On explicit questions, critical science, and current controversies: an ecosocial perspective. Am J Public Health. 2003;93:194–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.US Bureau of the Census. Census 2000 ZIP Code Tabulation Areas (ZCTAs). Available at: http://www.census.gov/geo/ZCTA/zcta.html. Accessed January 1, 2003.
- 83.US Bureau of the Census. Census 2000 ZCTAs ZIP Code Tabulation Areas technical documentation. Available at: http://www.census.gov/geo/ZCTA/zcta_tech_doc.pdf. Accessed January 1, 2003.
- 84.US Bureau of the Census. American Community Survey: what are the supplementary surveys? Available at: http://www.census.gov/acs/www/Sbasics/What/What2.htm. Accessed December 14, 2002.
- 85.Laws MB, Heckscher RA. Racial and ethnic identification practices in public health data systems in New England. Public Health Rep. 2002;117:50–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Anderson NB. Levels of analysis in health science. A framework for integrating sociobehavioral and biomedical research. Ann N Y Acad Sci. 1998;840:563–576. [DOI] [PubMed] [Google Scholar]
- 87.McMichael AJ. Prisoners of the proximate: loosening the constraints on epidemiology in an age of change. Am J Epidemiol. 1999;149:887–897. [DOI] [PubMed] [Google Scholar]
- 88.Susser M, Susser E. Choosing a future for epidemiology, II: from black boxes to Chinese boxes and eco-epidemiology. Am J Public Health. 1996;86:674–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McKinlay JB, Marceau LD. To boldly go. . . . Am J Public Health. 2000;90:25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Krieger N, Fee E. Measuring social inequalities in health in the United States: an historical review, 1900–1950. Int J Health Serv. 1996;26:391–418. [DOI] [PubMed] [Google Scholar]
- 91.Friedman DJ, Hunter EL, Parrish RG. Shaping a vision of health statistics for the 21st century. Washington, DC: Centers for Disease Control and Prevention, National Center for Health Statistics, National Committee on Vital and Health Statistics; 2002. Available at: http://www.ncvhs.hhs.gov/hsvision. Accessed March 8, 2003.