Abstract
Objectives. We sought to examine whether physician recommendations for cardiac revascularization vary according to patient race.
Methods. We studied patients scheduled for coronary angiography at 2 hospitals, one public and one private, between November 1997 and June 1999. Cardiologists were interviewed regarding their recommendations for cardiac resvacularization.
Results. African American patients were less likely than Whites to be recommended for revascularization at the public hospital (adjusted odds ratio [OR] = 0.31; 95% confidence interval [CI] = 0.12, 0.77) but not at the private hospital (adjusted OR = 1.69; 95% CI = 0.69, 4.14).
Conclusions. Physician recommendations for cardiac revascularization vary by patient race. Further studies are needed to examine physician bias as a factor in racial disparities in cardiac care and outcomes.
Cardiovascular diseases are still a major cause of mortality and morbidity in the developed world, including the United States.1–3 Thirteen million Americans have been diagnosed with coronary artery disease, and more than 7 million have had myocardial infarctions.1 Each year, more than 1 million Americans experience a myocardial infarction.1 Moreover, cardiovascular disease is the leading cause of death among both White and African Americans; in fact, death rates from cardiovascular causes among African Americans are among the highest in the industrialized world.2,4,5
In addition to early prevention and recognition, one of the primary strategies for reducing cardiovascular deaths has been the use of cardiac revascularization. Improved technology for assessing cardiovascular diseases, combined with the fact that about half of all myocardial infarctions occurring in the United States each year represent recurrent infarctions, has led to the rise of cardiac revascularization rates in the past 2 decades.5 For example, between 1987 and 1990 alone, rates of percutaneous transluminal angioplasty (PTCA) and coronary artery bypass grafting (CABG) increased by 55% and 18%, respectively, in the United States.6 The increased use of these procedures has resulted in lower short- and long-term mortality and morbidity rates among patients with coronary artery disease.6
Given the similar burden of cardiovascular diseases in African Americans and Whites and the increasing safety and efficacy of revascularization, one would expect relatively little racial/ethnic disparity in the use of this treatment. However, numerous studies have reported widespread racial disparities in cardiac revascularization rates, particularly between African American and White patients.7–11 This racial/ethnic disparity has generated concern given that cardiovascular diseases cause disproportionate mortality and morbidity in the African American community,2,12–14 which is one of the reasons why cardiovascular diseases are included in the 6 key health conditions targeted in the national effort to eliminate racial/ethnic disparities in health care by 2010.15
As is the case with disparities in other health conditions, the reasons for racial/ethnic disparities in cardiac revascularization rates remain poorly understood, but they have been hypothesized to include factors at the patient, provider, and system levels. Relatively few studies have examined provider or system factors that may contribute to these disparities. In one recent study conducted by Hannan et al., physicians were less likely to recommend revascularization to African American patients than to White patients, even in the case of patients who had a clinically indicated need for revascularization and who were similar in terms of disease status.16 The authors suggested that provider incentives may play a role in this disparity and called for further investigation. We report here a study that examined physician recommendations for revascularization among African American and White patients who had coronary angiographies (cardiac catheterization) at 2 health care facilities.
METHODS
Study Population
The present study evaluated all patients scheduled for coronary angiography at a Department of Veterans Affairs (VA) hospital and a university hospital during November 1997 through June 1999. The 2 hospitals are located in the same city in the northeastern United States, and both are tertiary care centers affiliated with a university program that performs PTCA and CABG.
Using the cardiac catheterization schedule, study staff identified all patients who were scheduled for coronary angiography during the study period. Transplant patients, patients scheduled for intervention angioplasty, and those undergoing primary or emergency angioplasty were ineligible. Consecutive eligible patients were approached by a study research assistant, except in instances in which multiple procedures performed simultaneously prevented all such patients from being approached; in these cases, the research assistant preferentially approached patients who appeared, on the basis of physical characteristics, to be African American. The present report includes only those patients who had at least one significant stenosis, defined as 70% or greater stenosis of any single epicardial vessel or 50% or greater stenosis of the left main coronary artery.
Data Collection
Trained research assistants of mixed racial/ethnic backgrounds contacted patients during the usual weekday business hours of 9 am to 5 pm to inquire about their interest in participating in the study. Structured and semistructured questionnaires were used to gather information from patients. Patients were surveyed regarding demographic characteristics, socioeconomic status (SES), and health status, as well as their knowledge, expectations, and attitudes regarding cardiac revascularization. Research assistants identified patients’ race on the basis of physical characteristics.
A total of 46 cardiologists and cardiology fellows from the 2 sites (the VA and the university hospital) were interviewed for the study. Specifically, cardiologists who delivered recommendations concerning revascularization to patients provided information for the study. Most cardiologists returned the survey regarding their recommendations immediately after reviewing procedure results or shortly after delivering a recommendation to the patient.
The primary outcome of interest in the present analysis was the cardiologists’ response to the question “Would you recommend revascularization for this patient?” (yes or no). In the case of patients not offered revascularization, cardiologists were asked to indicate a reason why either PTCA or CABG was not recommended. Response options included insignificant amount of myocardium at risk, insignificant disease, coronary anatomy is such that the chances of technical success are low, surgical risk is excessive, social situation makes intervention not feasible, and patient likely to refuse. Physicians were also given an option to write in a reason if the applicable one was not present on the list of options provided.
A trained research assistant, under the supervision of a physician, reviewed each patient’s coronary angiography reports to collect data regarding previous cardiac revascularization procedures and coronary anatomy. We classified disease severity as mild (disease involves 1–2 vessels and does not involve proximal left anterior descending artery), moderate (disease involves 1–2 vessels and involves proximal left anterior descending artery), or severe (disease involves left main coronary artery or 3 vessels). Throughout the period of data collection, the study coordinator reviewed each data abstraction form to ensure completeness and accuracy. A physician reviewed the classification of a 10% random sample of coronary angiography charts throughout the period to ensure ongoing quality.
Statistical Analysis
We compared baseline clinical and demographic characteristics of African American and White patients using χ2 tests (for categorical variables) and Student’s t tests (for continuous variables). At the univariate level, we used simple χ2 tests to assess associations between patient race and recommendation for revascularization according to procedure site. Also at the univariate level, we assessed associations between recommendations for revascularization and selected predictors such as gender, age, educational level, self-assessed health status, history of revascularization, disease severity, and procedure site. We then used logistic regression models to calculate the adjusted relationship between recommendation for revascularization and patient race, adjusting for appropriate covariates. All covariates were added into the model simultaneously.
The initial model included all variables. Because gender and a Gender × Race interaction term were not significant (Ps = .126 and .217, respectively) in the initial model, they were removed from the final model (the variables included in the final model are presented in Table 3 ▶ as a footnote). In addition, we assessed the effect of clustering of patients under cardiologists by including a random effect for cardiologist in the final model and using a generalized estimating equation (GEE) model. Because this effect also was nonsignificant, we based our conclusions on the unadjusted model. We used SPSS 10.0 (Stata Corp, College Station, Tex) in conducting all analyses other than those involving the GEE model, for which we used Stata 7.0 (SPSS Inc, Chicago, Ill).
TABLE 3—
Crude and Adjusted Odds of African American Patients (vs White Patients) Receiving Recommendations, by Site of Procedure
| Site | Crude Odds Ratio (95% Confidence Interval) | Adjusteda Odds Ratio (95% Confidence Interval) |
| VA hospital | 0.36 (0.13, 0.93) | 0.31 (0.12, 0.77) |
| University hospital | 1.37 (0.56, 3.70) | 1.69 (0.69, 4.14) |
aAdjusted for age, disease severity, history of revascularization, educational level, and health status.
RESULTS
Baseline Characteristics
Overall, 1109 patients agreed to participate in the study and had data from the angiography on number of stenotic (diseased) vessels; 316 patients had no stenosis on angiography and were eliminated from this analysis. One patient whose race was identified as other than African American or White was also excluded, resulting in a final sample for analysis of 792 patients. Table 1 ▶ summarizes sample baseline characteristics. There was a significant difference (P = .03) in overall health status reports between African American and White patients (not shown in Table 1 ▶), with African Americans generally rating their health status as lower.
TABLE 1—
Sample Baseline Characteristics, by Race
| Characteristic | African American (n = 54) | White (n = 738) | P |
| Age, y, mean (SD) | 61 (12) | 64 (10) | .12 |
| Male, % | 74 | 85 | .03 |
| High school education or more, % | 83 | 77 | .29 |
| History of revascularization, % | 33 | 46 | .08 |
| Disease severity,a % | .01 | ||
| Mild | 54 | 34 | |
| Moderate | 11 | 13 | |
| Severe | 35 | 53 | |
| Site of procedure, % | .65 | ||
| VA hospital | 48 | 51 | |
| University hospital | 52 | 49 |
aMild = 1–2-vessel disease not involving proximal left anterior descending (PLAD) artery; moderate = 1–2-vessel disease involving PLAD; severe = disease of left main coronary artery or 3-vessel disease.
Physician Recommendations for Revascularization
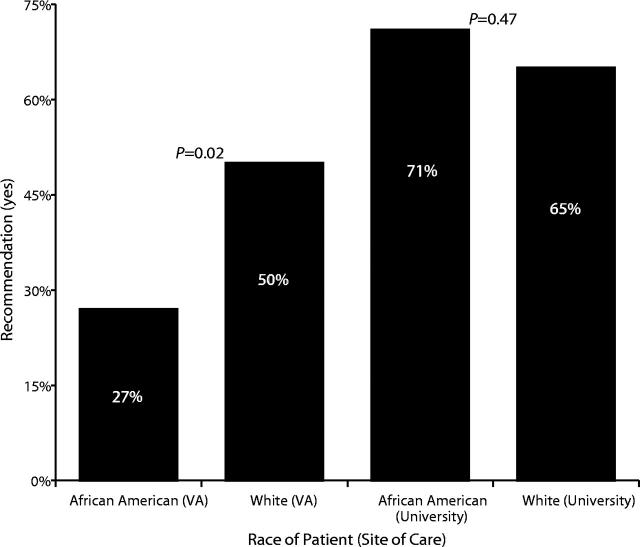
Cardiologists reported that they recommended revascularization for 27% of African Americans and 50% of Whites (P = .02) treated at the VA hospital and for 71% and 65% of African Americans and Whites, respectively, treated at the university hospital (P = .47; Figure 1 ▶). In both samples, female gender, high school education level or higher, no history of revascularization, higher disease severity, and site (i.e., university) were all individually, and significantly, associated with recommendations for revascularization (Table 2 ▶).
FIGURE 1—
Recommendations for percutaneous transluminal angioplasty and coronary artery bypass grafting, by race of patient and site of care.
TABLE 2—
Univariate Associations Between Predictors and Recommendations
| Recommendation Within Category, % | P | |
| Gender | .001 | |
| Male | 55 | |
| Female | 70 | |
| Education | .006 | |
| More than high school | 59 | |
| High school or less | 48 | |
| History of revascularization | .000 | |
| Yes | 44 | |
| No | 67 | |
| Disease severitya | .008 | |
| Mild | 49 | |
| Moderate | 60 | |
| Severe | 61 | |
| Site of procedure | .000 | |
| VA hospital | 49 | |
| University hospital | 65 |
aMild = 1–2-vessel disease not involving proximal left anterior descending (PLAD) artery; moderate = 1–2-vessel disease involving PLAD; severe = disease of left main coronary artery or 3-vessel disease.
In the VA sample, the adjusted odds ratio for African American patients (vs White patients) receiving a recommendation for revascularization from a cardiologist was 0.31 (95% confidence interval [CI] = 0.12, 0.75; P = .007). At the university site, the adjusted odds ratio was 1.69 (95% CI = 0.72, 4.40; P = .21; Table 3 ▶). Site, cardiac disease severity, education level, health status, and previous revascularization remained significant independent predictors in the multivariate model.
Reasons for Not Recommending Revascularization
Because physician recommendations for revascularization varied by patient race only at the VA site, we summarize in Table 4 ▶ the most frequent reasons offered by cardiologists at this site for not recommending either PTCA or CABG to African American and White patients. The 3 most frequent reasons for not offering PTCA to African American patients were insignificant myocardium at risk (9 patients), low chance of technical success (7 patients), and need for additional testing (4 patients). Among White patients, the 3 most frequent reasons were insignificant myocardium at risk (95 patients), low chance of technical success (92 patients), and insignificant disease (35 patients).
TABLE 4—
Most Frequent Reasons for Not Recommending Revascularization: VA Site
| Procedure and Reason | African American Patients, No. (%) | White Patients, No. (%) |
| PTCA | ||
| Insignificant myocardium at risk | 9 (33) | 95 (30) |
| Low chance of technical success | 7 (26) | 92 (29) |
| Additional testing needed | 4 (16) | 93 (11) |
| CABG | ||
| Insignificant myocardium at risk | 7 (26) | 101 (36) |
| CABG not technically feasible | 5 (16) | 64 (21) |
| Additional testing needed | 2 (7) | 37 (12) |
Note. PTCA = percutaneous transluminal angioplasty; CABG = coronary artery bypass grafting.
The most frequent reasons offered by physicians for not recommending CABG to African American patients were insignificant myocardium at risk (7 patients), insignificant disease (5 patients), CABG not technically feasible (5 patients), and too few vessels requiring revascularization (5 patients). Among White patients, the most frequent reasons were insignificant myocardium at risk (101 patients), CABG not technically feasible (64 patients), and insignificant disease (37 patients).
DISCUSSION
This study of patients undergoing cardiac catheterization at one public (VA) and one private (university) hospital located in the northeastern United States revealed that cardiologists at the VA site were less likely to recommend revascularization (PTCA or CABG) to African American patients than to White patients. This difference was not accounted for by differences between the 2 groups in number of stenotic vessels (disease status) or patient age, educational level (a marker of SES), previous revascularization, or self-rated health status. However, reasons offered for not recommending PTCA or CABG were generally similar in type and frequency in the case of both African American and White patients. As mentioned, we found no differences in revascularization recommendations according to patient race at the private (university) hospital.
Numerous studies have examined racial/ethnic differences in rates of cardiac care use, including revascularization.2,10,12,17–23 Most of these studies have involved the use of large administrative databases to examine differences. Relatively fewer studies have collected primary data to assess not only differences in rates of utilization but also reasons behind these differences. Our study is an example of the second type of study. Other studies that have examined provider factors involved in these rate disparities and found racial/ethnic differences include the aforementioned study of Hannan et al.16; our VA sample findings agree with their results.
Hannan et al. found that physicians were less likely to recommend cardiac revascularization to African American patients than to White patients who were at similar levels of need for revascularization according to the Rand criteria.16 However, these authors examined only recommendations for CABG, not recommendations for CABG and/or PTCA. This aspect of the Hannan et al. study represents a limitation in that, although their indications vary somewhat, these 2 procedures target the same condition. Furthermore, racial/ethnic differences in the use of CABG and PTCA vary.24 In addition, the Hannan et al. sample was composed mostly of patients with private health insurance coverage of unclear comprehensiveness; as a result, issues involved with inadequate access to care may have confounded their results. We included both privately insured patients and VA patients who already had full access to the health care system.
Looking at another dimension of this problem (i.e., cardiovascular care), Schulman et al. used simulated patients to examine provider behavior in terms of recommendations for angiography among patients with chest pain.25 These authors also found that physicians were less likely to recommend cardiac catheterization to African American female patients than to White female patients in a similar clinical scenario.25 Cardiac catheterization is a step up from cardiac revascularization in the process of cardiac care.
Some of the findings of our study were expected. For example, VA patients have greater frequencies of comorbid illnesses than patients who receive care at most private hospitals because the VA serves as a safety net for socioeconomically disadvantaged veterans.26 However, what is interesting in our findings is that racial/ethnic differences in physician recommendations for revascularization exist within a VA system.
We can offer several hypotheses for the observed racial variation in recommendations for revascularization among the VA patients. First, VA patients are, on average, of low SES, and among the members of this group it has been shown that African American patients are of even lower SES than White patients.27 Therefore, if doctor–patient communications can be influenced by discordance in socioeconomic class, then it is conceivable that our results reflect racial/ethnic differences in communication regarding treatment options. In other words, physicians in the VA system may be more likely to recommend revascularization for White patients than for African American patients in part because they may be able to relate easier to White patients, to whom they are closer on the socioeconomic ladder.
Second, it is possible that African American VA patients were generally sicker (e.g., higher frequencies of comorbidities) than White VA patients such that they were less appropriate candidates for cardiac revascularization. Although we did not extensively examine noncardiac disease burden in our sample, it is unlikely that comorbidity burden was a major factor. This supposition is supported by the fact that cardiologists did not mention comorbidity burden as a reason for not recommending revascularization.
Third, it is possible that VA African American patients were more likely than White patients to communicate a low degree of interest in aggressive treatment (i.e., revascularization) to their physicians, which could have produced the differences observed in physician recommendations. We did not assess this possibility. However, others have shown African American patients to be more risk averse than White patients in regard to invasive surgery.28
Several limitations are important to consider when interpreting our results. First, we examined predominantly male patients from 2 hospitals located in the same city. Therefore, our findings may not be generalizable. Second, we lacked detailed patient information on comorbidities and other nonmedical factors such as smoking status or willingness to adopt a healthier lifestyle, factors that could have affected physician recommendations. If these factors were more prevalent among VA African American patients than university African American patients, this could explain in part the observed differences in physician recommendations for revascularization in the VA sample.
Third, we did not adequately evaluate elements associated with the appropriateness of revascularization. It is possible that VA cardiologists performed fewer procedures for which the indications for revascularization were equivocal; thus, if White VA patients more often exhibited clear indications for surgery than African American patients, this difference could explain our findings. We did attempt to account for this possibility by including adjustments for the number of significant stenoses in our multivariate model.
Fourth, we had no data on physician characteristics such as age, number of years in practice, or racial/ethnic background. More information on physician characteristics would have allowed us to examine the relationship between such characteristics and recommendations for revascularization. It is also conceivable that some cardiologists completed the survey but changed their recommendation after attending the cardiac catheterization conference (physician meeting to discuss findings and possible interventions). However, it is unlikely that such changes in recommendations varied by patient race. Finally, the small number of sites precludes meaningful comparisons between VA and private (university) hospitals.
This study is important in that it adds to a growing and needed literature examining reasons for the marked and well-documented racial/ethnic disparities in use of cardiac care and consequent outcomes. We specifically addressed provider factors that have received relatively less research attention than patient cultural and psychosocial factors. The fact that one can observe racial/ethnic variations in medical treatment decisionmaking even in a system of equal access such as the VA fuels the notion that there is perhaps disparity in areas beyond access to care. Access to care is correctly believed to be an important solution to the nation’s disparities in health care. However, our results concur with a recent Institute of Medicine report indicating that equal access may not fully equalize care for all patients.29
In summary, we found that physicians (cardiologists) in a public (VA) hospital were less likely to recommend revascularization for African American patients than for White patients. This difference was not explained by important patient factors. Recommendations for revascularization did not differ by patient race in the private (university) study hospital. Further in-depth studies are needed to examine how physicians make decisions on cardiac care for patients of varying cultural/ethnic backgrounds.
Acknowledgments
This study was funded by grants from the American Heart Association and the VA Health Services Research and Development Office.
We would like to thank Kimberly Hansen and Kelly Hyman of the Center for Health Equity Research and Promotion, Pittsburgh VA Healthcare System, for their editorial assistance.
Human Participant Protection This research was approved by the institutional review boards of both study sites, and all of the patients included consented to study participation.
Contributors S. A. Ibrahim conducted the data analysis and drafted the article. B. Bean-Mayberry assisted in drafting and editing the article and in interpreting data. M. E. Kelley assisted with data analysis and interpretation. C. Good and J. Whittle assisted in conceiving the study and in drafting the article. J. Conigliaro assisted in conceiving the study, contributed to data interpretation, and assisted in drafting the article.
Peer Reviewed
References
- 1.Morbidity and Mortality: 2002 Chart Book on Cardiovascular, Lung, and Blood Diseases. Bethesda, Md: National Heart, Lung, and Blood Institute; 2002.
- 2.Gillum RF. Cardiovascular disease in the United States: an epidemiologic overview. In: Saunders E, ed. Cardiovascular Disease in Blacks. Philadelphia, Pa: FA Davis Co; 1991:1–15. [PubMed]
- 3.Health, United States, 1993. Hyattsville, Md: National Center for Health Statistics; 1994.
- 4.American Heart Association. Cardiovascular disease and stroke in African Americans and other racial minorities in the United States: a statement for public health professionals. Circulation. 1991;83:1462–1480. [DOI] [PubMed] [Google Scholar]
- 5.Gillum RF, Gillum BS, Francis CK. Coronary revascularization and cardiac catheterization in the United States: trends in racial differences. J Am Coll Cardiol. 1997;29:1557–1562. [DOI] [PubMed] [Google Scholar]
- 6.Peterson ED, Jollis JG, Bebchuk JD, et al. Changes in mortality after myocardial revascularization in the elderly: the national Medicare experience. Ann Intern Med. 1994;121:919–927. [DOI] [PubMed] [Google Scholar]
- 7.Ayanian JZ, Udvarhelyi IS, Gastonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angioplasty. JAMA. 1993;269:2642–2646. [PubMed] [Google Scholar]
- 8.Hannan E, Kilburn HJ, O’Donnell JF, Lukacik G, Shields EP. Interracial access to selected cardiac procedures for patients hospitalized with coronary artery disease in New York State. Med Care. 1991;29:430–441. [DOI] [PubMed] [Google Scholar]
- 9.Wenneker M, Epstein A. Racial inequalities in the use of procedures for patients with ischemic heart disease in Massachusetts. JAMA. 1989;261:253–257. [PubMed] [Google Scholar]
- 10.Whittle J, Conigliaro J, Good CB, Lofgren RP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs Medical System. N Engl J Med. 1993;329:621–627. [DOI] [PubMed] [Google Scholar]
- 11.McBean AM, Warren JL, Babish JD. Continuing differences in the rates of percutaneous transluminal coronary angioplasty and coronary artery bypass graft surgery between elderly black and white Medicare beneficiaries. Am Heart J. 1994;127:287–295. [DOI] [PubMed] [Google Scholar]
- 12.Ford E, Cooper R, Castaner A, Simmons B, Mar M. Coronary arteriography and coronary bypass survey among whites and other racial groups relative to hospital-based incidence rates for coronary artery disease: findings from NHDS. Am J Public Health. 1989;79:437–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gillum RF. Coronary heart disease in black populations: I. Mortality and morbidity. Am Heart J. 1982;104:839–851. [DOI] [PubMed] [Google Scholar]
- 14.Gillum RF, Liu KC. Coronary heart disease mortality in United States blacks, 1940–1978: trends and unanswered questions. Am Heart J. 1984;108:728–732. [DOI] [PubMed] [Google Scholar]
- 15.Healthy People 2010: Understanding and Improving Health. Washington, DC: US Dept of Health and Human Services; 2000.
- 16.Hannan E, van Ryn M, Burke JE, et al. Access to coronary artery bypass surgery by race/ethnicity and gender among patients who are appropriate for surgery. Med Care. 1999;37:68–77. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg KC, Hatz AJ, Jacobsen SJ, Krakauer H, Rimm AA. Racial and community factors influencing coronary artery bypass graft surgery for all 1986 Medicare patients. JAMA. 1992;267:1473–1477. [PubMed] [Google Scholar]
- 18.Johnson PA, Lee TH, Cook EF, Rouan GW, Goldman L. Effect of race on the presentation and management of patients with acute chest pain. Ann Intern Med. 1993;118:593–601. [DOI] [PubMed] [Google Scholar]
- 19.Maynard C, Fisher LD, Passamani ER. Survival of black persons compared with white persons in the Coronary Artery Surgery Study (CASS). Am J Cardiol. 1987;60:513–518. [DOI] [PubMed] [Google Scholar]
- 20.Maynard C, Fisher LD, Passamani ER, Pullum T. Blacks in the Coronary Artery Surgery Study (CASS): race and clinical decision making. Am J Public Health. 1986;76:1446–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mirvis DM, Burns R, Gaschen L, Cloar FT, Graney M. Variation in utilization of cardiac procedures in the Department of Veterans Affairs Health Care System: effect of race. J Am Coll Cardiol. 1994;24:1297–1304. [DOI] [PubMed] [Google Scholar]
- 22.Oberman A, Cutter G. Issues in the natural history and treatment of coronary heart disease in a black population: surgical treatment. Am Heart J. 1984;108:688–694. [DOI] [PubMed] [Google Scholar]
- 23.Peterson ED, Wright SM, Daley J, Thibault GE. Racial variation in cardiac procedure use and survival following acute myocardial infarction in the Department of Veterans Affairs. JAMA. 1994;271:1175–1180. [PubMed] [Google Scholar]
- 24.Schneider EC, Leape LL, Weissman JS, Piana RN, Gatsonis C, Epstein AM. Racial differences in cardiac revascularization rates: Does “overuse” explain higher rates among white patients? Ann Intern Med. 2001;135:328–337. [DOI] [PubMed] [Google Scholar]
- 25.Schulman KA, Berlin J, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–626. [DOI] [PubMed] [Google Scholar]
- 26.Kazis LE, Miller DE, Clark J, et al. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1997;158:626–632. [DOI] [PubMed] [Google Scholar]
- 27.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Differences in expectation of outcome mediate African-American/white differences in “willingness” to consider joint replacement. Arthritis Rheum. 2002;46:2429–2435. [DOI] [PubMed] [Google Scholar]
- 28.Oddone EZ, Horner RD, Diers T, et al. Understanding racial variation in the use of carotid endarterectomy: the role of aversion to surgery. J Natl Med Assoc. 1998;90:25–33. [PMC free article] [PubMed] [Google Scholar]
- 29.Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002.