Abstract
Objectives. This study examined antimicrobial prescribing patterns for adults and children with bronchitis or upper respiratory infections (URIs) before and after release of nationally disseminated pediatric practice recommendations.
Methods. Data from the 1993, 1995, 1997, and 1999 National Ambulatory Medical Care Survey were used to evaluate prescriptions for antimicrobials for URIs and bronchitis.
Results. From 1993 to 1999, the proportion of children receiving antimicrobials after visits for URIs and bronchitis decreased. However, the use of broad-spectrum antimicrobials rose from 10.6% of bronchitis visits to 40.5%. Prescriptions of antimicrobials for adults with URIs or bronchitis showed a decrease between 1993 and 1999.
Conclusions. Although antimicrobial prescribing for URIs and bronchitis has decreased for both children and adults, the prescribing of broad-spectrum antibiotics among children has shown a proportional rise.
Since the mid-1990s, a number of studies have documented the widespread use of antimicrobials in outpatient settings for viral upper respiratory infections (URIs).1–6 These studies, using administrative data from Medicaid populations (1993–1994), data from the 1992 National Ambulatory Medical Care Survey (NAMCS; a national survey of visits to office-based physicians), and chart reviews of primary care physicians, found rates of prescribing of antimicrobials for the common cold and uncomplicated URIs of 40% to 60%.1–3,5–7 Other studies examining the use of antibiotics for acute bronchitis, another predominantly viral respiratory illness, show even higher antimicrobial prescribing rates. Moreover, evidence from the NAMCS showed an increasing trend toward the use of broad-spectrum antimicrobials and decreasing rates of narrower-spectrum drugs over the decade from 1980 to 1992.1 A recent study using data from the NAMCS showed that the rate of antimicrobial prescribing overall and for respiratory infections for children and adolescents younger than 15 years decreased between 1989–1990 and 1999–2000.8
This information on the widespread use and potential overuse of antimicrobials for primarily viral URIs carries particular significance, because not only is there little evidence to support their effectiveness as treatments, but the inappropriate use of antimicrobial agents creates an environment for the development of resistance, placing both populations and individual patients at risk. Reducing the use of antimicrobial agents can decrease the spread of resistance. Therefore, judicious use of antimicrobials, especially for respiratory illnesses, has been advocated as a key strategy for reducing rising drug resistance.9–12
In an effort to change antibiotic prescribing practices, a variety of guidelines have been developed and implemented.13 Although the Centers for Disease Control and Prevention (CDC) began its campaign against overuse of antibiotics in 1995, the first of the nationally disseminated recommendations on judicious use of antimicrobials was produced by the CDC and the American Academy of Pediatrics and disseminated in 1998.14 These recommendations were distributed to all members of the American Academy of Pediatrics and were also disseminated through articles sent to all members of the American Academy of Family Physicians.15,16 In response to this set of recommendations, several strategies focusing on limited groups of providers were implemented with the use of some form of “academic detailing,” a process whereby physicians or other health professionals discuss with practicing physicians appropriate indications and use of medications in an effort to change prescribing practices, and presentations to small groups of providers.17,18 These interventions had varied degrees of success in changing prescribing practices.
Although most of the effort to date has been expended in curtailing the use of antibiotics for pediatric respiratory diseases, most studies have shown that antibiotics are prescribed more often for adults with colds than for children.2 Other observations show that physicians who treat both adults and children are more likely to prescribe antibiotics for children than are physicians who treat only children.19 These results suggest that antibiotic overuse is not simply a pediatric problem but may be even more widespread among adults. Guidelines for reducing antibiotic use in adults were published by the American College of Physicians in 2001,20 3 years after recommendations were disseminated for children. Although the creation and dissemination of clinical practice guidelines is a popular method for educating physicians in an effort to change practices, it has not been particularly successful.21 It is not clear what effect the delay in issuing guidelines for antibiotic use in adults has had on the use of antimicrobials in this age group.
The purpose of this study was to examine the impact of the principles of judicious use of antimicrobial agents for pediatric URIs on antimicrobial prescribing for children and adults with colds, uncomplicated URIs, and bronchitis.
METHODS
The data used in this study come from the 1993, 1995, 1997, and 1999 NAMCS. The NAMCS is conducted annually by the National Center for Health Statistics and surveys a sample of non–federally employed physicians selected from the master files of the American Medical Association and the American Osteopathic Association. The NAMCS uses a multistage probability sample to collect information from physicians in selected primary sampling units. Selected physicians complete a survey form for office visits during a randomly selected 1-week period.
Subjects
For analyses focusing on children, we limited the sample to patients younger than 18 years; we defined adults as patients aged 18 years and older.
Episodes of Care
To examine the use of antibiotics for primarily viral URIs, we examined all office visits with the primary diagnoses of acute nasopharyngitis (common cold) (using International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] code 460), acute URIs of multiple or unspecified sites (ICD-9-CM code 465), acute bronchitis (ICD-9-CM code 466), and bronchitis not otherwise specified (NOS) (ICD-9-CM code 490). In our assessment of overuse of antibiotics, we are aware that even though the primary diagnosis may not warrant antibiotic use, a secondary or tertiary diagnosis may suggest the effectiveness of antibiotic use. Previous studies have suggested that other respiratory infections are the most likely secondary and tertiary diagnoses suggesting antibiotic use.2,4 Because in some cases other conditions may be present that might warrant antibiotic use, we excluded from consideration visits with secondary or tertiary diagnoses of nonsuppurative otitis media (ICD-9-CM code 381–381.4), suppurative otitis media (ICD-9-CM code 382.xx), acute sinusitis (ICD-9-CM code 461.xx), chronic sinusitis (ICD-9-CM code 473.xx), acute pharyngitis (ICD-9-CM code 462), acute tonsillitis (ICD-9-CM code 463), streptococcal sore throat (ICD-9-CM code 034.0), and pneumonia (ICD-9-CM codes 481.xx–486.xx). We also excluded “bacterial infections” (ICD-9-CM code 041.xx) and urinary tract infections (ICD-9-CM codes 590.xx, 595.xx, 597.xx, and 599.0). An ICD-9-CM code with a designation of x indicates all codes (0–9) for that digit. Additionally, because the NAMCS does not allow a differentiation of dosage length for treatment, we excluded visits with the secondary or tertiary diagnoses of acne (ICD-9-CM code 706.1). Among adults we excluded these diagnoses as well as emphysema (ICD-9-CM code 492.xx) and chronic bronchitis (ICD-9-CM code 491.xx) because of evidence of effectiveness of antibiotics in acute exacerbations.22
We identified antibiotic prescription for each visit using both trade- and generic-named antimicrobial agents assigned by NAMCS to each medication prescribed. Because the diagnosis cannot be directly linked to the medication and to minimize the likelihood that an antibiotic prescription was unrelated to the principal diagnosis, we counted only those prescriptions entered as the primary medication related to the office visit on the patient record form. We classified penicillin, amoxicillin, ampicillin, erythromycin, tetracycline, doxycycline, trimethoprim, sulfamethoxazole, and trimethoprimsulfamethoxazole as narrow-spectrum agents and cephalosporins, other macrolides, fluoroquinolones, and amoxillicin–clavulanic acid as broad-spectrum agents. This classification strategy is consistent with those used in previous investigations.23
Data Analysis
We weighted the data and conducted the analysis using SUDAAN (Research Triangle Institute, Research Triangle Park, NC) in an effort to account for the complex survey design in the parameter and standard error estimates. Primary sampling unit weights for the 1993 and 1995 NAMCS are not currently available in the public use files and were provided to the investigators by the National Center for Health Statistics Research Data Center. This analysis plan allowed us to make national estimates of prescribing in all 4 years.
Although national population estimates could still be made, the NAMCS design showed a decline in the total number of physician visits collected in the 4 years: 35 978 in 1993, 36 875 in 1995, 24 715 in 1997, and 20 760 in 1999. The unweighted visits for respiratory infections for the 4 years were 1024 (349 adult visits, 675 child visits) in 1993, 1222 (690 adult visits, 532 child visits) in 1995, 703 (354 adult visits, 349 child visits) in 1997, and 495 (297 adult visits, 198 child visits) in 1999.
For conceptual simplicity and to provide sufficient numbers of episodes for analysis, we combined the diagnoses of common cold and URI together and acute bronchitis and bronchitis NOS together for the analysis. Among children, we computed the proportion of physician visits yielding prescriptions for antibiotics for 1993, 1995, 1997, and 1999 to allow an assessment of the change in prescribing from the studies using the 1992 NAMCS and to determine the potential impact of the 1998 CDC/American Academy of Pediatrics’ recommendations for judicious use of antimicrobials. We also examined the use of narrow- and broad-spectrum agents in those years. Because each year was a separate population estimate, we analyzed the population-based prescribing estimates from each year, controlling for the design effect in the NAMCS using Epistat (Centers For Disease Control and Prevention, Atlanta, Ga) with a χ2 for trend. In an effort to determine whether the recommendations for treating children had effects that were generalizable to the care of adults, we also examined prescribing for adults for the same diagnoses during the 4 years.
RESULTS
Table 1 ▶ illustrates some characteristics of the physician visits for the investigated respiratory tract infections in the 4 years under study. Primary care physicians accounted for the vast majority of these visits.
TABLE 1—
Characteristics of Physician Visits for Respiratory Infections, by Percentage: United States, 1993–1999
| 1993 | 1995 | 1997 | 1999 | |
| Patient age, y | ||||
| ≤ 5 | 27.10 | 30.20 | 29.51 | 25.73 |
| 6–13 | 10.19 | 13.57 | 11.14 | 11.00 |
| 14–17 | 4.24 | 5.07 | 5.48 | 4.85 |
| 18–24 | 5.36 | 4.85 | 4.35 | 5.33 |
| 25–34 | 10.65 | 9.58 | 7.93 | 7.89 |
| 35–49 | 18.93 | 15.40 | 17.51 | 18.84 |
| 50–64 | 11.16 | 9.20 | 11.00 | 12.82 |
| ≥ 65 | 12.37 | 12.13 | 13.09 | 13.53 |
| Patient gender | ||||
| Male | 54.32 | 55.87 | 53.86 | 55.99 |
| Female | 45.68 | 44.13 | 46.14 | 44.01 |
| Patient race/ethnicity | ||||
| White | 88.53 | 86.19 | 85.68 | 83.39 |
| Black | 7.05 | 8.95 | 10.19 | 12.65 |
| Asian/Pacific Islander | . . .a | . . .a | 4.02 | 3.79 |
| American Indian | . . .a | . . .a | 0.11 | 0.17 |
| Visit based on MD referral | ||||
| Yes | 4.99 | 1.62 | 1.66 | 1.90 |
| No | 95.01 | 98.38 | 98.34 | 98.10 |
| Specialty of treating physician | ||||
| Pediatrics | 27.42 | 28.70 | 34.14 | 26.56 |
| General/family practice | 42.03 | 45.38 | 30.73 | 41.65 |
| Internal medicine | 17.42 | 17.64 | 15.79 | 16.70 |
aOwing to small sample sizes, the values were suppressed by the National Center for Health Statistics Research Data Center in an effort to protect confidentiality and because the estimates were not reliable.
Antibiotic Prescribing in Children
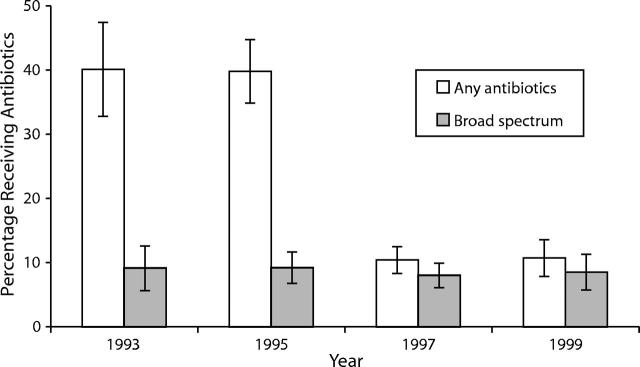
Figure 1 ▶ shows that the prescribing of antibiotics for URIs/common colds in children had a decreasing trend over the 4 time periods. A substantial decrease was noted between 1995 and 1997 with a stabilization in prescribing rates to approximately 10% in 1997 and 1999. The proportion of physician visits for URIs/common colds in children receiving broad-spectrum antibiotics showed a reasonably stable but slight downward trend. However, as the general proportion of physician visits yielding prescriptions for antibiotics decreased, the proportion accounted for by broad-spectrum antibiotics increased.
FIGURE 1—
Visits by children who had upper respiratory infection/common cold and received any antibiotics or broad spectrum antibiotics.
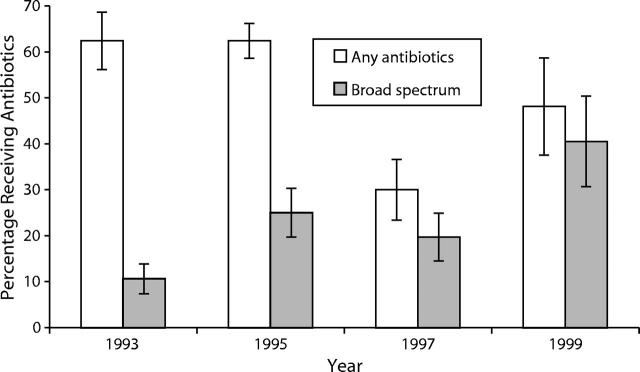
Figure 2 ▶ indicates that the prescribing of antibiotics for acute bronchitis/bronchitis NOS in children dropped between 1995 and 1997 but increased in 1999, although not to the 1993 and 1995 levels. For this set of conditions, the use of broad-spectrum antibiotics showed the most dramatic increase.
FIGURE 2—
Visits by children with acute bronchitis/bronchitis not otherwise specified who received any antibiotics or broad spectrum antibiotics.
Antibiotic Prescribing in Adults
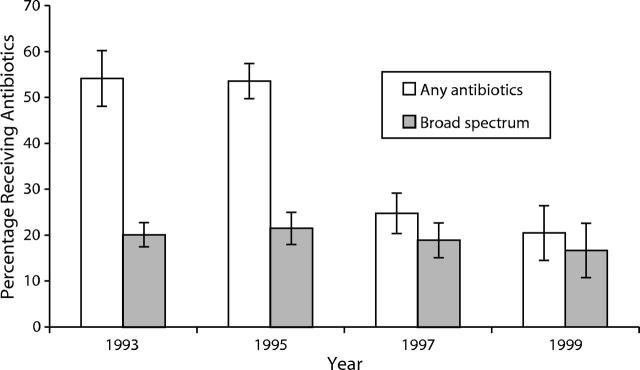
Even though the principles released in 1998 on judicious prescribing were focused on children, we also examined whether there were any changes in the prescribing of antibiotics for adult respiratory tract infections during the same time period. Like the prescribing for children, prescribing of antibiotics for URIs/common colds in adults showed a substantial decrease between 1995 and 1997 (Figure 3 ▶). Among adults, antibiotic prescribing for URIs/common colds continued to decrease both in general and for broad-spectrum antibiotics.
FIGURE 3—
Visits by adults with upper respiratory infection/common cold who received any antibiotics or broad spectrum antibiotics.
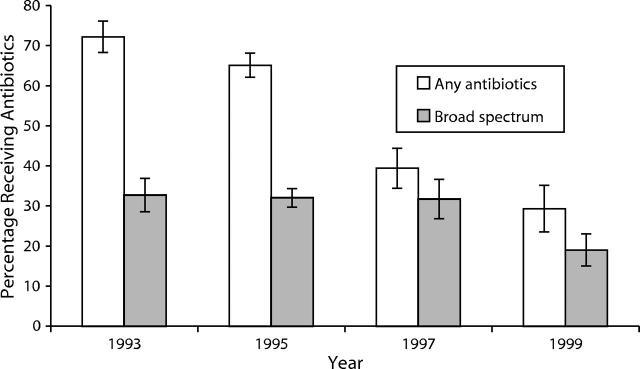
Figure 4 ▶ demonstrates that antibiotic prescribing for acute bronchitis/bronchitis NOS in adults continued to decrease throughout the 4 investigated time periods, from 72.2% in 1993 to 29.3% in 1999. Prescribing of broad-spectrum antibiotics was relatively stable from 1993 to 1997, with a substantial drop in 1999.
FIGURE 4—
Visits by adults with acute bronchitis/bronchitis not otherwise specified who received any antibiotics or broad spectrum antibiotics.
DISCUSSION
Our analysis of 8 years of prescribing data for ambulatory care visits to US physicians reveals that antibiotic use for primarily viral respiratory tract infections is decreasing. Antibiotic prescriptions for diagnoses of URIs, common colds, acute bronchitis, and bronchitis NOS in both children and adults dropped by 15%–40% during this time period. Antibiotic use for primarily viral respiratory tract infections decreased, with the primary point of decrease occurring between 1995 and 1997. This is a positive finding in the efforts to reduce inappropriate antibiotic use and correspondingly reduce antibiotic resistance.
The period showing the most substantial decrease in antibiotic use occurred between 1995 and 1997, well before most public efforts to reduce antibiotic prescribing had been mobilized. Efforts to educate health care providers and implementing initiatives urging conservative use of antibiotics for children did not reach their highest intensity until 1998, with recommendations made by the CDC, American Academy of Pediatrics, and American Academy of Family Physicians. Moreover, the primary dissemination of guidelines for treatment of adults was not released until 2001.20,24 Our data indicate that substantial declines in both pediatric and adult prescribing for viral respiratory conditions had occurred well before these efforts. The timing of this change suggests that information released in 1995 and 1996 may have had a more significant impact on the initial decrease in antibiotic prescribing than the release of the guidelines and educational programs by the CDC and other professional organizations. However, these programs may have reinforced the initial message and contributed substantially to the low prescribing rates in 1999 for several of the conditions.
Several studies identifying the overuse of antibiotics for primarily viral respiratory infections were disseminated in the medical literature,1–3 and these generated articles in medical news reports (e.g., Medical Tribune, American Medical News).25,26 The decrease in prescriptions that occurred between 1995 and 1997 is possibly the result of dissemination of information via these and other health services research studies. The results from the 1997 and 1999 NAMCS show antibiotic use for children with URIs or common colds to be approximately 10%. Due to the normal variability in patient presentation and prescribing practice differences among physicians, it is unlikely that this measure will ever reach zero. The ultimate nadir of antibiotic prescribing rates that the medical community can expect is unknown; however, the issue does have implications for public health officials. Initiatives toward education will eventually experience a “floor effect,” making further interventions to alter prescribing practices too cost- or time-intensive to be worthwhile. It is unclear whether we have reached this point.
The difference in antibiotic prescribing rates for adults compared with children, although confounded by inherent differences in diagnostic patterns between the groups, illustrates that there is substantial room for improvement in this regard for practitioners treating adults. Although the available data show a decrease leading up to 1999, the latest estimates of antibiotic prescribing for URIs in adults are still greater than 20%.
Because the CDC and others have suggested using broad-spectrum antibiotics sparingly because of implications for drug resistance, the rate at which broad-spectrum antibiotics are used is worthy of note. For children with diagnoses of URIs and adults with diagnoses of URIs/common colds or acute bronchitis/bronchitis NOS, we found a significant trend toward decreasing use of broad-spectrum antibiotics. However, the data also suggest that for children with diagnoses of acute bronchitis or bronchitis NOS, there was a substantial increase between 1993 and 1999 in the use of broad-spectrum antibiotics. This difference may reflect a tendency of practitioners to perceive children with bronchitic symptoms as more seriously ill than children with URIs/common colds or adults with either diagnosis. This finding may also indicate a need for practitioners treating children to receive further education regarding the appropriate treatment for viral lower respiratory tract infections.
Several limitations of this study exist. First, because of NAMCS’s sampling design and weights, the data presented here theoretically offer accurate estimates of physicians’ behavior. However, because the information available for analysis does not include more recent years, the timeliness of this report may limit its generalizability. The analysis shows that prescribing practices can change markedly over a few years’ time, implying that the current estimates are a guide but that practice patterns in 2003 may be somewhat different.
Second, although the current analysis used existing data and the participating physicians were unaware at the time of data collection of the present study’s aims, NAMCS data are based on physicians’ self-reports and may be affected by participants’ preferences to be seen as practicing in a socially desirable fashion. The actual practice of participants in the NAMCS could be different from what they indicated on their data collection instruments or could differ when they were not participating as subjects in the NAMCS. Moreover, although this study followed the general reporting style of the NAMCS by combining family and general practice, the proportion of family physicians in that group has increased over time.27 Thus, the change in respondent demographics may have affected prescribing practices.
Third, even though we attempted to use a rigorous method for linking the medication prescribed during a visit to the primary diagnosis, it is possible that the antibiotics were actually prescribed for a different condition than was addressed in the visit. However, to account for such a large change in antibiotic prescribing over the short time period observed in this study, the frequency of antibiotic prescribing for unrelated conditions would have had to fall substantially between the 1995 and 1997 NAMCS, which is highly unlikely.
Fourth, the NAMCS provides the ability to investigate the prescribing practices of office-based physicians. and provides visit-based rates of prescribing. However, it does not allow an assessment of the possible impact of changes in decisions to seek care by patients.
Fifth, it is possible that over time, because of the overlap in symptom constellation between URIs and other conditions, once physicians are told that antibiotics should not be given for URIs they will simply change the diagnosis to justify antibiotic use. The speculation would be that overall prescribing is still the same but that the incidence of certain diagnoses has changed. Other data from the NAMCS show that the rate of antimicrobial prescribing overall as well as for a wide range of respiratory tract infections has decreased among children younger than 15 years.8,28 Other data suggest that even when physicians are informed of the need to decrease the prescribing of antibiotics for URIs among children, they do not increase other diagnoses to justify antibiotic use.29
Because of emerging antibiotic resistance, a concerted effort to encourage judicious antibiotic prescribing, particularly for primarily viral respiratory tract infections, has been evident in the medical literature and the US education system for several years. The impact of these programs has extended throughout the medical community and has affected prescribing practices for these conditions. A substantial decrease in prescribing antibiotics has occurred, although the cause of this decrease is unclear. Moreover, the impact of the historic intervention that occurred between 1995 and 1997 is unclear, because the rate of prescribing antibiotics had already decreased. This change’s implications for slowing development of antibiotic resistance, although not completely understood, are encouraging.
Acknowledgments
This study was funded in part through grant 1D12HP00023–01 from the Health Resources and Services Administration.
Human Participant Protection This study used public use data; therefore, no protocol approval was needed.
Contributors A. G. Mainous, W. J. Hueston, and M. P. Davis contributed to the study design, data interpretation, and article preparation. W. S. Pearson performed the data analysis.
Peer Reviewed
References
- 1.McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA. 1995;273:214–219. [PubMed] [Google Scholar]
- 2.Mainous AG III, Hueston WJ, Clark JR. Antibiotics and upper respiratory infection: do some folks think there is a cure for the common cold? J Fam Pract. 1996;42:357–361 [PubMed] [Google Scholar]
- 3.Mainous AG III, Zoorob RJ, Hueston WJ. Current management of acute bronchitis in ambulatory care: the use of antibiotics and bronchodilators. Arch Fam Med. 1996;5:79–83. [DOI] [PubMed] [Google Scholar]
- 4.Mainous AG III, Hueston WJ. The cost of antibiotics in treating upper respiratory infections in a Medicaid population. Arch Fam Med. 1998;7:45–49. [DOI] [PubMed] [Google Scholar]
- 5.Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278:901–904. [PubMed] [Google Scholar]
- 6.Nyquist A-C, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA. 1998;279:875–877. [DOI] [PubMed] [Google Scholar]
- 7.Hueston WJ, Mainous AG III, Brauer N, Mercuri J. Evaluation and treatment of respiratory infections: does managed care make a difference? J Fam Pract. 1997;44:572–577. [PubMed] [Google Scholar]
- 8.McCaig LF, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents. JAMA. 2002;287:3096–3102. [DOI] [PubMed] [Google Scholar]
- 9.Chen DK, McGeer A, De Azavedo JC, Low DE. The Canadian Bacterial Surveillance Network. Decreased susceptibility of Streptococcus pneumoniae to fluoroquinolones in Canada. N Engl J Med. 1999;341:233–239. [DOI] [PubMed] [Google Scholar]
- 10.Seppälä H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. N Engl J Med. 1997;337:441–446. [DOI] [PubMed] [Google Scholar]
- 11.Rahal JJ, Urban C, Horn D, et al. Class restriction of cephalosporin use to control total cephalosporin resistance in nosocomial Klebsiella. JAMA. 1998;280:1233–1237. [DOI] [PubMed] [Google Scholar]
- 12.Austin DJ, Kristinsson KG, Anderson RM. The relationship between the volume of antimicrobial consumption in human communities and the frequency of resistance. Proc Natl Acad Sci USA. 1999;96:1152–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gross PA, Pujat D. Implementing practice guidelines for appropriate antimicrobial usage: a systematic review. Med Care. 2001;39(suppl 2):1155–1169. [DOI] [PubMed] [Google Scholar]
- 14.Dowell SF, ed. Principles of judicious use of antimicrobial agents for pediatric upper respiratory tract infections. Pediatrics. 1998;101(suppl 1):163–184. [Google Scholar]
- 15.Dowell SF, Schwartz B, Phillips WR, et al. Appropriate use of antibiotics for URIs in children, I: otitis media and acute sinusitis. Am Fam Physician. 1998;58:1113–1118. [PubMed] [Google Scholar]
- 16.Dowell SF, Schwartz B, Phillips WR, et al. Appropriate use of antibiotics for URIs in children, II: cough, pharyngitis, and the common cold. Am Fam Physician. 1998;58:1335–1342. [PubMed] [Google Scholar]
- 17.Finkelstein JA, Davis RL, Dowell SF, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics. 2001;108:1–7. [DOI] [PubMed] [Google Scholar]
- 18.Belongia EA, Sullivan BJ, Chyou PH, Madagame E, Reed KD, Schwartz B. A community intervention trial to promote judicious antibiotic use and reduce penicillin-resistant Streptococcus pneumoniae carriage in children. Pediatrics. 2001;108:575–583. [DOI] [PubMed] [Google Scholar]
- 19.Mainous AG III, Hueston WJ, Love MM. Antibiotics for colds in children: who are the high prescribers? Arch Pediatr Adolesc Med. 1998;152:349–352. [PubMed] [Google Scholar]
- 20.Snow V, Mottur-Pilson C, Gonzales R. Principles of appropriate antibiotic use for treatment of acute bronchitis in adults. Ann Intern Med. 2001;134:518–520. [DOI] [PubMed] [Google Scholar]
- 21.Greco PJ, Eisenberg JM. Changing physicians’ practices. N Engl J Med. 1993;329:1271–1274. [DOI] [PubMed] [Google Scholar]
- 22.Saint S, Bent S, Vittinghoff E, Grady D. Antibiotics in chronic obstructive pulmonary disease exacerbations. A meta-analysis. JAMA. 1995;273:957–960. [PubMed] [Google Scholar]
- 23.Steinman MA, Landefeld CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in primary care. JAMA. 2003;289:719–725. [DOI] [PubMed] [Google Scholar]
- 24.Gonzales R, Bartlett JG, Besser RE, Hickner JM, Hoffman JR, Sande MA. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults: background. Ann Emergency Med. 2001;37:698–702. [PubMed] [Google Scholar]
- 25.Antibiotics overused for bronchitis. American Medical News. 26February1996:16.
- 26.Carroll L. Too many doctors order antibiotics for colds. Medical Tribune. 23May1996:1, 4. [Google Scholar]
- 27.Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2000 summaryAdv Data. 2000;No. 328:1–32. [PubMed]
- 28.Halasa NB, Griffin MR, Zhu Y, Edwards KM. Decreased number of antibiotic prescriptions in office-based settings from 1993 to 1999 in children less than five years of age. Pediatr Infect Dis J. 2002;21:1023–1028. [DOI] [PubMed] [Google Scholar]
- 29.Mainous AG III, Hueston WJ, Love MM, Evans ME, Finger R. Statewide intervention to decrease antibiotics for pediatric respiratory infections. Fam Med. 2000;32:22–29. [PubMed] [Google Scholar]