Abstract
Objectives. We sought to separate age and cohort associations with depression, assessed 3 times within a 10-year period in 701 women born between 1928 and 1958.
Methods. We used regression analysis to examine age differences in women with depression in 2 birth cohorts, pre-1945 and post-1944, who were assessed at comparable ages. Multilevel modeling was used to estimate changes with age in successive birth year cohorts.
Results. An age by cohort interaction indicated more depression among younger than older women in the post-1944 cohort but a flat age profile in the pre-1945 cohort. Longitudinal analyses indicated declines in depression with age in more recent cohorts but increases in earlier ones.
Conclusions. Increases in depression in younger women in successive cohorts may be offset by decreases in middle age.
Reported rates of depressive disorders in women have risen steadily over the latter half of the 20th century, yet there is still no consensus as to what accounts for this trend.1 Some researchers have proposed that escalation of rates is a consequence of the dramatic historic shifts in work and family role expectations that took place at that time in the United States.2–5 Women entered the workforce in unprecedented numbers during World War II6 but soon were compelled to assume more traditional prewar roles to make way for returning servicemen in the civilian labor force. Over the next 2 decades, sanctioned roles for women outside the confines of domesticity remained narrowly defined.7 However, since the advent of the women’s movement in the mid-1960s, social restrictions have weakened and increasing endorsement of nontraditional gender roles have prevailed, radically changing the shape and content of women’s lives.8 Workforce participation by women and by married women with children has become the norm9; the number of female-headed single-parent families has increased10; and fertility rates have declined, with women having fewer children and having them at a later age.11 Although women have benefited from changes in work and family roles,12 there also has been concomitant stress13,14; increased depression in recent cohorts is construed, in part, as a consequence of that stress.
Other researchers have countered that study design limitations unduly influence reported rates.15,16 Considerable evidence of increasing depression in successive post–World War II female cohorts and of age differences within cohorts has come from cross-sectional surveys of lifetime disorder.2,4,5,17–19 Parallel findings for depressive symptoms also have been based on cross-sectional data.20,21 Consequently, some researchers have raised concerns regarding the usefulness of those data for examining age and cohort effects. One concern pertains to the assumption of individual age changes in depression on the basis of cross-sectional differences between individuals of different ages,1 the other to the risk of bias in longer recall intervals for past depression among older individuals.22 Those concerns have been reinforced by unlikely ratios between estimates of lifetime and current depression23 and by recent findings based on longitudinal data that challenge previous assumptions of a cohort effect.24 Indications that cross-sectional data may be misleading in other scientific fields bolster that argument.25,26
The interpretation of reported trends in rates of depressive disorders is further complicated by inconsistent findings across prominent longitudinal studies. The Lundby Study3 found a higher age-standardized incidence rate of depression per year among women in the period 1957–1972 compared with the period 1947–1957; however, this difference was in the rate of mildly impairing depression. In contrast, it was reported in the Stirling County Study that prevalence27 and incidence28 of depression in women remained stable in successive samples drawn over the past 40 years. Costa et al.29 also reported no longitudinal changes in scaled measures of negative and positive affect across a 9-year interval in a national sample of women aged 25–74 years who were first assessed in the early 1970s. However, in the Alameda County Study,30 conducted in 1965, 1974, and 1983, depressive symptoms increased longitudinally among older women, but the age at which symptoms increased was delayed in each successive wave, which suggested a cohort effect. The Midtown Manhattan Longitudinal Study15 classified women by age (40–49 y or 50–59 y) and year of assessment (1954 or 1974) in 2 generation-separated pairs of same-age cohorts. The 1954 cohorts were more impaired (on the General Mental Health Scale); however, a disproportionate loss of married women at follow-up limited the usefulness of the findings. Those discrepancies may be explained in part but not entirely by conceptual and methodological variations.
Our study attempts to separate age and cohort and their association with depression by examining (1) age differences in depression in 2 birth cohorts of women born between 1928 and 1944 or 1945 and 1958 assessed at comparable ages and (2) longitudinal age changes for individual women in successive birth-year cohorts. The study design that permitted these analyses included prospective data on depressive symptoms obtained at 3 points over 10 years in a representative sample of mothers in successive birth-year cohorts that spanned 30 years. Depressive symptoms are widespread among women31,21 and are associated with increased impairment and distress as well as subsequent clinical depression32–35; thus, it is important to document temporal trends accurately.
METHODS
Sample
The women in this study, mothers from a sample of 976 families residing in 1 of 2 upstate New York counties, had at least 1 child aged 1–10 years in 1975; they were randomly selected for a study of childhood behavior. Follow-up with an expanded protocol for mothers that included self-reports of depressive symptoms occurred in 1983, 1985–1986, and 1992–1994; mean age was 31 in 1975 and 39, 42, and 49, respectively, at follow-up.
In 1983, 718 mothers were reinterviewed; 54 mothers, randomly selected from urban poor areas in the same counties to replace that segment of the 1975 sample disproportionately lost to follow-up, were added to the 1983 sample for a total of 772. (More detailed information regarding study methodology is available from previous reports.36,37) The women were 91% White, resided in urban, suburban, and rural areas, spanned the full socioeconomic status (SES) range, and were representative of the sampled region. Retention rate in succeeding follow-ups was over 90%. After selection by birth years of 1928 or later, 701 women remained for analysis in this study.
Procedure
Trained lay interviewers collected study data in the women’s homes. Informed consent, in adherence to institutional guidelines, was obtained.
Index of Depression
A 9-item index of depression, based on the Symptom Checklist-90 Depression Scale,38 was used to assess severity of somatic (low energy, appetite and sleep problems), cognitive (difficulty concentrating), and melancholic (sadness, loss of interest, self-blame, loneliness, hopelessness) symptoms on a 5-point scale (1 = “not at all bothered by in the last year,” 5 = “extremely bothered by . . .”) at follow-ups 1, 2, and 3 (α = .85, .87, and .88, respectively). This index has been significantly associated with marital discord, poor parenting, and offspring reports of internalizing symptoms,39,40 and may reflect the chronic depressive affect found with dysthymia.
Covariates
SES and marital status have been linked to depression in women41,42; thus, they were included in the final model. SES was measured on an additive scale of women’s (and spouses, if married) educational and occupational status and combined family income.43 Marital status was coded 0 if a woman was married (living with a spouse or common law partner) or 1 if unmarried; of the 14.2%, 20.4%, 22.6%, and 23.7% who were unmarried in 1975, 1983, 1985–1986, and 1992–1994, respectively, more than 98% were separated or divorced.
Statistical Analysis
First, depression scores were regressed against age and cohort. To control for an age–cohort confound, we used 1983 scores for women born between 1928 and 1944 (preboomers) and 1992–1994 scores for women born between 1945 and 1958 (baby boomers); thus, the 2 cohorts were assessed at roughly equivalent mean ages: 44.4 (standard deviation [SD] = 4.3, range 38–55) and 43.2 (SD 3.0, range 34–52), respectively. Second, the PROC MIXED procedure from the SAS statistical package (SAS Institute; Cary, NC) was used to estimate random and fixed effects of longitudinal age changes in depression scores within the 10-year period covered by the 3 follow-ups in a multilevel model.44–46 The basic model without fixed predictors examined the between-subject (i.e., random) differences in mean depression scores and changes over time. That model was the basis for examining fixed effects of age, birth year, and the age by birth year interaction. Finally, fixed effects of marital status and SES in follow-ups 1, 2, and 3 were added to the model.
RESULTS
Depression in 2 Age-Matched Birth Cohorts
Mean (SD) and range of depression scores in follow-ups 1, 2, and 3 and across assessments were 18.5 (5.9), 9–40; 18.2 (6.0), 9–42; 17.8 (5.9), 9–43; and 18.1 (5.9), 9–43, respectively. Age was centered at 44; thus, the regression intercept represents the estimated mean score at age 44.
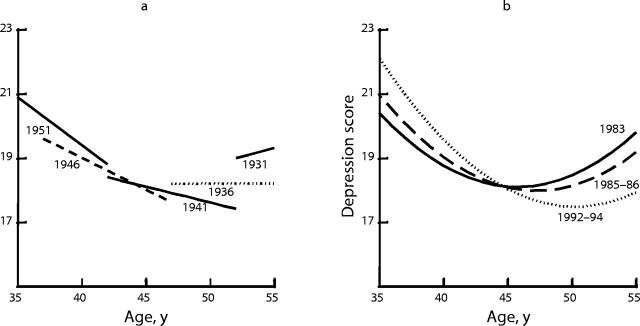
Cohorts were analyzed separately before adjusting for the age–cohort confound (Table 1 ▶). Age differences in depression were not significant in the preboomers; in contrast, an inverse association was noted in the baby boomers (β = −.260; SE = .117; P = .026), for whom depression scores dropped by 4.94 scale points between the ages of 34 and 52 (−.260 × 19 years = 4.94), or about −.84 SD (4.94/5.9). In analyses not shown here, there was no significant quadratic effect of age on depression scores in either the preboomer or the baby boomer cohort: (β = .023, SE = .016, P = .135 and β = −.004, SE = .032, P = .910, respectively). When cohorts were combined, there was no age or cohort association with depression scores; however, there was a significant age by cohort interaction consistent with the contrast noted above (β = −.352; SE = −.132; P = .008). Thus, at age 44, the 2 cohorts did not differ significantly in overall mean depression score; however, unlike the relatively flat age profile of the preboomer cohort, within the baby boomer cohort, older women were less depressed than younger women (Figure 1 ▶). Note that these estimates are sensitive to the age range examined. Depression increased with age among preboomers when the age cutoff was 60; the cutoff here was 55 for assessment age to be comparable between cohorts.
TABLE 1—
Agea and Cohort Differences in Depression Scores in Adult Women Assessed at Equivalent Ages
| Analyses | β | SE | P |
| Preboomer cohortb (n = 388) | |||
| Intercept | 18.312 | .294 | |
| Mean difference per y | .092 | .068 | .179 |
| Baby boomer cohortc (n = 313) | |||
| Intercept | 18.603 | .218 | |
| Mean difference per y | −.260 | .117 | .026 |
| Combined cohorts (n = 701) | |||
| Intercept | 18.312 | .304 | |
| Age at assessment | .092 | .071 | .194 |
| Cohortd | .292 | .463 | .529 |
| Age by cohort interaction | −.352 | .132 | .008 |
Note. SE = standard error; SD = standard deviation.
aAge centered at 44 years.
bMean age at assessment was 44.4 (SD = 4.3, range 38–55) in the preboomer cohort.
cMean age at assessment was 43.2 (SD = 3.0, range 34–52) in the baby boomer cohort.
dPreboomer cohort coded 0; baby boomer cohort coded 1.
Figure 1—
Age differences in depression scores in 2 birth cohorts of women assessed at comparable ages.
Age Changes in Depression by Successive Birth Year Cohorts
Multilevel modeling was used to examine individual birth-year and age-change effects on repeated measures of depression (Table 2 ▶). To reduce confounding between age and birth year, analyses were limited to observations between ages 35 and 55. The basic model examined random between-subject variance of the mean depression score averaged across assessments (23.477), and change over time (.052). The addition of fixed predictors age, birth year, and their interaction improved the fit to the data (χ2 = 15.8; degrees of freedom = 3; P < .01). There was no effect of birth year on depression score, but there was a significant average annual decline in depression score of −.138; moreover, that decline was more rapid in successively later birth years (−.020 per year). Thus, the model-estimated annual change in depression score was +.062 for women born in 1933, 10 years before the average birth year of 1943 (calculated as average annual decline .02 × 10 years) and −.338 for women born 10 years after, in 1953 (average annual decline .020 × 10 years). After consideration of the fixed predictor effects, random variance effects were estimated at 23.115 and .035, respectively, for between-subject differences in mean depression score and change over time. The model accounted for 1.5% ([23.477 − 23.115] / 23.477) and 32.7% ([.052 − .035] / .052) of the variance in mean depression score and change over time, respectively. That differential reflects the absence of a significant difference in mean depression scores in the preboomer and baby boomer cohorts in the prior analysis.
TABLE 2—
Two-Level Growth Models of Age and Cohort Effects on Depression Scores in Women Aged Between 35 and 55 Yearsa
| Basic Model | Predictors | Predictors and Covariates | ||||
| β | SE | β | SE | β | SE | |
| Random variance | ||||||
| Intercept | 23.477*** | 1.750 | 23.115*** | 1.732 | 21.447*** | 1.647 |
| Slope | 0.052 | 0.036 | 0.035 | 0.035 | 0.032 | 0.034 |
| Residual | 11.694*** | 0.865 | 11.83*** | 0.868 | 11.798*** | 0.855 |
| Fixed effects | ||||||
| Intercept | 18.203*** | 0.243 | 17.935*** | 0.252 | ||
| Age | −0.138*** | 0.036 | −0.097* | 0.039 | ||
| Birth year | 0.012 | 0.049 | 0.003 | 0.048 | ||
| Age–birth year | −0.020** | 0.008 | −0.017* | 0.008 | ||
| SES | −0.953*** | 0.200 | ||||
| Marital status | 1.724** | 0.562 | ||||
| Age–marital status | −0.262** | 0.089 | ||||
| Goodness of fitb | ||||||
| Parameters | 4 | 7 | 10 | |||
| Raw likelihood (−2LL) | 7 978.6 | 7 962.8 | 7 819.6 | |||
| χ2 | 15.8** | 159.0*** | ||||
| Degrees of freedom | 3 | 6 | ||||
Note. SE = standard error; SES = socioeconomic status; LL = log likelihood.
aAll parameter entries are maximum likelihood estimates fitted using SAS PROC MIXED. Age was centered at 44 years, birth year at 1943, and SES at the scaled mean.
bPredictor and predictor and covariate models are compared with the basic model.
*P < .05; **P < .01; ***P < .001
Fixed effects of covariates SES and marital status and the marital status by age change interaction were added to the predictor model. Mean depression scores were lower in high SES women (β = −.953, SE = .200, P < .001) and higher in unmarried women (β = 1.724, SE = .562, P < .01); however, scores declined with age more rapidly in unmarried women than in married women (β = −.262 [per year]; SE = .089; P < .01). Predictor model effects of a decline in depression with age and a more rapid decline in later birth years remained. The final model accounted for 8.6% and 38.5% of the variance in mean depression scores and change over time, respectively.
Do These Findings Fit Prior Cross-Sectional Findings?
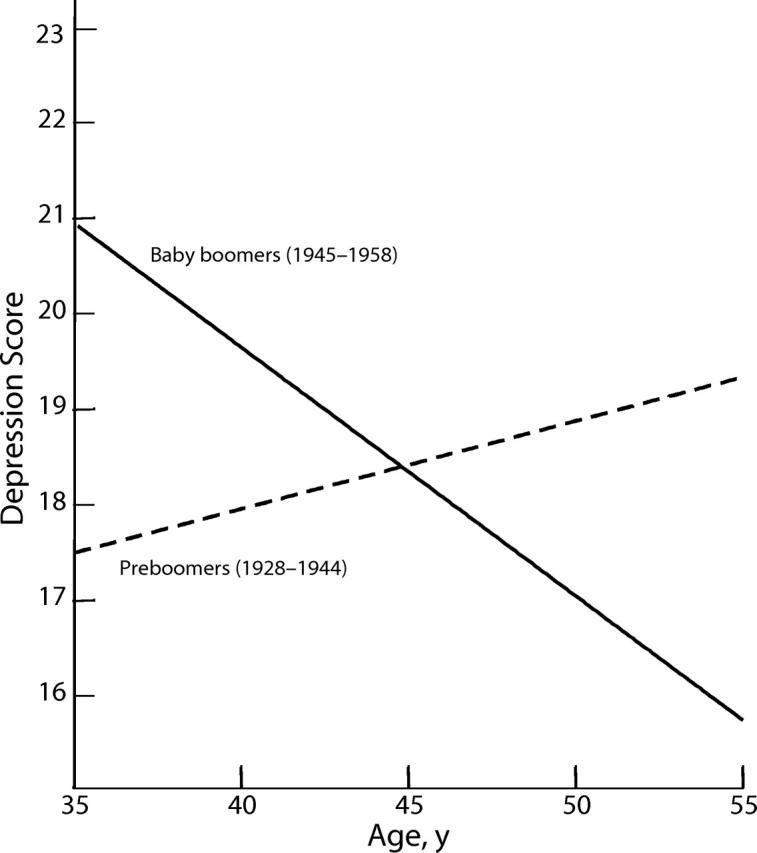
Consistent with others’ findings,2–5 more recent cohorts reported more depression in their youngest years; however, that early vulnerability was reversed in middle age. Figure 2a ▶ illustrates model-estimated depression scores plotted longitudinally for 5 single birth-year cohorts selected at 5-year intervals (1931–1951). Younger women in more recent cohorts had higher depression scores, but declines were steeper in successive cohorts as they aged. In contrast, depression scores in earlier cohorts declined more slowly (1941), remained fairly stable (1936), and, in the earliest (1931), increased with age.
Figure 2—
Two plots of the same depression scores: (a) longitudinal age changes in depression assessed in 5 female birth-year cohorts and (b) cross-sectional age differences in depression in 3 samples of women.
The discrepancy between the concave age curves in previously published cross-sectional data and trajectories depicted in Figure 2a ▶ may be due more to an age–cohort confound in earlier studies than to inconsistent findings. Figure 2b ▶ demonstrates the same depression scores plotted again, not by longitudinal age changes as in Figure 2a ▶ but by age at assessment in each wave of data. Thus, each line represents age differences in depression scores in 3 separate cross-sectional “samples.” The predicted U-shaped distribution typical of other cross-sectional data21 is indicated: depression declines with age in all 3 samples until, on average, approximately age 50, when it begins to rise. However, where ages overlap, the decline in each successive sample is steeper and persists for a longer time; furthermore, the rise at the greatest ages was smaller and more delayed. Appearance notwithstanding, Figure 2b ▶ is compatible with Figure 2a ▶: comparisons across overlapping ages in the successive cross-sectional samples support more depression among the youngest in more recent cohorts, whereas successive shifts in the curves suggest a cohort effect. Because the age overlap across birth cohorts is limited, we cannot project with any degree of accuracy whether that trend will continue as the most recent cohorts finish the sixth decade of life.
DISCUSSION
The analyses yielded 3 significant findings that merit discussion. First, more depression among the younger women in more recent cohorts may be explained by the historic shift in family and work-role norms for women. Workforce participation by women tripled between 1950 and 1986,47 particularly among married women with young children, who might have been more susceptible to the stress of juggling the demands of multiple roles.48 Moreover, certain conditions under which a disproportionate number of women work—low status, low pay, work overload, depersonalization, and inadequate rewards—have been associated with increased depression.13 In contrast, role factors that protect against depression, higher employment status and earnings, and reduced child care responsibilities typically peak by late middle age among women in more recent cohorts.49,50 Failure to find any mean difference in depression between 2 different birth cohorts of women assessed at parallel ages did not support the alternative conclusion of a period effect; nonetheless, it cannot be ruled out. Others have reported a peak in depression among women and men between 1960 and 1980, regardless of age, which may reflect the general social instability and upheaval of that period.5,30,51 The 10 years between assessments in the current study may be too short an interval to detect such an effect.
The second finding, supported here by cross-sectional and longitudinal analyses, is that intraindividual age changes in depression have been shifting in successive cohorts of women born after World War II. Depression scores declined with age more rapidly in more recent cohorts than in earlier cohorts; furthermore, this effect remained after controlling for SES and marital status. Possibly a gradual increase in health status among older women may account for these cohort effects, but given the more rapid changes in women’s roles it seems more likely that historical influences were in operation. In earlier generations of women, a traditional role was normative and other choices were few. Yet, by late middle age, family role wanes, particularly for mothers; consequently, less purposeful activities or opportunities for fulfillment await those whose focus was limited to that role. Increased depression in late middle age has been linked to traits correlated with traditional female roles.52 In contrast, more recent cohorts of women are expected to seek out multifaceted identities from a broad range of life roles; thus, by middle age these women may have reaped the rewards of taking on more challenges and more roles. Given that paradigm, the public health policy implications are twofold: to initiate or continue social programs that reduce the stress of balancing multiple family and work roles among younger women, and to afford middle-aged women opportunities to continue in productive life roles.
Consistent with others’ findings,41,42 advantaged SES status and being married were associated with less depression across the ages assessed. The decline in depression with age was more rapid among unmarried women than married women. Psychological distress due to marital breakup may be alleviated by increased acceptance of divorce as normative and by the growing economic independence of women.53 Despite the negative repercussions of divorce, not being married may be preferable to a conflict-ridden or stressful marriage.
The third finding is that what might appear to be age effects as deduced from cross-sectional data may represent a combination of age, cohort, and, potentially, period effects. We did not examine longitudinal trajectories of depression scores in individual women in the first set of analyses (Table 1 ▶) because we do not yet have a second point of assessment where age is comparable in the 2 birth cohorts. However, the significant discrepancy between the 2 cohorts in the pattern of age differences when assessed at nearly equivalent ages suggests that previous reports may indeed confound age and cohort effects.
Limitations in these data warrant attention. First, age and cohort effects on depression are assessed in a mother-only sample and may differ for other women. Role factors associated with depression in women (e.g., partner abuse) may have different connotations in mothers versus women without children; moreover, certain associations may not be applicable to the latter (e.g., parenting and psychological distress54). However, findings here may be generalized to women with children, who still represent the majority of the female population. Next, we employed a depression scale of symptom severity, which cannot be expected to follow the same pattern as lifetime incidence of depressive disorders. Lastly, the overlap of studied ages for women in different cohorts covered a smaller portion of the adult years than would be desirable for unambiguous interpretation; thus, we cannot project with any degree of accuracy whether temporal trends indicated here will continue as these cohorts age and infirmities, financial concerns, and spousal loss are more prevalent.
Another consideration is the tendency for symptom reports to decline on reassessment. That attenuation effect is a concern in estimating reliability, whether reported on a current55 or lifetime basis56; however, there are reasons why attenuation does not fully account for the individual changes in depression found here. First, attenuation is observed when reassessments are carried out in short intervals to minimize potential real change; here, the intervals were approximately 3 and 7 years, longer than expected for such effects. Second, attenuation is greater with reassessment of diagnoses, especially in cases at or near diagnostic threshold, than with reassessment of symptom severity, which is less susceptible to a threshold effect.57 Third, most attenuation appears at first reassessment, with little decline thereafter; this is contrary to the pattern observed here, where decline was greater per year between the second and third assessments, regardless of age or birth year. Possibly this steeper slope represents a period effect of an accelerated decline from the peak in depression noted between 1960 and 1980. The data herein may be indicative of a continuation of that decline; however, additional data points will be needed to specify age, cohort, and period effects.
Acknowledgments
This study was supported by the National Institute of Child Health and Human Development (grant HD-40685).
Human Participant Protection This study was approved by the institutional review board of New York State Psychiatric Institute. Informants participated under conditions of informed consent in adherence to institutional guidelines.
Contributors S. Kasen and P. Cohen (co–principal investigators) were responsible for conceptualization and design of the study and data collection. S. Kasen analyzed the data, interpreted the findings, and drafted the article. P. Cohen supervised the data analysis and assisted with the interpretation of findings and the critical revision of the article. H. Chen assisted with the study design and supervision of the data analysis and contributed to the critical revision of the article. D. Castille assisted with data collection, the interpretation of findings, and the critical revision of the article.
Peer Reviewed
References
- 1.Fombonne E. Time trends in affective disorders. In: Cohen P, Slomkowski C, Robins LN, eds. Historical and Geographic Influences on Psychopathology. Mahwah, NJ: L. Erlbaum Associates; 1999.
- 2.Cross-National Collaborative Group. The changing rate of major depression: cross-national comparisons. JAMA. 1992;268:3098–3105. [DOI] [PubMed] [Google Scholar]
- 3.Hagnell O, Lanke J, Rorsman B, Ojesjo L. Are we entering an age of melancholy? Depressive illnesses in a prospective epidemiological study over 25 years: the Lundby Study, Sweden. Psychol Med. 1982;12:279–289. [DOI] [PubMed] [Google Scholar]
- 4.Klerman GL, Weissman MM. Increasing rates of depression. JAMA. 1989;261:2229–2235. [PubMed] [Google Scholar]
- 5.Wickramaratne PJ, Weissman MM, Leaf PJ, Holford TR. Age, period and cohort effects on the risk of major depression: results from five United States communities. J Clin Epidemiol. 1989;42:333–343. [DOI] [PubMed] [Google Scholar]
- 6.Historical Statistics of the United States, Colonial Times to 1970s: Part I. Washington, DC: Bureau of the Census, US Dept of Commerce; 1975.
- 7.Reskin BF, Padavic I. Women and Men at Work. Thousand Oaks, Calif: Pine Forge Press; 1994.
- 8.Aube J, Fleury J, Smetana J. Changes in women’s roles: impact on and social policy implications for the mental health of women. Dev Psychopathol. 2000;12:633–656. [DOI] [PubMed] [Google Scholar]
- 9.Bond JT, Galinsky E, Swanberg JE. The 1997 National Study of the Changing Workforce. New York, NY: Families and Work Institute; 1998.
- 10.Furstenberg FF Jr. Divorce and the American family. Am Rev Sociol. 1990;16:379–403. [Google Scholar]
- 11.Bianchi SM, Spain D. American Women: Three Decades of Change. Washington, DC: US Dept of Commerce, Bureau of the Census; 1983.
- 12.Barnett RC, Hyde JS. Women, men, work, and family: an expansionist theory. Am Psychol. 2001;56:781–796. [DOI] [PubMed] [Google Scholar]
- 13.Aneshensel CS. Marital and employment role strain, social support, and depression among adult women. In: Hobfoll SE, ed. Stress, Social Support, and Women. New York, NY: Hemisphere; 1986:99–114.
- 14.Kandel DB, Davies M, Raveis VH. The stressfulness of daily social roles for women: marital, occupational and household roles. J Health Soc Behav. 1985;26:64–78. [PubMed] [Google Scholar]
- 15.Srole L, Fischer AK. The Midtown Manhattan Longitudinal Study vs “the Mental Paradise Lost” doctrine: a controversy joined. Arch Gen Psychiatry. 1980;37:209–221. [DOI] [PubMed] [Google Scholar]
- 16.Hasin D, Link B. Age and recognition of depression: implications for a cohort effect in major depression. Psychol Med. 1988;18:683–688. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. [DOI] [PubMed] [Google Scholar]
- 18.Robins LN, Locke BZ, Regier DA. An overview of psychiatric disorders in America. In: Robins LN, Regier DA, eds. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, NY: Free Press; 1991:328–366.
- 19.Weissman MM, Bruce ML, Leaf PJ, Florio LP, Holzer C. Affective disorders. In: Robins LN, Regier DA, eds. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, NY: Free Press; 1991:53–80.
- 20.Kessler RC, McRae JA Jr. Trends in the relationship between sex and psychological distress: 1957–1976. Am Sociol Rev. 1981;46:443–452. [PubMed] [Google Scholar]
- 21.Kessler RC, Foster C, Webster PS, House JS. The relationship between age and depressive symptoms in two national surveys. Psychol Aging. 1992;7:119–126. [DOI] [PubMed] [Google Scholar]
- 22.Aneshensel CS, Estrada AL, Hansell MJ, Clark VA. Social psychological aspects of reporting behavior: lifetime depressive episode reports. J Health Soc Behav. 1987;28:232–246. [PubMed] [Google Scholar]
- 23.Parker G. Are the lifetime prevalence estimates in the ECA study accurate? Psychol Med. 1987;17:275–282. [DOI] [PubMed] [Google Scholar]
- 24.Gallo JJ, Rabins PV, Anthony JC. Sadness in older persons: 13-year follow-up of a community sample in Baltimore, Maryland. Psychol Med. 1999;29:341–350. [DOI] [PubMed] [Google Scholar]
- 25.Berger MPF. A comparison of efficiencies of longitudinal, mixed longitudinal, and cross sectional designs. J Educ Stat. 1986;11:171–181. [Google Scholar]
- 26.Kraemer HC, Yesavage JA, Taylor JL, Kupfer D. How can we learn about developmental processes from cross-sectional studies, or can we? Am J Psychiatry. 2000;157:162–171. [DOI] [PubMed] [Google Scholar]
- 27.Murphy JM, Laird NM, Monson RR, Sobol AM, Leighton AH. A 40-year perspective on the prevalence of depression. Arch Gen Psychiatry. 2000;57:209–215. [DOI] [PubMed] [Google Scholar]
- 28.Murphy JM, Laird NM, Monson RR, Sobol AM, Leighton AH. Incidence of depression in the Stirling County Study: historical and comparative perspectives. Psychol Med. 2000;30:505–514. [DOI] [PubMed] [Google Scholar]
- 29.Costa PT Jr, Zonderman AB, McCrae RR, Cornoni-Huntley J, Locke BZ, Barbano HE. Longitudinal analyses of psychological well-being in a national sample: stability of mean levels. J Gerontol. 1987;42:50–55. [DOI] [PubMed] [Google Scholar]
- 30.Roberts RE, Lee ES, Roberts CR. Changes in prevalence of depressive symptoms in Alameda County. J Aging Health. 1991;3:66–86. [Google Scholar]
- 31.Weissman MM, Boyd JH. The epidemiology of affective disorders: rates and risk factors. In: Grinspoon L, ed. Psychiatry Update: American Psychiatric Association Annual Review. Vol II. Washington, DC: American Psychiatric Association; 1983:406–428.
- 32.Johnson J, Weissman MM, Klerman GL. Service utilization and social morbidity with depressive symptoms in the community. JAMA. 1992;267:1478–1483. [PubMed] [Google Scholar]
- 33.Broadhead WE, Blazer DG, George LK, Tse CK. Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA. 1990; 264:2524–2528. [PubMed] [Google Scholar]
- 34.Horwath E, Johnson J, Klerman GL, Weissman MM. Depressive symptoms as relative and attributable risk factors for first-onset major depression. Arch Gen Psychiatry. 1992;49:817–823. [DOI] [PubMed] [Google Scholar]
- 35.Zonderman AB, Herbst JH, Schmidt C Jr, Costa PT Jr, McCrae RR. Depressive symptoms as a nonspecific, graded risk for psychiatric diagnoses. J Abnormal Psychol. 1993;102:544–552. [DOI] [PubMed] [Google Scholar]
- 36.Cohen P, Cohen J. Life Values and Adolescent Mental Health. Mahwah, NJ: L. Erlbaum Associates; 1996.
- 37.Kogan LS, Smith J, Jenkins S. Ecological validity of indicator data as predictors of survey findings. J Soc Serv Res. 1977;1:117–132. [Google Scholar]
- 38.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Check List (HSCL): a self-report inventory. Behav Sci. 1974;19:1–15. [DOI] [PubMed] [Google Scholar]
- 39.Crawford TN, Cohen P, Midlarsky E, Brook JS. Internalizing symptoms in adolescents: gender differences in vulnerability to parental distress and discord. J Res Adolesc. 2001;11:95–118. [Google Scholar]
- 40.Johnson JG, Cohen P, Kasen S, Smailes E, Brook JS. Association of maladaptive parental behavior with psychiatric disorder among parents and their offspring. Arch Gen Psychiatry. 2001;58:453–460. [DOI] [PubMed] [Google Scholar]
- 41.Kessler RC, Cleary PD. Social class and psychological distress. Am Sociol Rev. 1980;45:463–478. [PubMed] [Google Scholar]
- 42.Gove WR, Hughes M, Style CB. Does marriage have positive effects on the psychological well-being of the individual? J Health Soc Behav. 1984;24:122–131. [PubMed] [Google Scholar]
- 43.Hollingshead AB, Redlich FC. Social Class and Mental Illness: A Community Study. New York, NY: John Wiley & Sons Inc.; 1958. [DOI] [PMC free article] [PubMed]
- 44.McArdle JJ, Bell RQ. An introduction to latent growth models for developmental data analysis. In: Little TD, Schnabel KU, Baumert J, eds. Modeling Longitudinal and Multiple Group Data: Practical Issues, Applied Approaches, and Specific Examples. Mahwah, NJ: Erlbaum; 2000:69–107.
- 45.Littell RC, Miliken GA, Stroup WW, Wolfinger RD. SAS System for Mixed Models. Cary, NC: SAS Institute; 1996.
- 46.Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat. 1998;23:323–355. [Google Scholar]
- 47.Hayghe H. Rise in mothers’ labor force activity includes those with infants. Mon Labor Rev. 1986;109:43–45. [Google Scholar]
- 48.Hochschild A. The Second Shift: Working Parents and the Revolution at Home. New York: Viking; 1989.
- 49.Kessler RC, Turner JB, House JS. Unemployment, reemployment, and emotional functioning in a community sample. Am Sociol Rev. 1989;54:648–657. [Google Scholar]
- 50.Baruch GK, Barnett R. Role quality, multiple role involvement, and psychological well-being in midlife women. J Pers Soc Psychol. 1986;51:578–585. [Google Scholar]
- 51.Leon AC, Klerman GL, Wickramaratne P. Continuing female predominance in depressive illness. Am J Public Health. 1993;83:754–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bromberger JT, Matthews KA. A “feminine” model of vulnerability to depressive symptoms: a longitudinal investigation of middle-aged women. J Pers Soc Psychol. 1996;70:591–598. [DOI] [PubMed] [Google Scholar]
- 53.Heidemann B, Suhomlinova O, O’Rand A. Economic independence, economic status, and empty nest in midlife marital disruption. J Marriage Fam. 1998;60:219–231. [Google Scholar]
- 54.Barnett RC, Brennan RT, Marshall NL. Gender and the relationship between parent role quality and psychological distress: a study of men and women in dual-earner couples. J Fam Issues. 1994;15:229–252. [Google Scholar]
- 55.Shaffer D, Fisher PW, Lucas CP. Respondent-based interviews. In: Shaffer D, Lucas CP, Richters JC, eds. Diagnostic Assessment in Child and Adolescent Psychopathology. New York, NY: Guilford Press; 1999:3–33.
- 56.Bromet EJ, Dunn LO, Connell MM, Dew MA, Schulberg HC. Long-term reliability of diagnosing lifetime major depression in a community sample. Arch Gen Psychiatry. 1986; 43:435–440. [DOI] [PubMed] [Google Scholar]
- 57.Jensen P, Roper M, Fisher P, et al. Test-retest reliability of the Diagnostic Interview Schedule for Children (DISC 2.1). Parent, child, and combined algorithms. Arch Gen Psychiatry. 1995;52:61–71. [DOI] [PubMed] [Google Scholar]