Abstract
Objective
Propensity score analyses attempt to control for confounding in non-experimental studies by adjusting for the likelihood that a given patient is exposed. Such analyses have been proposed to address confounding by indication, but there is little empirical evidence that they achieve better control than conventional multivariate outcome modeling.
Study design and methods
Using PubMed and Science Citation Index, we assessed the use of propensity scores over time and critically evaluated studies published through 2003.
Results
Use of propensity scores increased from a total of 8 papers before 1998 to 71 in 2003. Most of the 177 published studies abstracted assessed medications (N=60) or surgical interventions (N=51), mainly in cardiology and cardiac surgery (N=90). Whether PS methods or conventional outcome models were used to control for confounding had little effect on results in those studies in which such comparison was possible. Only 9 out of 69 studies (13%) had an effect estimate that differed by more than 20% from that obtained with a conventional outcome model in all PS analyses presented.
Conclusions
Publication of results based on propensity score methods has increased dramatically, but there is little evidence that these methods yield substantially different estimates compared with conventional multivariable methods.
Keywords: propensity score, epidemiology, confounding, bias, statistical methods, clinical effectiveness
Introduction
Randomized controlled trials are considered the gold standard for assessing the efficacy of medications, medical procedures, or clinical strategies. Nevertheless, particularly for research on the prevention of chronic disease, randomized trials are often infeasible because of their size, time, and budget requirements, questionable generalizability, and ethical constraints .[1]
On the other hand, non-experimental studies of interventions have frequently been criticized because of their potential for selection bias. This concern reached a crescendo with the disparity in estimated effects of hormone replacement therapy from randomized trials and non-experimental studies.[2] This imbroglio highlighted the need to develop and apply improved methods to reduce bias in non-experimental studies in which selection bias or confounding is likely to occur.[3]
The use of multivariate confounder scores to combine many covariates into a single variable can be traced back to Miettinen in 1976.[4] In 1983, Rosenbaum and Rubin developed the concept of propensity scores (PS) estimated at baseline to control for selection bias in cohort studies.[5] This technique has become popular to control confounding bias in epidemiologic studies that assess the outcomes of drugs and medical procedures. Propensity scores estimate the predicted probability (propensity) of use of a given drug or procedure in a particular subject, based on his or her characteristics when the treatment is chosen. In principle, the effect of the treatment can then be measured among patients who have the same predicted propensity of treatment, thus controlling for confounding.[5] Use of PS to reduce bias is especially appealing since, under the assumption that all relevant predictors of treatment have been adequately captured, subjects with the same PS should have the same chance of receiving treatment. Therefore, PS are often conceptualized as mimicking randomized trials, although they do so only with respect to factors that have been adequately measured. Randomization, in contrast, removes bias from both measured and unmeasured factors. PS allow simultaneous control for confounding by several variables in situations where conventional multivariable models might not be appropriate, owing to the small number of outcomes. PS, however, are frequently used in settings where the outcome is common; their value in this situation is not yet clear. We sought to review the application of PS in the medical literature and to assess its practical value.
Propensity scores
Background
A propensity score (PS) can be defined as the probability of exposure to e.g. a treatment given observed covariates.[5] The score is usually estimated using a multivariable logistic regression model, but can be estimated with a variety of multivariable scoring functions. In a logistic model, the scores range from 0 to 1 and reflect the estimated probability, based on the subject’s characteristics, that the subject will receive the treatment of interest, such that individuals with the same estimated PS have the same chance of receiving treatment. Any two subjects with the same PS can have different values for specific covariates, but overall, covariates entered in the PS model will tend to be balanced for treated and untreated subjects with similar PS. This balance of covariates can easily be checked and the performance of PS to achieve this goal can be clearly communicated, e.g. by presenting the distribution of covariates in exposed and unexposed separately, stratified by quintiles of the PS.
By estimating the PS and analyzing the data within homogeneous levels of PS, in theory one can achieve a ‘virtual randomization’, in which comparable patients are separated into the exposed and unexposed groups. Since PS are estimated using measured data, however, they cannot control for unmeasured or imperfectly measured variables. Therefore, residual systematic bias cannot be excluded.
Once PS are estimated they can be used in various ways to control for selection bias or confounding in non-experimental cohort studies. Possible implementations include matching on the PS, stratified analysis using PS as the stratification variable, and combinations of these two approaches with conventional multivariable outcome modeling. In theory, within each PS stratum, some patients will have received the treatment of interest while others will not. In practice, however, this is not always the case (see figure 1) and how one uses PS in analyses can make a difference.
Figure 1.
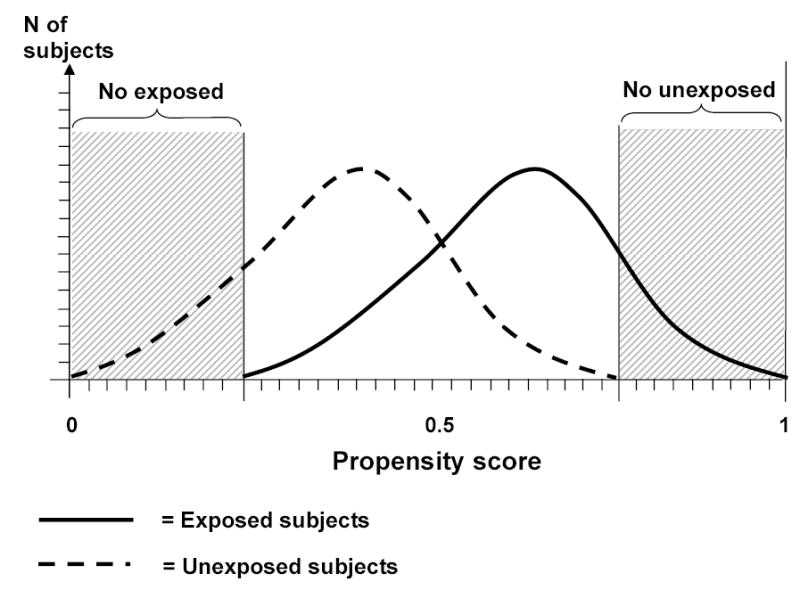
Non-overlap of the propensity score distributions among exposed and unexposed subjects*
* In this example subjects with low propensity scores are never exposed while subjects with high propensity scores are always exposed
Alternative ways to apply propensity scores
Matching
One strategy is to match each exposed subject to one or more unexposed subjects with a similar PS, thus avoiding the complexity of matching within multiple strata.[6] A variety of matching methods are available to identify unexposed subjects with PS similar to those of exposed subjects.[7,8] Effective balancing is achieved by any matching procedure that produces good agreement between the mean PS in exposed and unexposed subjects.[9] Selecting an equal number of exposed and unexposed subjects within categories of the PS (frequency matching) instead of individual matching enables the inclusion of exposed subjects for whom no exact unexposed match can be found, but may introduce bias stemming from non-overlapping ranges for exposed and unexposed subjects at the extremes of the distribution of the PS.[6] This bias can be avoided by restricting analyses to the range of PS common to both exposed and unexposed patients, i.e. excluding unexposed patients with a PS lower than the lowest PS observed in exposed patients and excluding exposed patients with a PS higher than the highest PS observed in unexposed patients. Plotting the PS distribution for exposed and unexposed subjects is an easy diagnostic for non-overlap (see figure 1).
Sub-classification on propensity score
As an alternative to matching, one can include all available subjects in an analysis and control for the PS. This can be achieved by simple stratification or modeling of the PS-disease association, e.g. as a continuous covariate. Often, a model with indicator variables for quintiles of the observed PS is used,[10] but control for confounding may be better when PS are modeled as continuous variables.[11] Again, inclusion of all subjects might introduce bias due to inclusion of subjects with a PS from outside the mutual range of scores among exposed and unexposed. Similar to matching, this bias may be reduced by excluding unexposed patients with a PS lower than the lowest PS observed in exposed patients and vice versa.
Combinations with ‘traditional’ multivariate outcome modeling
An issue of some controversy in use of PS is whether better control of confounding can be achieved, and hence better estimates of the effect of the treatment on the outcome can be obtained, by including the PS along with other important predictors of the outcome.[12,13] In theory, confounding can be controlled and a treatment effect can be estimated validly if only one of the two models - the treatment model (PS) or the outcome model (‘traditional’ multivariate modeling) - is specified correctly. Strategies that include both approaches, and thus involve possibly redundant control of confounding, have therefore been called ‘doubly robust’.[14] The theory behind these methods is complex, however, and software tools with adequate documentation are not yet available.
Literature search and abstraction
We identified studies in which the propensity score was used through PubMed and Science Citation Index. Initially, a keyword search was performed through PubMed, identifying studies including the term “propensity”. This broad search yielded 5311 unduplicated references published through December 31, 2003. After review of the abstracts, we identified 167 articles that used propensity score methods in the study of medical interventions and health outcomes (excluding articles focusing solely on methodological or statistical aspects, editorials, review articles or letters, and foreign language articles). To increase the sensitivity of our search, we also searched for articles that cited one of the important propensity score methods articles.[5, 6, 13, 15–17] This search yielded another 73 articles. All these papers were obtained and read by one of the authors. We excluded 48 articles that did not include analysis of data (28), randomized clinical trials (9), case-control studies (2), and articles primarily analyzing cost-effectiveness (6) or practice patterns (3).
Results
Our search revealed 58 substantive medical research studies that used PS in 2003,[18–75] 38 in 2002,[76–113] 28 in 2001, [114–141] 6 in 2000, [142–147] 5 in 1999, [148–152] 5 in 1998, [153–157] and a total of 5 before 1998 [158–162]. Additional articles found through a citation search of the significant methods articles written about PS, using Science Citation Index, yielded 13 medical research studies that used PS in 2003,[163–175]13 in 2002,[176–188] 11 in 2001,[189–199] 3 in 2000,[200–202]1 in 1999, [ 203], 3 in 1998, [204–206] and a total of 3 before 1998 [207–209]. We present the number of studies with results based on PS methods published in each of these years in figure 2.
Figure 2.
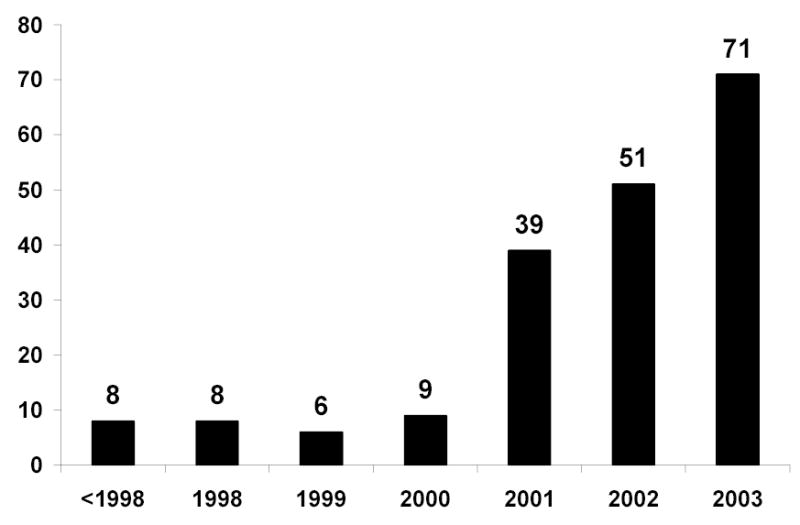
Number of medical research studies listed in PubMed and Science Citation Index using propensity score methods to control for confounding according to year of publication
After further review of articles, fifteen articles were excluded from further analysis as the outcomes were continuous and it was not possible to calculate an odds ratio or risk ratio [59, 86, 88, 111, 120, 124, 137, 150, 152, 160, 162, 193, 195, 196, 206]. The final selection of studies abstracted comprised 70 articles from 2003, 48 articles from 2002, 33 articles from 2001, 9 from 2000, 4 from 1999, 7 from 1998 and 6 articles before 1998.
For all selected papers published through 2003 we abstracted the following items: the number of variables used to predict treatment and outcome, respectively; the unadjusted (crude) estimate for the treatment-outcome association; the estimates for the treatment-outcome association adjusted by use of PS matching, PS adjustment, and/or multivariable outcome models, including models without PS and with PS as well as covariates; the predictive value of the PS as assessed by the area under the receiver operating characteristic (ROC) curve (equivalent to the c-statistic in logistic regression); and the percent of exposed participants that could be matched to unexposed participants (where applicable). We extracted or calculated odds ratios or relative risks whenever adequate data were presented.
In table 1, studies published in 2003 are presented. Corresponding tables for the years 2002 and prior years are included in the e-Extra online version. The following results are based on all 177 substantive studies reporting on dichotomous exposures and outcomes published through 2003. Among the medical specialties covered in these papers were cardiology (including cardiac and vascular surgery) (N=90), general internal medicine (N=34), oncology (N=20), nephrology (N=9), psychiatry (N=4), and rheumatology (N=2). The treatments studied included medications (N=60), surgical interventions (N=51), catheterization (N=13),other medical procedures (including care after myocardial infarction and in end-stage renal failure), lifestyle factors, or a wide variety of other comparisons. The main outcome assessed was mortality (N=118). Other outcomes included myocardial infarction (N=6), stroke (N=3), and a wide variety of other outcomes including complications of infection, gastrointestinal events, and emergency hospitalizations.
Table 1.
Substantive studies in 2003 using propensity score methods (PS)*
| Size |
Exposure |
Outcome |
Multivariable outcome modeling† |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | N | N | # of variables in model | N | # of variables in model | Crude | PS matching | PS adjustment | without PS | PS and covariates | AUC‡ | % matched§ | ||
| Allen-Ramey, Duong, Goodman, et al.21 | 960 | Inhaled steroids | 153 | ? | Hospitalizations | ? | Na | ? | - | - | - | 1.9 (0.7–4.6) | ? | Na |
| Bhatt, Chew, Lincoff, et al. 26 | 10,480 | Revascularization in acute CAD | 4175 | ? | Mortality | ~640 | 15 | ? | - | - | 0.8 (0.6–1.0) | ? | 0.84 | Na |
| Horwitz, Berlin, Sauer, et al.165 | 18,821 | Glycoprotein inhibitors | 2525 | 23 | Bleeding | 215 | Na | 1.9 (1.4–2.6) | - | 1.4 (1.0–2.0) | - | - | ? | Na |
| Rubins, Nelson, Noorbaloochi, et al. 64 | 16,470 | Lipid lowering drugs | 7012 | 31 | Mortality | 6066 | Na | 0.5 (0.5–0.5) | - | 0.8 (0.7–0.9) | - | 0.8 (0.7–0.8) | 0.83 | Na |
| Seeger, Walker, Williams, et al.68 | 8288 | Statins | 4144 | 58 | MI | 325 | Na | 2.1 (1.5–3.0) | 0.7 (0.5–0.9) | - | - | - | 0.92 | 70% |
| Vakili, Kaplan, Slater, et al.72 | 10,847 | Glycoprotein inhibitors in PTCA | 2183 | 17 | Mortality, CABG, MI | 507 | Na | 2.1 (1.7–2.6) | - | 1.5 (1.2–1.9) | - | 1.6 (1.2–2.0) | ? | Na |
| Schwarz, Smith, Keny, et al.67 | 61 | Intra-OP radiation in pancreatic-CA | 30 | ? | Mortality | ~46 | Na | “sign. diff.” | - | 1.5 (0.8–2.9) | - | 1.7 (p=0.3) | ? | Na |
| Ishani, Ibrahim, Gilbertson,et al.49 | 4046 | Residual renal function | 424 | 17 | Graft failure | 443 | 13 | 1.0 (0.8–1.4) | - | - | 1.0 (0.7–1.3) | 1.0 (0.7–1.3) | ? | Na |
| Cho, Bhatt, Marso, et al.34 | 7897 | Catheterizati on in acute MI | 3361 | ? | Mortality | 590 | 4 | 0.5 | - | 0.7 (0.6–0.8) | 0.5 (0.1–0.8) | - | 0.74 | Na |
| Harbarth, Garbino, Pugin, et al.46 | 904 | Inappropriate AB therapy | 211 | ? | Mortality | 250 | 20 | 2.0 (1.4–2.8) | - | - | - | 1.8 (1.2–2.6) | ? | Na |
| Leon, Solomon, Mueller, et al.56 | 285 | Antidepressa nt therapy | ? | 11 | Recovery | ? | Na | ? | - | 1.9 (1.3–2.7) | - | - | ? | Na |
| Urbach, Bell, Swanstrom,et al.174 | 1919 | Bile bypass in pancreatic CA | 945 | 23 | Mortality | 1845 | 24 | 1.2 (1.1–1.4) | - | 1.2 (1.1–1.3) | 1.2 (1.1–1.3) | - | 0.62 | Na |
| Ascione, Narayan, Rogers, et al.23 | 250 | Off vs on pump CABG | 74 | 38 | Mortality | 50 | Na | 2.5 (1.1–5.0) | - | 2.0 (0.8–5.0) | - | - | ? | Na |
| Boening, Friedrich, Hedderich, et al.27 | 650 | Off vs on pump CABG | 133 | 14 | Mortality | 3 | Na | ? | 2.7 (0.2–31) | - | - | - | ? | 54% |
| Calafiore, Di Mauro, Canosa, et al.30 | 1266 | Off vs on pump CABG | 510 | 24 | Mortality | 46 | Na | ? | 0.5 (0.3–1.0) | - | - | 0.3 (0.2–0.5) | ? | ? |
| Hamamoto, Bando, Kobayashi, et al.45 | 379 | Heart valve surgery | 80 | ? | Mortality | 53 | 6 | ? | - | - | - | 1.0 (0.5–2.0) | ? | Na |
| Kurlansky, Williams, Traad, et al.54 | 987 | Arterial vs venous graft CABG | 413 | 26 | Mortality | 403 | 25 | ? | ? | - | 0.8 (0.6–1.0) | - | ? | ? |
| Srinivasan, Grayson, Pullan,et al.69 | ? | Preop aspirin in CABG | 170 | 10 | Mortality | 5 | Na | ? | 0.7 | - | - | - | 0.68 | ? |
| Stamou, Kapetanakis ,Lowery, et al.70 | 511 | Minimally invasive valve surgery | 56 | 17 | Blood transfusion | 144 | Na | 0.4 (0.2–0.8) | 0.8 (0.4–1.8) | - | - | - | ? | 100% |
| Schumacher, Schneider, Reich, et al.66 | 689 | Mistletoe in BRCA | 219 | ? | BRCA relapse | 30 | ? | 0.5 (0.2–1.3) | - | - | - | 0.3 (0.1–0.8) | ? | Na |
| Aronow, Novaro, Lauer, et al.22 | 2126 | Lipid lowering drugs after coronary intervention | 175 | 7 | Persistent use after 6mo | 628 | 7 | 3.1 (2.8–3.3) | 2.3 (2.0–2.5) | 2.8 (2.5–3.1) | 3.2 (2.9–3.4) | 3.2 (2.9–3.4) | 0.73 | 91% |
| Stenestrand , Wallentin L.173 | 6891 | Fibrinolytic therapy in acute MI | 2994 | 22 | Mortality & stroke | 2476 | 29 | 0.9 | - | 0.8 (0.8–0.9) | 0.9 (0.8–0.9) | 0.9 (0.8–0.9) | 0.66 | Na |
| Murray, Singer, Dawson, et al.170 | 11,150 | Rehabilitatio n vs no rehabilitation group | 4738 | 112 | Discharge | 4404 | 36 | 0.3 (0.3–0.4) | 1.38 (1.29–1.47) | - | - | 1.5 (1.4–1.6) | 0.82 | 59% |
| Bukhari , Wiles, Lunt, et al.29 | 335 | DMARD in RA | 82 | 10 | RA progression | Na | Na | 2.0 (1.4–2.8) | - | 1.5 (1.0–2.2) | - | - | ? | Na |
| Abramov, Tamariz, Fremes, et al.19 | 2214 | Pre OP renal function | 507 | ? | Mortality | ? | Na | ? | - | 2.0 (1.1–3.8) | 1.9 (1.3–2.8) | - | ? | Na |
| Abramov, Tamariz, Serrick, et al.20 | 1820 | Pulsatile perfusion in CABG | 905 | ? | Cardiovascular accident | ? | 4 | ? | - | - | 1.9 (1.1–3.3) | 2.2 (1.1–4.4) | ? | Na |
| Martelli, Miceli, De Palo, et al.168 | 671 | Axillary dissection in BRCA | 172 | 6 | Mortality (BRCA) | 60 | 7 | “no sign. diff.” | - | - | - | 1.0 (0.7–1.4) | 0.72 | Na |
| Chan, Bhatt, Chew, et al.32 | 1552 | Statins before PTCA | 615 | 22 | Mortality & MI | ? | 3 | 0.5 (p=0.003) | - | - | - | 0.4 (p=0.04) | 0.71 | Na |
| Hachamovitch, Hayes, Friedman, et al.43 | 10,627 | Revasc in CAD | 671 | 12 | Mortality | 146 | 12 | 2.3 (1.4–3.7) | - | - | ? | ? | 0.94 | Na |
| Landesberg, Mosseri, Wolf, et al.55 | 407 | Revasc in CAD | 74 | ? | Mortality | ? | 8 | 0.8 (0.5–1.3) | - | 0.4 (0.2–0.7) | 0.5 (0.3–0.9) | - | ? | Na |
| Magee, Coombs, Peterson, et al.58 | 204, 602 | Off vs on pump CABG | 17,969 | 19 | Mortality | ~ 5860 | 27 | 0.8 (0.7–0.9) | 0.8 (0.7–1.0) | - | 0.8 (0.7–0.8) | - | ? | 94% |
| McGuire, Anstrom, Peterson.169 | 9619 | Clinical alert | 2644 | ? | % PTCA after vs before | ? | 12 | 0.9 (p=0.06) | - | - | - | 1.2 (1.0–1.3) | ? | Na |
| Moss, Humphries, Gao, et al.60 | 1981 | Mitral valve repair vs replacement | 338 | 43 | Mortality | ? | Na | ? | 0.5 (0.3–0.8) | - | - | - | ? | 95% |
| Trichon, Glower, Shaw, et al.71 | 2757 | Surgery in mitral regurg | 278 | ? | Mortality | ~ 1400 | ? | 0.5 | ? | - | 0.6 (0.5–0.7) | - | ? | ? |
| Yu, Platt, Lanken, et al.175 | 1010 | Pulmonary artery catheter | 275 | 18 | Mortality | 404 | 3 | 1.3 (1.0–1.7) | 0.8 (0.5–1.3) | 1.0 (0.6–1.7) | - | - | 0.85 | 51% |
| Brener, Ellis, Schneider, et al.28 | 10,471 | Abciximab in PTCA | 4816 | 21 | Mortality | 1504 | 25 | 0.9 (0.8–1.0) | - | - | 1.0 (0.9–1.1) | ? | 0.83 | Na |
| Calafiore, Di Mauro, Canosa,et al.30 | 4381 | Off vs on pump CABG | ~960 | 10 | Mortality | 44 | Na | ? | 0.4 (0.2–0.8) | - | - | - | ? | ? |
| Karthik, Musleh, Grayson, et al.50 | 828 | Off vs on pump CABG | 411 | 20 | Mortality | 31 | Na | 0.9 (0.5–1.9) | - | 0.8 (0.4–1.9) | - | - | 0.8 | Na |
| MacDonald, Morant, Goldstein , Burke, et al.167 | ~1,380, 000 | Coxib vs NSAID | ~ 1600 | 18 | GI bleeding | 8526 | 18 | 0.6 (0.2–1.5) | - | 0.4 (0.2–1.1) | 0.4 (0.1–1.0) | 0.4 (0.1–1.0) | ? | Na |
| Dendukuri, Normand, McNeil.36 | 37,788 | Angiography in acute MI | 9849 | 16 | Mortality | ? | Na | “no sign. diff.” | “no sign. diff.” | - | - | - | ? | 61% |
| O'Neill, Iturria, Link, et al.171 | 97 | Surgery for brain Meta | 23 | 25(sic!) | Mortality | 80 | 3 | “no sign. diff.” | - | - | 1.2 (0.7–2.0) | 1.0 (0.5–1.8) | 0.89 | Na |
| Chan, Moliterno, Berger,et al.33 | 4809 | Clopidogrel in PTCA | 332 | 8 | Mortality | 88 | >10 | 0.5 (0.3–0.9) | - | - | - | 0.5 (0.3–1.0) | 0.64 | Na |
| Johnson,Jin, Quan,et al.166 | 11,854 | Treatment in CHF | 546 | ? | Mortality | 2681 | 18 | ? | - | “analogous” | 0.5 (0.4–0.7) | - | ? | Na |
| Peterson, Pollack, Roe ,et al.62 | 60,770 | Glycoprotein inhib in acute MI | 15,379 | 23 | Mortality | ~ 4860 | ? | 0.3 (0.3–0.4) | 0.9 (0.8–1.0) | - | 0.6 (0.6–0.7) | 0.9 (0.8–1.0) | 0.78 | 92% |
| Young-Xu, Chan, Liao, et al.75 | 371 | Satin use | 140 | 24 | Well being (depression) | ? | 25 | 0.7 (0.5–0.9) | - | - | 0.6 (0.4–0.9) | 0.6 (0.4–0.9) | 0.86 | Na |
| Beddhu, Samore, Roberts,et al. 25 | 2920 | Timing of dialysis | 1444 | 11 | Mortality | 1070 | 21 | ? | - | 1.5 (1.3–1.6) | 1.4 (1.3–1.4) | 1.1 (1.1–1.2) | ? | Na |
| Reddan, Szczech, Tuttle,et al.172 | 4584 | Revasc in CAD | 1380 | ? | Mortality | ? | 14 | ? | - | - | - | 0.4 (0.3–0.5) | ? | Na |
| Winkelmayer,Ow en, Levin, et al.74 | 3014 | Late referral in ESRF | 1039 | 48 | Mortality | 1429 | ? | ? | 1.4 (1.2–1.6) | - | 1.4 (1.2–1.5) | 1.3 (1.2–1.5) | 0.68 | 100% |
| Ezri, Weisenberg, Khazin, et al.37 | 644 | CABG | 200 | ? | Difficult laryngoscopy | 43 | ? | 2.0 (p=0.02) | - | - | - | “no sign. assoc.” | ? | Na |
| Krzyzanowska, Weeks, Earle.53 | 1696 | Treatment in pancreatic CA | 746 | 5(?) | Mortality | >> 50% | 3 | ? | - | 0.5 | 0.5 (0.5–0.6) | - | ? | Na |
| Hall, Summers, Obenchain.44 | 11,443 | Insulin (Lispro vs regular) | 3341 | 25 | Health care utilization (hosp) | 678 | Na | ? | 0.7 (0.6–0.8) | - | - | - | ? | 55% |
| Abbott, Trespalacios, Agodoa.18 | 993 | AV-fistula in dialysis | 257 | 12 | CHF | 462 | ? | ? | - | - | “almost same” | 0.9 (0.6–1.1) | 0.70 | Na |
| Banbury, White, Blackstone, et al.24 | 357 | Vacuum assisted venous return | 150 | 6 | Blood usage | 94 | 4 | 0.4 (0.2–0.6) | - | - | 0.3 (0.2–0.6) | 0.2 (0.1–0.5) | 0.79 | Na |
| Flameng, Herijgers, Dewilde, et al.38 | 1098 | Cardioplegy in cardiac surgery | 504 | 36 | Mortality | 74 | 6 | 0.6 (0.4–1.0) | - | - | 0.4 (0.2–0.8) | 0.4 (0.2–0.9) | ? | Na |
| Gillinov, Faber, Houghtaling, et al.40 | 679 | Mitral valve repair | 232 | 8 | Mortality | 30 | Na | 0.6 (0.3–1.2) | - | - | - | 1.0 (0.4–2.4) | 0.86 | Na |
| Gillinov, Blackstone, Cosgrove,et al.163 | 813 | Mitral valve repair vs double replacement | 295 | 13 | Mortality | 52 | 11 | 0.8 (.4–1.4) | - | - | - | - | .81 | Na |
| Koch, Khandwala, Nussmeier, et al.52 | 15,597 | Female gender in CABG | 3596 | 68 | Mortality | 257 | 9 | 1.7 (1.3–2.2) | 0.9 (0.5–1.7) | - | 1.3 (1.0–1.8) | “not sign.” | ? | 26% |
| Murthy, Law, Whooley,et al.61 | 921 | Atrial fib after esophagecto my | 198 | 4 | Mortality | 42 | Na | - | 4.5 (2.0–9.7) | - | - | - | 0.7 | 73% |
| Rice, Adelstein, Chidel, et al.63 | 83 | Chemo in esophageal CA | 31 | 15 | Mortality | ~54 | Na | 0.7 | 0 (no treated cases) | - | - | - | ? | 65% |
| Schmitz, Weinreich, White, et al.65 | 582 | Intra-aortic filtration in CABG | 278 | 9 | Stroke | 46 | 6 | 0.4 | “no diff.” | - | “no diff.” | 0.4 (0.2–0.8) | 0.64 | 81% |
| Girou, Brun-Buisson, Taille, et al.41 | 479 | Non-invasive ventilation | 166 | 6 | Mortality | 53 | 4 | 0.5 (0.3–0.9) | - | - | 0.4 (0.2–0.8) | 0.4 (0.2–0.8) | ? | Na |
| Gregg, Cauley, Stone,et al.164 | 3009 | Start of physical activity | 811 | ? | Mortality | ~400 | 11 | ? | - | “similar” | 0.5 (0.4–0.7) | - | ? | Na |
| Grzybowski, Clements, Parsons, et al.42 | 19,917 | Revasc in acute MI | 4705 | 23 | Mortality | 5173 | Na | 0.3 (0.3–0.3) | 0.5 (0.4–0.6) | - | - | - | 0.80 | 83% |
| Vikram, Buenconsejo, Hasbun, et al.73 | 513 | Valve surgery | 230 | 12 | Mortality | 131 | 7 | 0.4 (0.3–0.6) | 0.5 (0.2–0.9) | 0.5 (0.2–0.9) | 0.4 (0.2–0.5) | - | 0.86 | 47% |
| Macaubas, de Klerk , Holt.57 | 407 | Antenatal cytokines | 110 | ? | Asthma | 138 | Na | 0.7 (0.5–1.2) | - | 0.6 (0.4–1.0) | - | - | ? | Na |
| Frolkis, Pothier, Blackstone, et al.39 | 29,244 | Ventricular ectopy | 1080 | 30 | Mortality | 1862 | 30 | 2.4 (2.0–2.9) | 1.5 (1.1–1.9) | - | 1.6 (1.3–1.9) | - | 0.80 | 99% |
| Katzan, Cebul, Husak, et al.51 | 11,286 | Pneumonia in stroke | 635 | 38 | Mortality | 644 | 20 | 6.1 | - | - | 4.4 (3.7–5.2) | 3.0 (2.4–3.7) | 0.83 | Na |
| Christakis, Iwashyna. 35 | 195,553 | Hospice use in widowers | 30, 916 | 28 | Mortality | 4191 | Na | ? | 0.9 (0.8–1.0) | - | - | - | ? | 100% |
| Heuschmann, Berger, Misselwitz, et al.47 | 13,440 | Thrombolysis in stroke | 384 | 14 | Mortality | 486 | Na | 2.8 (2.0–3.9) | 1.7 (1.0–2.8) | - | - | - | 0.94 | 98% |
| Hughes, Evans, Lightfoot, et al.48 | 1228 | Transfusion in infection | 587 | 7 | Mortality | 218 | 12 | 3.6 (2.6–5.0) | - | - | - | 0.9 (0.5–1.5) | ? | Na |
From PubMed search and Science Citation Index.
Numbers presented are odds ratios, relative risks, or incidence rate ratios with their corresponding 95% confidence intervals (in brackets)
Area under the receiver operating characteristics (ROC) curve (c-statistic) from logistic regression model used to estimate the PS
Percent of all exposed subjects for whom an unexposed subject could be matched on the PS; exposed subjects without match are discarded from analysis; Na = not applicable (no matching)
qualitative statement; data not presented
The number of exposed subjects (or unexposed subjects, if this number was smaller) ranged from 61 to over 1,380,000, and the number of outcomes ranged from 23 to 285,965. In 109 studies, the number of exposed subjects was larger than the number of subjects who experienced the outcome; in 13 studies it was smaller. To estimate the PS, 2 to 112 variables were used (in those papers in which this information was presented), compared with 1 to 45 used in multivariable outcome models. Direct comparison of the number of variables was possible in 90 studies, of which only 51 used more variables to estimate the PS than to estimate the corresponding outcome model; 27 used fewer variables to do so. Sixty-five studies had fewer than 8 outcomes for each variable entered into the PS model, i.e. a setting where the use of PS methods was shown to be advantageous compared with conventional outcome modeling.[210] In 60% of studies (96 out of 161) the number of outcomes would have been sufficient to enter all variables used in the propensity score model in the corresponding outcome model.
The area under the receiver operating characteristic (ROC) curve or c-statistic was presented for 73 studies. It ranged from 0.56 to 0.93, indicating poor to good predictive power. The lowest predictive value (c=0.56) was achieved predicting the annual volume of patients treated by admitting physicians (in a study assessing its association with mortality in acute myocardial infarction);[199] the highest (c=0.94) was achieved when predicting revascularization in coronary artery disease [43] and thrombolysis in patients with stroke [47]. Very high values (c > 0.90) were reported in six additional studies for treatments including statins [68], amiodarone after acute myocardial infarction [87], chemotherapy in colon cancer [85], heart valve repair vs. replacement [122], bilateral thoracic artery bypass [148], and a hospital comparison [90].
Fifty-one studies used matching on the PS as either the main analytic strategy or as one of several analytic strategies presented. The percentage of exposed participants that could be matched to an unexposed participant was presented for 49 studies, and ranged from 26% to 100% (median=90%).
Most studies showed clear evidence of confounding, with substantial changes in the point estimate after adjustment. Whether PS methods or conventional outcome models were used to control for confounding, however, seemed to matter little in most of those 69 studies in which such a comparison was possible. These included 10 studies in which the authors made a qualitative statement that (mostly PS) analyses showed “similar” results.
In 20% of studies (14 out of 69), however, there was a more than 20% difference in the point estimate obtained from the conventional outcome model compared with any propensity score method presented.[22, 24, 34, 51, 52, 62, 73, 100, 102, 105, 107, 121, 123, 192] We used this arbitrary cut-point as a marker of a substantial difference in results. Of these, 5 [22, 100, 107, 121, 123] showed results not meeting our 20% criterion for at least one of the analytic strategies using PS. In four of these studies, the PS strategy not meeting criterion was when the PS was added to the conventional multivariable outcome model [22, 100, 107, 123]. In the study by Foody et al. [121], the result matched on the PS did not meet our criterion. This left the remaining 13% of studies (9 out of 69) in which all PS analyses presented showed a substantial difference compared with conventional outcome models.
Discussion
The number of studies using PS methods, though not yet large, is climbing rapidly.[211] According to the authors of many of these studies, the main reason to use PS methods was better control for confounding compared with conventional multivariable outcome modeling. We found no empirical evidence, however, that PS analyses controlled confounding more effectively than conventional outcome modeling in the majority of the studies where results from both methods were presented. Potentially meaningful differences in the control of confounding were observed in less than 15% of studies. Since the true underlying association is unknown, it remains unclear whether these differences are due to better control for confounding using the PS or whether adjusting for an inaccurate PS distorted results in some studies.[212,213] The use of PS as the only analytic technique applied comes at the price of losing potentially useful information about predictors of outcome. It therefore seems desirable to use PS only if a reduction in bias or an improvement in efficiency can be achieved.
Cook and Goldman compared the performance of tests of significance under the null hypothesis (i.e. assuming no difference between treatments) for PS and for ‘traditional’ multivariable outcome models using simulations.[214] PS appeared to produce valid results in most circumstances, but were biased in situations with very strong treatment-confounder associations.
In some practical situations the choice of analytic method will be limited. Because 10 events per covariate is usually considered to be a minimum requirement for stable estimates in multivariable models,[215,216] PS analyses combining multiple covariates into a single score are especially desirable if the treatment is common and the outcome is rare.[217,218] A recent simulation study comparing PS with multivariable outcome models concluded that PS performed better in situations with less than 8 outcomes per covariate.[210] Apart from this specific condition (relevant in 65 of the 161 studies presenting the necessary information), there is little if any practical guidance for researchers regarding when the use of PS will produce different, and in particular, better estimates compared with conventional multivariable outcome models.
PS are used to reduce bias. Drake observed that the magnitude and direction of bias resulting from omitting an important confounder from analysis was similar in multivariable outcome modeling and in estimating the treatment-outcome relation controlling for PS.[219] This observation implies that PS may not be superior to conventional multivariable outcome models in controlling bias from unobserved confounders.
Several strategies for using PS are currently being applied in medical research, and often the results from more than one of these strategies are reported in a single paper. Individual matching on a PS has intuitive appeal and in those studies that used matching, the proportion of exposed subjects that could be matched ranged from 26% to 100%. Excluding a large proportion of exposed subjects because of a lack of unexposed matches, however, may severely alter the composition of the study population. Because comparisons may be valid within that altered population, we would therefore not call this issue a bias. Nevertheless, it is essential to appreciate and to describe clearly the differences between this altered population and the original study population. On the other hand, including subjects with a PS outside the overlapping range, such as using conventional outcome modeling or PS methods including non-overlapping ranges, can lead to bias due to model extrapolation or smoothing. Such subjects might include, for example, patients with absolute indications or contraindications to treatment, who should not be included in any treatment comparison,[220] but are usually not recognized using conventional multivariable outcome modeling. Since this is a clear advantage of PS, a graphical exploration similar to figure 1 could be used as a routine procedure before doing any multivariable outcome modeling in treatment comparisons. Unfortunately, systematic comparisons of the different strategies to apply PS with respect to validity and efficiency with specific attention to exclusion of participants and non-linear associations between the PS and the outcome are sparse.[221]
Variable selection in constructing PS is at present an ad hoc process that lacks guidelines and well-understood model diagnostics. The area under the ROC curve or c-statistic (from logistic regression) to quantify the predictive power of a model is a well established concept in clinical epidemiology.[222] Its value when assessing the performance of PS to control confounding is unclear, however. Indeed, a very high c-statistic can indicate considerable non-overlap in PS distributions between exposed and unexposed as shown in figure 1.
Some authors argue that variables that only predict treatment choice but are not associated with the study outcome should not be included in the PS.[223] By definition, these are not confounders, but they may increase the area under the ROC curve and thereby erroneously imply a high validity of the PS analysis.
A practical way of assessing the value of the PS model in controlling for confounding is to check the balance of important risk factors for the outcome between exposed and unexposed within levels of the estimated PS. This method has the advantage of being driven by substantive knowledge rather than statistics, and the results can easily be communicated to the reader in a table. It allows direct assessment of comparability of exposed and unexposed by the reader, a clear advantage of using PS methods compared with the ‘black box’ of the conventional outcome model.
This review of the application of propensity score methods in the medical literature has several limitations. We may well have missed some studies by using a specific search strategy, but this problem should not affect the comparison over time. Important information in understanding similarities and differences between the analytic approaches, including description of the types of variables, variable selection procedures, and measures of model adequacy, could not be abstracted systematically, since these are rarely presented with sufficient detail in published papers.
In conclusion, methods using propensity scores may be good candidates for improving inference in non-experimental studies, but a better understanding of the benefits and limitations of these methods in practical circumstances is needed. Meanwhile, propensity scores, like any other method, should not be automatically regarded as a preferable and sole method to control for confounding in non-experimental research, but rather as a promising addition.
Acknowledgments
The project was funded by a grant from the National Institute on Aging (RO1 AG023178)
References
- 1.Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med. 2000;342:1887–1892. doi: 10.1056/NEJM200006223422507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Writing group for the Women’s Health Initiative investigators. Risk and benefits of estrogen plus progestin in healthy postmenopausal women. Principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321–333. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 3.Walker AM. Confounding by indication. Epidemiology. 1996;7:335–336. [PubMed] [Google Scholar]
- 4.Miettinen OS. Stratification by a multivariate confounder score. Am J Epidemiol. 1976;104:609–620. doi: 10.1093/oxfordjournals.aje.a112339. [DOI] [PubMed] [Google Scholar]
- 5.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 6.Rosenbaum PR, Rubin DB. The bias due to incomplete matching. Biometrics. 1985;41:103–116. [PubMed] [Google Scholar]
- 7.Gu XS, Rosenbaum PR. Comparison of multivariate matching methods: structures, distances, and algorithms. J Comput Graph Stat. 1993;2:405–420. [Google Scholar]
- 8.Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. 2001. http://www2.sas.com/proceedings/sugi26/p214-26.pdf Accessed Jan, 2005.
- 9.Rubin DB, Thomas N. Matching using estimated propensity scores: relating theory to practice. Biometrics. 1996;52:249–264. [PubMed] [Google Scholar]
- 10.Cochran WG. The effectiveness of adjustment by subclassification in removing bias in observational studies. Biometrics. 1968;24:205–213. [PubMed] [Google Scholar]
- 11.Brenner H, Blettner M. Controlling for continuous confounders in epidemiologic research. Epidemiology. 1997;8:429–434. [PubMed] [Google Scholar]
- 12.Rubin DB, Thomas N. Combining propensity score matching with additional adjustment for prognostic covariates. J Am Stat Assoc. 2000;95:573–585. [Google Scholar]
- 13.D’Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 14.Brookhart MA, van der Laan MJ. A semiparametric model selection criterion with applications to the marginal structural model. Comput Stat Data Anal (in press). [DOI] [PMC free article] [PubMed]
- 15.Joffe MM, Rosenbaum PR. Invited commentary: propensity scores. Am J Epidemiol. 1999;150:327–333. doi: 10.1093/oxfordjournals.aje.a010011. [DOI] [PubMed] [Google Scholar]
- 16.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using sub-clasification on the propensity score. J Am Stat Assoc. 1984;79:516–524. [Google Scholar]
- 17.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 18.Abbott KC, Trespalacios FC, Agodoa LY. Arteriovenous fistula use and heart disease in long-term elderly hemodialysis patients: analysis of United States Renal Data System Dialysis Morbidity and Mortality Wave II. J Nephrol. 2003;16:822–830. [PubMed] [Google Scholar]
- 19.Abramov D, Tamariz M, Fremes S, et al. Impact of preoperative renal dysfunction on cardiac surgery results. Asian Cardiovasc Thorac Ann. 2003;11:42–47. doi: 10.1177/021849230301100111. [DOI] [PubMed] [Google Scholar]
- 20.Abramov D, Tamariz M, Serrick CI, et al. The influence of cardiopulmonary bypass flow characteristics on the clinical outcome of 1820 coronary bypass patients. Can J Cardiol. 2003;19:237–243. [PubMed] [Google Scholar]
- 21.Allen-Ramey FC, Duong PT, Goodman DC, et al. Treatment effectiveness of inhaled corticosteroids and leukotriene modifiers for patients with asthma: an analysis from managed care data. Allergy Asthma Proc. 2003;24:43–51. [PubMed] [Google Scholar]
- 22.Aronow HD, Novaro GM, Lauer MS, et al. In-hospital initiation of lipid-lowering therapy after coronary intervention as a predictor of long-term utilization: a propensity analysis. Arch Intern Med. 2003;163:2576–2582. doi: 10.1001/archinte.163.21.2576. [DOI] [PubMed] [Google Scholar]
- 23.Ascione R, Narayan P, Rogers CA, Lim KH, Capoun R, Angelini GD. Early and midterm clinical outcome in patients with severe left ventricular dysfunction undergoing coronary artery surgery. Ann Thorac Surg. 2003;76:793–799. doi: 10.1016/s0003-4975(03)00664-7. [DOI] [PubMed] [Google Scholar]
- 24.Banbury MK, White JA, Blackstone EH, Cosgrove DM., 3rd Vacuum-assisted venous return reduces blood usage. J Thorac Cardiovasc Surg. 2003;126:680–687. doi: 10.1016/s0022-5223(03)00048-5. [DOI] [PubMed] [Google Scholar]
- 25.Beddhu S, Samore MH, Roberts MS, et al. Impact of timing of initiation of dialysis on mortality. J Am Soc Nephrol. 2003;14:2305–2312. doi: 10.1097/01.asn.0000080184.67406.11. [DOI] [PubMed] [Google Scholar]
- 26.Bhatt DL, Chew DP, Lincoff AM, et al. Effect of revascularization on mortality associated with an elevated white blood cell count in acute coronary syndromes. Am J Cardiol. 2003;92:136–140. doi: 10.1016/s0002-9149(03)00527-7. [DOI] [PubMed] [Google Scholar]
- 27.Boening A, Friedrich C, Hedderich J, Schoettler J, Fraund S, Cremer JT. Early and medium-term results after on-pump and off-pump coronary artery surgery: a propensity score analysis. Ann Thorac Surg. 2003;76:2000–2006. doi: 10.1016/s0003-4975(03)01298-0. [DOI] [PubMed] [Google Scholar]
- 28.Brener SJ, Ellis SG, Schneider J, Apperson-Hansen C, Topol EJ. Abciximab-facilitated percutaneous coronary intervention and long-term survival--a prospective single-center registry. Eur Heart J. 2003;24:630–638. doi: 10.1016/s0195-668x(02)00812-6. [DOI] [PubMed] [Google Scholar]
- 29.Bukhari MA, Wiles NJ, Lunt M, et al. Influence of disease-modifying therapy on radiographic outcome in inflammatory polyarthritis at five years: results from a large observational inception study. Arthritis Rheum. 2003;48:46–53. doi: 10.1002/art.10727. [DOI] [PubMed] [Google Scholar]
- 30.Calafiore AM, Di Mauro M, Canosa C, et al. Myocardial revascularization with and without cardiopulmonary bypass in multivessel disease: impact of strategy on midterm outcome. Ann Thorac Surg. 2003;76:32–36. doi: 10.1016/s0003-4975(03)00316-3. [DOI] [PubMed] [Google Scholar]
- 31.Calafiore AM, Di Mauro M, Canosa C, Di Giammarco G, Iaco AL, Contini M. Early and late outcome of myocardial revascularization with and without cardiopulmonary bypass in high risk patients (EuroSCORE > or = 6) Eur J Cardiothorac Surg. 2003;23:360–367. doi: 10.1016/s1010-7940(02)00800-x. [DOI] [PubMed] [Google Scholar]
- 32.Chan AW, Bhatt DL, Chew DP, et al. Relation of inflammation and benefit of statins after percutaneous coronary interventions. Circulation. 2003;107:1750–1756. doi: 10.1161/01.CIR.0000060541.18923.E9. [DOI] [PubMed] [Google Scholar]
- 33.Chan AW, Moliterno DJ, Berger PB, et al. Triple antiplatelet therapy during percutaneous coronary intervention is associated with improved outcomes including one-year survival: results from the Do Tirofiban and ReoProGive Similar Efficacy Outcome Trial (TARGET) J Am Coll Cardiol. 2003;42:1188–1195. doi: 10.1016/s0735-1097(03)00944-6. [DOI] [PubMed] [Google Scholar]
- 34.Cho L, Bhatt DL, Marso SP, et al. An invasive strategy is associated with decreased mortality in patients with unstable angina and non-ST-elevation myocardial infarction: GUSTO IIb trial. Am J Med. 2003;114:106–111. doi: 10.1016/s0002-9343(02)01446-8. [DOI] [PubMed] [Google Scholar]
- 35.Christakis NA, Iwashyna TJ. The health impact of health care on families: a matched cohort study of hospice use by decedents and mortality outcomes in surviving, widowed spouses. Soc Sci Med. 2003;57:465–475. doi: 10.1016/s0277-9536(02)00370-2. [DOI] [PubMed] [Google Scholar]
- 36.Dendukuri N, Normand SL, McNeil BJ. Impact of cardiac service availability on case-selection for angiography and survival associated with angiography. Health Serv Res. 2003;38:21–40. doi: 10.1111/1475-6773.00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ezri T, Weisenberg M, Khazin V, et al. Difficult laryngoscopy: incidence and predictors in patients undergoing coronary artery bypass surgery versus general surgery patients. J Cardiothorac Vasc Anesth. 2003;17:321–324. doi: 10.1016/s1053-0770(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 38.Flameng WJ, Herijgers P, Dewilde S, Lesaffre E. Continuous retrograde blood cardioplegia is associated with lower hospital mortality after heart valve surgery. J Thorac Cardiovasc Surg. 2003;125:121–125. doi: 10.1067/mtc.2003.77. [DOI] [PubMed] [Google Scholar]
- 39.Frolkis JP, Pothier CE, Blackstone EH, Lauer MS. Frequent ventricular ectopy after exercise as a predictor of death. N Engl J Med. 2003;348:781–790. doi: 10.1056/NEJMoa022353. [DOI] [PubMed] [Google Scholar]
- 40.Gillinov AM, Faber C, Houghtaling PL, et al. Repair versus replacement for degenerative mitral valve disease with coexisting ischemic heart disease. J Thorac Cardiovasc Surg. 2003;125:1350–1362. doi: 10.1016/s0022-5223(02)73274-1. [DOI] [PubMed] [Google Scholar]
- 41.Girou E, Brun-Buisson C, Taille S, Lemaire F, Brochard L. Secular trends in nosocomial infections and mortality associated with noninvasive ventilation in patients with exacerbation of COPD and pulmonary edema. JAMA. 2003;290:2985–2991. doi: 10.1001/jama.290.22.2985. [DOI] [PubMed] [Google Scholar]
- 42.Grzybowski M, Clements EA, Parsons L, et al. Mortality benefit of immediate revascularization of acute ST-segment elevation myocardial infarction in patients with contraindications to thrombolytic therapy: a propensity analysis. JAMA. 2003;290:1891–1898. doi: 10.1001/jama.290.14.1891. [DOI] [PubMed] [Google Scholar]
- 43.Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900–2907. doi: 10.1161/01.CIR.0000072790.23090.41. [DOI] [PubMed] [Google Scholar]
- 44.Hall JA, Summers KH, Obenchain RL. Cost and utilization comparisons among propensity score-matched insulin lispro and regular insulin users. J Manag Care Pharm. 2003;9:263–268. doi: 10.18553/jmcp.2003.9.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hamamoto M, Bando K, Kobayashi J, et al. Durability and outcome of aortic valve replacement with mitral valve repair versus double valve replacement. Ann Thorac Surg. 2003;75:28–33. doi: 10.1016/s0003-4975(02)04405-3. [DOI] [PubMed] [Google Scholar]
- 46.Harbarth S, Garbino J, Pugin J, Romand JA, Lew D, Pittet D. Inappropriate initial antimicrobial therapy and its effect on survival in a clinical trial of immunomodulating therapy for severe sepsis. Am J Med. 2003;115:529–535. doi: 10.1016/j.amjmed.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 47.Heuschmann PU, Berger K, Misselwitz B, et al. Frequency of thrombolytic therapy in patients with acute ischemic stroke and the risk of in-hospital mortality: the German Stroke Registers Study Group. Stroke. 2003;34:1106–1113. doi: 10.1161/01.STR.0000065198.80347.C5. [DOI] [PubMed] [Google Scholar]
- 48.Hughes MG, Evans HL, Lightfoot L, et al. Does prior transfusion worsen outcomes from infection in surgical patients? Surg Infect (Larchmt) 2003;4:335–343. doi: 10.1089/109629603322761391. [DOI] [PubMed] [Google Scholar]
- 49.Ishani A, Ibrahim HN, Gilbertson D, Collins AJ. The impact of residual renal function on graft and patient survival rates in recipients of preemptive renal transplants. Am J Kidney Dis. 2003;42:1275–1282. doi: 10.1053/j.ajkd.2003.08.030. [DOI] [PubMed] [Google Scholar]
- 50.Karthik S, Musleh G, Grayson AD, et al. Effect of avoiding cardiopulmonary bypass in non-elective coronary artery bypass surgery: a propensity score analysis. Eur J Cardiothorac Surg. 2003;24:66–71. doi: 10.1016/s1010-7940(03)00255-0. [DOI] [PubMed] [Google Scholar]
- 51.Katzan IL, Cebul RD, Husak SH, Dawson NV, Baker DW. The effect of pneumonia on mortality among patients hospitalized for acute stroke. Neurology. 2003;60:620–625. doi: 10.1212/01.wnl.0000046586.38284.60. [DOI] [PubMed] [Google Scholar]
- 52.Koch CG, Khandwala F, Nussmeier N, Blackstone EH. Gender and outcomes after coronary artery bypass grafting: a propensity-matched comparison. J Thorac Cardiovasc Surg. 2003;126:2032–2043. doi: 10.1016/s0022-5223(03)00950-4. [DOI] [PubMed] [Google Scholar]
- 53.Krzyzanowska MK, Weeks JC, Earle CC. Treatment of locally advanced pancreatic cancer in the real world: population-based practices and effectiveness. J Clin Oncol. 2003;21:3409–3414. doi: 10.1200/JCO.2003.03.007. [DOI] [PubMed] [Google Scholar]
- 54.Kurlansky PA, Williams DB, Traad EA, et al. Arterial grafting results in reduced operative mortality and enhanced long-term quality of life in octogenarians. Ann Thorac Surg. 2003;76:418–426. doi: 10.1016/s0003-4975(03)00551-4. [DOI] [PubMed] [Google Scholar]
- 55.Landesberg G, Mosseri M, Wolf YG, et al. Preoperative thallium scanning, selective coronary revascularization, and long-term survival after major vascular surgery. Circulation. 2003;108:177–183. doi: 10.1161/01.CIR.0000080292.11186.FB. [DOI] [PubMed] [Google Scholar]
- 56.Leon AC, Solomon DA, Mueller TI, et al. A 20-year longitudinal observational study of somatic antidepressant treatment effectiveness. Am J Psychiatry. 2003;160:727–733. doi: 10.1176/appi.ajp.160.4.727. [DOI] [PubMed] [Google Scholar]
- 57.Macaubas C, de Klerk NH, Holt BJ, et al. Association between antenatal cytokine production and the development of atopy and asthma at age 6 years. Lancet. 2003;362:1192–1197. doi: 10.1016/s0140-6736(03)14542-4. [DOI] [PubMed] [Google Scholar]
- 58.Magee MJ, Coombs LP, Peterson ED, Mack MJ. Patient selection and current practice strategy for off-pump coronary artery bypass surgery. Circulation. 2003;108S1:II9–14. doi: 10.1161/01.cir.0000089187.51855.77. [DOI] [PubMed] [Google Scholar]
- 59.Martin S, Kolb H, Beuth J, van Leendert R, Schneider B, Scherbaum WA. Change in patients’ body weight after 12 months of treatment with glimepiride or glibenclamide in Type 2 diabetes: a multicentre retrospective cohort study. Diabetologia. 2003;46:1611–1617. doi: 10.1007/s00125-003-1238-x. [DOI] [PubMed] [Google Scholar]
- 60.Moss RR, Humphries KH, Gao M, et al. Outcome of mitral valve repair or replacement: a comparison by propensity score analysis. Circulation. 2003;108S1:II90–97. doi: 10.1161/01.cir.0000089182.44963.bb. [DOI] [PubMed] [Google Scholar]
- 61.Murthy SC, Law S, Whooley BP, Alexandrou A, Chu KM, Wong J. Atrial fibrillation after esophagectomy is a marker for postoperative morbidity and mortality. J Thorac Cardiovasc Surg. 2003;126:1162–1167. doi: 10.1016/s0022-5223(03)00974-7. [DOI] [PubMed] [Google Scholar]
- 62.Peterson ED, Pollack CV, Jr, Roe MT, et al. Early use of glycoprotein IIb/IIIa inhibitors in non-ST-elevation acute myocardial infarction: observations from the National Registry of Myocardial Infarction 4. J Am Coll Cardiol. 2003;42:45–53. doi: 10.1016/s0735-1097(03)00514-x. [DOI] [PubMed] [Google Scholar]
- 63.Rice TW, Adelstein DJ, Chidel MA, et al. Benefit of postoperative adjuvant chemoradiotherapy in locoregionally advanced esophageal carcinoma. J Thorac Cardiovasc Surg. 2003;126:1590–1596. doi: 10.1016/s0022-5223(03)01025-0. [DOI] [PubMed] [Google Scholar]
- 64.Rubins HB, Nelson DB, Noorbaloochi S, Nugent S. Effectiveness of lipid-lowering medications in outpatients with coronary heart disease in the Department of Veterans Affairs System. Am J Cardiol. 2003;92:1177–1182. doi: 10.1016/j.amjcard.2003.07.026. [DOI] [PubMed] [Google Scholar]
- 65.Schmitz C, Weinreich S, White J, et al. Can particulate extraction from the ascending aorta reduce neurologic injury in cardiac surgery? J Thorac Cardiovasc Surg. 2003;126:1829–1838. doi: 10.1016/s0022-5223(03)01285-6. [DOI] [PubMed] [Google Scholar]
- 66.Schumacher K, Schneider B, Reich G, et al. Influence of postoperative complementary treatment with lectin-standardized mistletoe extract on breast cancer patients. A controlled epidemiological multicentric retrolective cohort study. Anticancer Res. 2003;23:5081–5087. [PubMed] [Google Scholar]
- 67.Schwarz RE, Smith DD, Keny H, et al. Impact of intraoperative radiation on postoperative and disease-specific outcome after pancreatoduodenectomy for adenocarcinoma: a propensity score analysis. Am J Clin Oncol. 2003;26:16–21. doi: 10.1097/00000421-200302000-00004. [DOI] [PubMed] [Google Scholar]
- 68.Seeger JD, Walker AM, Williams PL, Saperia GM, Sacks FM. A propensity score-matched cohort study of the effect of statins, mainly fluvastatin, on the occurrence of acute myocardial infarction. Am J Cardiol. 2003;92:1447–1451. doi: 10.1016/j.amjcard.2003.08.057. [DOI] [PubMed] [Google Scholar]
- 69.Srinivasan AK, Grayson AD, Pullan DM, Fabri BM, Dihmis WC. Effect of preoperative aspirin use in off-pump coronary artery bypass operations. Ann Thorac Surg. 2003;76:41–45. doi: 10.1016/s0003-4975(03)00182-6. [DOI] [PubMed] [Google Scholar]
- 70.Stamou SC, Kapetanakis EI, Lowery R, Jablonski KA, Frankel TL, Corso PJ. Allogeneic blood transfusion requirements after minimally invasive versus conventional aortic valve replacement: a risk-adjusted analysis. Ann Thorac Surg. 2003;76:1101–1106. doi: 10.1016/s0003-4975(03)00885-3. [DOI] [PubMed] [Google Scholar]
- 71.Trichon BH, Glower DD, Shaw LK, et al. Survival after coronary revascularization, with and without mitral valve surgery, in patients with ischemic mitral regurgitation. Circulation 2003; 108S1:II103–110. [DOI] [PubMed] [Google Scholar]
- 72.Vakili BA, Kaplan RC, Slater JN, et al. A propensity analysis of the impact of platelet glycoprotein IIb/IIIa inhibitor therapy on in-hospital outcomes after percutaneous coronary intervention. Am J Cardiol. 2003;91:946–950. doi: 10.1016/s0002-9149(03)00109-7. [DOI] [PubMed] [Google Scholar]
- 73.Vikram HR, Buenconsejo J, Hasbun R, Quagliarello VJ. Impact of valve surgery on 6-month mortality in adults with complicated, left-sided native valve endocarditis: a propensity analysis. JAMA. 2003;290:3207–3214. doi: 10.1001/jama.290.24.3207. [DOI] [PubMed] [Google Scholar]
- 74.Winkelmayer WC, Owen WF, Jr, Levin R, Avorn J. A propensity analysis of late versus early nephrologist referral and mortality on dialysis. J Am Soc Nephrol. 2003;14:486–492. doi: 10.1097/01.asn.0000046047.66958.c3. [DOI] [PubMed] [Google Scholar]
- 75.Young-Xu Y, Chan KA, Liao JK, Ravid S, Blatt CM. Long-term statin use and psychological well-being. J Am Coll Cardiol. 2003;42:690–697. doi: 10.1016/S0735-1097(03)00785-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ayanian JZ, Landrum MB, Guadagnoli E, Gaccione P. Specialty of ambulatory care physicians and mortality among elderly patients after myocardial infarction. N Engl J Med. 2002;347:1678–1686. doi: 10.1056/NEJMsa020080. [DOI] [PubMed] [Google Scholar]
- 77.Carmeli Y, Eliopoulos G, Mozaffari E, Samore M. Health and economic outcomes of vancomycin-resistant enterococci. Arch Intern Med. 2002;162:2223–2228. doi: 10.1001/archinte.162.19.2223. [DOI] [PubMed] [Google Scholar]
- 78.Chan AW, Bhatt DL, Chew DP, et al. Early and sustained survival benefit associated with statin therapy at the time of percutaneous coronary intervention. Circulation. 2002;105:691–696. doi: 10.1161/hc0602.103586. [DOI] [PubMed] [Google Scholar]
- 79.Chan AW, Quinn MJ, Bhatt DL, et al. Mortality benefit of beta-blockade after successful elective percutaneous coronary intervention. J Am Coll Cardiol. 2002;40:669–675. doi: 10.1016/s0735-1097(02)02013-2. [DOI] [PubMed] [Google Scholar]
- 80.Cole JA, Loughlin JE, Ajene AN, Rosenberg DM, Cook SE, Walker AM. The effect of zanamivir treatment on influenza complications: a retrospective cohort study. Clin Ther. 2002;24:1824–1839. doi: 10.1016/s0149-2918(02)80082-0. [DOI] [PubMed] [Google Scholar]
- 81.Elad Y, French WJ, Shavelle DM, Parsons LS, Sada MJ, Every NR. Primary angioplasty and selection bias inpatients presenting late (>12 h) after onset of chest pain and ST elevation myocardial infarction. J Am Coll Cardiol. 2002;39:826–833. doi: 10.1016/s0735-1097(01)01817-4. [DOI] [PubMed] [Google Scholar]
- 82.Ferguson TB, Jr, Coombs LP, Peterson ED. Internal thoracic artery grafting in the elderly patient undergoing coronary artery bypass grafting: room for process improvement? J Thorac Cardiovasc Surg. 2002;123:869–880. doi: 10.1067/mtc.2002.121679. [DOI] [PubMed] [Google Scholar]
- 83.Ferguson TB, Jr, Coombs LP, Peterson ED. Preoperative beta-blocker use and mortality and morbidity following CABG surgery in North America. JAMA. 2002;287:2221–2227. doi: 10.1001/jama.287.17.2221. [DOI] [PubMed] [Google Scholar]
- 84.Grunkemeier GL, Payne N, Jin R, Handy JR., Jr Propensity score analysis of stroke after off-pump coronary artery bypass grafting. Ann Thorac Surg. 2002;74:301–305. doi: 10.1016/s0003-4975(02)03783-9. [DOI] [PubMed] [Google Scholar]
- 85.Iwashyna TJ, Lamont EB. Effectiveness of adjuvant fluorouracil in clinical practice: a population-based cohort study of elderly patients with stage III colon cancer. J Clin Oncol. 2002;20:3992–3998. doi: 10.1200/JCO.2002.03.083. [DOI] [PubMed] [Google Scholar]
- 86.Jenkins NP, Keevil BG, Hutchinson IV, Brooks NH. Beta-blockers are associated with lower C-reactive protein concentrations in patients with coronary artery disease. Am J Med. 2002;112:269–274. doi: 10.1016/s0002-9343(01)01115-9. [DOI] [PubMed] [Google Scholar]
- 87.Kilborn MJ, Rathore SS, Gersh BJ, Oetgen WJ, Solomon AJ. Amiodarone and mortality among elderly patients with acute myocardial infarction with atrial fibrillation. Am Heart J. 2002;144:1095–1101. doi: 10.1067/mhj.2002.125836. [DOI] [PubMed] [Google Scholar]
- 88.Luedtke R, Weber U, Fischer I, Friese KH, Moeller H. An example on the value of non-randomisation in clinical trials in complementary medicine. Forsch Komplementarmed Klass Naturheilkd. 2002;9:105–109. doi: 10.1159/000057272. [DOI] [PubMed] [Google Scholar]
- 89.Magee MJ, Jablonski KA, Stamou SC, et al. Elimination of cardiopulmonary bypass improves early survival for multivessel coronary artery bypass patients. Ann Thorac Surg. 2002;73:1196–1202. doi: 10.1016/s0003-4975(01)03587-1. [DOI] [PubMed] [Google Scholar]
- 90.Majahalme S, Kim MH, Bruckman D, Tarkka M, Eagle KA. Atrial fibrillation after coronary surgery: comparison between different health care systems. Int J Cardiol. 2002;82:209–218. doi: 10.1016/s0167-5273(01)00622-2. [DOI] [PubMed] [Google Scholar]
- 91.Mehta RL, McDonald B, Gabbai F, et al. Nephrology consultation in acute renal failure: does timing matter? Am J Med. 2002;113:456–461. doi: 10.1016/s0002-9343(02)01230-5. [DOI] [PubMed] [Google Scholar]
- 92.Mehta RL, Pascual MT, Soroko S, Chertow GM. Diuretics, mortality, and nonrecovery of renal function in acute renal failure. JAMA. 2002;288:2547–2553. doi: 10.1001/jama.288.20.2547. [DOI] [PubMed] [Google Scholar]
- 93.Mukherjee D, Mahaffey KW, Moliterno DJ, et al. Promise of combined low-molecular-weight heparin and platelet glycoprotein IIb/IIIa inhibition: results from Platelet IIb/IIIa Antagonist for the Reduction of Acute coronary syndrome events in a Global Organization Network B (PARAGON B) Am Heart J. 2002;144:995–1002. doi: 10.1067/mhj.2002.126118. [DOI] [PubMed] [Google Scholar]
- 94.Neugut AI, Fleischauer AT, Sundararajan V, et al. Use of adjuvant chemotherapy and radiation therapy for rectal cancer among the elderly: a population-based study. J Clin Oncol. 2002;20:2643–2650. doi: 10.1200/JCO.2002.08.062. [DOI] [PubMed] [Google Scholar]
- 95.Newby LK, Kristinsson A, Bhapkar MV, et al. Early statin initiation and outcomes in patients with acute coronary syndromes. JAMA. 2002;287:3087–3095. doi: 10.1001/jama.287.23.3087. [DOI] [PubMed] [Google Scholar]
- 96.Patel U, Spitznagel E, Piccirillo J. Multivariate analyses to assess treatment effectiveness in advanced head and neck cancer. Arch Otolaryngol Head Neck Surg. 2002;128:497–503. doi: 10.1001/archotol.128.5.497. [DOI] [PubMed] [Google Scholar]
- 97.Pereira JJ, Lauer MS, Bashir M, et al. Survival after aortic valve replacement for severe aortic stenosis with low transvalvular gradients and severe left ventricular dysfunction. J Am Coll Cardiol. 2002;39:1356–1363. doi: 10.1016/s0735-1097(02)01759-x. [DOI] [PubMed] [Google Scholar]
- 98.Rahme E, Pettitt D, LeLorier J. Determinants and sequelae associated with utilization of acetaminophen versus traditional nonsteroidal antiinflammatory drugs in an elderly population. Arthritis Rheum. 2002;46:3046–3054. doi: 10.1002/art.10604. [DOI] [PubMed] [Google Scholar]
- 99.Sabik JF, Gillinov AM, Blackstone EH, et al. Does off-pump coronary surgery reduce morbidity and mortality? J Thorac Cardiovasc Surg. 2002;124:698–707. doi: 10.1067/mtc.2002.121975. [DOI] [PubMed] [Google Scholar]
- 100.Shavelle DM, Parsons L, Sada MJ, French WJ, Every NR. Is there a benefit to early angiography in patients with ST-segment depression myocardial infarction? An observational study Am Heart J. 2002;143:488–496. doi: 10.1067/mhj.2002.120970. [DOI] [PubMed] [Google Scholar]
- 101.Shireman TI, Braman KS. Impact and cost-effectiveness of respiratory syncytial virus prophylaxis for Kansas medicaid’s high-risk children. Arch Pediatr Adolesc Med. 2002;156:1251–1255. doi: 10.1001/archpedi.156.12.1251. [DOI] [PubMed] [Google Scholar]
- 102.Shishehbor MH, Baker DW, Blackstone EH, Lauer MS. Association of educational status with heart rate recovery: a population-based propensity analysis. Am J Med. 2002;113:643–649. doi: 10.1016/s0002-9343(02)01324-4. [DOI] [PubMed] [Google Scholar]
- 103.Sin DD, McAlister FA. The effects of beta-blockers on morbidity and mortality in a population-based cohort of 11,942 elderly patients with heart failure. Am J Med. 2002;113:650–656. doi: 10.1016/s0002-9343(02)01346-3. [DOI] [PubMed] [Google Scholar]
- 104.Stamou SC, Jablonski KA, Pfister AJ, et al. Stroke after conventional versus minimally invasive coronary artery bypass. Ann Thorac Surg. 2002;74:394–399. doi: 10.1016/s0003-4975(02)03636-6. [DOI] [PubMed] [Google Scholar]
- 105.Stenestrand U, Wallentin L. Early revascularisation and 1-year survival in 14-day survivors of acute myocardial infarction: a prospective cohort study. Lancet. 2002;359:1805–1811. doi: 10.1016/S0140-6736(02)08710-X. [DOI] [PubMed] [Google Scholar]
- 106.Sundararajan V, Mitra N, Jacobson JS, Grann VR, Heitjan DF, Neugut AI. Survival associated with 5-fluorouracil-based adjuvant chemotherapy among elderly patients with node-positive colon cancer. Ann Intern Med. 2002;136:349–357. doi: 10.7326/0003-4819-136-5-200203050-00007. [DOI] [PubMed] [Google Scholar]
- 107.Teufelsbauer H, Prusa AM, Wolff K, et al. Endovascular stent grafting versus open surgical operation in patients with infrarenal aortic aneurysms: a propensity score-adjusted analysis. Circulation. 2002;106:782–787. doi: 10.1161/01.cir.0000028603.73287.7d. [DOI] [PubMed] [Google Scholar]
- 108.Umana JP, Lai DT, Mitchell RS, et al. Is medical therapy still the optimal treatment strategy for patients with acute type B aortic dissections? J Thorac Cardiovasc Surg. 2002;124:896–910. doi: 10.1067/mtc.2002.123131. [DOI] [PubMed] [Google Scholar]
- 109.Umana JP, Miller DC, Mitchell RS. What is the best treatment for patients with acute type B aortic dissections--medical, surgical, or endovascular stent-grafting? Ann Thorac Surg. 2002;74:S1840–1843. doi: 10.1016/s0003-4975(02)04140-1. [DOI] [PubMed] [Google Scholar]
- 110.Vincent JL, Baron JF, Reinhart K, et al. Anemia and blood transfusion in critically ill patients. JAMA. 2002;288:1499–1507. doi: 10.1001/jama.288.12.1499. [DOI] [PubMed] [Google Scholar]
- 111.Weber U, Luedtke R, Friese KH, Fischer I, Moeller H. A non-randomised pilot study to compare complementary and conventional treatments of acute sinusitis. Forsch Komplementarmed Klass Naturheilkd. 2002;9:99–104. doi: 10.1159/000057271. [DOI] [PubMed] [Google Scholar]
- 112.Weiss JP, Saynina O, McDonald KM, McClellan MB, Hlatky MA. Effectiveness and cost-effectiveness of implantable cardioverter defibrillators in the treatment of ventricular arrhythmias among medicare beneficiaries. Am J Med. 2002;112:519–527. doi: 10.1016/s0002-9343(02)01078-1. [DOI] [PubMed] [Google Scholar]
- 113.Winkelmayer WC, Glynn RJ, Mittleman MA, Levin R, Pliskin JS, Avorn J. Comparing mortality of elderly patients on hemodialysis versus peritoneal dialysis: a propensity score approach. J Am Soc Nephrol. 2002;13:2353–2362. doi: 10.1097/01.asn.0000025785.41314.76. [DOI] [PubMed] [Google Scholar]
- 114.Aronow HD, Topol EJ, Roe MT, et al. Effect of lipid-lowering therapy on early mortality after acute coronary syndromes: an observational study. Lancet. 2001;357:1063–1068. doi: 10.1016/S0140-6736(00)04257-4. [DOI] [PubMed] [Google Scholar]
- 115.Beuth J, Ost B, Pakdaman A, et al. Impact of complementary oral enzyme application on the postoperative treatment results of breast cancer patients--results of an epidemiological multicentre retrolective cohort study. Cancer Chemother Pharmacol. 2001;47S:S45–54. doi: 10.1007/s002800170009. [DOI] [PubMed] [Google Scholar]
- 116.Carmeli Y, Castro J, Eliopoulos GM, Samore MH. Clinical isolation and resistance patterns of and superinfection with 10 nosocomial pathogens after treatment with ceftriaxone versus ampicillin-sulbactam. Antimicrob Agents Chemother. 2001;45:275–279. doi: 10.1128/AAC.45.1.275-279.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dammann O, Allred EN, Kuban KC, et al. Hypocarbia during the first 24 postnatal hours and white matter echolucencies in newborns < or = 28 weeks gestation. Pediatr Res. 2001;49:388–393. doi: 10.1203/00006450-200103000-00013. [DOI] [PubMed] [Google Scholar]
- 118.Earle CC, Tsai JS, Gelber RD, Weinstein MC, Neumann PJ, Weeks JC. Effectiveness of chemotherapy for advanced lung cancer in the elderly: instrumental variable and propensity analysis. J Clin Oncol. 2001;19:1064–1070. doi: 10.1200/JCO.2001.19.4.1064. [DOI] [PubMed] [Google Scholar]
- 119.Ellis SG, Brener SJ, Lincoff AM, et al. beta-blockers before percutaneous coronary intervention do not attenuate postprocedural creatine kinase isoenzyme rise. Circulation. 2001;104:2685–2688. doi: 10.1161/hc4701.099782. [DOI] [PubMed] [Google Scholar]
- 120.Feng D, D’Agostino RB, Silbershatz H, et al. Hemostatic state and atrial fibrillation (the Framingham Offspring Study) Am J Cardiol. 2001;87:168–171. doi: 10.1016/s0002-9149(00)01310-2. [DOI] [PubMed] [Google Scholar]
- 121.Foody JM, Cole CR, Blackstone EH, Lauer MS. A propensity analysis of cigarette smoking and mortality with consideration of the effects of alcohol. Am J Cardiol. 2001;87:706–711. doi: 10.1016/s0002-9149(00)01487-9. [DOI] [PubMed] [Google Scholar]
- 122.Gillinov AM, Wierup PN, Blackstone EH, et al. Is repair preferable to replacement for ischemic mitral regurgitation? J Thorac Cardiovasc Surg. 2001;122:1125–1141. doi: 10.1067/mtc.2001.116557. [DOI] [PubMed] [Google Scholar]
- 123.Gum PA, Thamilarasan M, Watanabe J, Blackstone EH, Lauer MS. Aspirin use and all-cause mortality among patients being evaluated for known or suspected coronary artery disease: A propensity analysis. JAMA. 2001;286:1187–1194. doi: 10.1001/jama.286.10.1187. [DOI] [PubMed] [Google Scholar]
- 124.Hayashi K, Hasegawa K, Kobayashi S. Effects of angiotensin-converting enzyme inhibitors on the treatment of anemia with erythropoietin. Kidney Int. 2001;60:1910–1916. doi: 10.1046/j.1523-1755.2001.00028.x. [DOI] [PubMed] [Google Scholar]
- 125.Ioannidis JP, Galanos O, Katritsis D, et al. Early mortality and morbidity of bilateral versus single internal thoracic artery revascularization: propensity and risk modeling. J Am Coll Cardiol. 2001;37:521–528. doi: 10.1016/s0735-1097(00)01112-8. [DOI] [PubMed] [Google Scholar]
- 126.Keating NL, Weeks JC, Landrum MB, Borbas C, Guadagnoli E. Discussion of treatment options for early-stage breast cancer: effect of provider specialty on type of surgery and satisfaction. Med Care. 2001;39:681–691. doi: 10.1097/00005650-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 127.Margolis DJ, Kantor J, Santanna J, Strom BL, Berlin JA. Effectiveness of platelet releasate for the treatment of diabetic neuropathic foot ulcers. Diabetes Care. 2001;24:483–488. doi: 10.2337/diacare.24.3.483. [DOI] [PubMed] [Google Scholar]
- 128.Mast ST, Gersing KR, Anstrom KJ, Krishnan KR, Califf RM, Jollis JG. Association between selective serotonin-reuptake inhibitor therapy and heart valve regurgitation. Am J Cardiol. 2001;87:989–993. doi: 10.1016/s0002-9149(01)01435-7. A984. [DOI] [PubMed] [Google Scholar]
- 129.Mitra N, Schnabel FR, Neugut AI, Heitjan DF. Estimating the effect of an intensive surveillance program on stage of breast carcinoma at diagnosis: a propensity score analysis. Cancer. 2001;91:1709–1715. [PubMed] [Google Scholar]
- 130.Mukamal KJ, Maclure M, Muller JE, Sherwood JB, Mittleman MA. Prior alcohol consumption and mortality following acute myocardial infarction. JAMA. 2001;285:1965–1970. doi: 10.1001/jama.285.15.1965. [DOI] [PubMed] [Google Scholar]
- 131.Normand ST, Landrum MB, Guadagnoli E, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001;54:387–398. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- 132.Osswald BR, Blackstone EH, Tochtermann U, et al. Does the completeness of revascularization affect early survival after coronary artery bypass grafting in elderly patients? Eur J Cardiothorac Surg. 2001;20:120–125. doi: 10.1016/s1010-7940(01)00743-6. [DOI] [PubMed] [Google Scholar]
- 133.Peterson JG, Topol EJ, Roe MT, et al. Prognostic importance of concomitant heparin with eptifibatide in acute coronary syndromes. PURSUIT Investigators. Platelet Glycoprotein IIb/IIIa in Unstable Angina: Receptor Suppression Using Integrilin Therapy. Am J Cardiol. 2001;87:532–536. doi: 10.1016/s0002-9149(00)01426-0. [DOI] [PubMed] [Google Scholar]
- 134.Polanczyk CA, Rohde LE, Goldman L, et al. Right heart catheterization and cardiac complications in patients undergoing noncardiac surgery: an observational study. JAMA. 2001;286:309–314. doi: 10.1001/jama.286.3.309. [DOI] [PubMed] [Google Scholar]
- 135.Rathore SS, Gersh BJ, Weinfurt KP, Oetgen WJ, Schulman KA, Solomon AJ. The role of reperfusion therapy in paced patients with acute myocardial infarction. Am Heart J. 2001;142:516–519. doi: 10.1067/mhj.2001.117602. [DOI] [PubMed] [Google Scholar]
- 136.Sernyak MJ, Desai R, Stolar M, Rosenheck R. Impact of clozapine on completed suicide. Am J Psychiatry. 2001;158:931–937. doi: 10.1176/appi.ajp.158.6.931. [DOI] [PubMed] [Google Scholar]
- 137.Sernyak MJ, Rosenheck R, Desai R, Stolar M, Ripper G. Impact of clozapine prescription on inpatient resource utilization. J Nerv Ment Dis. 2001;189:766–773. doi: 10.1097/00005053-200111000-00006. [DOI] [PubMed] [Google Scholar]
- 138.Stenestrand U, Wallentin L. Early statin treatment following acute myocardial infarction and 1-year survival. JAMA. 2001;285:430–436. doi: 10.1001/jama.285.4.430. [DOI] [PubMed] [Google Scholar]
- 139.Suero JA, Marso SP, Jones PG, et al. Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 2001;38:409–414. doi: 10.1016/s0735-1097(01)01349-3. [DOI] [PubMed] [Google Scholar]
- 140.Welch RD, Zalenski RJ, Frederick PD, et al. Prognostic value of a normal or nonspecific initial electrocardiogram in acute myocardial infarction. JAMA. 2001;286:1977–1984. doi: 10.1001/jama.286.16.1977. [DOI] [PubMed] [Google Scholar]
- 141.Wiles NJ, Lunt M, Barrett EM, et al. Reduced disability at five years with early treatment of inflammatory polyarthritis: results from a large observational cohort, using propensity models to adjust for disease severity. Arthritis Rheum. 2001;44:1033–1042. doi: 10.1002/1529-0131(200105)44:5<1033::AID-ANR182>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 142.Hagan H, Thiede H. Changes in injection risk behavior associated with participation in the Seattle needle-exchange program. J Urban Health. 2000;77:369–382. doi: 10.1007/BF02386747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Holman WL, Li Q, Kiefe CI, et al. Prophylactic value of preincision intra-aortic balloon pump: analysis of a statewide experience. J Thorac Cardiovasc Surg. 2000;120:1112–1119. doi: 10.1067/mtc.2000.110459. [DOI] [PubMed] [Google Scholar]
- 144.Murdoch SD, Cohen AT, Bellamy MC. Pulmonary artery catheterization and mortality in critically ill patients. Br J Anaesth. 2000;85:611–615. doi: 10.1093/bja/85.4.611. [DOI] [PubMed] [Google Scholar]
- 145.Potosky AL, Legler J, Albertsen PC, et al. Health outcomes after prostatectomy or radiotherapy for prostate cancer: results from the Prostate Cancer Outcomes Study. J Natl Cancer Inst. 2000;92:1582–1592. doi: 10.1093/jnci/92.19.1582. [DOI] [PubMed] [Google Scholar]
- 146.Weiss JP, Gruver C, Kaul S, Harrell FE, Jr, Sklenar J, Dent JM. Ordering an echocardiogram for evaluation of left ventricular function: level of expertise necessary for efficient use. J Am Soc Echocardiogr. 2000;13:124–130. doi: 10.1016/s0894-7317(00)90023-3. [DOI] [PubMed] [Google Scholar]
- 147.Yau TM, El-Ghoneimi YA, Armstrong S, Ivanov J, David TE. Mitral valve repair and replacement for rheumatic disease. J Thorac Cardiovasc Surg. 2000;119:53–60. doi: 10.1016/s0022-5223(00)70217-0. [DOI] [PubMed] [Google Scholar]
- 148.Lytle BW, Blackstone EH, Loop FD, et al. Two internal thoracic artery grafts are better than one. J Thorac Cardiovasc Surg. 1999;117:855–872. doi: 10.1016/S0022-5223(99)70365-X. [DOI] [PubMed] [Google Scholar]
- 149.Nakamura Y, Moss AJ, Brown MW, Kinoshita M, Kawai C. Long-term nitrate use may be deleterious in ischemic heart disease: A study using the databases from two large-scale postinfarction studies. Multicenter Myocardial Ischemia Research Group. Am Heart J. 1999;138:577–585. doi: 10.1016/s0002-8703(99)70163-8. [DOI] [PubMed] [Google Scholar]
- 150.Schofer J, Rau T, Schluter M, Mathey DG. Restenosis after stenting of matched occluded and non-occluded coronary arteries. Should there be a difference? Eur Heart J. 1999;20:1175–1181. doi: 10.1053/euhj.1998.1476. [DOI] [PubMed] [Google Scholar]
- 151.Shepardson LB, Youngner SJ, Speroff T, Rosenthal GE. Increased risk of death in patients with do-not-resuscitate orders. Med Care. 1999;37:727–737. doi: 10.1097/00005650-199908000-00003. [DOI] [PubMed] [Google Scholar]
- 152.Takizawa T, Haga M, Yagi N, et al. Pulmonary function after segmentectomy for small peripheral carcinoma of the lung. J Thorac Cardiovasc Surg. 1999;118:536–541. doi: 10.1016/S0022-5223(99)70193-5. [DOI] [PubMed] [Google Scholar]
- 153.Barker FG, 2nd, Chang SM, Gutin PH, et al. Survival and functional status after resection of recurrent glioblastoma multiforme. Neurosurgery. 1998;42:709–720. doi: 10.1097/00006123-199804000-00013. [DOI] [PubMed] [Google Scholar]
- 154.Barosi G, Ambrosetti A, Centra A, et al. Splenectomy and risk of blast transformation in myelofibrosis with myeloid metaplasia. Italian Cooperative Study Group on Myeloid with Myeloid Metaplasia. Blood. 1998;91:3630–3636. [PubMed] [Google Scholar]
- 155.Intrator O, Berg K. Benefits of home health care after inpatient rehabilitation for hip fracture: health service use by Medicare beneficiaries, 1987–1992. Arch Phys Med Rehabil. 1998;79:1195–1199. doi: 10.1016/s0003-9993(98)90261-1. [DOI] [PubMed] [Google Scholar]
- 156.Regueiro CR, Hamel MB, Davis RB, Desbiens N, Connors AF, Jr, Phillips RS. A comparison of generalist and pulmonologist care for patients hospitalized with severe chronic obstructive pulmonary disease: resource intensity, hospital costs, and survival. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Am J Med. 1998;105:366–372. doi: 10.1016/s0002-9343(98)00290-3. [DOI] [PubMed] [Google Scholar]
- 157.Smith NL, Reiber GE, Psaty BM, et al. Health outcomes associated with beta-blocker and diltiazem treatment of unstable angina. J Am Coll Cardiol. 1998;32:1305–1311. doi: 10.1016/s0735-1097(98)00408-2. [DOI] [PubMed] [Google Scholar]
- 158.Connors AF, Jr, Speroff T, Dawson NV, et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT Investigators. JAMA. 1996;276:889–897. doi: 10.1001/jama.276.11.889. [DOI] [PubMed] [Google Scholar]
- 159.Lieberman E, Lang JM, Cohen A, D’Agostino R, Jr, Datta S, Frigoletto FD., Jr Association of epidural analgesia with cesarean delivery in nulliparas. Obstet Gynecol. 1996;88:993–1000. doi: 10.1016/s0029-7844(96)00359-6. [DOI] [PubMed] [Google Scholar]
- 160.Stone RA, Obrosky DS, Singer DE, Kapoor WN, Fine MJ. Propensity score adjustment for pretreatment differences between hospitalized and ambulatory patients with community-acquired pneumonia. Pneumonia Patient Outcomes Research Team (PORT) Investigators. Med Care. 1995;33S:AS56–66. [PubMed] [Google Scholar]
- 161.Myers WO, Gersh BJ, Fisher LD, et al. Medical versus early surgical therapy in patients with triple-vessel disease and mild angina pectoris: a CASS registry study of survival. Ann Thorac Surg. 1987;44:471–486. doi: 10.1016/s0003-4975(10)62104-2. [DOI] [PubMed] [Google Scholar]
- 162.Myers WO, Gersh BJ, Fisher LD, et al. Time to first new myocardial infarction in patients with mild angina and three-vessel disease comparing medicine and early surgery: a CASS registry study of survival. Coronary Artery Surgery Study. Ann Thorac Surg. 1987;43:599–612. doi: 10.1016/s0003-4975(10)60230-5. [DOI] [PubMed] [Google Scholar]
- 163.Gillinov AM, Blackstone EH, Cosgrove DM, 3rd, et al. Mitral valve repair with aortic valve replacement is superior to double valve replacement. J Thorac Cardiovasc Surg. 2003;125:1372–1387. doi: 10.1016/s0022-5223(02)73225-x. [DOI] [PubMed] [Google Scholar]
- 164.Gregg EW, Cauley JA, Stone K, et al. Relationship of changes in physical activity and mortality among older women. JAMA. 2003;289:2379–2386. doi: 10.1001/jama.289.18.2379. [DOI] [PubMed] [Google Scholar]
- 165.Horwitz PA, Berlin JA, Sauer WH, Laskey WK, Krone RJ, Kimmel SE. Bleeding risk of platelet glycoprotein IIb/IIIa receptor antagonists in broad-based practice (results from the Society for Cardiac Angiography and Interventions Registry) Am J Cardiol. 2003;91:803–806. doi: 10.1016/s0002-9149(03)00012-2. [DOI] [PubMed] [Google Scholar]
- 166.Johnson D, Jin Y, Quan H, Cujec B. Beta-blockers and angiotensin-converting enzyme inhibitors/receptor blockers prescriptions after hospital discharge for heart failure are associated with decreased mortality in Alberta, Canada. J Am Coll Cardiol. 2003;42:1438–1445. doi: 10.1016/s0735-1097(03)01058-1. [DOI] [PubMed] [Google Scholar]
- 167.MacDonald TM, Morant SV, Goldstein JL, Burke TA, Pettitt D. Channelling bias and the incidence of gastrointestinal haemorrhage in users of meloxicam, coxibs, and older, non-specific non-steroidal antiinflammatory drugs. Gut. 2003;52:1265–1270. doi: 10.1136/gut.52.9.1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Martelli G, Miceli R, De Palo G, et al. Is axillary lymph node dissection necessary in elderly patients with breast carcinoma who have a clinically uninvolved axilla? Cancer. 2003;97:1156–1163. doi: 10.1002/cncr.11173. [DOI] [PubMed] [Google Scholar]
- 169.McGuire DK, Anstrom KJ, Peterson ED. Influence of the Angioplasty Revascularization Investigation National Heart, Lung, and Blood Institute Diabetic Clinical Alert on practice patterns: results from the National Cardiovascular Network Database. Circulation. 2003;107:1864–1870. doi: 10.1161/01.CIR.0000064901.21619.01. [DOI] [PubMed] [Google Scholar]
- 170.Murray PK, Singer M, Dawson NV, Thomas CL, Cebul RD. Outcomes of rehabilitation services for nursing home residents. Arch Phys Med Rehabil. 2003;84:1129–1136. doi: 10.1016/s0003-9993(03)00149-7. [DOI] [PubMed] [Google Scholar]
- 171.O’Neill BP, Iturria NJ, Link MJ, Pollock BE, Ballman KV, O’Fallon JR. A comparison of surgical resection and stereotactic radiosurgery in the treatment of solitary brain metastases. Int J Radiat Oncol Biol Phys. 2003;55:1169–1176. doi: 10.1016/s0360-3016(02)04379-1. [DOI] [PubMed] [Google Scholar]
- 172.Reddan DN, Szczech LA, Tuttle RH, et al. Chronic kidney disease, mortality, and treatment strategies among patients with clinically significant coronary artery disease. J Am Soc Nephrol. 2003;14:2373–2380. doi: 10.1097/01.asn.0000083900.92829.f5. [DOI] [PubMed] [Google Scholar]
- 173.Stenestrand U, Wallentin L. Fibrinolytic therapy in patients 75 years and older with ST-segment-elevation myocardial infarction: one-year follow-up of a large prospective cohort. Arch Intern Med. 2003;163:965–971. doi: 10.1001/archinte.163.8.965. [DOI] [PubMed] [Google Scholar]
- 174.Urbach DR, Bell CM, Swanstrom LL, Hansen PD. Cohort study of surgical bypass to the gallbladder or bile duct for the palliation of jaundice due to pancreatic cancer. Ann Surg. 2003;237:86–93. doi: 10.1097/00000658-200301000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Yu DT, Platt R, Lanken PN, et al. Relationship of pulmonary artery catheter use to mortality and resource utilization in patients with severe sepsis. Crit Care Med. 2003;31:2734–2741. doi: 10.1097/01.CCM.0000098028.68323.64. [DOI] [PubMed] [Google Scholar]
- 176.Ferraris VA, Ferraris SP, Joseph O, Wehner P, Mentzer RM., Jr Aspirin and postoperative bleeding after coronary artery bypass grafting. Ann Surg. 2002;235:820–827. doi: 10.1097/00000658-200206000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Goldstein CL, Racz M, Hannan EL. Impact of cardiac catheterization-percutaneous coronary intervention timing on inhospital mortality. Am Heart J. 2002;144:561–567. doi: 10.1067/mhj.2002.125322. [DOI] [PubMed] [Google Scholar]
- 178.Hu FB, Bronner L, Willett WC, et al. Fish and omega-3 fatty acid intake and risk of coronary heart disease in women. JAMA. 2002;287:1815–1821. doi: 10.1001/jama.287.14.1815. [DOI] [PubMed] [Google Scholar]
- 179.Jasmer RM, Saukkonen JJ, Blumberg HM, et al. Short-course rifampin and pyrazinamide compared with isoniazid for latent tuberculosis infection: a multicenter clinical trial. Ann Intern Med. 2002;137:640–647. doi: 10.7326/0003-4819-137-8-200210150-00007. [DOI] [PubMed] [Google Scholar]
- 180.Kimmel SE, Berlin JA, Kinman JL, et al. Parenteral ketorolac and risk of myocardial infarction. Pharmacoepidemiol Drug Saf. 2002;11:113–119. doi: 10.1002/pds.670. [DOI] [PubMed] [Google Scholar]
- 181.Mukamal KJ, Maclure M, Muller JE, Sherwood JB, Mittleman MA. Tea consumption and mortality after acute myocardial infarction. Circulation. 2002;105:2476–2481. doi: 10.1161/01.cir.0000017201.88994.f7. [DOI] [PubMed] [Google Scholar]
- 182.Patel NC, Grayson AD, Jackson M, et al. The effect off-pump coronary artery bypass surgery on in-hospital mortality and morbidity. Eur J Cardiothorac Surg. 2002;22:255–260. doi: 10.1016/s1010-7940(02)00301-9. [DOI] [PubMed] [Google Scholar]
- 183.Schneeweiss S, Walker AM, Glynn RJ, Maclure M, Dormuth C, Soumerai SB. Outcomes of reference pricing for angiotensin-converting-enzyme inhibitors. N Engl J Med. 2002;346:822–829. doi: 10.1056/NEJMsa003087. [DOI] [PubMed] [Google Scholar]
- 184.Schomig A, Mehilli J, Holle H, et al. Statin treatment following coronary artery stenting and one-year survival. J Am Coll Cardiol. 2002;40:854–861. doi: 10.1016/s0735-1097(02)02053-3. [DOI] [PubMed] [Google Scholar]
- 185.Soumerai SB, McLaughlin TJ, Ross-Degnan D, Christiansen CL, Gurwitz JH. Effectiveness of thrombolytic therapy for acute myocardial infarction in the elderly: cause for concern in the old-old. Arch Intern Med. 2002;162:561–568. doi: 10.1001/archinte.162.5.561. [DOI] [PubMed] [Google Scholar]
- 186.Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288:1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- 187.Turner BJ, Laine C, Cohen A, Hauck WW. Effect of medical, drug abuse, and mental health care on receipt of dental care by drug users. J Subst Abuse Treat. 2002;23:239–246. doi: 10.1016/s0740-5472(02)00249-0. [DOI] [PubMed] [Google Scholar]
- 188.Wright RS, Williams BA, Cramner H, et al. Elevations of cardiac troponin I are associated with increased short-term mortality in noncardiac critically ill emergency department patients. Am J Cardiol. 2002;90:634–636. doi: 10.1016/s0002-9149(02)02570-5. [DOI] [PubMed] [Google Scholar]
- 189.Ascione R, Nason G, Al-Ruzzeh S, Ko C, Ciulli F, Angelini GD. Coronary revascularization with or without cardiopulmonary bypass in patients with preoperative nondialysis-dependent renal insufficiency. Ann Thorac Surg. 2001;72:2020–2025. doi: 10.1016/s0003-4975(01)03250-7. [DOI] [PubMed] [Google Scholar]
- 190.Cen YY, Glower DD, Landolfo K, et al. Comparison of survival after mitral valve replacement with biologic and mechanical valves in 1139 patients. J Thorac Cardiovasc Surg. 2001;122:569–577. doi: 10.1067/mtc.2001.115418. [DOI] [PubMed] [Google Scholar]
- 191.Kachele H, Kordy H, Richard M Research group TR-EAT. Therapy amount and outcome of inpatient psychodynamic treatment of eating disorders in Germany: Data from a multicenter study. Psychotherapy Research. 2001;11:239–257. [Google Scholar]
- 192.Mehta RH, Bruckman D, Das S, et al. Implications of increased left ventricular mass index on in-hospital outcomes in patients undergoing aortic valve surgery. J Thorac Cardiovasc Surg. 2001;122:919–928. doi: 10.1067/mtc.2001.116558. [DOI] [PubMed] [Google Scholar]
- 193.Novaro GM, Tiong IY, Pearce GL, Lauer MS, Sprecher DL, Griffin BP. Effect of hydroxymethylglutaryl coenzyme a reductase inhibitors on the progression of calcific aortic stenosis. Circulation. 2001;104:2205–2209. doi: 10.1161/hc4301.098249. [DOI] [PubMed] [Google Scholar]
- 194.O’Day SJ, Boasberg PD, Kristedja TS, et al. High-dose tamoxifen added to concurrent biochemotherapy with decrescendo interleukin-2 in patients with metastatic melanoma. Cancer. 2001;92:609–619. doi: 10.1002/1097-0142(20010801)92:3<609::aid-cncr1361>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 195.Popiela T, Kulig J, Hanisch J, Bock PR. Influence of a complementary treatment with oral enzymes on patients with colorectal cancers--an epidemiological retrolective cohort study. Cancer Chemother Pharmacol. 2001;47S:S55–63. doi: 10.1007/s002800170010. [DOI] [PubMed] [Google Scholar]
- 196.Rumsfeld JS, Magid DJ, Plomondon ME, et al. Predictors of quality of life following acute coronary syndromes. Am J Cardiol. 2001;88:781–784. doi: 10.1016/s0002-9149(01)01852-5. [DOI] [PubMed] [Google Scholar]
- 197.Schnuelle P, Berger S, de Boer J, Persijn G, van der Woude FJ. Effects of catecholamine application to brain-dead donors on graft survival in solid organ transplantation. Transplantation. 2001;72:455–463. doi: 10.1097/00007890-200108150-00017. [DOI] [PubMed] [Google Scholar]
- 198.Shlipak MG, Browner WS, Noguchi H, Massie B, Frances CD, McClellan M. Comparison of the effects of angiotensin converting-enzyme inhibitors and beta blockers on survival in elderly patients with reduced left ventricular function after myocardial infarction. Am J Med. 2001;110:425–433. doi: 10.1016/s0002-9343(01)00652-0. [DOI] [PubMed] [Google Scholar]
- 199.Tu JV, Austin PC, Chan BT. Relationship between annual volume of patients treated by admitting physician and mortality after acute myocardial infarction. JAMA. 2001;285:3116–3122. doi: 10.1001/jama.285.24.3116. [DOI] [PubMed] [Google Scholar]
- 200.Auerbach AD, Hamel MB, Davis RB, et al. Resource use and survival of patients hospitalized with congestive heart failure: differences in care by specialty of the attending physician. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 2000;132:191–200. doi: 10.7326/0003-4819-132-3-200002010-00004. [DOI] [PubMed] [Google Scholar]
- 201.Hannan EL, Racz MJ, Arani DT, McCallister BD, Walford G, Ryan TJ. A comparison of short- and long-term outcomes for balloon angioplasty and coronary stent placement. J Am Coll Cardiol. 2000;36:395–403. doi: 10.1016/s0735-1097(00)00752-x. [DOI] [PubMed] [Google Scholar]
- 202.Petersen LA, Normand SL, Daley J, McNeil BJ. Outcome of myocardial infarction in Veterans Health Administration patients as compared with medicare patients. N Engl J Med. 2000;343:1934–1941. doi: 10.1056/NEJM200012283432606. [DOI] [PubMed] [Google Scholar]
- 203.Shwartz M, Saitz R, Mulvey K, Brannigan P. The value of acupuncture detoxification programs in a substance abuse treatment system. J Subst Abuse Treat. 1999;17:305–312. doi: 10.1016/s0740-5472(99)00010-0. [DOI] [PubMed] [Google Scholar]
- 204.Cooper GS, Chak A, Connors AF, Jr, Harper DL, Rosenthal GE. The effectiveness of early endoscopy for upper gastrointestinal hemorrhage: a community-based analysis. Med Care. 1998;36:462–474. doi: 10.1097/00005650-199804000-00003. [DOI] [PubMed] [Google Scholar]
- 205.Fraenkel L, Zhang Y, Chaisson CE, Evans SR, Wilson PW, Felson DT. The association of estrogen replacement therapy and the Raynaud phenomenon in postmenopausal women. Ann Intern Med. 1998;129:208–211. doi: 10.7326/0003-4819-129-3-199808010-00009. [DOI] [PubMed] [Google Scholar]
- 206.Van den Eeden SK, Glasser M, Mathias SD, Colwell HH, Pasta DJ, Kunz K. Quality of life, health care utilization, and costs among women undergoing hysterectomy in a managed-care setting. Am J Obstet Gynecol. 1998;178:91–100. doi: 10.1016/s0002-9378(98)70633-7. [DOI] [PubMed] [Google Scholar]
- 207.King SB, 3rd, Barnhart HX, Kosinski AS, et al. Angioplasty or surgery for multivessel coronary artery disease: comparison of eligible registry and randomized patients in the EAST trial and influence of treatment selection on outcomes. Emory Angioplasty versus Surgery Trial Investigators. Am J Cardiol. 1997;79:1453–1459. doi: 10.1016/s0002-9149(97)00170-7. [DOI] [PubMed] [Google Scholar]
- 208.Soumerai SB, McLaughlin TJ, Spiegelman D, Hertzmark E, Thibault G, Goldman L. Adverse outcomes of underuse of beta-blockers in elderly survivors of acute myocardial infarction. JAMA. 1997;277:115–121. [PubMed] [Google Scholar]
- 209.Fiebach NH, Cook EF, Lee TH, et al. Outcomes in patients with myocardial infarction who are initially admitted to stepdown units: data from the Multicenter Chest Pain Study. Am J Med. 1990;89:15–20. doi: 10.1016/0002-9343(90)90091-q. [DOI] [PubMed] [Google Scholar]
- 210.Cepeda MSRB, Farrar JT, Strom BL. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol. 2003;158:280–287. doi: 10.1093/aje/kwg115. [DOI] [PubMed] [Google Scholar]
- 211.Weitzen S, Lapane KL, Toledano AY, Hume AL, Mor V. Principles for modeling propensity scores in medical research: a systematic literature review. Pharmacoepidemiol Drug Saf. 2004;13:841–853. doi: 10.1002/pds.969. [DOI] [PubMed] [Google Scholar]
- 212.Greenland S, Robins JM. Confounding and misclassification. Am J Epidemiol. 1985;122:495–506. doi: 10.1093/oxfordjournals.aje.a114131. [DOI] [PubMed] [Google Scholar]
- 213.Robins JM, Greenland S. The role of model selection in causal inference from nonexperimental data. Am J Epidemiol. 1986;123:392–402. doi: 10.1093/oxfordjournals.aje.a114254. [DOI] [PubMed] [Google Scholar]
- 214.Cook EF, Goldman L. Performance of tests of significance based on stratification by a multivariate confounder score or by a propensity score. J Clin Epidemiol. 1989;42:317–324. doi: 10.1016/0895-4356(89)90036-x. [DOI] [PubMed] [Google Scholar]
- 215.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 216.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49:1373–1379. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 217.Braitman LE, Rosenbaum PR. Rare outcomes, common treatments: analytic strategies using propensity scores. Ann Intern Med. 2002;137:693–695. doi: 10.7326/0003-4819-137-8-200210150-00015. [DOI] [PubMed] [Google Scholar]
- 218.Cepeda MS. The use of propensity scores in pharmacoepidemiologic research. Pharmacoepidemiol Drug Saf. 2000;9:103–104. doi: 10.1002/(SICI)1099-1557(200003/04)9:2<103::AID-PDS477>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 219.Drake C. Effects of misspecification of the propensity score on estimators of treatment effect. Biometrics. 1993;49:1231–1236. [Google Scholar]
- 220.Dehejia R, Wahba S. Causal effect in non-experimental studies: reevaluating the evaluation of training programs. J Am Stat Assoc. 1999;94:1053–1062. [Google Scholar]
- 221.Stürmer T, Schneeweiss S, Brookhart MA, Rothman KJ, Avorn J, Glynn RJ. Analytic Strategies to adjust confounding using Exposure Propensity Scores and Disease Risk Scores: Nonsteroidal Antiinflammatory Drugs and Short-Term Mortality in the Elderly. Am J Epidemiol. 2005;161:891–898. doi: 10.1093/aje/kwi106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Hosmer DW, Lemenshow S. Applied Logistic regression (2nd Ed): Wiley, New York; 2000. 223. Perkins SM, Tu W, Underhill MG, Zhou XH, Murray MD. The use of propensity scores in pharmacoepidemiologic researc. Pharmacoepidemiol Drug Saf. 2000;9:93–101. doi: 10.1002/(SICI)1099-1557(200003/04)9:2<93::AID-PDS474>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]


