Abstract
Certain groups in the United States remain at high risk and suffer disproportionately from tobacco-related illness and death despite progress made in reducing tobacco use. To address gaps in research on tobacco-related disparities and develop a comprehensive agenda aimed at reducing such disparities, representatives from funding agencies, community-based organizations, and academic institutions convened at the National Conference on Tobacco and Health Disparities in 2002. Conference participants reviewed the current research, identified existing gaps, and prioritized scientific recommendations. Panel discussions were organized to address research areas affecting underserved and understudied populations. We report major research recommendations made by the conference participants in several scientific domains. These recommendations will ultimately help guide the field in reducing and eliminating tobacco-related disparities in the United States.
ACCORDING TO THE 2000 surgeon general’s report Reducing Tobacco Use, eliminating health disparities related to tobacco use is a major public health challenge.1 Members of racial/ethnic minority groups, individuals of low socioeconomic status, and other groups remain at high risk for tobacco use and suffer disproportionately from tobacco-related illness and death.2–4 Health disparities exist within and between populations, and little is known about the causes of population differences observed in exposure and susceptibility to, and the consequences of, tobacco use, addiction, and related diseases.
Consequently, the evidence base for designing and implementing effective prevention and cessation interventions aimed at understudied and historically underserved populations in the United States is limited. Additional scientific investigation is needed to identify optimal entry points to address health inequities and to understand how to interrupt increasing disparities among certain populations.
The challenge of eliminating disparities requires concerted efforts by scientists, health professionals, policymakers, and others to address inequities in health as well as to amend the scientific research agenda. Such efforts will help to raise critical questions that will generate empirical data, identify action steps for research, and facilitate the development of strategic plans and interventions to address tobacco-related disparities in present and future initiatives. Few efforts to date have systematically addressed research initiatives for populations in which disparities are present or have identified key scientific domains upon which to base future inquiry.
The National Conference on Tobacco and Health Disparities (NCTHD), held in December 2002, represented the first scientific gathering to convene researchers and practitioners to review the current research, identify gaps, and develop a research agenda to eliminate tobacco-related health disparities. Collaborators who supported and developed the meeting content and agenda included representatives from the National Cancer Institute, the Centers for Disease Control and Prevention, the American Legacy Foundation, the Robert Wood Johnson Foundation, the Campaign for Tobacco-Free Kids, the American Cancer Society, the National Latino Council on Alcohol and Tobacco Prevention, and the National African American Tobacco Prevention Network, along with the planning committee members.
The NCTHD planning committee defined tobacco-related health disparities as follows: “differences in the patterns, prevention, and treatment of tobacco use; the risk, incidence, morbidity, mortality, and burden of tobacco-related illness that exist among specific population groups in the United States; and related differences in capacity and infrastructure, access to resources, and environmental tobacco smoke exposure.” This definition was employed by conference participants from multiple disciplines to advance our understanding of tobacco-related disparities in 11 specific research domains5: epidemiology, surveillance, psychosocial, basic biology, harm reduction, marketing, policy, community and state, prevention of tobacco use, treatment of nicotine addiction, and research capacity and infrastructure (Table 1 ▶).
TABLE 1—
Definitions of Key Scientific Areas
| Scientific Area | Definition |
| Epidemiologya | Assesses the relationships between tobacco use, behavioral factors, biological/genetic factors, the environment, and disease outcomes in populations |
| Surveillancea | Monitors and evaluates trends in tobacco use, tobacco-related risk factors, behaviors, and health services, and the influence of these trends on disease incidence, morbidity, mortality, and survival |
| Psychosocial researcha | Identifies the behavioral, cultural, psychological, and social factors that influence tobacco use behaviors and studies to develop and test interventions aimed at changing tobacco-related behaviors |
| Basic biologya | Assesses the effects of tobacco and tobacco products on cell biology and cellular mechanisms of action, including the role of tobacco and tobacco by-products in the initiation and promotion of disease and the biological and health effects of exposure to tobacco |
| Harm reductionb | Minimizes the net damage to health associated with the use of tobacco products, constituents of tobacco products, and other substitutes for tobacco products |
| Marketingc | Examines audience segmentation, distribution patterns, brands, advertisements, promotion, and production of tobacco products |
| Policya | Assesses the effects of worksite, community, state, and federal policies on tobacco initiation and use |
| Community and statea | Focuses on the impact and dissemination of single and multiple interventions on the prevention and cessation of tobacco use among large groups of people |
| Prevention of tobacco usea | Identifies and tests interventions designed to prevent the initiation of tobacco use and nicotine addiction |
| Treatment of nicotine addictiona | Identifies, tests, and effectively disseminates interventions to treat tobacco users addicted to nicotine |
| Research capacity and infrastructurea | Ensures the availability of necessary human, financial, and technological resources; systems for collaboration; and mechanisms for information dissemination feedback to provide a strong foundation upon which effective research can be designed and conducted, and public health initiatives can be developed and implemented |
aAdapted from Tobacco Research Implementation Plan: Priorities for Tobacco Research Beyond the Year 2000.5
bK. Warner, unpublished data presented at Reducing Tobacco Harm Conference, May 10, 2001.
cDefinition developed by conference planning committee.
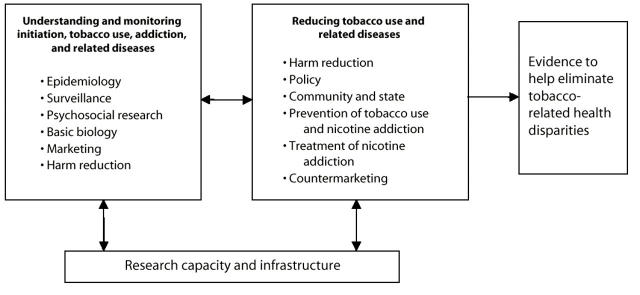
Research in these scientific domains can contribute enormously to our understanding of tobacco use, addiction, and related diseases; help to identify interventions to reduce tobacco use; and help to determine the resources and infrastructure needed to implement interventions (Figure 1 ▶). In this article, we outline the research recommendations developed by conference participants in each of the scientific domains.
FIGURE 1—
Scientific areas to be addressed in efforts to eliminate tobacco-related health disparities.
RECOMMENDATIONS FOR RESEARCH
More than 100 research recommendations focusing on high-risk, underserved, and understudied populations were generated at the NCTHD. The major recommendations are reported in Table 2 ▶.
TABLE 2—
Summary of Major Recommendations in Each Scientific Domain
| Domain | Recommendations |
| Epidemiology | Continue and expand research on prevalence and effects of environmental tobacco smoke in small/special populations; develop and implement longitudinal studies focusing on small, understudied, and underserved populations; examine and collect data on tobacco use and individual and community variables that may influence use and quitting behaviors; investigate mechanisms mediating the effects of low socioeconomic status on tobacco use behaviors; increase the study of socioeconomic status in smoking initiation and cessation; conduct more qualitative research on aspects of socioeconomic status, stress, locus of control, cultural affinity, and sexual orientation and their relationship to tobacco use; fund research to examine the effects of acculturation, stress, coping, racism, and discrimination on the etiology of smoking, trajectories, quitting, and disease onset; examine predictors of cessation among African Americans and other ethnic minority adult populations |
| Surveillance | Develop culturally and ethnically appropriate sampling, methods, and measures to obtain larger samples and to assess the smoking behavior of small populations at the national, regional, and local levels; include questions about the use of menthol, light, and other types of cigarettes in national and state surveys; provide further analysis of data collected from national surveys to obtain information on populations in which there are disparities and ethnic communities; expand national and state surveys to include questions relevant to tobacco use behaviors of understudied populations, including questions on smokeless tobacco and other methods of using tobacco |
| Psychosocial research | Convene grant review committees that recognize and value different perspectives and worldviews on research and health; use special peer review groups for grants that examine innovative qualitative and quantitative research needs of small populations; encourage ongoing funding for pilot projects for exploratory studies that develop innovative theories and methods from the perspective of the target population; promote an understanding that psychosocial issues are broader than the individual and encompass that individual’s social context, experience in society, culture, history, and so forth; support research that examines the role of cultural beliefs, perceptions, and behaviors in tobacco use and exposure within multiple populations and channels; develop and assess reliable measures, protocols, methods, and models to assess cultural dimensions; investigate how social support networks can be used to help reduce tobacco use |
| Basic biological | Increase the use of current technologies to determine molecular changes resulting from tobacco exposure to provide clues on biological mechanistic pathways; explore the combination of constituents in tobacco (e.g., menthol) and the effects of differing levels (within products or brands) on addiction and subsequent health effects; conduct larger studies to assess whether observed differences in nicotine addiction and tobacco-related diseases are correlated with genetic variations in racially or ethnically classified social groups; systematically analyze the effects of interactions among tobacco constituents, genetic factors, and other environmental risks on health; create broader multidisciplinary teams to develop a comprehensive perspective on tobacco use, addiction, and health consequences |
| Harm reduction | Create a network of researchers to facilitate communications and collaboration regarding harm reduction studies and recommendations; investigate the impact of products with “harm-reducing” claims on cessation practices of underserved populations; assess patterns of use with ecological momentary assessment in special populations; expand Food and Drug Administration regulation of tobacco product content and claims |
| Marketing | Encourage the use of marketing research to develop communication strategies that address prevention, cessation interventions, and maintenance of quit behaviors; conduct countermarketing research using social marketing techniques and principles with specific application to populations in which there are disparities; develop funding for research on the tobacco industry, including industry documents, and integrate this research into tobacco control practice |
| Policy | Conduct research on different tobacco industry pricing practices in communities, especially low-income neighborhoods; study the impact of tax increases on consumption patterns, quitting, or reductions in numbers of cigarettes smoked in specific minority groups or communities in which there are disparities; conduct research on differential consequences of tobacco use policies in underserved neighborhoods; conduct research in underserved communities on the enforcement of existing tobacco policies (i.e., environmental tobacco smoke), voluntary policies, and the synergy between them; prioritize funding for community-based policy research to build the case for innovative tobacco control policy activities related to populations in which there are disparities; improve use of research, including basic biological research, in formulating policy; improve understanding of how tobacco control programs, tax increases, and smoking restriction policies together affect changes in tobacco use or quit rates among populations in which there are disparities; collect data on the economic impact of environmental tobacco smoke policies on restaurants, bars, the gaming industry, and so forth in minority communities; conduct research on how to obtain support for environmental tobacco smoke policies in communities in which there are disparities; disseminate information about research findings back to communities |
| Community and state | Conduct community assessment or capacity studies to determine optimal strategies for building, strengthening, and developing tobacco control initiatives; provide sustained funding for long-term community research; document state-level best practices for tobacco policy and control in communities in which there are disparities; build a network for state and community researchers to facilitate effective communication and collaboration; encourage research on the sustainability and effectiveness of anti-tobacco coalitions in addressing tobacco issues in communities of color; develop a system of accountability that ensures funds are spent and priorities are set in accordance with data regarding disparities |
| Prevention of tobacco use | Create a repository of tobacco control resources developed for populations in which there are disparities; ensure that evidence-based programs are culturally appropriate and effective; develop surveys and intervention materials in the native (non-English) language of survey respondents, intervention participants, communities, and so forth; fund randomized controlled trials of comprehensive community-based adolescent prevention programs; fund more studies to develop interventions to reduce children’s exposure to environmental tobacco smoke in homes |
| Treatment of nicotine addiction | Develop and evaluate interventions to promote delivery and use of treatment for nicotine addiction in various groups, including substance abusers and the mentally ill; conduct research on how evidence-based treatment programs are adopted, implemented, and maintained in health care systems, schools, and so forth; develop novel therapies and innovative ways of treating nicotine dependence; examine treatment in other fields for relevance to the treatment of nicotine dependence; examine barriers to use of behavioral and pharmacological treatments at the individual, organizational, and community levels and assess ways of improving access to treatments |
| Research capacity and infrastructure | Expand and fund mentorship programs, such as minority supplements, with mentor stipends to increase opportunities for training in community-based intervention research; fund the training and mentoring of minority researchers; train researchers in effective community research and skills related to building and maintaining relationships, negotiation, and group facilitation; develop strategies to facilitate change in the culture of research in academic and federal settings to make research more receptive to diverse perspectives; develop community-based research processes based on establishing and maintaining long-term relationships within the community; disseminate scientific data in a usable manner for academic research, community researchers, community members, and the general public; develop and explore funding mechanisms that incorporate methods to increase the likelihood that tobacco prevention efforts are culturally relevant and evidence based; develop funding mechanisms that allow for co-principal investigator structure between researchers and community organizations and develop mechanisms to ensure equity in terms of resources; incorporate principles of community participatory research and outcomes into studies and databases; develop funding mechanisms to promote collaborations between investigators at minority-serving institutions and investigators at larger research institutions |
Epidemiology
Epidemiology is a critical scientific domain that can greatly influence our understanding of tobacco use, addiction, and variations in disease. A 1998 report of the surgeon general, Tobacco Use Among U.S. Racial/Ethnic Minority Groups, concluded that few studies have examined the relationships between tobacco use and known health effects in racial/ethnic groups, and, furthermore, few extant databases contain sufficient information to conduct the types of analyses needed.3
This general assessment also applies to other underserved and understudied groups. For example, it was not until 1980 that causal relationships between tobacco use and tobacco-related diseases were established for women.6 Cross-sectional and cohort studies of many populations are lacking or inadequately designed to answer key research questions. The Black Women’s Health Study7 is one of the few empirical investigations to elucidate the associations between risk factors and disease outcomes in understudied populations. The conference participants’ recommendations in regard to addressing these gaps were to support the research needs of small populations, examine the sociological context of tobacco use, implement longitudinal studies, and explore the social context and factors associated with tobacco use and quitting behavior among burdened populations.
Surveillance
Surveillance research helps us monitor trends to identify disparities in use behaviors, diseases, and deaths associated with tobacco. Although many national and state surveillance systems monitor trends in tobacco use, most do not specifically focus on disparities and do not collect or report data on smaller population groups. For example, certain tobacco products such as Iq’mik, a form of chewing tobacco used by Alaska Natives, are not measured on national surveys (C. C. Renner, unpublished data presented at the NCTHD, December 12, 2002). Furthermore, national surveys do not regularly ask questions about sexual orientation, yet a recent review study of lesbian, gay, and bisexual populations indicates that their smoking prevalence rates may be as high as 50%,8 suggesting that there is a need to include questions focusing on sexual orientation. Data on Asians are typically reported in an aggregate manner, masking high rates of smoking among Southeast Asian men (e.g., Vietnamese, Laotian, and Cambodian men)9,10; when sample sizes are small, it is not possible to conduct multilevel analyses. Such differences in smoking suggest that there are important intra-ethnic, nativity, and regional variations3,9,11,12 that should be considered in developing interventions.
The recommendations from conference participants were to address the needs of small populations and communities, explore study designs and methodologies, determine the appropriateness of survey measures, and address the comprehensiveness of surveillance systems.
Psychosocial Research
Understanding tobacco use also requires knowledge of the context of specific cultural variables, norms, values, and community determinants and how these factors vary and interact within and between groups. Depending on context or other environmental attributes, variables such as acculturation may operate as risk factors in some populations and as protective factors in others. An understanding of how constructs are operationalized requires qualitative empirical strategies that provide context to the experiences and processes associated with tobacco use, as well as quantitative inquiry, which provides data on the relationships between multiple variables.
The field is just beginning to recognize the symbiotic nature between these types of investigations, which will enable us to comprehend the complexity of interactions among individual and community factors that influence tobacco use, cessation, and relapse. Also of note is researchers’ tendency to operationalize psychosocial variables mainly in terms of the individual, with less focus on the community as the unit of analysis. The recommendations of the NCTHD participants were to identify risk and protective factors, develop appropriate measures for constructs, address systems issues, and examine the context of tobacco use behavior among racial/ethnic groups; immigrant populations; prison populations; the mentally ill; lesbian, gay, bisexual, and transgender populations; and faith-based communities.
Basic Biology
While observational and field research can help increase our understanding of tobacco use, basic biological research could provide additional information necessary to explain differences in tobacco-related disease outcomes among populations and the role of menthol in tobacco use and tobacco-related disease. Basic biological research may also explain the relationship between green tobacco sickness (an occupational illness resulting from transdermal nicotine exposure) and nicotine exposure among Latino tobacco farm workers.13 Research in basic biology may require greater interdisciplinary collaborations to better integrate the science so that researchers can explore multiple biological pathways. The recommendations of the conference participants included the following: continue laboratory research, expand networks, and examine multiple interactions between risk factors.
Harm Reduction
While new to the tobacco research agenda, the study of harm reduction products will add to our understanding of tobacco product use and help to identify methods to reduce tobacco use and associated negative health consequences. Harm reduction, used as an intervention strategy in drug abuse research,14–17 has become increasingly accepted in tobacco control research since the Institute of Medicine published Clearing the Smoke18 in 2000, which explored this topic and provided tobacco control recommendations. The connection between harm reduction and health disparities is still evolving; however, given the availability of products with harm reduction claims, the use of strategies to reduce numbers of cigarettes smoked, and consumer practices in regard to brand preferences, it remains important to assess, monitor, and evaluate harm reduction’s relevance to disparities research and impact on tobacco use. The recommendations of the NCTHD participants were to improve networking practices, investigate regulations associated with harm reduction claims, and conduct additional research.
Marketing
Marketing and countermarketing research can help increase our understanding of tobacco use and strategies to reduce rates of use among populations with disparities. The tobacco industry has a long history of targeting its marketing efforts toward populations such as women, youths, young adults, African Americans, Hispanics, Asian American/Pacific Islanders, Native Americans, and lesbian, gay, bisexual, and transgender populations.3,4,19–24 It is still not clear how point-of-purchase advertising affects consumption patterns or how best to mobilize retailers in underserved communities to reject incentives and change promotional practices. Furthermore, additional evidence is needed to clarify the effects of countermarketing campaigns on understudied and underserved populations. The NCTHD participants recommended increased research on communications, countermarketing, and the tobacco industry itself (e.g., industry documents).
Policy
Public clean indoor air regulations, tobacco excise taxes, and home and car restrictions on smoking are strategies that protect nonsmokers and help reduce smoking prevalence rates in many states. Despite funding cuts to tobacco control budgets, many states, such as Delaware, California, Connecticut, Massachusetts, and New York, have been successful in passing clean indoor air ordinances.25,26 Twenty-one states raised excise taxes in 2002, and past research suggests that increases in excise taxes decrease consumption rates among the general population.27–29 However, little research has been conducted to assess the impact of policy interventions on tobacco use, cessation, and relapse behavior or to assess the economic impact of interventions such as taxes on low-income groups, blue-collar workers, farmers, service workers, and other understudied populations. Additional studies focusing on views and perceptions of tobacco control policies are also needed among populations with disparities.30 NCTHD participants’ recommendations focused on examining the effects of policies and perceptions of policies in underserved communities.
Community and State
Given that the states have received funds from the Master Settlement Agreement (MSA) to implement tobacco control initiatives, it is prudent to conduct community and state research to evaluate and assess what is being done and to determine the efficacy of community and state efforts. Despite monetary allocations from states, the lack of infrastructure and resources has affected communities’ and states’ ability to conduct and sustain educational programs, clinical services, media programs, and policy interventions in a variety of settings. It is unclear how effective MSA-funded programs have been in reaching communities or the extent of involvement of low-income, rural, and racial/ethnic communities in the development of these programs. Many of the conference participants’ recommendations were not directed at developing new interventions, instead focusing on building networks, synthesizing research, and developing tools for conducting community- and state-level research to reach underserved and understudied populations.
Prevention of Tobacco Use
Tobacco use prevention research has primarily focused on young people, but for many populations, such as African Americans and Asian ethnic groups, targeted prevention programs may be necessary to prevent adult onset of tobacco use. However, little research is available to clarify the risk and protective factors along the age continuum or at different developmental stages, which would provide information regarding the ways in which disparities evolve in high-risk groups. Additional youth-focused studies are needed to help prevent exposure to environmental tobacco smoke in the home and to target groups of young people with multiple risks or problem behaviors. Additional work is also needed to help ensure the effectiveness of research prevention protocols, materials, and interventions aimed at populations in which disparities exist.31 The recommendations of the NCTHD participants were to fund intervention research and synthesize existing evidence on prevention efforts.
Treatment of Nicotine Addiction
Additional epidemiological, surveillance, marketing, and psychosocial research may inform the treatment of nicotine addiction in populations exhibiting disparities. The limited knowledge of treating tobacco use, addiction, and related diseases provides little information on which to base effective intervention programs for underserved and understudied populations. Several recent reviews of cessation interventions for African Americans concluded that more studies are needed to identify successful smoking cessation interventions.32,33 While some progress has been made in assessing treatment efficacy among populations in which disparities are present,34 it is not clear how evidence-based treatments are adopted, implemented, and maintained in certain community systems (e.g., rural residents; the elderly; substance abusers; mentally ill individuals; lesbian, gay, bisexual, and transgender populations; low-income individuals; and racial/ethnic groups). The recommendations stemming from the NCTHD were to investigate therapies and interventions for treatment and to identify treatment barriers.
Research Capacity and Infrastructure
The scientific domains just described cannot be addressed without building the capacity and developing the infrastructure at multiple levels to conduct research involving understudied and underserved populations. In recent years, funding agencies have paid more attention to building infrastructure at multiple levels to support research and advocacy efforts, particularly in the areas of training, community-based participatory research, and dissemination. In addition, many national organizations, including the National Cancer Institute, the Robert Wood Johnson Foundation, the Centers for Disease Control and Prevention, and the American Legacy Foundation, have funded training programs to increase the pool of researchers from minority and underrepresented groups, cross train researchers in multiple disciplines, and work with community organizations to build capacity and conduct research.
Building research infrastructure allows researchers to raise incisive questions relevant to underserved and understudied populations, work more effectively with these populations, and develop community relationships to facilitate intervention and evaluation research. The conference participants recommended that support be provided in the areas of research training and mentoring, building collaborations between communities and academic institutions, and facilitating community-based research.
DISCUSSION
Embedded in the challenge to eliminate health disparities is the need to address tobacco use and related diseases among underserved and understudied populations. Addressing each of the 11 scientific domains described here will contribute to our understanding of tobacco use and related diseases and ultimately help to identify the entry points necessary to reduce tobacco-related disparities by enhancing our collective capability to intervene in burdened populations. Many of the recommendations stemming from the NCTHD focus heavily on expanding our understanding of tobacco use, addiction, and related diseases, thus reflecting the viewpoint that the tobacco control field is minimally prepared to develop effective interventions for populations exhibiting disparities. A more solid evidence base is needed, one that involves both quantitative and qualitative data upon which to develop interventions for populations in which disparities are present. How we move forward to build this evidence base represents an additional challenge to the field.
Several barriers, including limited financial resources, may affect the implementation of a research agenda on tobacco and health disparities. Many state organizations, as well as some private organizations, have eliminated or severely curtailed tobacco control programs and have diverted funds to other priority areas. If this trend continues, fewer resources will be available to reduce tobacco use and disease in underserved and understudied populations. No single organization can fully support these efforts; however, creative funding options and collaborative projects among researchers could help minimize the effects of recent changes.
The recent focus on disparity-based research in public health represents a major change in conceptualizing and understanding differences in health behavior, risks, and outcomes. The viewpoint that differences in health status are linked to economic, social, and political inequalities is a fundamental aspect of this perspective. Equally important is the proposition that research on disparities demands methodologically sound scientific innovations, professional dedication, and courage. These steps partly entail acknowledging the shortcomings and inequities involved in our scientific disciplines and rethinking what we decide to study. In addition, these recommendations are intended to encourage researchers, funders, and policymakers to discuss, debate, amend, and work to meet the challenges of this research agenda.
The process of collaboration between stakeholders such as researchers, practitioners, and community organizations with respect to research on disparities indicates the need for alternative viewpoints. In this regard, the work of Friere35 and others has much to offer to the proposed research agenda on tobacco-related disparities, especially concerning community perceptions about research as “another structure of domination.” Thus, the proposed recommendations for a national agenda to address disparities in tobacco use and related diseases require the research community to consider novel and practical approaches to the process of conducting research focusing on tobacco prevention and control. Disparity-based research will compel investigators not only to focus on quantitative and qualitative differences between groups but to examine the underlying reasons for these differences, adopt appropriate measures and standards of comparison, address the needs of smaller populations, conduct intragroup research, and translate research findings into policy.
Finally, moving forward with these recommendations requires that the research community and funding organizations allow for a certain degree of creativity and risk taking among investigators who use innovative research strategies to address tobacco-related health disparities. The trial-and-error process of using rigorous scientific standards, albeit protracted, has proven to be effective in advancing public health. In addition, the commitment to this challenge must be undergirded with the fortitude and patience to build upon conventional and long-established approaches to empirical investigations and develop new ideas and research strategies.
Acknowledgments
The National Cancer Institute, the Centers for Disease Control and Prevention, the American Legacy Foundation, the Robert Wood Johnson Foundation, the Campaign for Tobacco-Free Kids, and the American Cancer Society provided funding for the National Conference on Tobacco and Health Disparities.
Note. This article represents the views of the authors and conference participants and does not reflect the respective policy positions of the funding agencies.
Human Participant Protection No protocol approval was needed for this study.
Contributors P. Fagan summarized the recommendations, revised drafts of the article, and led the writing team. G. King and D. Lawrence contributed to the recommendation synthesis and editing of the article. S. Petrucci contributed to editing and to developing the recommendations section. R. Robinson, D. Banks, and S. Marable contributed to editing and to development of the recommendations and discussion sections. R. Grana assisted with the background research, synthesis of conference notes, and editing of the article.
Peer Reviewed
References
- 1.Reducing Tobacco Use. Atlanta, Ga: Centers for Disease Control and Prevention; 2000.
- 2.The Health Consequences of Smoking: Cancer and Chronic Lung Disease in the Workplace. Atlanta, Ga: Centers for Disease Control and Prevention; 1985.
- 3.Tobacco Use Among U.S. Racial/Ethnic Minority Groups. Atlanta, Ga: Centers for Disease Control and Prevention; 1998.
- 4.Women and Smoking. Atlanta, Ga: Centers for Disease Control and Prevention; 2001.
- 5.Tobacco Research Implementation Plan: Priorities for Tobacco Research Beyond the Year 2000. Bethesda, Md: National Cancer Institute; 1998. DHHS publication T644.
- 6.The Health Consequences of Smoking for Women. Atlanta, Ga: Centers for Disease Control and Prevention; 1980.
- 7.Russell C, Palmer JR, Adams-Campbell LL, Rosenberg L. Follow-up of a large cohort of black women. Am J Epidemiol. 2001;154:845–853. [DOI] [PubMed] [Google Scholar]
- 8.Ryan H, Wortley PM, Easton A, Pederson L, Greenwood G. Smoking among lesbians, gays, and bisexuals: a review of the literature. Am J Prev Med. 2001;21:142–149. [DOI] [PubMed] [Google Scholar]
- 9.Ma GX, Shive S, Tan Y, Toubbeh J. Prevalence and predictors of tobacco use among Asian Americans in the Delaware Valley region. Am J Public Health. 2002;92:1013–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moeschberger ML, Anderson J, Kuo YF, Chen MS, Wewers ME, Guthrie R. Multivariate profile of smoking in Southeast Asian men: a biochemically verified analysis. Prev Med. 1997;26:53–58. [DOI] [PubMed] [Google Scholar]
- 11.King G, Polednak AP, Bendel R. Regional variation in smoking among African Americans. Prev Med. 1999;29:126–132. [DOI] [PubMed] [Google Scholar]
- 12.King G, Polednak AP, Bendel R, Hovey D. Cigarette smoking among native and foreign-born African Americans. Ann Epidemiol. 1999;9:236–244. [DOI] [PubMed] [Google Scholar]
- 13.Arcury TA, Quandt SA, Preisser JS, Bernert JT, Norton D, Wang J. High levels of transdermal nicotine exposure produce green tobacco sickness in Latino farmworkers. Nicotine Tob Res. 2003;5:315–321. [DOI] [PubMed] [Google Scholar]
- 14.Berridge V. Histories of harm reduction: illicit drugs, tobacco, and nicotine. Subst Use Misuse. 1999;34:35–47. [DOI] [PubMed] [Google Scholar]
- 15.Decorte T. Quality control by cocaine users: underdeveloped harm reduction strategies. Eur Addict Res. 2001;7:161–175. [DOI] [PubMed] [Google Scholar]
- 16.Hilton BA, Thompson R, Moore-Dempsey L, Janzen RG. Harm reduction theories and strategies for control of human immunodeficiency virus: a review of the literature. J Adv Nurs. 2001;33:357–370. [DOI] [PubMed] [Google Scholar]
- 17.Pollack HA. Ignoring ‘downstream infection’ in the evaluation of harm reduction interventions for injection drug users. Eur J Epidemiol. 2001;17:391–395. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine. Clearing the Smoke: Assessing the Science Base for Tobacco Harm Reduction. Washington, DC: National Academy Press; 2001:23. [DOI] [PubMed]
- 19.Preventing Tobacco Use Among Young People. Atlanta, Ga: Centers for Disease Control and Prevention; 1994.
- 20.Geobel K. Lesbians and gays face tobacco targeting. Tob Control. 1994;3:65–67. [Google Scholar]
- 21.Ling PM, Glantz SA. Why and how the tobacco industry sells cigarettes to young adults: evidence from industry documents. Am J Public Health. 2002;92:908–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yerger VB, Malone RE. African American leadership groups: smoking with the enemy. Tob Control. 2002;11:336–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robinson RG, Barry M, Bloch M, et al. Report of the Tobacco Policy Research Group on marketing and promotions targeted at African Americans, Latinos, and women. Tob Control. 1992;1:S24–S30. [Google Scholar]
- 24.Robinson RG, Pertschuk M, Sutton C. Smoking and African Americans: spotlighting the effects of smoking and tobacco promotion in the African American community. In: Samuels SE, Smith MD, eds. Improving the Health of the Poor. Menlo Park, Calif: Henry J. Kaiser Family Foundation; 1992.
- 25.Americans for Nonsmokers’ Rights. Municipalities with 100% smokefree ordinances. Available at: http://www.no-smoke.org/100ordlisttabs.pdf. Accessed March 31, 2003.
- 26.Americans for Nonsmokers’ Rights. Municipalities with 100% clean indoor air ordinances. Available at: http://www.no-smoke.org/100ordgraph.pdf. Accessed March 31, 2003.
- 27.Centers for Disease Control and Prevention. Cigarette smoking before and after an excise tax increase and an antismoking campaign—Massachusetts, 1990–1996. MMWR Morb Mortal Wkly Rep. 1996;45:966–970. [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Responses to increases in cigarette prices by race/ethnicity, income, and age groups—United States, 1976–1993. MMWR Morb Mortal Wkly Rep. 1998;47:605–609. [PubMed] [Google Scholar]
- 29.Zhang P, Husten C, Giovino G. Effect of the tobacco price support program on cigarette consumption in the United States: an updated model. Am J Public Health. 2000;90:746–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.King G, Mallett RK, Kozlowski LT, Bendel RB. African Americans’ attitudes toward cigarette excise taxes. Am J Public Health. 2003;93:828–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robinson RG. Community development model for public health applications: overview of a model to eliminate population disparities. J Health Educ Pract. In press. [DOI] [PubMed]
- 32.Lawrence D, Graber JE, Mills SL, Meissner HI, Warnecke R. Smoking cessation interventions in U.S. racial/ethnic minority populations: an assessment of the literature. Prev Med. 2003;36:204–216. [DOI] [PubMed] [Google Scholar]
- 33.Peterson LL, Ahluwalia JS, Harris KJ, McGrady GA. Smoking cessation among African Americans: what we know and don’t know about interventions and self quitting. Prev Med. 2000;31:23–38. [DOI] [PubMed] [Google Scholar]
- 34.Boyd NR, Sutton C, Orleans CT, et al. Quit today! A targeted communications campaign to increase use of the Cancer Information Service by African American smokers. Prev Med. 1998;27:S50–S60. [DOI] [PubMed] [Google Scholar]
- 35.Friere P. Pedagogy of the Oppressed. New York, NY: Continuum; 1970.