Abstract
In the United States in 1997, the smoking prevalence among blue-collar workers was nearly double that among white-collar workers, underscoring the need for new approaches to reduce social disparities in tobacco use. These inequalities reflect larger structural forces that shape the social context of workers’ lives.
Drawing from a range of social and behavioral theories and lessons from social epidemiology, we articulate a social-contextual model for understanding ways in which socioeconomic position, particularly occupation, influences smoking patterns. We present applications of this model to worksite-based smoking cessation interventions among blue-collar workers and provide empirical support for this model. We also propose avenues for future research guided by this model.
Persistent and growing disparities in smoking prevalence by occupation underscore the need for new approaches to tobacco control. In the United States in 1997, the smoking prevalence among male blue-collar workers was nearly twice that of men in white-collar occupations (37% vs 21%), and similar disparities were observed among women (33% for women in blue-collar vs 20% for those in white-collar occupations).1
In addition, blue-collar workers’ rates of smoking are declining more slowly than those of other workers.2 A recent analysis of data from the 2000 National Health Interview Survey found that smoking prevalence was highest among persons with working-class jobs, low education, and low income and that each of these indicators of socioeconomic position was independently and positively associated with smoking prevalence. These findings also indicated that whereas there was no socioeconomic gradient in attempts to quit, success with quitting was highest among those with the most socioeconomic resources.3
These disparities reflect larger structural forces that shape the social context of people’s lives—the fabric and texture of day-to-day experiences and realities. Social context includes an array of social and material factors that ultimately have profound effects on health and health behaviors.4–6 For example, results of the Alameda County Study demonstrated that behaviors such as smoking are associated with low income and cluster with social-contextual factors such as unemployment, lack of social support, living in unsafe neighborhoods, and having unmet needs for food and medical care.6
Similarly, Graham5,7 reported that social-contextual factors associated with low income are particularly relevant for smoking patterns. She concluded that different factors influence patterns of tobacco use among low-income women relative to women in the middle and upper classes. For low-income women, smoking may be used as a means of coping with economic pressures and the resulting demands placed on them to care for others. Graham categorized these influences as including everyday responsibilities, such as child care and patterns of paid work; material circumstances, including housing, debt load, and access to a car; social support and social networks; and personal and health resources, including patterns of health-related behavior and alternative coping strategies. Even among low-income women, smoking rates were associated with having fewer resources and greater role responsibilities such as work responsibilities and child care.
To date, little research has been conducted to develop effective methods to reduce class-based disparities in tobacco use. We present a social-contextual model for understanding the influence of socioeconomic position on smoking patterns, apply this model to worksite-based smoking cessation efforts among blue-collar workers, and suggest avenues along which future research may be guided by this model. We incorporate a range of social and behavioral theories and lessons from social epidemiology to explicate the social-contextual pathways by which socioeconomic position may influence tobacco use.8–13 Socioeconomic position may be defined as a social relationship premised on people’s structural location within the economy14; it determines one’s prospects in life, exposures to life stressors, and access to social, educational, and economic resources.15
We focus particularly on occupation to identify approaches to reducing tobacco use among workers in the lowest occupational ranks. These positions include those traditionally defined as “blue collar,” including crafts and kindred occupations, operatives, transportation operatives, and laborers. Illuminating the pathways by which occupation may influence tobacco use patterns, will perhaps make it possible to improve the relevance and efficacy of tobacco control interventions for blue-collar workers.
SOCIAL CONTEXT: A MODEL FOR ADDRESSING SOCIAL DISPARITIES
Figure 1 ▶ summarizes current standard practice in tobacco control interventions for adults.16,17 Interventions are designed to influence mediating mechanisms along the pathway between the intervention and outcomes. The social-ecological model provides a useful framework for intervening on mediating mechanisms at multiple levels of influence, one that promotes change not only in individuals but also in organizations and policies. This multilevel approach increases the overall potency of intervention efforts.18,19
FIGURE 1—
Tobacco control interventions: current practice.
At the individual level, interventions may be based on the rich tradition of behavioral research, incorporating guidance from social cognitive theory,20–23 the theory of reasoned action,24–26 or the transtheoretical model of behavior change.27–30 Accordingly, interventions focused on individual behavior change often aim to increase intrinsic motivation to quit, build self-efficacy,21 modify beliefs about the benefits and costs of performing the behavior,31 address nicotine addiction,32 and build skills needed for quitting. Policy- and organizational-level influences on adult smoking cessation have included regulatory efforts prohibiting smoking in public places, including worksites; pricing and taxation policies; and restrictions on the advertising and marketing of tobacco.17,33 As Figure 1 ▶ illustrates, in traditional tobacco control programs, population characteristics such as socioeconomic position are generally examined as background variables needing to be controlled within analyses of intervention effects.
Although this approach has been effective in reducing the overall prevalence of tobacco in the United States,17 it has been less effective in addressing social inequalities in smoking prevalence, as demonstrated by persistent class-based disparities in smoking prevalence. What we are ignoring in this framework is the “black box” through which population characteristics influence smoking behaviors. In Figure 1 ▶, we might imagine a black box positioned between population characteristics and the mediating mechanisms targeted by the intervention. It is important to illuminate this black box, to understand the pathways by which population characteristics influence tobacco use, and thereby to enhance the effectiveness of interventions aimed at reducing social inequalities in risk behaviors.11,34–36
Figure 2 ▶ illustrates a conceptual model that explicates the role of social context in tobacco use cessation.37 We have defined a set of modifying conditions—that is, factors that independently affect outcomes but that interventions are not intended to influence. In essence, we are illuminating the black box described above by explicating a set of modifying conditions that express the influence of socioeconomic position on patterns of tobacco use. These social-contextual factors add to our understanding of the pathways through which factors such as occupation may influence tobacco use patterns.
FIGURE 2—
A social-contextual model for tobacco control.
Source. This figure is adapted from Sorensen et al.93
Note. HP = worksite health promotion only; HP/OSH = worksite health promotion plus occupational safety and health.
This figure also adds a set of social-contextual factors included as mediating mechanisms. Thus, social-contextual factors may function as either modifying conditions or mediating mechanisms, depending on their location within or outside the causal pathway between the intervention and the outcomes. We do not attempt to present the entire universe of factors that might influence or mediate behavior change; rather, we present examples of factors that may be used to guide the intervention and measurement that are particularly relevant to blue-collar workers. Others might use this model to define different mediating mechanisms and modifying conditions salient to different audiences.
Explicating these elements of the social context may enhance interventions in 2 ways. First, on the basis of social and behavioral theory and prior research, intervention planners may identify social-contextual factors that potentially are amenable to change within the context of the planned intervention. These variables are located in the “mediating mechanisms” box in the figure. Second, even when it is not feasible to intervene to change the social context, understanding the variables included in the “modifying mechanisms” box can inform interventions, increasing their salience to the participants.
In Figure 2 ▶, we use a social ecological framework to organize these social-contextual factors across multiple levels of influence, focusing on examples of particular relevance to blue-collar workers.18,19,38,39
Individual factors may include material circumstances that are clearly associated with income and are likely to increase one’s stress, such as debt load and the daily stressors and worries that arise from living in disadvantaged situations. For example, the prevalence of depression is high among both low-income individuals and smokers; smoking is thought to represent a way of coping with mood issues caused by stress and depression.40–42
Individual factors may also intersect with job conditions to define the functional meanings of tobacco use. This construct has been used to describe the meaning given to tobacco use or the purposes such use serves in one’s life, and the construct incorporates both positive and negative beliefs, attitudes, and perceptions about smokers and cigarette smoking.43–46 For workers, tobacco use may serve a range of functions, relieving boredom, isolation, or stress; increasing alertness; and facilitating camaraderie with other workers.
Interpersonal factors may include social ties, family roles and responsibilities, social norms, and relationships at work. In particular, smokers’ social networks often include substantial numbers of other smokers, which limits opportunities for change. Additionally, recent research on smoking shows that characteristics of spousal support influence the ability of a smoker to quit successfully.47 Social norms may function as mediators of the intervention; they vary by social class and are likely to be potent correlates of health behaviors.48 Relationships with supervisors and coworkers are also pivotal. Work group life can shape the discourse on health, including how workers define threats and how they formulate coping strategies.49,50 Tobacco use patterns have been associated with perceived support from one’s supervisor and coworkers.51,52
Organizational factors may include job conditions,51,53,54 such as job characteristics or features of the work task that have been found to influence health behaviors, including job control and job stress, hazardous exposures at work, and the perceived benefits of the work setting.51 Although much of the research on job stress has focused on its implications for health status, it has also been linked to various health-related behaviors, including tobacco use, by previous studies.53,55–57 These studies have indicated, for example, that smoking is more prevalent among workers whose abilities are underused or who have monotonous and repetitive jobs; low success in quitting smoking has been associated with higher levels of occupational stress. A key job characteristic emerging from many of these studies is that of job control, which refers to the nature and amount of the discretion workers may exercise in performing their jobs, including the degree of their control over the volume, speed, and terms of their work. Smoking is among the health behaviors associated with low job control.58,59 Job conditions may also include the potential for exposures to physical hazards on the job.
Neighborhood and community factors may include exposure to tobacco advertising and ready availability of tobacco products. For example, Laws and colleagues60 reported that the proportion of businesses selling tobacco, and thus displaying tobacco advertising, is inversely associated with per capita income in census tracts. Research into the tobacco industry documents made available as a result of lawsuits filed against the major tobacco manufacturers has shown that the tobacco industry views less-educated, working-class individuals as a critical market segment (E. Barbeau et al., unpublished data, 2003). For example, an RJ Reynolds document characterizing smokers of Philip Morris’s Marlboro brand reports:
The loyal Marlboro younger adults can be characterized as having a “working class/present oriented” mindset . . . and worry about their lives of today. . . . The concept of a working class/present oriented mindset is fully consistent with lowered levels of education. Previous analyses have shown that our market is much less highly educated than consumers in general, with the younger adult smokers becoming much less educated . . . in the future, marketing to a working class/present oriented mindset will be even more important in appealing to younger adult smokers.61
Larger societal forces may also shape health behavior. For example, at the policy level, interventions have included regulatory efforts prohibiting smoking in public places, restrictions on youth access to tobacco products, pricing and taxation policies, and restrictions on advertising and marketing of tobacco.33
As illustrated in Figure 2 ▶, these socialcontextual factors are shaped by a range of population characteristics. We focused on socioeconomic position, particularly occupation, as an important predictor of smoking behavior; although other population characteristics, such as gender, race/ethnicity, and age are not the prime focus of this report, we also recognize their importance. These sociodemographic characteristics shape people’s social context; this context in turn influences a range of interrelated health behaviors. Understanding these relationships is paramount to the development of interventions that will be efficacious in reducing health disparities.
EMPIRICAL EVIDENCE IN SUPPORT OF THE MODEL
Worksites are an important venue for efforts to reduce cancer morbidity and mortality62,63; they also provide a promising channel for tobacco control interventions. Through worksites, it is possible to influence the health behaviors of large proportions of the population64,65 and to conduct repeated multilevel interventions to influence health behaviors.63,66,67 Applying the social-contextual model in tobacco control trials among blue-collar workers, we have conceptualized and evaluated interventions that specifically address occupational safety and health conditions as mechanisms that mediate between blue-collar occupations and smoking behavior. Blue-collar workers experience a high prevalence of hazardous exposures on the job,68,69 and those workers exposed to workplace hazards are more likely to be smokers even when gender, race, and education are controlled.70 Thus, we tested interventions that included efforts to reduce hazardous occupational exposures as a means of enhancing smoking cessation rates among bluecollar workers.
There are several reasons to address occupational health and safety as part of comprehensive tobacco control initiatives for blue-collar workers.71 First, workers’ overall risk of disease is increased when they experience exposures to both job hazards and cigarettes.72 The same toxic agents in tobacco smoke may also be present in the worksite (e.g., benzene), thereby increasing exposures to the agent among smokers. In addition, smoking may act synergistically with toxic agents found in the worksite, resulting in a more profound effect than that which might be expected from the separate influences of either the occupational hazard or smoking alone (e.g., asbestos).
Second, workers may view tobacco use as being outside management’s purview, whereas job-related health and safety issues may be seen as a too-often ignored responsibility of management.73–75 Indeed, the risks that matter the most to workers may be those that have been identified as key priorities in risk communication research—risks that are involuntary, outside personal control, undetectable, and inequitably distributed between workers and management,76–78 features that often characterize occupational hazards. Skepticism about management’s commitment to improve worker health may reduce workers’ interest in participating in individually focused health promotion programs at work, particularly when occupational exposures are not addressed.63,79,80 Reduction of job risks may be required to gain credibility with this audience and to increase their receptivity to health education messages about individual health behaviors.74,81 Finally, workers may see little point in attempting to improve personal health habits in view of continuing involuntary exposure to hazardous workplace conditions.
Increasing calls have been made for a comprehensive approach to worker health that addresses health behaviors such as tobacco use within the overall aim of creating healthy workplaces.63,69,82–86 Nearly 2 decades ago, the National Institute for Occupational Safety and Health, the nation’s leading research agency for preventing occupational diseases and injuries, called for simultaneous application of protection from occupational hazards and exposure to health behavior change programs to “make possible a ‘synergism of prevention’ to improve the health of workers through comprehensive risk reduction.”87(iv) Since then, there have been growing numbers of worksite programs that integrate efforts to reduce behavioral risks, including tobacco use, with health protection initiatives such as occupational health and safety programs.81,88–91
We have conducted a series of studies to examine the efficacy of interventions that integrate tobacco control with occupational health and safety. The first of these studies was part of the Working Well Trial. Four research intervention sites tested the effects of a comprehensive worksite cancer prevention model aimed at nutrition and smoking, using a randomized controlled design in 114 worksites nationwide, including 24 at the WellWorks site.65 Only the WellWorks project tested the effectiveness of a model that integrates health promotion and health protection.62 This intervention integrated messages on tobacco control, nutrition, and occupational health in programs for both workers and management. The WellWorks site was the only study center in which a significant result for smoking cessation was observed; the 6-month quit rate in the intervention worksites was 17.3%, compared with 12.7% in the control sites (P = .037).92
In a second study, we asked the question, Does the addition of worksite health protection increase the effectiveness of the program over and above worksite health promotion only?93 The WellWorks-2 study used a randomized, controlled design with the worksite as the unit of assignment and intervention; analyses controlled for worksite. After baseline assessments, 15 manufacturing worksites were randomly assigned to 1 of 2 conditions: (1) worksite health promotion only (HP group; 8 worksites) and (2) worksite health promotion plus occupational safety and health (HP/OSH group; 7 worksites). The intervention components are summarized in Table 1 ▶. This comparison tested the integrated intervention, which included the addition of efforts to reduce occupational hazards; following the framework presented in Figure 2 ▶, these efforts were considered a social-contextual mediating mechanism.
TABLE 1—
Intervention Activities in the WellWorks-2 Study
| Intervention Components | Health Promotion | Health Promotion Plus Occupational Safety and Health |
| Joint worker–management participation | Representation:
|
Representation:
|
| Interventions targeting workplace organizational and environmental change | Consultation to management regarding:
|
Consultation to management regarding:
|
| Interventions targeting change in individual health behaviors | Traditional interventions addressing tobacco and nutrition:
|
Traditional plus integrated b interventions addressing tobacco, nutrition, and occupational health:
|
aCatering policies specify offering healthful food options when food is served at company activities.
bIntegrated interventions address occupational health and nutrition, smoking, or both.
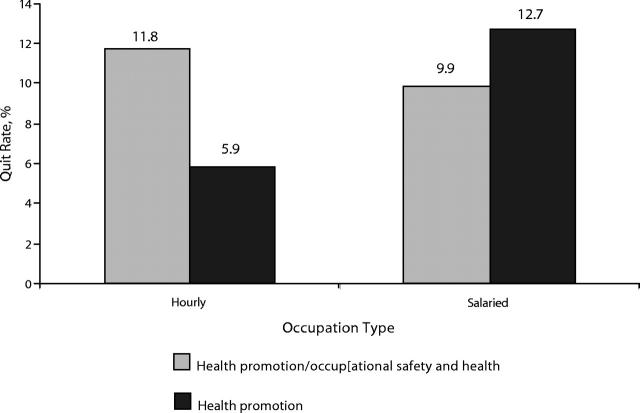
Results of this study for tobacco use cessation for blue-collar (hourly) and white-collar (salaried) workers are presented in Figure 3 ▶. We hypothesized a priori that the integrated health promotion–health protection intervention would have the most relevance to workers in hourly positions, where exposures to hazards on the job are more common than among salaried workers. Smoking quit rates among hourly workers in the HP/OSH condition doubled relative to those among hourly workers in the HP condition (11.8% vs 5.9%; P = .04) and were comparable to quit rates of salaried workers. We found no differences in quit rates between groups for salaried workers.
FIGURE 3—
Results of the WellWorks-2 study: adjusted 6-month quit rates at final assessment by intervention and occupation type (cohort of smokers at baseline: n = 880).
Additionally, we observed that worksites in the intervention condition made statistically significant improvements in their health and safety programs, compared with control sites (A. D. LaMontagne et al., unpublished data). The sample size of worksites in the study did not provide sufficient statistical power to enable us to examine relationships between these improvements and worksite-level smoking cessation rates. These results, however, are important because they demonstrate a positive change in overall worksite health and safety, which was identified as a key social-contextual mediating variable in the intervention. We also found that worker participation in intervention programs was significantly higher in the HP/OSH condition than in the HP condition (M. K. Hunt et al., unpublished data), as measured by process tracking of the intervention “dose” delivered in intervention sites. This finding suggests that the HP/OSH intervention resonated more strongly with workers than did the HP approach.
IMPLICATIONS OF THE SOCIAL-CONTEXTUAL MODEL
This research provides an example of the application of the social-contextual model of health behavior change that focuses on 1 element of the context of work for blue-collar workers: the potential for hazardous occupational exposures. Findings from these studies illustrate that the effectiveness of tobacco control efforts among blue-collar workers is likely to be enhanced when health promotion programs are integrated with occupational health initiatives. There are numerous additional pathways in this model yet to be explored. The next generation of research applying a social-contextual model of behavior change might consider assessing and addressing the roles of other social-contextual features of blue-collar workers’ lives, both inside and outside of work. We offer examples of promising directions for future intervention research aimed at reducing tobacco use among blue-collar workers—either by intervening to change elements of the social context or by enhancing the relevance of interventions by understanding these important realities of workers’ lives.
Management Commitment and Support
Evidence indicates that management commitment to a comprehensive worker health program provides a key foundation for success.94–96 Management commitment and support is necessary for improvements in organizational factors, such as job conditions and organization support for behavior change, as shown in Figure 2 ▶. For findings from worksite-based research to be broadly adopted by employers, it will be necessary to gain their support and commitment—as indicated, for example, by their willingness to allocate resources to worker health initiatives. Employer support may be reflected in corporate plans or mission statements that enable workers to act in the interests of their health.97
Research is needed to identify ways to mobilize and sustain management commitment across a range of settings, from small to large firms, within the public and private sector, and across a range of industries. The WellWorks interventions with management to improve health and safety programs provide 1 promising model (A. D. LaMontagne et al., unpublished data); additional studies are needed (1) to learn whether such interventions are effective in other types of worksites and (2) to identify strategies for increasing management support for health promotion activities as part of occupational health programs.
The Role of Labor Unions
The influence of organized labor has been underused in efforts to reduce tobacco use among blue-collar workers. Yet unions have a long-standing commitment to worker health, as evidenced by their advocacy of worker health and safety and the support many unions demonstrate for worksite tobacco control programs and policies.98 As shown in Figure 2 ▶, labor unions can encourage a supportive organizational climate for health behavior changes by influencing reductions in occupational exposures or improvements in job conditions. Research is needed in several areas: (1) to assess whether labor unions—alone or in labor–management collaborations—provide an effective community-based channel through which to implement integrated health promotion–health protection programs to reduce smoking; (2) to identify successful strategies for engaging labor–management–sponsored health and welfare funds, which are providers of health insurance to many unionized workers, in increasing financial coverage of smoking cessation therapies99; and (3) to assess strategies for encouraging labor–management cooperation in developing and enforcing worksite policies to protect workers from exposure to environmental tobacco smoke.100
Organization of Work and Job Characteristics That Influence Worker Health
Job characteristics and the organization of work are also important correlates of smoking behavior. Shift workers have particularly high rates of smoking.101 Job content and the dynamics of the workplace have ramifications for a worker’s health. These effects clearly extend well beyond blue-collar workers to influence workers in a range of jobs. “Job strain” results when workers face high psychological workload demands combined with low control or decisionmaking latitude in meeting those demands102 and may be compounded by a lack of social support.103 Other specific stressful working conditions may include involuntary overtime, piece-rate work, inflexible hours, arbitrary supervision, and deskilled work.
Assessment of job content may lead to necessary changes in the organization of work, which has been described as central in a range of worksite interventions.54,88,104,105 Breaks must be structured to provide fair and adequate rest; in some workplaces, a smoking break may be the only valid way a worker can have temporary relief from physically or mentally demanding work. Research is needed to develop intervention methods to improve the nature of work and to explore the role of modifications in work organization in contributing to the success of tobacco control efforts.
Social Support and Social Norms Supporting Worker Health
Prior research indicates that coworker support is important in quitting smoking.56 Coworker discouragement of quitting has been associated with lower confidence in one’s ability to quit smoking, and the pressure that smokers feel from nonsmokers has been shown to be effective in motivating them to quit.106 Blue-collar workers are likely to experience social norms less supportive of tobacco control than are whitecollar workers.79 Social norms and social support, from both coworkers and supervisors, are also important in workers’ compliance with protective recommendations.79,107 Research on ways to incorporate social resources in the job setting to support smoking cessation may be instructive. Incorporation of buddy systems, support groups, and peer-led programs may be useful in encouraging smoking cessation.84 Research is needed to explore ways to influence social norms among blue-collar workers, on the basis of a tangible understanding of their norms, values, priorities, and day-to-day realities.
Other Aspects of Workers’ Social Contexts
The social contexts in which workers live, both on and off the job, clearly influence workers’ health behaviors, including tobacco use. These forces are also likely to shape the effectiveness of interventions. It is important to understand, for example, how time on the job is structured, the meaning of smoking within one’s work group, and work stressors, such as those described under Organization of Work and Job Characteristics that Influence Worker Health. The worker’s social context also includes socioeconomic conditions, as well as the physical, social, and cultural environments that influence access to health information, social support, social networks, social norms, cultural beliefs, and attitudes regarding health.97,108 Research is needed to explicate the smoking patterns of family members and friends, the strains presented by balancing multiple roles at home and at work, available social resources, and cultural norms and beliefs, as well as ways to incorporate this information into delivering interventions.
Structural Barriers to Blue-Collar Workers’ Participation in Interventions
Blue-collar workers are less likely than white-collar workers to participate in health promotion programs. It is necessary to understand and address structural barriers to workers’ participation.109 Organizational support for health behavior change may involve strategies to reduce structural barriers to program participation. For blue-collar workers, supervisors function as gatekeepers who control worker access to health promotion activities.79 For instance, to keep production lines moving, supervisors may refuse to allow workers to attend programs on company time. Further barriers may include working overtime, doing shift work, having a second job, carpooling to work, commuting long distances to work, and responsibilities at home.110
As noted above, management support and commitment can serve to reduce these structural barriers by placing high priority on a comprehensive program supporting worker health, with the same levels of support communicated for different groups of workers. Given the push to keep production moving, it may also be necessary to structure smoking cessation programs around the schedules of line workers, bring programs to production floors and break rooms, provide self-help and tailored strategies that do not depend on group attendance, or time programs to fit within the break times of workers. Intervention research is needed to identify effective strategies to reduce these barriers.
DISCUSSION
Growing disparities in tobacco use prevalence are a major challenge facing tobacco control efforts. Rates of tobacco use are especially elevated among some groups of workers, particularly those employed in blue-collar occupations. These workers are employed in settings generally less supportive of nonsmoking. For example, they also report a lower prevalence of restrictive smoking policies in worksites where they are employed111 and less assistance in quitting smoking from employers1 compared with the assistance reported by other workers.112 Health promotion programs are less available to workers with low education levels.113 Evidence also suggests that blue-collar workers are less likely to participate in worksite health promotion programs than are white-collar workers.79,114–118 When they do participate, they may be less successful in changing health behaviors than are their white-collar counterparts.119
We have proposed a social-contextual model for understanding the pathways by which socioeconomic position may influence disparities in tobacco use. We have illustrated the application of this conceptual model by examining the implications of the work experiences of blue-collar workers. Through a series of studies, we have expanded worksite tobacco control interventions to include 1 component of workers’ day-to-day experiences: exposures to occupational hazards. In the WellWorks-2 study, the integrated health promotion–occupational health and safety intervention resulted in a doubling of quit rates among blue-collar workers. According to estimates by Colditz, if this intervention were disseminated to the population of blue-collar smokers in Massachusetts, an estimated 2880 cases of lung cancer could be avoided, with additional benefits expected to accrue in other tobacco-related diseases.120
Our research to date has focused on testing the efficacy of this integrated approach. As discussed under Empirical Evidence in Support of the Model, several factors might account for the synergy between hazardous occupational exposures and tobacco control issues, such as workers’ exposure to job hazards and to cigarettes, workers’ sense of futility in addressing their own health behaviors while being exposed involuntarily to hazardous substances at work, and workers’ concerns that job-related health and safety issues may not be addressed by management. Future research may articulate the role and relative salience of each of these factors, thereby refining the basis for intervention approaches.
Broad adoption of an integrated approach to tobacco control, such as the approach tested in the WellWorks studies, must address key structural barriers. Given the complexity required for effective interventions, it becomes increasingly important that we build bridges across disciplines interested in worker health. Worksite tobacco control programs generally are offered separately from occupational health and safety efforts, usually within the context of health promotion programs. There is a need for synthesis, integration, and communication between separate training programs for health educators and occupational health and safety professionals, who seldom share curricula and intervention methodology.63,104,121
Research to develop effective intervention strategies integrating tobacco control and occupational health and safety also requires an interdisciplinary approach, with representation from occupational health and safety, behavioral and social sciences, organizational change, health promotion, labor education, and quantitative and qualitative methods.71,104,121 Experts in these areas are likely to read different journals, attend different professional meetings, and employ different research methodologies. Indeed, our diverse backgrounds have contributed to differing ideological approaches to and understanding of responsibility for worker health. Starting with the assumption that worker health begins with individual behavior change leads to a different set of intervention strategies than does starting with the assumption that management bears primary responsibility for worker health.71,121
Overcoming the segmentation of these fields ultimately will require a common model of work and health, which will provide for resolution—or at least understanding—of our different assumptions, vocabulary, research methods, and intervention approaches. Full implementation of these recommendations regarding intervention and research needed may also require changes in the ways that funders view tobacco control and occupational health. A comprehensive view of worker health would be supported by systematic funding of interdisciplinary, collaborative research and training.
The social-contextual model helps us frame new interventions in promising directions by targeting previously untargeted elements of the social context of the work setting to reduce tobacco use among blue-collar workers. We have articulated directions for future research based on the social-contextual model. This model provides a structure for examining the ways in which social-contextual factors help explain observed patterns of tobacco use. It is important that we understand workers’ resources, available social supports, and sources of social capital; social norms supporting tobacco use as well as those supporting nonsmoking; and the implications of daily stressors, competing role responsibilities, occupational exposures, and other pressures on the job. Through an understanding of these factors, we will be able to identify modifying conditions and mediating mechanisms that can be incorporated into intervention design. This research agenda needs to include the design and testing of interventions that aim to modify features in the social context; in addition, it is necessary to understand the patterns of social circumstance that occur with social disadvantage and to use this information to inform and improve intervention design.
To accomplish this research agenda, it will be necessary to deploy a broad range of research methodologies and designs, from hypothesis generation and methods development to dissemination research.122 The social-contextual model underlines the importance of formative research to understand the realities of people’s daily experiences—to illuminate the black box representing the pathways by which socioeconomic position influences tobacco use patterns. It is necessary that we incorporate qualitative methods to enrich the depth of our understanding and to explore uncharted territory.123,124 Observational studies may suggest new intervention directions as we observe the evolution of change.125 Targeted methods development studies are needed to provide the opportunity to refine interventions for specific populations and must lead to randomized trials.125–127 Durability and dissemination research is needed to identify ways to sustain interventions and maximize their impact through wide-scale adoption.128
The social-contextual model provides a useful framework for enhancing interventions aimed at reducing socioeconomic disparities, and it can be applied to other sources of disparity and within other settings. For example, the Harvard Cancer Prevention Program Project is applying this model to cancer prevention interventions that target improvements in diet and physical activity with working-class, multiethnic populations through health centers as well as worksites.37 Future research is needed to test aspects of this model across a range of settings, such as schools, housing developments, and faith-based and other community organizations.
In summary, the social-contextual model provides a framework for incorporating into tobacco control interventions important lessons from social epidemiology about the pathways through which socioeconomic position may influence tobacco use. To reduce social disparities in tobacco use, we must disentangle the meaning of socioeconomic position; we must translate occupation into the ways it shapes everyday experiences on and off the job. With broadened understanding of blue-collar workers’ social context and an appreciation of their available assets and resources, it will be possible to identify new intervention opportunities and methods to enhance the efficacy of existing intervention approaches.
Acknowledgments
This work was supported by grants from the National Cancer Institute (5 R01 CA68087 and 5 P01 CA75308) and the Liberty Mutual Insurance Group.
The authors thank co-investigators Anne Stoddard and Lisa Berkman for their input on an earlier draft of this article. We also appreciate the participation of the worksites taking part in the WellWorks-2 study and the long-term input of our research team: David Christiani, Candance Combe, Elizabeth Harden, Kerry Kokkinogenis, Ruth Lederman, Anthony LaMontagne, Marvin Lewiton, Deborah McLellan, Melissa Perry, Natania Remba, Lorraine Wallace, and Richard Youngstrom.
Contributors G. Sorensen provided overall direction to the studies’ design and implementation and prepared the first draft of the article. E. Barbeau, M. K. Hunt, and K. Emmons were coinvestigators and assisted in preparing the article.
Peer Reviewed
References
- 1.Giovino G, Pederson L, Trosclair A. The prevalence of selected cigarette smoking behaviors by occupation in the United States. In: Work, Smoking and Health: A NIOSH Scientific Workshop. Washington, DC: Centers for Disease Control and Prevention; 2000:22–31. Also available at: http://www.cdc.gov/niosh/docs/2002-148/2002-148pd.html. Accessed November 25, 2003.
- 2.Nelson DE, Emont SL, Brackbill RM, Cameron LL, Peddicord J, Fiore MC. Cigarette smoking prevalence by occupation in the United States. J Occup Environ Med. 1994;36:516–525. [PubMed] [Google Scholar]
- 3.Barbeau E, Krieger N, Soobader M. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health. 2004;94:269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freudenberg N. Time for a national agenda to improve the health of urban populations [editorial]. Am J Public Health. 2000;90:837–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Graham H. Promoting health against inequality: using research to identify targets for intervention—a case study of women and smoking. Health Educ J. 1998;57:292–302. [Google Scholar]
- 6.Kaplan GA. Where do shared pathways lead? Some reflections on a research agenda. Psychosom Med. 1995;57:208–212. [DOI] [PubMed] [Google Scholar]
- 7.Graham H. When Life’s a Drag: Women, Smoking and Disadvantage. London, England: Dept of Health, University of Warwick; 1994.
- 8.Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: W. H. Freeman & Co; 1997.
- 9.Glanz K, Lewis FM, Rimer B, eds. Health Behavior Health Education: Theory, Research, and Practice. San Francisco, Calif: Jossey-Bass; 1990.
- 10.Prochaska JO, Redding C, Evers K. The transtheoretical model and stages of change. In: Glanz K, Lewis FM, Rimer BK, eds. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, Calif: Jossey-Bass; 1997:60–84.
- 11.Berkman LF, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press; 2000.
- 12.Krieger N. Epidemiology and the web of causation: has anyone seen the spider? Soc Sci Med. 1994;39:887–903. [DOI] [PubMed] [Google Scholar]
- 13.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol. 2001;30:668–677. [DOI] [PubMed] [Google Scholar]
- 14.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. [DOI] [PubMed] [Google Scholar]
- 15.Amick BC, Levine S, Tarlov AR, Walsh DC, eds. Society and Health. Oxford, England: Oxford University Press; 1995.
- 16.Eriksen MP, Gottlieb NH. A review of the health impact of smoking control at the workplace. Am J Health Promot. 1998;13:83–104. [DOI] [PubMed] [Google Scholar]
- 17.Warner KE. The need for, and value of, a multi-level approach to disease prevention: the case of tobacco control. In: Smedley BD, Syme SL, eds. Promoting Health: Intervention Strategies From Social and Behavioral Research. Washington, DC: National Academy Press; 2000:417–449.
- 18.McLeroy K, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. [DOI] [PubMed] [Google Scholar]
- 19.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10:282–298. [DOI] [PubMed] [Google Scholar]
- 20.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. [DOI] [PubMed] [Google Scholar]
- 21.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986.
- 22.Bandura A. Self-efficacy mechanism in psychological activation and health-promoting behavior. In: Madden J, ed. Neurobiology of Learning, Emotion and Affect. New York, NY: Raven; 1991.
- 23.Bandura A. Social cognitive theory and exercise of control over HIV infection. In: DiClemente RJ, Peterson JL, eds. Preventing AIDS: Theories and Methods of Behavioral Interventions. New York, NY: Plenum Press; 1994.
- 24.Fishbein M, Ajzen I. Belief, Attitude, Intention and Behavior: An Introduction to Theory and Research. Reading, Mass: Addison-Wesley; 1975.
- 25.Fishbein M, Middlestadt SE, Hitchcock PJ. Using information to change sexually transmitted disease-related behaviors: an analysis based on the theory of reasoned action. In: Wasserheit JN, Aral SO, Holmes KK, eds. Research Issues in Human Behavior and Sexually Transmitted Diseases in the AIDS Era. Washington, DC: American Society for Microbiology; 1991:243–257.
- 26.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice Hall; 1980.
- 27.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. [DOI] [PubMed] [Google Scholar]
- 28.Prochaska JO, DiClemente CC. Toward a comprehensive model of change. In: Miller WR, Neather N, eds. Treating Addictive Behaviors: Processes of Change. New York, NY: Plenum Press; 1986.
- 29.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: applications to addictive behaviors. Am Psychol. 1992;47:1102–1114. [DOI] [PubMed] [Google Scholar]
- 30.Prochaska JO, Redding CA, Harlow LL. The transtheoretical model of change and HIV prevention: a review. Health Educ Q. 1994;21:471–486. [DOI] [PubMed] [Google Scholar]
- 31.Rosenstock IM, Kirscht JP. The health belief model and personal health behavior. Health Educ Monogr. 1974;2:354–386. [Google Scholar]
- 32.Fiore MC, Bailey WC, Cohen SJ, et al. Clinical Practice Guideline: Treating Tobacco Use and Dependence. Rockville, Md: Public Health Service; 2000.
- 33.Women and Smoking: A Report of the Surgeon General. Rockville, Md: Public Health Service, Office of the Surgeon General; 2001.
- 34.House JS, Williams DR. Understanding and reducing socioeconomic and racial/ethnic disparities in health. In: Smedley BD, Syme SL, eds. Promoting Health: Intervention Strategies From Social and Behavioral Research. Washington, DC: National Academy Press; 2000:81–124. [PubMed]
- 35.Marmot MG, Davey-Smith G, Stansfeld S, et al. Health inequities among British civil servants: the Whitehall II Study. Lancet. 1991;337:1387–1393. [DOI] [PubMed] [Google Scholar]
- 36.Kaplan GA, Everson SA, Lynch JW. The contribution of social and behavioral research to an understanding of the distribution of disease: a multilevel approach. In: Smedley BD, Syme SL, eds. Promoting Health: Intervention Strategies From Social and Behavioral Research. Washington, DC: National Academy Press; 2000:37–80.
- 37.Sorensen G, Emmons K, Hunt MK, et al. A model for incorporating the social context in health behavior interventions: applications for cancer prevention for working-class, multiethnic populations. Prev Med. 2003;37:188–197. [DOI] [PubMed] [Google Scholar]
- 38.Sallis JF, Owen N. Ecological models of health behavior. In: Glanz K, Rimer BK, Lewis FM, eds. Health Behavior and Health Education: Theory, Research and Practice. 3rd ed. San Francisco, Calif: Jossey-Bass; 2002:462–484.
- 39.McKinlay JB. The promotion of health through planned sociopolitical change: challenges for research and policy. Soc Sci Med. 1993;36:109–117. [DOI] [PubMed] [Google Scholar]
- 40.Glassman AH, Helzer JE, Covey LS, et al. Smoking, smoking cessation, and major depression. JAMA. 1990;264:1583–1584. [PubMed] [Google Scholar]
- 41.Covey LS, Glassman AH, Stetner F. Cigarette smoking and major depression. J Addict Dis. 1998;17:35–46. [DOI] [PubMed] [Google Scholar]
- 42.Pomerleau CS, Zucker AN, Stewart AJ. Patterns of depressive symptomatology in women smokers, ex-smokers, and never smokers. Addict Behav. 2003;28:575–582. [DOI] [PubMed] [Google Scholar]
- 43.French SA, Perry CL. Smoking among adolescent girls: prevalence and etiology. J Am Med Womens Assoc. 1996;51:25–28. [PubMed] [Google Scholar]
- 44.Perry CL, Murray DM, Klepp KI. Predictors of adolescent smoking and implications for prevention. MMWR Morb Mortal Wkly Rep. 1987;36(suppl 4):41S–47S. [PubMed] [Google Scholar]
- 45.McGee R, Stanton WR. A longitudinal study of reasons for smoking in adolescence. Addiction. 1993;88:265–271. [DOI] [PubMed] [Google Scholar]
- 46.Preventing Tobacco Use Among Young People: A Report of the Surgeon General. Atlanta, Ga: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994.
- 47.Cohen S, Lichtenstein E. Partner behaviors and support for quitting smoking. J Consult Clin Psychol. 1990;58:304–309. [DOI] [PubMed] [Google Scholar]
- 48.Sorensen G, Emmons K, Stoddard AM, Linnan L, Avrunin J. Do social influences contribute to occupational differences in smoking behaviors? Am J Health Promot. 2002;16:135–141. [DOI] [PubMed] [Google Scholar]
- 49.Johnson JV. Collective control: strategies for survival in the workplace. Int J Health Serv. 1989;19:469–480. [DOI] [PubMed] [Google Scholar]
- 50.Nelkin D, Brown MS. Workers and Risk. Chicago, Ill: University of Chicago Press; 1984.
- 51.Eakin JM. Work-related determinants of health behavior. In: Gochman DS. Institutional and Cultural Determinants. New York, NY: Plenum Press; 1997.
- 52.Mullen K. A question of balance: health behaviour and work context among male Glaswegians. Sociol Health Illn. 1992;14:73–97. [Google Scholar]
- 53.Johansson G, Johnson JV, Hall EM. Smoking and sedentary behavior as related to work organization. Soc Sci Med. 1991;32:837–846. [DOI] [PubMed] [Google Scholar]
- 54.Landsbergis PA, Schnall PL, Deitz DK, Warren K, Pickering TG, Schwartz JE. Job strain and health behaviors: results of a prospective study. Am J Health Promot. 1998;12:237–245. [DOI] [PubMed] [Google Scholar]
- 55.Kalimo R. Psychosocial factors and workers’ health: an overview. In: Kalimo R, El-Batawi RMA, Cooper CL, eds. Psychosocial Factors at Work and Their Relation to Health. Geneva, Switzerland: World Health Organization; 1987.
- 56.Green KL, Johnson JV. The effect of psychological work organization on patterns of cigarette smoking among male chemical plant employees. Am J Public Health. 1990;80:1368–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Caplan RD, Cobb S, French JRP, Harrison RV, Pinneau SR. Job Demands and Worker Health. Washington, DC: National Institute for Occupational Safety and Health; 1975. NIOSH publication 75–168.
- 58.Marmot M, Theorell T. Social class and cardiovascular disease: the contribution of work. In: Johnson J, Johansson G, eds. The Psychosocial Work Environment: Work Organization, Democratization and Health. Amityville, NY: Baywood Publishing Co; 1991:21–48.
- 59.Karasek R, Gardell B, Lindell J. Work and non-work correlates of illness and behaviour in male and female Swedish white-collar workers. J Occup Behav. 1987;8:187–207. [Google Scholar]
- 60.Laws MB, Whitman J, Bowser D, Krech L. Tobacco availability and point of sale marketing in demographically contrasting districts of Massachusetts. Tob Control. 2002;11(suppl 2):ii71–ii73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reynolds RJ. Analysis of the virile segment. 1986. Bates No. 505923292–3295. Available at: http://legacy.library.ucsf.edu/tid/iqd94d00. Accessed February 18, 2003.
- 62.Glasgow RE, Terborg JR, Hollis JF, Severson HH, Boles SM. Take heart: results from the initial phase of a work-site wellness program. Am J Public Health. 1995;85:207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sorensen G, Himmelstein JS, Hunt MK, et al. A model for worksite cancer prevention: integration of health protection and health promotion in the WellWorks project. Am J Health Promot. 1995;10:55–62. [DOI] [PubMed] [Google Scholar]
- 64.Klesges RC, Cigrant JA. Worksite smoking cessation programs: clinical and methodological issues. In: Hersen M, Eisler RM, Miller RM, eds. Progress in Behavioral Modification. Newbury Park, Calif: Sage Publications; 1988:37–61. [PubMed]
- 65.Abrams DB, Boutwell WB, Grizzle J, Heimendinger J, Sorensen G, Varnes J. Cancer control at the workplace: the Working Well trial. Prev Med. 1994;23:1–13. [DOI] [PubMed] [Google Scholar]
- 66.Emmons K. Behavioral and social science contributions to the health of adults in the United States. In: Smedley BD, Syme SL, eds. Promoting Health: Intervention Strategies From Social and Behavioral Research. Washington, DC: Institute of Medicine; 2001:254–321.
- 67.Pelletier KR. A Review and analysis of the clinical- and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: 1998–2000 update. Am J Health Promot. 2001;16:107–116. [DOI] [PubMed] [Google Scholar]
- 68.Bureau of Labor Statistics, US Dept of Labor. Injuries, illnesses, and fatalities. Available at: http://www.bls.gov/iif/home.htm#tables. Accessed March 26, 2003.
- 69.Walsh DC, Jennings SE, Mangione T, Merrigan DM. Health promotion versus health protection? Employees’ perceptions and concerns. J Public Health Policy. 1991;12:148–164. [PubMed] [Google Scholar]
- 70.Sorensen G, Stoddard A, Hammond SK, Hebert JR, Ocklene JK. Double jeopardy: job and personal risks for craftspersons and laborers. Am J Health Promot. 1996;10:355–363. [DOI] [PubMed] [Google Scholar]
- 71.Sorensen G. Worksite tobacco control programs: the role of occupational health. Respir Physiol. 2001;189:89–102. [DOI] [PubMed] [Google Scholar]
- 72.Adverse Effects of Smoking and the Occupational Environment. Bethesda, Md: US Dept of Health and Human Services, National Institute for Occupational Safety and Health; 1979.
- 73.Youngstrom R. Unions and tobacco control. New Solutions. 1996;6:51–56. [DOI] [PubMed] [Google Scholar]
- 74.Green KL. Issues of control and responsibility in worker’s health. Health Educ Q. 1988;15:473–486. [DOI] [PubMed] [Google Scholar]
- 75.Barnard C. The Functions of the Executive. Cambridge, Mass: Harvard University Press; 1968.
- 76.Baker F. Risk communication about environmental hazards. J Public Health Policy. 1990;11:341–359. [PubMed] [Google Scholar]
- 77.Fischoff B, Bostrom A, Quadrel MJ. Risk perception and communication. Annu Rev Health. 1993;14:183–200. [DOI] [PubMed] [Google Scholar]
- 78.Bradbury JA. The policy implications of differing concepts of risk. Sci Technol Hum Values. 1989;14:381–396. [Google Scholar]
- 79.Morris W, Conrad K, Marcantonio R, Marks B, Ribisl K. Do blue-collar workers perceive the worksite health climate differently than white-collar workers? J Health Promot. 1999;13:319–324. [DOI] [PubMed] [Google Scholar]
- 80.Warshaw LJ, Messite J. Health protection and promotion in the workplace: an Overview. In: Stellman JM, ed. Encyclopaedia of Occupational Health and Safety. Geneva, Switzerland: International Labor Organization Publications; 1998:79–89.
- 81.Sorensen G, Stoddard A, Hunt MK, et al. Effects of a health promotion–health protection intervention on behavior change: the WellWorks study. Am J Public Health. 1998;88:1685–1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chu C, Driscoll T, Dwyer S. The health-promoting workplace: an integrative perspective. Aust N Z J Public Health. 1997;21:377–385. [DOI] [PubMed] [Google Scholar]
- 83.DeJoy D, Southern D. An integrative perspective on work-site health promotion. J Occup Med. 1993;35:1221–1230. [PubMed] [Google Scholar]
- 84.Baker E, Israel B, Schurman S. The integrated model: implications for worksite health promotion and occupational health and safety practice. Health Educ Q. 1996;23:175–188. [DOI] [PubMed] [Google Scholar]
- 85.Blewett V, Shaw A. Health promotion, handle with care: issues for health promotion in the workplace. J Occup Health Safety. 1995;11:461–465. [Google Scholar]
- 86.Robins T, Klitzman S. Hazard communication in a large US manufacturing firm: the ecology of health education in the workplace. Health Educ Q. 1988;15:451–472. [DOI] [PubMed] [Google Scholar]
- 87.NIOSH Program Plan by Program Areas for Fiscal Years 1984–89. Rockville, Md: Centers for Disease Control, National Institute for Occupational Safety and Health; 1984.
- 88.Maes S, Verhoeven C, Kittel F, Scholten H. Effects of a Dutch worksite wellness-health program: the Brabantia project. Am J Public Health. 1998;88:1037–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Marcus AC, Baker DB, Froines J. The ICWU cancer control and evaluation program: research design and needs assessment. J Occup Med. 1986;28:226–236. [PubMed] [Google Scholar]
- 90.Schenck A, Thomas R, Hochbaum G, Beliczky L. A labor and industry focus on education: using baseline survey data in program design. Health Educ Res. 1987;2:33–44. [Google Scholar]
- 91.Roter DL, Rudd RE, Keogh J, Robinson B. Worker produced health education material for the construction trades. Int Q Community Health Educ. 1986;7:109–117. [DOI] [PubMed] [Google Scholar]
- 92.Sorensen G, Thompson B, Glanz K, et al. Working Well: results from a worksite-based cancer prevention trial. Am J Public Health. 1996;86:939–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sorensen G, Stoddard A, LaMontagne A, et al. A comprehensive worksite cancer prevention intervention: behavior change results from a randomized controlled trial in manufacturing worksites (United States). Cancer Causes Control. 2002;13:493–502. [DOI] [PubMed] [Google Scholar]
- 94.O’Donnell M, Bishop C, Kaplan K. Benchmarking best practices in workplace health promotion programs. Art Health Promot. 1997;1:1–8. [Google Scholar]
- 95.Emmons KM, Thompson B, Sorensen G, et al. The relationship between organizational characteristics and the adoption of workplace smoking policies. Health Educ Behav. 2000;27:483–501. [DOI] [PubMed] [Google Scholar]
- 96.Allen JR. Building supportive cultural environments. In: O’Donnell MP, ed. Health Promotion in the Workplace. 3rd ed. Albany, NY: Delmar Thomson Learning; 2002:202–217.
- 97.Emmons KM. Behavioral and social science contributions to the health of adults in the United States. In: Smedley BD, Syme L, eds. Promoting Health: Intervention Strategies From Social and Behavioral Research. Washington, DC: Institute of Medicine, National Academy Press; 2000:254–321.
- 98.Sorensen G, Stoddard A, Youngstrom R, et al. Local labor unions’ positions on worksite tobacco control. Am J Public Health. 2000;90:618–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Barbeau E, Li Y, Sorensen G, Conlan K, Youngstrom R, Emmons K. Coverage of smoking cessation treatment by union health and welfare funds. Am J Public Health. 2001;91:1412–1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Siqueira CE, Youngstrom R, Barbeau E, Levenstein C, Sorensen G. Worksite tobacco control policies and labor-management cooperation and conflict in New York state. New Solutions. In press. [DOI] [PubMed]
- 101.Knutsson A, Nilsson T. Tobacco use and exposure to environmental tobacco smoke in relation to certain work characteristics. Scand J Soc Med. 1998;26:183–189. [DOI] [PubMed] [Google Scholar]
- 102.Karasek R, Theorell T. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life. New York, NY: Basic Books; 1990.
- 103.Johnson JV, Hall EM. Job strain, workplace social support, and cardiovascular ease: a cross-sectional study of a random sample of Swedish working population. Am J Public Health. 1988;78:483–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Israel B, Baker E, Goldenhar L, Heaney C, Schurman S. Occupational stress, safety, and health: conceptual framework and principals for effective prevention interventions. J Occup Health Psychol. 1996;1:261–286. [DOI] [PubMed] [Google Scholar]
- 105.Landsbergis PA, Cahill J. Labor union programs to reduce or prevent occupational stress in the United States. Int J Health Serv. 1994;24:105–129. [DOI] [PubMed] [Google Scholar]
- 106.Gottlieb N, Nelson A. A systematic effort to reduce smoking at the worksite. Health Educ Q. 1990;17:99–118. [DOI] [PubMed] [Google Scholar]
- 107.DeVries H, Lechner L. Motives for protective behavior against carcinogenic substances in the workplace: a pilot study among Dutch workers. J Occup Environ Med. 2000;42:88–95. [DOI] [PubMed] [Google Scholar]
- 108.Stokols D, Pelletier K, Fielding J. The ecology of work and health: research and policy directions for the promotion of employee health. Health Educ Q. 1996;23:137–158. [DOI] [PubMed] [Google Scholar]
- 109.Linnan LA, Sorensen G, Colditz G, Klar N, Emmons K. Using theory to understand the multiple determinants of low participation in worksite health promotion programs. Health Educ Behav. 2001;28:591–607. [DOI] [PubMed] [Google Scholar]
- 110.Alexy B. Workplace health Promotion and the blue-collar worker. Am Assoc Occup Health Nurses J. 1990;38:12–16. [PubMed] [Google Scholar]
- 111.Gerlach K, Shopland D, Hartman A, Gibson J, Pechacek T. Workplace smoking policies in the United States: results from a national survey of more than 100,000 workers. Tob Control. 1997;6:199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Holman D, Corti B, Donovan R, Jalleh G. Association of the health-promoting workplace with trade unionism and other industrial factors. Am J Health Promot. 1998;12:325–334. [DOI] [PubMed] [Google Scholar]
- 113.Grosch J, Alterman T, Petersen M, Murphy L. Worksite health promotion programs in the US: factors associated with availability and participation. Am J Health Promot. 1998;13:36–45. [DOI] [PubMed] [Google Scholar]
- 114.Sorensen G, Stoddard A, Ockene JK, Hunt MK, Youngstrom R. Worker participation in an integrated health promotion/health protection program: results from the WellWorks Project. Health Educ Q. 1996;23:191–203. [DOI] [PubMed] [Google Scholar]
- 115.Erfurt J. The Wellness Outreach at Work Program: A Step-by-Step Guide. Washington, DC: National Institutes of Health; 1995.
- 116.Conrad P. Wellness in the work place: Potentials and pitfalls of work-site health promotion. Milbank Q. 1987;65:255–275. [PubMed] [Google Scholar]
- 117.Gebhardt DL, Crump C. Employee fitness and wellness programs in the workplace. Am Psychol. 1990;45:262–272. [DOI] [PubMed] [Google Scholar]
- 118.Glasgow RE, McCaul KD, Fisher KJ. Participation in worksite health promotion: a critique of the source. Health Educ Q. 1993;20:391–408. [DOI] [PubMed] [Google Scholar]
- 119.Niknian M, Linnan LA, Lasater TM, Carleton RA. Use of population-based data to assess risk factor profiles of blue- and white-collar workers. J Occup Med. 1991;33:29–36. [DOI] [PubMed] [Google Scholar]
- 120.Colditz G. Disseminating research findings into public health practice [editorial]. Cancer Causes Control. 2002;13:503–504. [DOI] [PubMed] [Google Scholar]
- 121.Sorensen G. Smoking cessation at the worksite: what works and what is the role of occupational health? In: Work, Smoking, and Health, A NIOSH Scientific Workshop: June 15–16, 2000; Washington, DC. Cincinnati, Ohio: Public Health Service, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2002:99–120. DHHS (NIOSH) publication 2002-148.
- 122.Sorensen G, Emmons K, Hunt MK, Johnston D. Implications of the results of community intervention trials. Annu Rev Public Health. 1998;19:379–416. [DOI] [PubMed] [Google Scholar]
- 123.Fortmann SP, Floa JA, Winkleby MA, Schooler C, Barr Taylor C, Farquhar JW. Community intervention trials: reflections on the Stanford Five-City project experience. Am J Epidemiol. 1995;142:576–586. [DOI] [PubMed] [Google Scholar]
- 124.McKinlay J. The new public health approach to improving physical activity and autonomy in older populations. In: Heikkinon E, ed. Preparation for Aging. New York, NY: Plenum Press; 1995:87–103.
- 125.Susser M. The tribulations of trials—intervention in communities [editorial]. Am J Public Health. 1995;85:156–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Fisher EB. The results of the COMMIT trial. Community intervention trial for smoking cessation [editorial]. Am J Public Health. 1995;85:159–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Winkleby MA. The future of community-based cardiovascular disease intervention studies. Am J Public Health. 1994;84:1369–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sorensen G, Thompson B, Basen-Engquist K, et al. Durability, dissemination, and institutionalization of worksite tobacco control programs: results from the Working Well trial. Int J Behav Med. 1998;5:335–351. [DOI] [PubMed] [Google Scholar]