Abstract
Objectives. Our study presents national estimates of the proportion of youths in each of 7 stages of smoking and investigates the associations between risk/protective factors and progression to established smoking.
Methods. We analyzed data from the 1999 and 2000 National Youth Tobacco Surveys.
Results. In 1999 and 2000, 48.6% of US adolescents had at least experimented with tobacco, and 7.8% were established smokers. Important correlates of progression to established smoking included parental advice not to smoke, antismoking lessons in school, susceptibility to tobacco industry advertising and promotion, peer smoking, and exposure to smoking at home.
Conclusions. Interventions to stop adolescent progression to established smoking should target susceptible never smokers and early experimenters as well as those in later stages of smoking.
Despite the decline in adolescent smoking from 1970 to 1984,1 adolescent smoking prevalence in the United States increased during the 1990s. The Youth Risk Behavior Survey estimated the prevalence of past-30-day smoking among US high school students increased from 27.5% to 34.8% between 1991 and 2000.2 Results from the Monitoring the Future Study show a rapid increase in prevalence between 1991 and 1997, which was followed by a dramatic decline in prevalence between 1997 and 2002.3 Although the 2002 prevalence of 26.7% among high school seniors is the lowest high school senior prevalence ever measured in the Monitoring the Future Study, the fact that more than 25% of all high school seniors had smoked during the 30 days preceding the survey represents a huge potential source of addicted adult smokers.
The model that we used for assessing progression toward established smoking is based on work by Leventhal and Cleary4 and Flay.5 Leventhal and Cleary describe the process of smoking onset as occurring in 4 distinct stages: (1) preparation, (2) initiation, (3) becoming a smoker, and (4) maintenance of smoking. Progression through these stages occurs over a period of 1 or more years. In the preparation stage, the nonsmoker begins to develop a self-image of being a smoker and forms ideas and beliefs about the utility of smoking. Initiation is defined as the first few tries. During the becoming a smoker stage, there is a gradual increase in the frequency of smoking, and persons smoke in an increasing variety of situations. During the maintenance of smoking stage, smoking is a part of self-regulation in a variety of situations, and smoking is used for a number of purposes that include pleasure, relaxation, and anxiety reduction. Flay5 divides the maintenance stage into regular use (e.g., smoking every day before school or smoking every weekend), and addiction. Nicotine addiction is associated with compulsive smoking, cravings during periods of abstinence from use of tobacco, difficulty quitting smoking, and tolerance to increasing doses of nicotine.6
In order to estimate from epidemiological data the numbers of youths in each stage of smoking, we adapted the above scheme as follows. First, we needed a stage for those nonsmokers who were not in the preparation stage. This stage is called not open to smoking. Nonsmokers in the preparation stage are characterized as open to smoking. Second, because the National Youth Tobacco Survey instrument did not measure the precise definition of initiation as described by Leventhal and Cleary4 and Flay,5 the initiation and becoming a smoker stages were slightly modified into 2 stages that we call early experimenters and late experimenters. Third, for consistency with other epidemiological studies, we needed a definition of current smoking. To accomplish this, the regular use and addiction stages described by Flay5 were modified into 2 stages: nondaily current smoker and established smoker. Finally, we needed to account for youths who had progressed through the becoming a smoker stage but who were not smoking at the time of interview. We call them former smokers.
Experimentation with smoking occurs primarily during adolescence.7 Since the 1970s, the average age of first trying a cigarette and the average age of smoking daily has decreased. By the 1990s, few people began smoking regularly after 20 years of age.7 Recognizing this, public health workers and educators have targeted prevention programs at increasingly younger persons. It is generally agreed that effective prevention requires a comprehensive set of conditions, including education, the promotion of social norms that promote not smoking, a reduction in smoking among peers and family members, and reductions in tobacco advertising and promotion targeted at young people.7–10
Our study presents national estimates of the prevalence of adolescents in each stage of progression to established smoking by age, race/ethnicity, and gender. Additionally, we explore selected risk and protective factors associated with progression to established smoking.
METHODS
Data Sources
We used data from the National Youth Tobacco Surveys (NYTS) conducted in middle schools and high schools during the fall of 1999 and the spring of 2000.11 The 1999 and 2000 NYTS were school-based, anonymous, self-administered pencil and paper questionnaires that included questions about tobacco use, exposure to environmental tobacco smoke, minors’ ability to purchase or otherwise obtain tobacco products, knowledge and attitudes about tobacco, and familiarity with pro- and anti-tobacco media messages. For the 1999 NYTS, 15 058 students in 131 schools completed questionnaires; for the 2000 NYTS, 35 828 students in 324 schools completed questionnaires. For both years, the school response rate was 90% and the student response rate was 93%, which resulted in an overall response rate of 84%.
Measures of Progression to Established Smoking
We defined 7 mutually exclusive categories to describe the stages of smoking uptake that were adapted from previous research on progression to established smoking.12 Never smokers are classified as being open to smoking or not open to smoking. They are considered to be open to smoking if they have not made a firm decision to not smoke a cigarette in the near future. Three questions, which were identically worded in the 1999 and 2000 NYTS, are used to evaluate openness to smoking: (1) “Do you think that you will try a cigarette soon?” (2) “Do you think you will smoke a cigarette anytime during the next year?” and (3) “If 1 of your best friends offered you a cigarette, would you smoke it?” Students who answered “no” to the first question and “definitely not” to the second and third questions are classified as not open to smoking. Students are classified as open to smoking if they provide any other responses to any of the 3 questions.
Experimenters are adolescents who have tried a cigarette but have smoked fewer than 100 cigarettes. We further classify experimenters as either early experimenters or late experimenters on the basis of the number of cigarettes they have ever smoked. Early experimenters have tried smoking (at least 1 puff) but have smoked no more than 25 cigarettes. Late experimenters have smoked 26 to 99 cigarettes. Students who have smoked 100 or more cigarettes but have not smoked in the past 30 days are classified as former smokers.
Current smokers who have progressed beyond experimentation (smoked at least 100 cigarettes) are further classified as either nondaily smokers or established smokers on the basis of their smoking behavior in the 30 days preceding the survey. Nondaily smokers are persons who have smoked more than 100 cigarettes in their lifetime and have smoked on 1 to 19 of the past 30 days, and established smokers are persons who have smoked more than 100 cigarettes in their lifetime and have smoked on at least 20 of the past 30 days.
Measurement of Risk and Protective Factors Associated with Progression to Established Smoking
The 2000 NYTS included questions about the respondent’s home and school environment. The question “Have either of your parents (or guardians) told you not to smoke cigarettes in the past 12 months?” was used to assess parental advice not to smoke. The NYTS included 4 questions about students’ exposure to smoking-prevention education lessons: (1) “During this school year, did you practice ways to say ‘no’ to tobacco in any of your classes (for example, by role playing)?” (2) During this school year, were you taught in any of your classes the reasons why people your age smoke?” (3) “During this school year, were you taught in any of your classes that most people your age do not smoke cigarettes?” and (4) “During this school year, were you taught in any of your classes about the effects of smoking, like it makes your teeth yellow, causes wrinkles, or makes you smell bad?” Students who answered “yes” to at least 3 of the 4 questions are considered to have been exposed to a multistrategy approach to smoking-prevention education. We evaluated exposure to antismoking advertising with 2 questions: “During the past 30 days, about how often have you seen antismoking commercials on TV or heard them on the radio?” and “During the past 30 days, about how often have you seen antismoking messages on billboards or outdoor signs”? Students who had seen or heard antismoking commercials 1 or more times in the past 30 days were classified as exposed to countersmoking advertising.
The 2000 NYTS instrument included questions about tobacco company promotional items, such as sports gear, T-shirts, lighters, hats, jackets, and sunglasses, that are given away or are sold by tobacco companies. Students were asked, “During the past 12 months, did you buy or receive anything that has a tobacco company name or picture on it?” Another question was, “Would you ever use or wear something that has a tobacco company name or picture on it, such as a lighter, T-shirt, hat, or sunglasses?” Students who responded “definitely yes” or “probably yes” were considered to be open to using or wearing a tobacco promotional item.
Students also were asked about the smoking habits of others in their households via the question, “Besides yourself, does anyone who lives in your home smoke cigarettes now?” Finally, we evaluated the effect of having friends who smoke with the question, “How many of your 4 closest friends smoke cigarettes?” Students who indicated that 1 or more close friends smoke were considered to be in the risk category for this factor.
Statistical Analysis
Responses were weighted to adjust for nonresponse and unequal sampling probabilities. We analyzed the data with SUDAAN 7.0 software (Research Triangle Institute, Research Triangle Park, NC), which takes the complex sampling design and the unequal weighting of responses into account when calculating standard errors for prevalence estimates. We used logistic regression models to analyze the 2000 NYTS data and identified factors associated with stage of smoking uptake. The models were fit with 2 different outcomes: (1) open to smoking among all never smokers, and (2) established smoking among all youths. We analyzed middle school and high school groups separately. The high school group regression models contained the same variables used in the middle school group models with the exception of the “smoking-prevention education lessons” variable. This variable is included in the younger age group models only, because these prevention lessons are most common in middle school.
The 1999 and 2000 NYTS questionnaires were not identical; however, we restricted our analysis of combined 1999 and 2000 NYTS data to a limited subset of items that are common to both questionnaires. Records that contained conflicting or incomplete responses to the questions used to determine smoking status are not included in our analysis. Respondents who described themselves as a race/ethnicity other than Black or African American, Hispanic or Latino, Asian, or White were excluded from the logistic regression analysis. Population projections from the US Census Bureau were used to estimate the number of adolescent established smokers in the US population by age group.
RESULTS
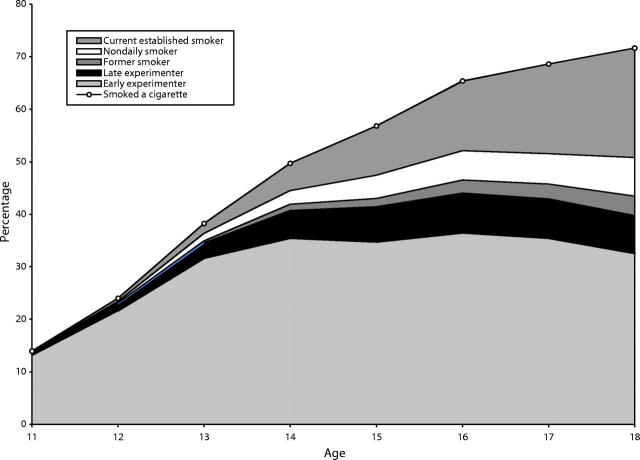
Table 1 ▶ and Figure 1 ▶ show the estimated percentages of US adolescents aged 11 to 18 years in each stage of smoking uptake. Progression to established smoking is strongly associated with age. Only a few of the 11-year-old students had initiated established smoking, while approximately 21% of adolescents aged 18 years were established smokers in 1999 and 2000. Approximately 51% of the US population aged 11 to 18 years had at least tried smoking, and the majority of them were early experimenters.
TABLE 1—
Percentage Distribution of Open to Smoking and Established Smoking Among Youths, by Age, Race/Ethnicity, and Gender: Combined 1999 and 2000 National Youth Tobacco Surveys
| Smoking Stage | ||||||||
| Respondents, No. | Never Smoker, Not Open to Smoking (95% CI) | Never Smoker, Open to Smoking (95% CI) | Early Experimenter (95% CI) | Late Experimenter (95% CI) | Former Smoker (95% CI) | Nondaily Current Smoker (95% CI) | Established Smoker (95% CI) | |
| Age, y | ||||||||
| 11 | 3428 | 72.21 (69.85, 74.56) | 13.83 (12.59, 15.08) | 13.11 (10.99, 15.23) | 0.41 (0.14, 0.67) | 0.03 (0.00, 0.08) | 0.30 (0.00, 0.67) | 0.11 (0.00, 0.22) |
| 12 | 6952 | 58.34 (56.05, 60.62) | 17.64 (16.63, 18.66) | 21.65 (19.67, 23.62) | 1.31 (0.99, 1.63) | 0.15 (0.06, 0.25) | 0.31 (0.17, 0.45) | 0.60 (0.38, 0.82) |
| 13 | 7726 | 44.76 (42.75, 46.76) | 17.01 (15.83, 18.19) | 31.64 (29.71, 33.57) | 2.91 (2.42, 3.41) | 0.38 (0.20, 0.55) | 1.42 (1.06, 1.78) | 1.88 (1.48, 2.29) |
| 14 | 7097 | 35.62 (33.56, 37.68) | 14.71 (13.59, 15.82) | 35.47 (33.54, 37.40) | 5.25 (4.63, 5.87) | 1.20 (0.90, 1.50) | 2.58 (2.09, 3.08) | 5.17 (4.33, 6.01) |
| 15 | 6708 | 32.30 (30.11, 34.49) | 10.88 (9.97, 11.79) | 34.71 (32.99, 36.43) | 6.73 (6.02, 7.45) | 1.58 (1.24, 1.93) | 4.43 (3.85, 5.01) | 9.36 (8.09, 10.64) |
| 16 | 6352 | 27.12 (25.26, 28.97) | 7.52 (6.78, 8.26) | 36.48 (34.98, 37.99) | 7.53 (6.73, 8.34) | 2.52 (2.03, 3.02) | 5.56 (4.87, 6.25) | 13.26 (11.73, 14.79) |
| 17 | 6088 | 25.81 (24.07, 27.55) | 5.58 (4.97, 6.19) | 35.44 (33.72, 37.16) | 7.48 (6.68, 8.27) | 2.85 (2.37, 3.33) | 5.74 (5.04, 6.43) | 17.11 (15.40, 18.82) |
| 18 | 2746 | 22.99 (20.46, 25.52) | 5.37 (4.34, 6.40) | 32.58 (30.34, 34.82) | 7.15 (6.09, 8.21) | 3.73 (2.96, 4.50) | 7.33 (5.82, 8.83) | 20.85 (18.45, 23.25) |
| Race/ethnicity | ||||||||
| White | 27 166 | 39.89 (37.88, 41.90) | 11.87 (11.18, 12.56) | 27.31 (26.27, 28.36) | 5.40 (4.97, 5.83) | 1.74 (1.53, 1.96) | 3.98 (3.59, 4.36) | 9.81 (8.85, 10.76) |
| Black | 7667 | 37.67 (35.23, 40.10) | 11.84 (10.88, 12.81) | 42.04 (39.70, 44.38) | 3.29 (2.77, 3.81) | 0.70 (0.46, 0.94) | 1.22 (0.85, 1.60) | 3.24 (2.57, 3.90) |
| Hispanic | 8648 | 36.62 (34.05, 39.18) | 13.71 (12.75, 14.66) | 38.02 (36.04, 40.00) | 4.86 (4.15, 5.58) | 0.82 (0.59, 1.04) | 2.54 (2.00, 3.08) | 3.45 (2.67, 4.22) |
| Asian | 2133 | 49.41 (46.38, 52.43) | 13.91 (11.92, 15.89) | 24.92 (22.36, 27.48) | 2.40 (1.66, 3.13) | 1.04 (0.57, 1.52) | 2.36 (1.59, 3.13) | 5.97 (4.43, 7.51) |
| Other | 1483 | 32.89 (29.17, 36.61) | 12.18 (9.99, 14.37) | 36.21 (31.92, 40.50) | 5.78 (4.12, 7.45) | 1.57 (0.85, 2.29) | 3.04 (1.83, 4.25) | 8.32 (6.03, 10.62) |
| Gender | ||||||||
| Male | 23 437 | 37.97 (36.31, 39.63) | 11.92 (11.25, 12.58) | 31.29 (30.19, 32.39) | 5.05 (4.61, 5.48) | 1.72 (1.52, 1.92) | 3.79 (3.36, 4.22) | 8.28 (7.46, 9.09) |
| Female | 23 660 | 40.57 (38.83, 42.30) | 12.37 (11.70, 13.03) | 30.95 (29.63, 32.27) | 4.76 (4.37, 5.16) | 1.16 (0.96, 1.36) | 2.79 (2.47, 3.11) | 7.41 (6.53, 8.29) |
| Total | 47 097 | 39.28 (37.66, 40.89) | 12.14 (11.58, 12.70) | 31.12 (30.01, 32.22) | 4.91 (4.57, 5.25) | 1.44 (1.28, 1.60) | 3.28 (2.97, 3.60) | 7.84 (7.05, 8.63) |
Note: CI = confidence interval.
FIGURE 1—
Smoking stage distribution of US adolescents who had at least tried a cigarette, by age: 1999–2000 National Youth Tobacco Surveys.
Across all ages, about one quarter of all never smokers were open to smoking. The percentage of open to smoking among all never smokers increases with age until 14 years, at which time about 29% of never smokers were open to smoking. At older ages, the percentage open to smoking decreases to 19% of all 18-year-old never smokers.
The prevalences of smoking in the various stages of progression to established smoking differed by gender and by race/ethnicity. More males than females were established smokers, and the prevalence of never smokers was higher among females. The prevalence of established smokers was highest among White youths and was lowest among Black youths. In contrast, the percentage of never smokers who were open to smoking was highest among Hispanic youths and was lowest among White youths, which suggests that the probability of progressing to established smoking and the speed of the trajectory to established smoking may be different for youths of different race/ethnicities.
Correlates of Progression to Open to Smoking
Table 2 ▶ (students aged 11–14 years) and Table 3 ▶ (students aged 15–18 years) show adjusted odds ratios for the 7 self-reported risk and protective factors included in the logistic regression models. Odds ratios are adjusted for all other variables in the table. Age, gender, and race/ethnicity were all predictors of open to smoking among never smokers in both middle school and high school. Among both middle school and high school students, being receptive to tobacco industry promotions and having friends who smoke were associated with being open to smoking. Among younger adolescents, exposure to smoking-prevention classes in school and parental advice not to smoke were protective of open to smoking. However, parental advice was not a significant predictor of open to smoking among older youths. For youths of all ages, exposure to smoking at home and exposure to countertobacco advertising during the 30 days preceding the survey were not significantly associated with being open to smoking.
TABLE 2—
Adjusted Odds Ratios for Smoking Stage Among US Adolescents Aged 11 to 14 Years, by Survey Response: 2000 National Youth Tobacco Survey
| Never Smokers, Open to Smoking a Odds Ratio (95% Confidence Interval) | Established Smokersb Odds Ratio (95% Confidence Interval) | |
| Age, y | ||
| 11–12 | Reference | Reference |
| 13 | 1.27 (1.11, 1.46) | 1.94 (1.26, 2.99) |
| 14 | 1.26 (1.07, 1.48) | 4.75 (2.98, 7.57) |
| Gender | ||
| Male | Reference | Reference |
| Female | 1.14 (1.02, 1.29) | 0.80 (0.63, 1.01) |
| Race | ||
| White | Reference | Reference |
| Black or African American | 1.09 (0.91, 1.30) | 0.61 (0.34, 1.10) |
| Hispanic or Latino | 1.28 (1.09, 1.51) | 0.46 (0.30, 0.71) |
| Asian | 1.13 (0.88, 1.44) | 1.23 (0.66, 2.30) |
| Parental advice not to smoke | ||
| Yes | Reference | Reference |
| No | 1.17 (1.03, 1.32) | 0.67 (0.46, 1.00) |
| School antismoking lessons | ||
| Yes | Reference | Reference |
| No | 1.40 (1.22, 1.62) | 1.04 (0.72, 1.51) |
| Exposure to anti-tobacco ads on TV or radio | ||
| Yes | Reference | Reference |
| No | 0.98 (0.84, 1.14) | 1.33 (0.84, 2.11) |
| Exposure to anti-tobacco ads on outdoor signs or billboards | ||
| Yes | Reference | Reference |
| No | 1.03 (0.90, 1.18) | 0.89 (0.65, 1.22) |
| Buy or receive tobacco promotional item | ||
| No | Reference | Reference |
| Yes | 1.55 (1.29, 1.85) | 2.16 (1.55, 3.00) |
| Would ever use or wear tobacco promotional item | ||
| No | Reference | Reference |
| Yes | 2.59 (2.17, 3.08) | 5.93 (4.12, 8.55) |
| Smoking at home | ||
| No | Reference | Reference |
| Yes | 1.11 (1.00, 1.23) | 2.88 (2.00, 4.14) |
| Friends smoke | ||
| No | Reference | Reference |
| Yes | 2.67 (2.33, 3.07) | 7.12 (4.90, 10.34) |
Note. Odds ratios are adjusted for all other variables in the table.
aDenominator is all never smokers.
bDenominator is all respondents.
TABLE 3—
Adjusted Odds Ratios for Open to Smoking and Established Smoking Among US Adolescents Aged 15 to 18 Years, by Survey Response: 2000 National Youth Tobacco Survey
| Never Smokers, Open to Smokinga Odds Ratio (95% Confidence Interval) | Established Smokersb Odds Ratio (95% Confidence Interval) | |
| Age, y | ||
| 15 | Reference | Reference |
| 16 | 0.71 (0.59, 0.85) | 1.58 (1.31, 1.91) |
| 17 | 0.54 (0.45, 0.66) | 2.21 (1.85, 2.65) |
| 18 | 0.57 (0.44, 0.73) | 2.97 (2.35, 3.74) |
| Gender | ||
| Male | Reference | Reference |
| Female | 1.18 (1.01, 1.38) | 1.21 (1.05, 1.38) |
| Race | ||
| White | Reference | Reference |
| Black or African American | 0.92 (0.75, 1.15) | 0.43 (0.32, 0.59) |
| Hispanic or Latino | 1.35 (1.06, 1.72) | 0.32 (0.23, 0.44) |
| Asian | 1.03 (0.74, 1.42) | 0.81 (0.60, 1.11) |
| Parental advice not to smoke | ||
| Yes | Reference | Reference |
| No | 0.88 (0.76, 1.01) | 0.38 (0.34, 0.44) |
| Exposure to anti-tobacco ads on TV or radio | ||
| Yes | Reference | Reference |
| No | 1.17 (0.95, 1.44) | 1.18 (0.99, 1.41) |
| Exposure to anti-tobacco ads on outdoor signs or billboards | ||
| Yes | Reference | Reference |
| No | 1.02 (0.86, 1.21) | 0.96 (0.82, 1.12) |
| Buy or receive tobacco promotional item | ||
| No | Reference | Reference |
| Yes | 1.25 (1.03, 1.52) | 1.84 (1.64, 2.05) |
| Would ever wear tobacco promotional item | ||
| No | Reference | Reference |
| Yes | 2.30 (1.95, 2.72) | 3.12 (2.73, 3.55) |
| Smoking at home | ||
| No | Reference | Reference |
| Yes | 0.96 (0.82, 1.13) | 2.64 (2.34, 2.98) |
| Friends smoke | ||
| No | Reference | Reference |
| Yes | 1.72 (1.47, 2.02) | 5.80 (4.94, 6.82) |
Note. Odds ratios are adjusted for all other variables in the table.
aDenominator is all never smokers.
bDenominator is all respondents.
Correlates of Established Smoking
Among both younger and older adolescents, receptivity to tobacco industry promotions was a significant variable in the logistic regression. Both a history of buying or receiving a promotional item and the willingness to use or wear a tobacco promotional item were significantly associated with established smoking. Other significant predictors for established smoking were having friends who smoke and being exposed to smoking at home.
DISCUSSION
Our data reinforce the widely documented facts that smoking is often considered a pediatric condition and that prevention programs should begin in middle school and earlier.13–15 We estimate that in 2000, there were about 2.7 million adolescent established smokers aged 11 to 18 years in the United States. While about one third of the adolescent established smokers in 2000 were aged 18 years, the two thirds who were younger than 18 years included about 300 000 youths aged 11 to 14 years.
Early experimenters comprised about 31% of all adolescents. In previous analyses of national data, the Centers for Disease Control and Prevention16 and Choi et al.17 estimated that 30% or more of experimenters become established smokers. When the 30% estimate is applied to the cohort of adolescents aged 11 to 18 years who were early experimenters in 2000, about 2.9 million of these early experimenters have now become or will become established smokers, assuming that past trends continue into the future. Prevention efforts should be particularly targeted to the early experimenters because (1) almost one third of adolescents are in this stage, (2) these youths are at more immediate risk for future established smoking and nicotine addiction than never smokers, and (3) there is sufficient time to intervene prior to daily smoking. Questions on the national and state-based Youth Tobacco Surveys11 can be used to identify early experimenters.
Among middle school youths who had never smoked, we found that those who had received advice from parents about the dangers of smoking or had received multiple strategies of smoking-prevention education in school were more likely to be not open to smoking. These findings are consistent with previous studies that show parental guidance combined with school antismoking classes can prevent smoking uptake.18,19 Exposure to smoking at home was not significantly associated with being open to smoking but was a significant correlate of established smoking; however, we were not able to identify who smoked in the household.
There was a strong association between receptivity to tobacco industry promotions and open to smoking. Adolescents who had bought or received a tobacco promotional item or were willing to use or wear a promotional item were more likely to be open to smoking. This relationship holds for both younger and older adolescents and persisted after adjustment for demographic and other environmental variables, including having friends who smoke and exposure to smoking at home.
In a large prospective study, Pierce et al.8 identified adolescent never smokers not open to smoking in California in 1993 and reinterviewed them in 1996. They showed that never smokers not open to smoking in 1993 who had a high level of receptivity to tobacco industry promotions were almost 3 times more likely to progress to a later stage of uptake by 1996. Biener et al.9 interviewed a sample of Massachusetts adolescents who at baseline had smoked no more than 1 cigarette. At follow-up, those youths who owned a tobacco promotional item and who named a brand whose advertisements attracted their attention were more than twice as likely to become established smokers as adolescents than those who did neither. In a cross-sectional study, Kaufman et al.20 measured the influence of tobacco industry advertising and promotion on a 4-point scale. A dose–response correlation between this factor and established smoking was found. Youths who did not have a favorite cigarette advertisement and who did not own or would not use a tobacco industry promotional item were least likely to be established smokers, while those who had a favorite advertisement and owned or would use a promotional item were most likely to be established smokers.
We did not find that youths who were exposed to countertobacco advertising were less likely to be open to smoking. This is not surprising, because awareness of antismoking advertisements is measured crudely in the NYTS. By using a more rigorous measure of exposure, Sly et al.21 found that the Florida “truth” campaign was effective in preventing or at least delaying smoking initiation. Siegel and Biener22 found that younger adolescents (aged 12 to 13 years at baseline) in Massachusetts who reported baseline exposure to television antismoking advertisements were less likely to have progressed to established smoking over a 4-year follow-up period. Both Florida and Massachusetts have conducted comprehensive antismoking interventions targeted at youths that included extensive paid media campaigns.
When the NYTS was administered in the spring of 2000, 2 national antismoking media campaigns targeted at youths were in place. The Philip Morris Companies’ “Think Don’t Smoke” advertisements had been appearing on national television networks. The American Legacy Foundation’s “truth” national countermarketing campaign had just started in February 2000 and was focused on the primary prevention of smoking among at-risk youths aged 12 to 17 years.23 Results from 2 national phone surveys show that exposure to the American Legacy Foundation’s “truth” advertisements is associated with an increase in anti-tobacco attitudes and beliefs.24
CONCLUSIONS
The illustration of progression to established smoking in Figure 1 ▶ highlights the importance of early interventions to curb smoking uptake. Between the ages of 11 and 18 years, the prevalence of established smoking increases at an increasing rate with age. Our results suggest that parental influences and school antismoking classes can slow or prevent progression to established smoking. Our results also suggest that exposure to smoking at home, peer smoking, and tobacco industry marketing are important risk factors for established smoking. An especially promising public health intervention is paid antismoking media campaigns. Results from 2 state campaigns and preliminary results from the American Legacy Foundation’s national “truth” campaign suggest that paid antismoking media campaigns directed at youths and used as 1 component of a comprehensive tobacco control program can be effective in reducing progression.
Because of the cross-sectional nature of the NYTS, a statistically significant relationship between a risk factor and the stage of smoking represents a contemporaneous correlation and cannot be interpreted as having a causal impact on smoking. However, such associations may indicate fruitful areas of exploration for interventions targeted at slowing the progression of smoking uptake.
Acknowledgments
The 1999 National Youth Tobacco Survey was conceived and was funded by the Centers for Disease Control and Prevention, Office on Smoking and Health. The 2000 National Youth Tobacco Survey and this study were funded by the American Legacy Foundation.
The authors thank Jane Appleyard for reviewing the manuscript, Pat Dean Brick for statistical and data analysis assistance, and Susan Murchie for editorial review.
Human Participant Protection No protocol approval was needed for this study.
Contributors P. D. Mowery conceptualized the study, directed the data analysis, and wrote the article. M. C. Farrelly participated in preparing the article. M. L. Haviland participated in the design of the study and wrote parts of the article. J. M. Gable conducted data analyses and participated the writing the article. H. E. Wells conducted data analyses and reviewed the final draft of the manuscript.
Peer Reviewed
References
- 1.Nelson DE, Giovino GA, Shopland DR, Mowery PD, Mills SL, Eriksen MP. Trends in cigarette smoking among US adolescents, 1974 through 1991. Am J Public Health. 1995;85:34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Trends in cigarette smoking among high school students—US, 1991–1999. MMWR Morb Mortal Wkly Rep. 2000;49:755–758. [PubMed] [Google Scholar]
- 3.Johnston LD, O’Malley PM, Bachman JG. Teen smoking declines sharply in 2002, more than offsetting large increases in the early 1990s. University of Michigan News and Information Services Web site. Available at http://www.monitoringthefuture.org. Accessed December 16, 2002.
- 4.Leventhal H, Cleary PD. The smoking problem: a review of the research and theory in behavioral risk modification. Psychol Bull. 1980;88:370–405. [DOI] [PubMed] [Google Scholar]
- 5.Flay BR. Youth tobacco use: risks, patterns, and control. In: Orleans CT, Slade J, eds. Nicotine Addiction: Principles and Management. New York, NY: Oxford University Press; 1993.
- 6.US Dept of Health and Human Services. The Health Consequences of Smoking: Nicotine Addiction: A Report of the Surgeon General. Atlanta, Ga: Centers for Disease Control and Prevention, Office on Smoking and Health; 1988.
- 7.US Dept of Health and Human Services. Preventing Tobacco Use Among Young People: A Report of the Surgeon General. Atlanta, Ga: Centers for Disease Control and Prevention, Office on Smoking and Health; 1994.
- 8.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Berry CC. Tobacco industry promotion of cigarettes and adolescent smoking. JAMA. 1998;279:550–552. [DOI] [PubMed] [Google Scholar]
- 9.Biener L, Siegel M. Tobacco marketing and adolescent smoking: more support for a causal inference. Am J Public Health. 2000;90:407–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choi WS, Gilpin EA, Farkas AJ, Pierce JP. Determining the probability of future smoking among adolescents. Addiction. 2001;96:313–323. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Youth tobacco surveillance—United States, 2000. MMWR Morb Mortal Wkly Rep. 2001;50(SS-4):1–46.11215787 [Google Scholar]
- 12.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol. 1996;15:355–361. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs—August 1999. Atlanta, Ga: Centers for Disease Control and Prevention, Office on Smoking and Health; 1999.
- 14.Centers for Disease Control and Prevention. Guidelines for school health programs to prevent tobacco use and addiction. MMWR Morb Mortal Wkly Rep. 1994;43(RR-2). [PubMed]
- 15.Orleans CT, Arkin EB, Backinger CL, et al. Youth Tobacco Cessation Collaborative and National Blueprint for Action. Am J Health Behav. 2003;27(suppl 2):S103–S119. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Selected cigarette smoking initiation and quitting behaviors among high school students—US, 1997. MMWR Morb Mortal Wkly Rep. 1998;47:386–389. [PubMed] [Google Scholar]
- 17.Choi WS, Pierce JP, Gilpin EA, Farkas AJ, Berry CC. Which adolescent experimenters progress to established smoking in the United States. Am J Prev Med. 1997;13:385–391. [PubMed] [Google Scholar]
- 18.Bauman KE, Foshee VA, Ennett ST, et al. The influence of a family program on adolescent tobacco and alcohol use. Am J Public Health. 2001;91:604–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Distefan JM, Gilpin EA, Choi WS, Pierce JP. Parental influences predict adolescent smoking in the United States, 1989–1993. J Adolesc Health. 1998;22:466–474. [DOI] [PubMed] [Google Scholar]
- 20.Kaufman NJ, Castrucci BC, Mowery PD, Gerlach KK, Emont S, Orleans CT. Predictors of change on the smoking uptake continuum among adolescents. Arch Pediatr Adolesc Med. 2002;156:581–587. [DOI] [PubMed] [Google Scholar]
- 21.Sly DF, Hopkins RS, Trapido E, Ray S. Influence of a counteradvertising media campaign on initiation of smoking: the Florida “truth” campaign. Am J Public Health. 2001;91:233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siegel M, Biener L. The impact of an antismoking media campaign on progression to established smoking: results of a longitudinal youth study. Am J Public Health. 2000;90:380–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Healton C. Who’s afraid of the truth? Am J Public Health. 2001;91:554–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farrelly MC, Healton CG, Davis KC, Messeri P, Hersey JC, Haviland ML. Getting to the truth: evaluating national tobacco countermarketing campaigns. Am J Public Health. 2002;92:901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]