Abstract
Our study quantifies the impact of achieving specific Healthy People 2010 targets and of eliminating racial/ethnic health disparities on summary measures of health. We used life table methods to calculate gains in life expectancy and healthy life expectancy that would result from achievement of Healthy People 2010 objectives or of current mortality rates in the Asian/Pacific Islander (API) population.
Attainment of Healthy People 2010 mortality targets would increase life expectancy by 2.8 years, and reduction of populationwide mortality rates to current API rates would add 4.1 years. Healthy life expectancy would increase by 5.8 years if Healthy People 2010 mortality and assumed morbidity targets were attained and by 8.1 years if API mortality and activity limitation rates were attained.
Achievement of specific Healthy People 2010 targets would produce significant increases in longevity and health, and elimination of racial/ethnic health disparities could result in even larger gains.
THE PRACTICE OF ESTABLISHING national health objectives has been in effect for more than 2 decades. Beginning in 1979 with Healthy People: The Surgeon General’s Report on Health Promotion and Disease Prevention,1 each succeeding decade has brought an increasing number of quantifiable objectives for preventing disease and for promoting health. The current objectives, Healthy People 2010, were developed by coordinating input from more than 350 national organizations, 250 state public health–related agencies, and the general public.2 Experts from various federal agencies were responsible for developing the final 467 objectives, with different agencies taking the lead for each of the 28 focus areas.
The large number and the many types of objectives are designed to provide a road map for achieving 2 overarching goals: (1) increase life expectancy and improve quality of life, and (2) eliminate health disparities.2 Aiming for the elimination of health disparities is arguably the most ambitious goal of Healthy People 2010. When the US population is divided by any of a number of demographic criteria—gender, race/ethnicity, education or income level, geographic location, disability, or sexual orientation—we find substantial differences in health status and longevity. Differences in health status reflect disparities in many types of health determinants: social and environmental factors, health-related behaviors, access to and use of health services, and quality of health care received.3–6
For the specific population-based objectives in Healthy People 2010, the goal of eliminating health disparities was acknowledged by setting a single national target that applies to all population subgroups. However, 2 different principles were used to establish these targets.7 For objectives related to access to and use of health services, and for objectives in areas that can be influenced in the short term by changes in health behaviors or health policy, targets were set at a level “better than the best” racial/ethnic group. For other objectives, achievement of a “better than the best” target for all racial/ethnic groups within 10 years was considered unrealistic regardless of the level of resources invested. For these objectives, the target was set at a level that represented improvement for a substantial proportion of the population but did not imply the elimination of racial/ethnic health disparities.
In contrast to the specific Healthy People 2010 objectives, the overarching goal of increasing life expectancy and improving quality of life does not specify a numerical target. Although it is certain that achieving the specific targets will increase both longevity and health for the average American, as will eliminating racial/ethnic health disparities in a manner consistent with these goals, the expected increase in life expectancy and healthy life expectancy has not been estimated. Making these estimates will provide public health policymakers and planners with benchmarks against which the variable progress toward the many specific Healthy People 2010 objectives can be evaluated.
ASSESSING THE EFFECT OF ACHIEVING GOALS
Life Table Methods
Our analysis quantifies the gains that can be expected in both life expectancy and healthy life expectancy from achieving specific Healthy People 2010 mortality and morbidity targets and from eliminating racial/ethnic health disparities. Life expectancy, perhaps the most often cited summary indicator of population health, is calculated by applying age-specific death rates for a given year to a hypothetical cohort of persons born in that year. The result is the number of years an individual can expect to live if he or she is subject to the annual age-specific death rates of that year over his or her entire lifetime. Life expectancy is a useful tool for summarizing mortality, because it is not affected by the age structure of the population and it is easily interpreted by both policymakers and the general public. Because of these advantages, the strategy of extending life expectancy calculations to incorporate measures of health, although originally introduced in the 1960s, has recently received renewed attention. The most commonly used methodology, developed by Sullivan,8 separates life expectancy into healthy and unhealthy years by incorporating estimates of the age-specific prevalence of morbidity or disability.
We used age-specific death rates obtained from US vital statistics for 1998, the original baseline year for the Healthy People 2010 objectives, to calculate life expectancy for the US population. To calculate healthy life expectancy, we used age-specific prevalence rates of activity limitation caused by chronic health conditions as the indicator of morbidity. Activity limitation rates for 1998 were obtained from the 1998 National Health Interview Survey (NHIS). We used Sullivan’s method in conjunction with the standard life table used by the National Center for Health Statistics9 to apply age-specific death rates and activity limitation rates to a hypothetical cohort. We then altered the 1998 baseline mortality and activity limitation rates to reflect the reductions that would occur if the specified Healthy People 2010 objectives were to be attained or if rates for the population as a whole were lowered to the level of the healthiest racial/ethnic subgroup in 1998.
Mortality Reductions
Twenty-six of the 467 Healthy People 2010 objectives specify reductions in 1998 age-adjusted death rates for specific causes of death, 7 objectives specify reductions for specific age groups, and 5 objectives specify reductions for a specific cause and a specific age group.2 Some objectives are broader than others and are assumed to encompass several more detailed targets. For example, the targeted reduction in total mortality for persons aged 20 to 24 years encompasses the relevant cause-specific mortality reductions specified in other objectives, the targeted death rate for all cancer encompasses site-specific cancer targets, and the targeted death rate for chronic obstructive pulmonary disease encompasses the asthma targets for persons aged 25 years and older. For our analysis, we used the more comprehensive objective and assumed that it incorporated the targets for the more specific objectives.
For each cause of death, the overall percentage reduction in the 1998 age-adjusted mortality rate was applied to the 1998 age-specific rates (at 10-year age intervals) for persons aged 25 years and older. For each age interval, the reduced rates for each cause of death were summed and were added to the unreduced residual (other and unspecified causes) to form the targeted age-specific death rates for all causes combined. For persons younger than 25 years, the targeted age-specific total mortality rates were used.
To evaluate the impact of eliminating racial/ethnic mortality disparities, we examined agespecific death rates for 1997, 1998, and 1999 for the 5 largest racial and ethnic groups in the US population: non-Hispanic Whites, African Americans, American Indians/Alaska Natives, Asians/Pacific Islanders, and Hispanics. For these 3 years combined, Asians/Pacific Islanders (API) had the lowest death rate overall and the lowest age-specific rates for all age groups younger than 85 years.
Misreporting of race and Hispanic origin on the death certificate affects the numerators of reportd race/ethnicity-specific death rates. Undercoverage in the census affects the denomnators of reported race/ethnicity-specific death rates. Rosenberg et al.10 used a file of death certificates linked to the Current Population Survey to evaluate misreporting of race on death certificates. They estimated that the underreporting of API race on the death certificate artificially lowered death rates for this group by 13% overall and by 6% to 46% within specific age intervals. We applied these agespecific estimates of underreporting of API race on death certificates to the death rates for this group for 1997, 1998, and 1999 combined. Rosenberg et al. also reported a slight net undercount of API race on the 1990 census (2%), but they were unable to differentiate this undercount by age groups. Therefore, we did not attempt to correct for the impact of the undercount on the denominator of the death rates. As a result, the adjusted API death rates used in our analysis are higher than the death rates officially reported for this racial group, and they are probably slightly higher than the true rates.
Reductions in Health-Related Activity Limitation
Summarizing the effect of targeted reductions in morbidity from specific diseases is more difficult than summarizing the effect of attaining mortality targets. For the purposes of our analysis, we have chosen to define healthy years as years free of activity limitation owing to chronic health conditions. However, only a few of the Healthy People 2010 objectives specifically address reduction of activity limitation caused by diseases and conditions. These objectives include reducing activity limitation associated with arthritis and chronic back conditions, lung and breathing problems, and asthma. Data from the NHIS indicate that whereas arthritis and other musculoskeletal conditions are the leading causes of activity limitation among adults, heart and other circulatory conditions, vision and hearing impairments, fractures and joint injuries, diabetes, and mental illness also are important contributors to health-related activity limitation. Among children, major contributors to activity limitation are learning disabilities and other developmental problems, behavioral and emotional problems, vision and hearing impairments, and asthma.11
Although most Healthy People 2010 objectives do not target specific reductions in activity limitation, many of the objectives specify reductions either in diseases that cause activity limitation or in the disabling sequelae of these diseases. For example, separate objectives specify reductions in the annual number of new cases of diabetes as well as reductions in cases of end-stage renal disease, foot ulcers, and lower-extremity amputations among diabetic individuals.2 We attempted to translate these types of objectives into reductions in activity limitation by assuming that the targeted reductions in diseases or their sequelae implied an equal percentage reduction in activity limitation owing to these same diseases or conditions. Our estimates of current levels of activity limitation attributable to categories of specific chronic diseases were derived from the NHIS for the years 1997, 1998, and 1999. This procedure resulted in implied age-specific reductions in activity limitation of between 8% and 33%, with greater reductions in older than in younger age groups. However, this very crude methodology could not adequately account for activity limitation related to multiple chronic conditions, and many targets could not be matched to diseases specifically identified as causes of activity limitation.
Because of the imprecision of this methodology, we chose to examine the impact of achieving a 25% reduction in activity limitation for individuals younger than 50 years and of achieving a 33% reduction for persons aged 50 years and older. This simplification preserves the general magnitude and age pattern resulting from our attempt to translate specific objectives into activity limitation reductions, yet it makes it easier to evaluate changes in these assumed values. If smaller reductions are assumed, the impact on healthy life expectancy will be smaller; if larger reductions are assumed, the impact on healthy life expectancy will be magnified.
To assess the impact on healthy life expectancy of eliminating racial/ethnic disparities in activity limitation owing to chronic illnesses, we again examined age-specific rates for each of the 5 major racial/ethnic groups in the US population. When we examined combined data from the 1997, 1998, and 1999 NHIS, we found that the API population had the lowest activity limitation rates—both overall and within each age group. We therefore assumed that to meet the targeted objective of eliminating racial/ethnic disparities, the entire US population would have to achieve activity limitation levels equal to those of the API population.
MORTALITY REDUCTIONS
Table 1 ▶ shows the age-specific death rates for the 1998 US population (baseline year), the death rates implied by achieving the age- and cause-specific Healthy People 2010 targets, and the 1997–1999 age-specific death rates for the API population adjusted for racial misclassification on the death certificate. Comparing the percentage reductions from the actual 1998 rates implied by these alternative targets reveals a striking difference in the age pattern of mortality reductions. The reductions are similar for infants and for persons aged 25 to 29 years; however, whereas the Healthy People 2010 objectives imply substantially larger reductions in death rates for persons aged 1 through 24 years, the API mortality rates imply greater improvements for persons aged 30 years and older.
TABLE 1—
Age-Specific Mortality Reductions Implied by Achievement of Alternative Objectives: Healthy People 2010 Targets and Asian/Pacific Islander Rates
| Age- and Combined Condition-Specific Healthy People 2010 Targets | Adjusteda Death Rates for Asians/Pacific Islanders, 1997–1999 | ||||
| Age, y | 1998 Death Rate | Death Rate From All Causes (per 100 000) | Reduction From 1998, % | Death Rate From All Causes (per 100 000) | Reduction From 1998, % |
| < 1 | 751.4 | 469.6 | −37.5 | 492.3 | −34.5 |
| 1–4 | 34.6 | 18.6 | −46.2 | 32.5 | −6.0 |
| 5–9 | 17.7 | 12.3 | −30.5 | 18.4 | 3.8 |
| 10–14 | 22.1 | 16.8 | −24.0 | 23.6 | 6.3 |
| 15–19 | 70.6 | 39.8 | −43.6 | 60.0 | −15.0 |
| 20–24 | 95.3 | 49.0 | −48.6 | 75.2 | −21.0 |
| 25–29 | 97.7 | 58.0 | −40.6 | 57.8 | −40.8 |
| 30–34 | 120.7 | 74.1 | −38.6 | 61.5 | −49.0 |
| 35–39 | 164.6 | 106.9 | −35.0 | 82.8 | −49.7 |
| 40–44 | 235.9 | 164.1 | −30.4 | 123.6 | −47.6 |
| 45–49 | 346.9 | 255.8 | −26.3 | 182.9 | −47.3 |
| 50–54 | 515.6 | 396.4 | −23.1 | 284.6 | −44.8 |
| 55–59 | 811.3 | 635.5 | −21.7 | 475.9 | −41.3 |
| 60–64 | 1 296.1 | 1 026.4 | −20.8 | 743.0 | −42.7 |
| 65–69 | 1 978.6 | 1 576.4 | −20.3 | 1 297.1 | −34.4 |
| 70–74 | 3 059.0 | 2 458.7 | −19.6 | 2 109.6 | −31.0 |
| 75–79 | 4 565.3 | 3 724.0 | −18.4 | 3 227.0 | −29.3 |
| 80–84 | 7 440.8 | 6 182.9 | −16.9 | 5 429.3 | −27.0 |
| ≥ 85 | 15114.3 | 12970.6 | −14.2 | 10558.0 | −30.1 |
aDeath rates were adjusted for misclassification of race on the death certificate.
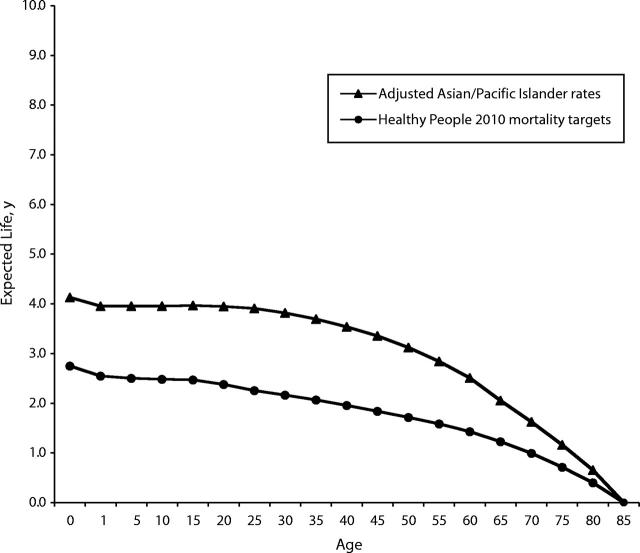
In 1998, the life expectancy at birth in the United States was 76.7 years. Achievement of the mortality reductions specified in the Healthy People 2010 targets would increase life expectancy at birth by 2.8 years, while reduction of populationwide mortality rates to the levels of the API population in 1998 would increase life expectancy at birth by 4.1 years. Figure 1 ▶ shows the additions to life expectancy at given ages implied by these alternative targets. Reducing mortality in the US population to the adjusted death rates for the API population would produce greater gains in life expectancy at all ages for persons younger than 85 years, despite the greater mortality reductions for persons aged 1 through 24 years implied by the specific Healthy People 2010 objectives. This result is derived from the lower API death rates at older ages, when mortality is highest.
FIGURE 1—
Additional years of expected life gained at specific ages, assuming achievement of alternative national health objectives.
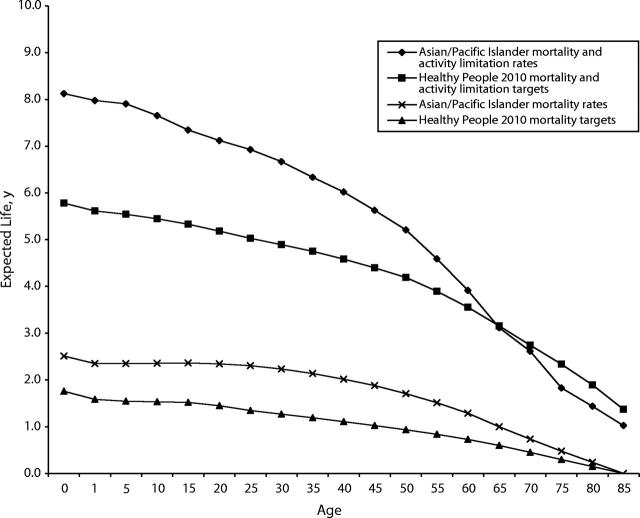
We used age-specific death rates and activity limitation rates for 1998 to calculate healthy life expectancy in the United States. On the basis of these rates, healthy life expectancy at birth was 64.6 years. Reductions in death rates implied by attainment of the Healthy People 2010 mortality targets (when the agespecific rates of activity limitation are at their 1998 levels) would increase healthy life expectancy at birth by 1.8 years, while reducing mortality rates to the 1997–1999 API levels would add 2.5 years. As is the case with life expectancy, attainment of the adjusted API death rates would produce a greater gain in healthy life expectancy at all ages than would attainment of the age- and cause-specific Healthy People 2010 mortality targets (Figure 2 ▶).
FIGURE 2—
Additional years of expected healthy life gained at specific ages, assuming achievement of alternative national health objectives.
MORBIDITY REDUCTIONS
Table 2 ▶ shows the age-specific activity limitation rates for the 1998 US noninstitutionalized population, the rates that would result from the assumed percentage reductions in limiting conditions implied by the Healthy People 2010 targets, and the age-specific activity limitation rates for the 1997, 1998, and 1999 API population. Compared with our assumed Healthy People 2010 targets, the 1997–1999 API rates would produce substantially greater reductions in activity limitation at all ages for persons younger than 65 years but smaller reductions for persons 75 years and older.
TABLE 2—
Age-Specific Reductions in Activity Limitation Implied by Achievement of Alternative Objectives: Healthy People 2010 Targets and Asian/Pacific Islander Rates
| Estimates for Healthy People 2010 Targets | Asians/Pacific Islanders, 1997–1999 | ||||
| Age, y | Any Activity Limitation Because of Chronic Conditions—1998, % | Any Activity Limitation Due to Chronic Conditions, % | Reduction From 1998, % | Any Activity Limitation Due to Chronic Conditions, % | Reduction From 1998, % |
| < 1 | 3.4 | 2.6 | −25.0 | 1.5 | −57.6 |
| 1–4 | 3.4 | 2.6 | −25.0 | 1.5 | −57.6 |
| 5–9 | 7.0 | 5.2 | −25.0 | 1.8 | −74.7 |
| 10–14 | 8.7 | 6.5 | −25.0 | 2.3 | −73.0 |
| 15–19 | 6.4 | 4.8 | −25.0 | 1.9 | −69.8 |
| 20–24 | 5.4 | 4.0 | −25.0 | 1.8 | −65.9 |
| 25–29 | 5.3 | 4.0 | −25.0 | 1.3 | −74.8 |
| 30–34 | 6.5 | 4.9 | −25.0 | 1.6 | −75.8 |
| 35–39 | 7.9 | 5.9 | −25.0 | 3.6 | −54.2 |
| 40–44 | 10.2 | 7.6 | −25.0 | 4.6 | −54.6 |
| 45–49 | 12.7 | 9.5 | −25.0 | 7.0 | −44.4 |
| 50–54 | 16.1 | 10.8 | −33.0 | 6.7 | −58.6 |
| 55–59 | 19.8 | 13.2 | −33.0 | 9.4 | −52.4 |
| 60–64 | 24.6 | 16.5 | −33.0 | 12.7 | −48.3 |
| 65–69 | 27.5 | 18.4 | −33.0 | 20.1 | −27.0 |
| 70–74 | 31.4 | 21.0 | −33.0 | 17.4 | −44.4 |
| 75–79 | 39.3 | 26.3 | −33.0 | 32.1 | −18.3 |
| 80–84 | 51.2 | 34.3 | −33.0 | 41.7 | −18.5 |
| ≥ 85 | 66.8 | 44.8 | −33.0 | 50.4 | −24.6 |
Applying the reduced rates of activity limitation in conjunction with the specific Healthy People 2010 mortality targets increases healthy life expectancy at birth by 5.8 years, 4 years more than the increase effected by attaining the Healthy People 2010 mortality targets alone. Eliminating racial/ethnic disparities by bringing the entire US population to the API mortality and activity limitation levels for 1997–1999 increases healthy life expectancy by 8.1 years, 5.6 years more than what would be achieved by eliminating only the disparity in mortality. Compared with attaining the assumed Healthy People 2010 targets, achieving API activity limitation and mortality rates implies greater increases in healthy life expectancy at each age up to age 65 years, but slightly smaller gains at ages 70 years and older (Figure 2 ▶).
DISCUSSION
Assessing the impact on life expectancy and healthy life expectancy of attaining the specific Healthy People 2010 objectives is not as simple as public health professionals, policymakers, and the general public might wish. Although translating cause- or age-specific death rate targets into an implied increase in life expectancy is relatively straightforward, even this translation requires assumptions about how age-specific targets can be reconciled with cause-specific targets. It is far more difficult to determine the impact on healthy life expectancy of the many objectives aimed at reducing health risks and disease, increasing access to health care, and improving the functioning of persons with chronic health conditions. Only 2 focus areas—(1) arthritis, osteoporosis, and chronic back conditions and (2) respiratory diseases—contain objectives that specify targets for reducing activity limitation caused by these conditions. Additionally, health-related activity limitation, or any other summary measure of health, reflects the total health experience of individuals, many of whom have multiple chronic conditions that contribute to their functional ability and overall health status. Even if more focus areas contained objectives specifying reductions in activity limitation, assessment of the impact of these targets on healthy life expectancy would still require making assumptions to account for comorbidity.
We believe that the assumptions used in our analysis are consistent with deriving the maximum benefit from attainment of each Healthy People 2010 target. The previous decade’s objectives, Healthy People 2000, specified a 15% reduction in the age-adjusted proportion of the population who experience limitation in their major daily activities due to chronic conditions. The assumption of 25% to 33% reductions in rates of all activity limitation attributable to chronic conditions is in keeping with the greater number of—and the generally more optimistic character of—targets in Healthy People 2010 relative to those in its earlier counterpart.1,12,13
Addressing and reducing health disparities among subgroups of the US population has long been a focus of public health. Healthy People 2000 included the overarching goal of reducing health disparities,12 and Healthy People 2010 took an ambitious leap forward by calling for the elimination of health disparities. It is possible to eliminate disparities by improving health in some groups while reducing it in others, but eliminating disparities in this manner would be inconsistent with improving health for all Americans, which is the overall aim of the Healthy People initiative.2
For many of the 467 objectives, elimination of health disparities was incorporated into the target-setting process by setting the target “better” than the level in the healthiest racial/ethnic subgroup.7 For some health measures, however, the targets implicitly acknowledged that an equal health outcome for all population subgroups was unlikely to be achieved over the remainder of the decade, regardless of the level of resources invested. Many morbidity and mortality measures fall into this latter category because of the time lag between exposure and outcome.
For our analysis, eliminating health disparities was defined as achieving the mortality and the morbidity levels of the currently healthiest racial/ethnic group. Thus, our estimates of the impact of eliminating health disparities on life expectancy and healthy life expectancy are equivalent to estimates of the impact achieving the current best levels for all morbidity and mortality outcomes. Comparing the gains in life expectancy and healthy life expectancy produced by attaining specific Healthy People 2010 objectives with the gains achieved by eliminating racial/ethnic health disparities can be viewed as comparing what may be attained over a decade through maximal investments in health with what we may hope to see in the long run once the fruits of these investments have been fully realized.
Achieving the age- and cause-specific mortality targets contained in Healthy People 2010 will increase life expectancy at birth by nearly 3 years and will increase healthy life expectancy at birth by nearly 2 years. Alternatively, if all Americans were to experience the 1998 API death rates, life expectancy at birth would rise by 4 years and healthy life expectancy would increase by 2.5 years. Although it may not be realistic to contemplate mortality declines unaccompanied by morbidity reductions, the comparison of mortality targets and the target of eliminating racial/ethnic disparities in mortality is more precise, because calculating the impact of the Healthy People 2010 mortality targets requires fewer simplifying assumptions than does calculating the combined mortality and morbidity effects.
Despite the difficulty in translating the Healthy People 2010 morbidity objectives into reductions in activity limitation, comparing activity limitation rates assumed to reflect Healthy People 2010 targets with activity limitation rates for the 1998 API population is instructive. For example, the age-specific Healthy People 2010 mortality targets for persons less than age 25 years are lower than the 1998 API death rates at these ages. Conversely, 1997–1999 rates of API activity limitation for the same age are well below our estimates that reflect Healthy People 2010 targets. This discrepancy may arise from the lack of targets that address learning impairments and other developmental disabilities, which are the primary causes of activity limitation in children.11 This comparison points to areas that may need additional attention in future target-setting endeavors.
Overall, achieving the 25% to 33% reductions in activity limitation assumed to be consistent with Healthy People 2010 morbidity targets would add 4 years to healthy life expectancy at birth over what would be gained by reaching the mortality targets alone. Attaining the 1997–1999 levels of API activity limitation would add another 5.6 years to healthy life expectancy at birth over what would be gained by achieving 1998 API death rates.
When we examine these alternative targets in the light of past trends, it is clear that even the more modest gains in life expectancy and healthy life expectancy implied by the specific Healthy People 2010 objectives represent a major improvement over past achievements. Between 1988 and 1998, life expectancy at birth increased by 1.8 years. Years of healthy life, as measured by combining activity limitation with self-assessed health, increased by 1.2 years between 1990 and 1998, a gain that reflects only the increase in life expectancy during this period. The other global measures of morbidity included in the Healthy People 2000 targets—self-assessed health, limitation in major daily activity, and difficulty with self-care among persons aged 70 years and older—showed no improvement during the first half of the 1990s.14 (Because of the redesign of the NHIS in 1997, trends in these indicators over the entire decade cannot be determined.) Progress toward reducing health disparities over the past decade also was modest. In 1990, life expectancy at birth for Whites was 7 years higher than that for Blacks. By 1999, this difference had been reduced to 5.9 years.15 And although racial/ethnic health disparities decreased for 12 of the 17 Healthy People health status indicators, the reduction was less than 10% for 8 of these measures.16
Viewed in this light, the Healthy People 2010 objectives—especially the goal of eliminating health disparities—may seem overly optimistic, but overly optimistic is not synonymous with unachievable. The commitment to address racial/ethnic health disparities is reflected by incorporating their elimination into many Healthy People 2010 objectives through the “better than the best” target-setting method. Healthy People 2010 does not make recommendations about how to achieve the targets; however, establishing the target does enable the monitoring of progress toward achievable health goals. Monitoring progress, whether toward narrowly defined objectives or toward overarching goals, provides a mechanism for the continuous reevaluation of priorities on the basis of recorded successes and failures.
The contrast between the specific Healthy People 2010 objectives and the overarching goal of eliminating health disparities embodies an essential tension in the process of setting national health objectives. It is both desirable and prudent to establish specific, measurable goals that reflect what we believe to be achievable over the next decade by applying current health knowledge and by establishing best practices, but it is also important to recognize and to acknowledge the full scope of what could be achieved if we were to realize our most fundamental ideals. The larger impact of eliminating health disparities shows that we can expect to achieve more than we otherwise could by addressing the large differences in life experiences, health, and, ultimately, death that exist within the US population.
Acknowledgments
The authors wish to thank Tom Hodgson and Jennifer Madans for their useful comments on the initial version of this article.
Human Participant Protection No protocol approval was needed for this study.
Contributors E. R. Pamuk and D. K. Wagner conceived of and designed the study. M. T. Molla and E. R. Pamuk conducted the data analyses. E. R. Pamuk wrote the article, and all authors contributed to writing and revision.
Peer Reviewed
References
- 1.US Public Health Service. Healthy People: Surgeon General’s Report on Health Promotion and Disease Prevention. Washington, DC: US Dept of Health and Human Services; 1979.
- 2.Healthy People 2010, 2nd ed., With Understanding and Improving Health and Objectives for Improving Health. Washington, DC: US Department of Health and Human Services; 2001.
- 3.Pamuk E, Makuc D, Heck K, Reuben C, Lochner K. Socioeconomic Status and Health Chartbook. Health, United States, 1998. Hyattsville, Md: National Center for Health Statistics; 1998.
- 4.Eberhardt MS, Ingram DD, Makuc DM, et al. Urban and Rural Health Chartbook. Health, United States, 2001. Hyattsville, Md: National Center for Health Statistics; 2001.
- 5.National Research Council. America Becoming: Racial Trends and Their Consequences. Vol. 2. Washington, DC: National Academy Press; 2001.
- 6.Gay and Lesbian Medical Association. Healthy People 2010 Companion Document for Lesbian, Gay, Bisexual, and Transgender (LGBT) Health. San Francisco, Calif: Gay and Lesbian Medical Association; 2001. Available at: http://www.glma.org. Accessed April 23, 2002.
- 7.US Dept of Health and Human Services. Tracking Healthy People 2010. Washington, DC: US Government Printing Office; November2000.
- 8.Sullivan DF. A single index of mortality and morbidity. HSMHS Health Reports. 1971;86:347–354. [PMC free article] [PubMed] [Google Scholar]
- 9.Molla MT, Wagener DK, Madans JH. Summary measures of population health: methods for calculating healthy life expectancy. In: Healthy People Statistical Notes, No. 21. Hyattsville, Md: National Center for Health Statistics; August2001. [DOI] [PubMed]
- 10.Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: a summary of current research, 1999. Vital Health Stat 2. 1999;No. 128:1–13. [PubMed] [Google Scholar]
- 11.Pastor P, Makuc DM, Reuben C, Xia H. Trends in Health of Americans Chartbook. Health, United States, 2002. Hyattsville, Md: National Center for Health Statistics; 2002.
- 12.US Dept of Health and Human Services. Healthy People 2000: National Health Promotion and Disease Prevention Objectives. Washington, DC: US Public Health Service; 1991.
- 13.Stoto MA, Durch JS. National health objectives for the year 2000: the demographic impact of health promotion and disease prevention. Am J Public Health. 1991;81:1456–1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Center for Health Statistics. Healthy People 2000 Final Review. Hyattsville, Md: US Public Health Service; 2001.
- 15.National Center for Health Statistics. Health, United States, 2002. Hyattsville, Md: National Center for Health Statistics; 2002.
- 16.Keppel KG, Pearcy JN, Wagener DK. Trends in racial and ethnic-specific rates for the Health Status Indicators: United States, 1990–98. In: Healthy People Statistical Notes, No. 23. Hyattsville, Md: National Center for Health Statistics; January2002. [PubMed]