Abstract
The classification of disease burdens is an important topic that receives little attention or debate. One common classification scheme, the broad cause grouping, is based on etiology and health transition theory and is mainly concerned with distinguishing communicable from noncommunicable diseases. This may be of limited utility to policymakers and planners. We propose a broad care needs framework to complement the broad cause grouping. This alternative scheme may be of equal or greater value to planners. We apply these schemes to disability-adjusted life year estimates for 2000 and to mortality data from Tanzania. The results suggest that a broad care needs approach could shift the priorities of health planners and policymakers and deserves further evaluation.
HOW DISEASE BURDENS ARE characterized and categorized in terms of broad groupings is an important issue that receives little attention or debate. The application of conventional broad cause groups (i.e., communicable, noncommunicable, and injuries) to the disease burden determines much of the field on which important debates in international health are conducted. The broad cause view of disease burdens in developing countries has informed both influential policy recommendations that poor countries invest solely in communicable disease reduction to achieve the greatest future health returns,1 and potent warnings that noncommunicable diseases loom as “tomorrow’s pandemics” in the developing world.2
The time is ripe for challenging the conventional categories underlying these discussions. A move away from groupings based on causes to ones that stress the effects and care needs of disease burdens would be instructive. Perhaps more importantly, they may be of greater intrinsic use for high-level public health policy and services planning. Our concerns echo recent calls for a reassessment of models of health care delivery that move away from a narrow focus on acute, episodic treatment to ones that more closely reflect the increasing burden of conditions requiring long-term care and management regardless of etiology.3
To illustrate our point, we present a simple broad care needs scheme for categorizing the burden of disease. We then apply both the conventional broad cause scheme used in the 1990 Global Burden of Disease (GBD) study4,5 and the proposed needs-oriented scheme to 2 sets of data: GBD disability-adjusted life year (DALY) estimates for sub-Saharan Africa for 2000, and community-based data on cause-specific mortality from a rural district in the United Republic of Tanzania for 2000.
CONCERNS ABOUT THE BROAD CAUSE SCHEME
Chief among the aims of the GBD 1990 study was to inform health policy and decisionmaking. Its authors used a broad classification of diseases based on etiology, epidemiological risks, and epidemiological transition theory6 to provide a simplified bird’s eye view of the many conditions constituting the total disease burden. The 3 GBD groups are:
Group I: Communicable, maternal, perinatal, and nutritional conditions
Group II: Noncommunicable diseases
Group III: Injuries
Broad cause groups formulated in this way have been used to provide overarching descriptions of the type of health care and preventive measures required for the conditions within those groups.1 The typical group I condition, for example, is a classic infectious illness requiring acute, episodic, and (depending on severity) short-term hospital care.
Of particular concern is the distinction between broad cause groups I and II. The distinction between these groups, based as it is on the causes rather than the effects of disease, provides a weak compass for setting high-level planning and priority directions and may lead decisionmakers astray in predicting the types of health intervention and care that will be needed by the populations they serve.3 Although HIV/AIDS and tuberculosis may be infectious in nature (i.e., group I conditions), their management has much more in common with that of severe stroke (group II) than measles (group I). Conversely, treatment of appendicitis (group II) is more similar to that of bacterial meningitis (group I) than to that of lung cancer (group II).
The use of the broad cause scheme without a broad care needs perspective to complement it could perpetuate a misapprehension about where today’s care needs actually lie in many developing countries.
A BROAD CARE NEEDS CLASSIFICATION FOR HEALTH PLANNERS
We propose a simple alternative classification based on a 2-axis health effects or care needs orientation. Two of the most fundamental criteria for discriminating between the effects of different illnesses on individuals and the resulting demands on health services are (1) the length of time they produce ill health in an individual (chronicity) and (2) their relative likelihood of causing death (mortality).
Other aspects of particular illnesses, such as the availability of cost-effective preventive interventions or likelihood of disablement and the typical age at which patients are afflicted by the illness will also affect the implied need for health services. However, for the purposes of simplicity, we have limited our care needs classification criteria to the 2 parameters of chronicity and mortality. We divided these parameters into 2 groups. All major disease conditions were rated as either acute or chronic along 1 axis, and as having a low or high mortality along the other. The combination of these categories yields a 4-way effect-oriented broad care needs classification scheme: (1) acute care needs, with low- and highmortality subgroups, and (2) long-term care and management needs, with low- and highmortality subgroups (see Table 1 ▶ for definitions).
TABLE 1—
Criteria for Broad Care Needs Classification of Disease Groups
| Chronicity | ||
| Likelihood of Mortality | Acute | Chronic |
| Low | Potentially curable with > 1 mo of current appropriate treatment and < 20% chance of mortality within 1 mo if untreated | Either incurable or requires > 1 mo of appropriate treatment and < 5%/y chance of developing an intercurrent episode or acute illness associated with the chronic condition, with > 20% chance of mortality within 1 mo if untreated |
| High | Potentially curable with > 1 mo of current appropriate treatment and > 20% chance of mortality within 1 month if untreated | Either incurable or requires > 1 mo of appropriate treatment and < 5%/y chance of developing an intercurrent episode or acute illness associated with the chronic condition, with > 20% chance of mortality within 1 mo if untreated |
OUR APPROACH
Comparison Using GBD 2000 DALY Estimates for Sub-Saharan Africa
Two physicians reclassified selected causes of public health importance in Africa from the 1990 GBD study into the care needs scheme. The reclassification was based on their knowledge of the typical clinical course of each disease group. It is acknowledged that the chronicity and mortality risks of some diseases differ in different settings. We have not attempted to take this into account in this illustrative exercise. Conditions placed under the 4 different categories shown in Table 1 ▶ are available from the authors. When assigning disease groups that include several subgroups of conditions, we attempted to achieve a best fit for the disease group in question. Some specific disease groups included conditions that fell into different categories within the effect-oriented scheme (e.g., digestive diseases included appendicitis [acute care need, high mortality] and cirrhosis [long-term care need, high mortality]). In these situations we classified groups according to the most common disease in that group in the GBD study estimates. Years of life lost (YLLs) due to injuries were assigned to the acute care need, high-mortality category. Years lived with disability (YLDs) due to injuries were classified as chronic care need, low mortality. We then abstracted the predicted number of DALYs for each category from the GBD estimates and tabulated them. The results are compared with the 2000 broad cause estimates for the same list of causes, as published in the original study.4
It should be noted that we did not include in our analysis diseases or disease groups classified as acute care need, low mortality. Although such diseases are responsible for a significant proportion of a health service’s workload, they do not represent a high number of lost DALYs. Also, for the sake of brevity, results are presented for 2 age groups only: (1) children younger than 5 years and (2) the remainder of the population.
Comparison Using Data From Tanzania
The comparison was repeated using data from the Tanzanian Ministry of Health’s National Sentinel System of linked demographic surveillance sites. Since 1992, the Adult Morbidity and Mortality Project has been facilitating the establishment of this system and has engaged in demographic and cause-specific mortality surveillance among rural and urban populations amounting to approximately 1% of the total national population.7 These data are regarded as one of the only reliable sources of longitudinal population-based mortality data in Africa.8 Methods of data collection and surveillance areas have previously been described.9 Briefly, they include the annual re-enumeration of the population under surveillance in the rural areas, semiannual re-enumeration in the urban area, and networks of village and neighborhood reporters who record incident deaths on a continuous basis. Trained health care workers follow up each death in the surveillance areas and administer a verbal autopsy interview with the kin and carers of the deceased person. When they are available from the household, data from medical records are abstracted. Probable cause of death is attributed using a list of causes derived from the International Statistical Classification of Diseases, 10th Revision.10 A panel of 3 physicians assigns the cause. Coders are blind to each other’s diagnosis, and cause of death is assigned when 2 coders agree. A cause is assigned in more than 90% of cases.
Only mortality data (deaths and YLLs) are available. Data from Morogoro District for 2000 were selected for presentation. Of the 3 current sentinel sites in Tanzania, Morogoro has the highest proportion of deaths with group I causes and therefore represents a good test case for the comparison of disease burden categorization schemes. YLLs were calculated with the formula published in the 1990 GBD study. We categorized causes of death available from the project into 1990 GBD broad cause categories following that source, and into the broad care needs classification scheme using the criteria previously described.
OUR RESULTS
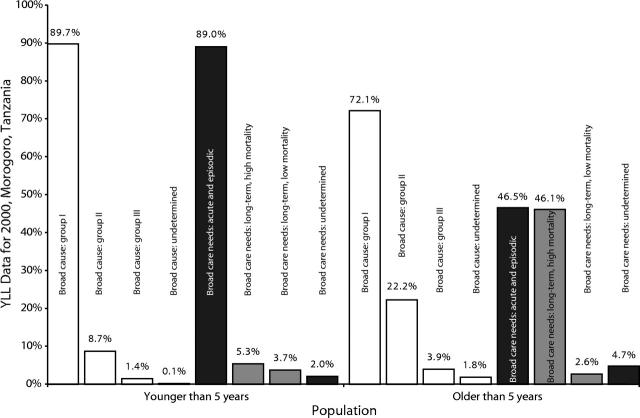
Figure 1 ▶ compares the percentage of estimated DALYs for 2000 attributable to the broad cause and broad care needs classification schemes. Group I causes predominated among children younger than 5 years (86% of DALYs). According to the broad care needs scheme, a similar but smaller proportion of DALYs were lost to conditions requiring acute or episodic care. Only 7% of lost DALYs in children were due to noncommunicable (group II) diseases. However, taking a broad care needs perspective suggests that over one fifth (23%) of lost DALYs expected among children in 2000 were from conditions needing long-term care and management.
FIGURE 1—
Percentage of disability-adjusted life years (DALYs) owing to broad cause and broad care needs conditions (estimates for 2000).
Note. White bars = broad cause groups; black bars = broad care needs (acute care and undetermined); gray bars = broad care needs (long-term care and management).
In the rest of the population, 35% of lost DALYs were from group I causes. An equal proportion of lost DALYs among the population older than 5 years were from the group II set of conditions, whereas injuries and accidents accounted for 30%. From a care needs perspective, just 14% of DALYs lost were expected to be due to conditions needing acute care services, as opposed to 86% of DALYS attributable to conditions requiring long-term care and management. Note that HIV and tuberculosis are classified as group I conditions in the GBD study but are classified as high mortality and requiring long-term care and management in the effectorientated classification.
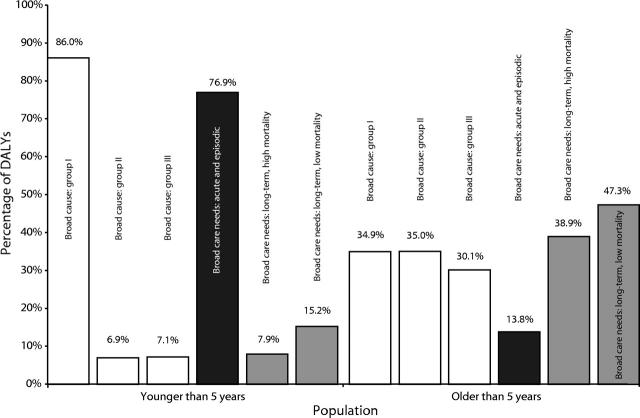
Figure 2 ▶ applies the classification schemes to mortality data from Tanzania. Among children, very similar proportions were observed in the group I and acute care needs groups (90% and 89%, respectively). The percentage (9%) of group II conditions matched the 10% of the disease burden among children needing long-term care; less than 2% of the mortality burden in children was due to group III conditions.
FIGURE 2—
Percentage of years of life lost (YLLs) due to broad cause and broad care needs conditions (Morogoro, Tanzania, 2000).
Note. White bars = broad cause groups; black bars = broad care needs (acute care and undetermined); gray bars = broad care needs (long-term care and management).
In the remainder of the population, group I causes of death predominated (72% of YLLs), with most of the remainder (22%) attributed to noninfectious group II conditions. This contrasts with a care needs perspective in which 44% of YLLs were due to conditions needing acute and episodic health care, whereas just under half of all mortality (49%) was caused by diseases needing long-term care and management.
DISCUSSION
In writing this article, we have sought to stimulate debate about the broad categorization of disease burdens in developing countries by proposing a simple alternative to the conventional cause-based scheme. We have also tried to point out how different categorization schemes might lead planners to divergent conclusions about where high-level service priorities may lie. In doing so, we hope to stimulate further development of useful approaches to the categorization of disease burdens for different audiences, including policymakers and planners. In particular, there is a growing need for understanding and debating how priorities are set at the local or district level. This level is increasingly where initial planning and decisionmaking take place in the era of decentralization and health reform. At all levels, there is a need for more and better sources of data, however one may group and categorize them. New information techniques such as sentinel demographic surveillance may contribute to filling these gaps.
Two main points are suggested by this exercise. First, the effect-oriented broad care needs scheme applied to both DALY estimates and YLL data suggests that radically different approaches to health care are needed for the populations younger than and older than 5 years in Africa. As some recent high-profile publications suggest,11 the conventional policy interpretation of a high burden in the GBD broad cause group I is that health care priorities be placed on services for communicable diseases requiring acute and episodic care. Our analysis has shown that this interpretation may hold for the disease burden in children younger than 5 years, but for the majority of the population it may well lead in some wrong directions. When the disease burden is regrouped in such a way as to specifically reflect the care needs implied by acute versus chronic conditions, this conventional interpretation is materially changed.
Infants and younger children are burdened by conditions needing acute and episodic care, whereas the majority of the population (who are older than age 5 years) clearly need a health system that can provide long-term care and management. Among women, diseases categorized as chronic account for 75% of deaths and 83% of DALYs. Among men they account for 64% of deaths and 96% of DALYs. These differences largely reflect the fact that men are more likely to suffer serious injuries. Therefore, deaths from external causes and years lived with the disabling effects of injury are both more common in men. In addition, maternal mortality and illness substantially influence total female DALYs lost. This suggests even more strongly the need to provide services for the management of chronic conditions in health systems in Africa.
The health policy and health care requirements for chronic conditions are substantially different from those for acute conditions, whatever their etiology. Chronic conditions require the ability of a health system to deliver treatment over a prolonged period of time. Patient education with the aim of promoting long-term behavioral change is usually a feature of care, and for most chronic conditions the aim is management rather than cure.
Second, the effect-oriented classification provides a relatively easy method for assessing the need for broad types of care. Because it does not require an in-depth understanding of the underlying abnormality and detailed management of particular diseases, it could easily be used by health policymakers and planners from nonclinical backgrounds. A greater burden of disease caused by chronic illnesses implies a greater need for the type of innovative care called for by the World Health Organization and also implies the need for a greater emphasis on preventive programs and services.
The 2 classification schemes compared in this paper are not mutually exclusive. The broad cause classification remains an informative way of summarizing the impact of major types of causes on differences in disease patterns over time and between populations. A classification based on acuteness-chronicity should better serve the needs of health care policymakers and planners. It is a matter of choosing the most appropriate classification for a given use.
We have illustrated how a classification based on chronicity and mortality could be useful to health care policymakers and planners, particularly for patients older than 5 years. Clearly, further work on this approach would be required before it could be adopted. This would include detailed modeling of the potential costs and health benefits of using such a framework for policy decisions. We hope that others will be encouraged to contribute to this work.
Acknowledgments
This article is, in part, an output of the Adult Morbidity and Mortality Project (AMMP). AMMP is a project of the Tanzanian Ministry of Health and local councils, funded by the UK Department for International Development (DFID) and implemented in partnership with the University of Newcastle upon Tyne. The views expressed are not necessarily those of DFID. The authors also thank the District Councils and residents of Hai, Igunga, and Morogoro Districts, and Ilala, Kigoma, and Temeke Municipalities.
The following individuals are members of the AMMP Team, without whose work this publication would not have been possible: KGMM Alberti, Richard Amaro, Gregory Kabadi, Berlina Job, Judith Kahama, Joel Kalula, Ayoub Kibao, John Kissima, Regina Kutaga, Mary Lewanga, Frederic Macha, Haroun Machibya, Mkamba Mashombo, Godwill Massawe, Gabriel Masuki, Louisa Masayanyika, Ali Mhina, Veronica Mkusa, Ades Moshy, Hamisi Mponezya, Robert Mswia, Deo Mtasiwa, Ferdinand Mugusi, Samuel Ngatunga, Mkay Nguluma, Peter Nkulila, Seif Rashid, JJ Rubona, Asha Sankole, Daudi Simba. The authors also thank the District Councils and residents of of Hai, Igunga, and Morogoro Districts, and Ilala, Kigoma, and Temeke Municipalities.
Human Participant Protection Mortality data were obtained from a Tanzanian Ministry of Health development project. Ethical clearance was not required or sought for the mortality surveillance component. All project activities were overseen by the Tanzanian Ministry of Health and representatives of local government.
Contributors P. Setel and N. Unwin conceived the article. N. Unwin, L. Saker, and P. Setel designed the analysis. L. Saker, D. Whiting, N. Unwin, P. Setel, Y. Hemed, and H. Kitange participated in data preparation and carried out the analysis. P. Setel, L. Saker, and N. Unwin wrote the article, and Y. Hemed, D. Whiting, and H. Kitange assisted in editing and revision.
Peer Reviewed
References
- 1.Gwatkin DR, Guillot M. The Burden of Disease Among the Global Poor. Current Situation, Future Trends, and Implications for Strategy. Washington DC: The World Bank; 2000.
- 2.Alberti KGMM. Noncommunicable diseases: tomorrow’s pandemics. Bull World Health Organ. 2001;79:907. [PMC free article] [PubMed] [Google Scholar]
- 3.Innovative Care for Chronic Conditions: Building Blocks for Action. Geneva, Switzerland: World Health Organization; 2002.
- 4.Murray CJL, Lopez AD, eds. The Global Burden of Disease. Boston, Mass: The Harvard School of Public Health on behalf of the World Health Organization and the World Bank; 1996.
- 5.Murray CJL, Lopez AD. Global Health Statistics. Boston, Mass: The Harvard School of Public Health on behalf of the World Health Organization and the World Bank; 1996.
- 6.Murray CJL, Lopez AD. Estimating causes of death: new methods and global and regional applications for 1990. In: Murray CJL, Lopez AD, eds. The Global Burden of Disease. Boston, Mass: The Harvard School of Public Health on behalf of the World Health Organization and the World Bank; 1996:117–200.
- 7.The Policy Implications of Adult Morbidity and Mortality. End of Phase 1 Report. Dar es Salaam, United Republic of Tanzania: Ministry of Health and AMMP Team; 1997.
- 8.Lopez AD, Salomon J, Ahmad O, Murray CJL, Mafat D. Life Tables for 191 Countries: Data, Methods and Results. Geneva, Switzerland: World Health Organization; 1999. GPE Discussion Paper Series, No. 9.
- 9.Setel P, Hemed Y, Unwin N, Alberti K, for the AMMP Team. Six-year cause-specific adult mortality in Tanzania: evidence from community-based surveillance in three districts 1992–1998. MMWR Morb Mortal Wkly Rep. 2000;49:416–419. [PubMed] [Google Scholar]
- 10.International Statistical Classification of Diseases and Related Health Problems. 10th rev. Vol 2. Geneva, Switzerland: World Health Organization; 1993.
- 11.Gwatkin DR, Guillot M, Heuveline P. The burden of disease among the global poor. Lancet. 1999;354:586–589. [DOI] [PubMed] [Google Scholar]