Abstract
Summary measures of population health, such as health-adjusted life expectancy, are increasingly being used to monitor the health status of regions and to evaluate public health interventions. Such measures are based on aggregated indicators of individual health and summarize health in a population. They describe population health status but have limitations in analytic studies of population health.
We propose a broader framework for population health measurement. This classifies indicators according to their application (descriptive, prognostic, or explanatory), according to the conception of population (as an aggregate or a dynamic entity), and according to the underlying model of health. This approach extends the measurement repertoire to include indicators of the health of a population.
THE EMERGING FIELD OF population health has been influenced by a variety of academic traditions, and this has led to a diversity of approaches and considerable debate over definitions and conceptual models, as reviewed in recent articles.1–5 At the same time, growing attention has been paid to measuring population health status, largely stimulated by the World Health Organization’s reviews of health system performance.6,7 Our thesis is that current approaches measuring population health do not adequately reflect the complexities of recent thinking in the field, and that a more detailed classification of population health measures is required.
Any approach to measuring population health will reflect how it is defined. There are currently 2 contrasting approaches to definition, leading Kindig and Stoddart2 to acknowledge that there can be no definitive measure of population health, arguing that “the development and validation of such measures for different purposes is a critical task for the field of population health research.”2(p381) Of the 2 approaches to defining population health, the first simply takes it as a shorthand for the health status of a population, sometimes also considering the equity of the distribution of health in the population.2 We will refer to this as the descriptive model of population health. For this model, measures of health status such as health-adjusted life expectancy will be sufficient, supplemented by indicators of disparity in health status. However, this approach to defining population health is limited and does not adequately capture its scope as an academic field of study; it is akin to defining economics as the study of gross national product, without any theory of economic forces of production. Hence, a second definition views population health as a broad conceptual approach to understanding (and perhaps also intervening upon) the determinants of health status.2 This analytic model of population health refers to a conceptual and analytic approach to explaining why some people are healthy and others are not4,8; at its broadest, it seeks to analyze not only how this occurs, but also why.5 This conception demands a much broader measurement protocol that includes not only outcome variables in terms of morbidity and mortality indexes, but also direct measures of health processes within the population. We do not here argue for 1 model over the other, for both have merit. Instead, our argument is that we should set out a full array of measures, classifying them into those that fit the descriptive model and those that are relevant to the conception of population health as a broader, analytic field of study.
MEASUREMENT DESIGNS SHOULD REFLECT THEIR PURPOSE
Recent discussion of population health measures has focused on how best to combine indicators of mortality and morbidity. From early work in the 1960s and 1970s,9–12 a general approach to establishing a set of summary indicators of population health outcomes has emerged.7,13 These suit the descriptive model of population health but are inadequate for the analytic conception. This can be illustrated by considering the potential range of applications for population health measures.
We may distinguish 4 applications of health measures, and the design of the measure will be different for each application. This holds for individual and for population-level measures. First, scales such as disability indexes describe current health status and are principally relevant to the descriptive model of population health. Health status measures are used in surveys or as diagnostic tools for individuals, and (with additional information) in estimating needs for care, or disease burden in groups of people. In a second application, predictive, or prognostic, measures look forward in time to anticipate future health status: screening tests or indicators of risk and prognosis for individuals, and general demographic projections of disease burden at the population level. This extends descriptive measures to consider sustainability: we should not regard as equal 2 populations with the same current health status if 1 population is unlikely to maintain that level (due, perhaps, to personal risk profiles, environmental factors, or political instability).14 In the third application, measures are used for explanation. This is chiefly relevant to the analytic model of population health and addresses why some people are healthy and others are not.15 These are similar to predictive measures, but for explanation the implicit time dimension is retrospective. At the individual level, they might include exposures, genetic factors, or even facets of personality. At the population level, explanatory indicators might include social determinants of health such as income inequality or social cohesion. The fourth application includes evaluation, in which measures again record current health status but differ from descriptive measures in being sensitive to small changes in health; they typically use continuous numerical scales. Evaluative instruments record outcomes of interventions at the individual level and monitor the creation and impact of programs or policies at the societal level.
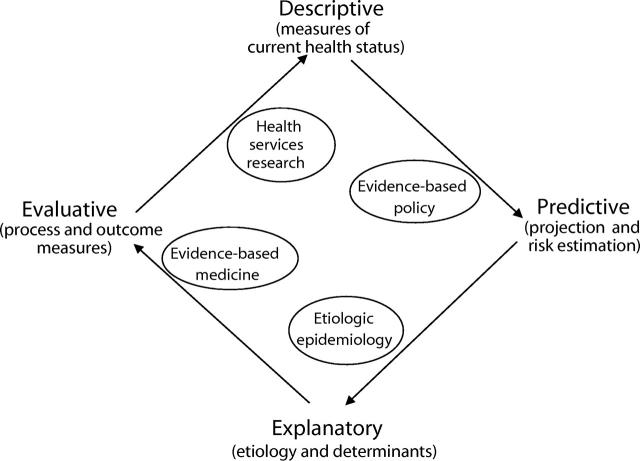
We have presented these 4 applications in a sequence that follows the logic of health research.16 We begin with studies of current and projected future health status to identify important population health issues, then proceed to analytic stages that inform the design of interventions, and finally proceed to studies that evaluate those interventions (Figure 1 ▶). Rarely would measures of all 4 types be included in a single study; the placement of the ovals within the figure illustrates the blend of measurement approaches typically found in selected academic fields: evidence-based policy, for example, relies on predictive and, to a lesser extent, descriptive measures.
FIGURE 1—
Sequential presentation of applications of population health measurements, with illustrations of the fields of research for which each application (or blend of applications) is suited.
As well as classifying measures according to their purpose, one may arrange them hierarchically according to their level of aggregation. At the finest level, health indicators aggregate markers of body chemistry or physiological processes. At a broader level, they could summarize the functioning of a body system or a whole individual. They can also describe groups of people, as with morbidity rates, or complete social institutions, as with hospital process indicators. In discussing population health measures, Morgenstern17 helpfully distinguished between aggregate, environmental, and global indexes. Aggregate measures combine data from individuals, summarized regionally or nationally, as with rates of smoking or lung cancer. Environmental indicators cover factors external to the individual, such as air or water quality, but these can have analogues at the individual level (exposure levels), even though these may not often be assessed. By contrast, global indicators have no obvious analogue at the individual level. Examples include contextual variables such as policies promoting equity in access to care, or laws restricting smoking in public places.
Morgenstern’s categories of measures roughly correspond to differing purposes of population health research. Measures based on aggregated individual data are typically used in descriptive studies of health status as in a prevalence survey; they may also serve as outcome indicators in evaluative studies. They represent the descriptive model of population health. The focus is on the individuals within the population; the intention might, for example, be to evaluate a community health promotion program or to identify gaps in health services.13 In philosophical terms, these are idiographic or particularizing studies. Here the population forms a convenient context within which to analyze personal health, and the relevant indicators record “health in the population.”
Environmental measures are most commonly used in analytic or explanatory studies. These may also be idiographic if the goal is to understand how environmental factors influence the health of particular groups of people, as in occupational health research. Here, environmental indicators form the independent variables, whereas aggregate measures may be used to record health outcomes. Research of this type lies midway between the descriptive and analytic models of population health and corresponds to the “variables approach to analysis” criticized by Coburn et al.5 But analytic studies may also be more abstract, seeking to delineate general principles, such as the association between social capital or income inequalities and health. Generalizing, or nomothetic, studies of this type aim to generate theory. Here, global indicators represent the explanatory factors, and they can also form the outcome variables: for example, a study might examine how the political system influences social cohesiveness. As the research goal tends toward the explanatory and nomothetic, the population health measurements must include more than aggregated individual health indicators; the global indicators provide measures of the “health of a population.” Examples range from social cohesion or social capital to race relations. At the same time, this distinction between particularizing and generalizing studies introduces a contrast in ways that “population” may be conceptualized.
Most discussions of population health implicitly treat the population as an aggregation of individual people. In geographic presentations, populations are typically defined somewhat arbitrarily as the people living in a specified area. This aggregate model of population is adequate for descriptive studies, but as we move toward explanatory studies it may become relevant to focus on populations that form self-identifying groups, the “settings of everyday life” in Kickbusch’s term.3(p385) This echoes contemporary references to complexity theory and to emergent phenomena.18 In emergent conceptions of a population, membership in a particular group takes on importance as an influence on health5: a sense of community and feelings of belonging predict mutual support and are empirically related to health.19–21 In this dynamic sense of population, there is a purposive collaboration among members that makes them behave differently than they would outside that context. But because of these interactions, the functioning of the whole cannot be fully understood by dismantling it and examining its component parts, so in terms of an explanatory model of population health, measures must extend beyond aggregated individual indicators to include social, environmental, and global indicators. Before deciding which indicators to choose within these broad categories, we must first review alternative meanings of “health.”
EVOLVING DEFINITIONS OF HEALTH
Conceptions of health have changed through a succession of stages, which loosely reflect the current health issues facing societies as they develop. We measure things that are considered important and, in turn, topics that are measured and reported become a focus of attention, so the prevailing conception of health interacts with the indicators that record it. We may distinguish 3 dominant conceptualizations of health: the biomechanical model, the holistic model, and the wellness model. Although these were developed in reference to individual health, they can be applied to thinking about population health.
The biomechanical model
Although historically not the first, the biomechanical, or reductionistic, model of health dominated thinking in the 20th century. The body is viewed as a machine, to be fixed when broken. The focus lies on resolving health problems, so measurements focus on death, disease, disability, or distress. Applied to a population viewed as an aggregate, a healthy population would be one with low rates of disease. However, the mechanical metaphor could also be applied to the emergent model of population: a healthy society would be one in which the various systems (governmental, legal, medical) function smoothly and which is thereby equipped to deal with challenges.
The virtues of the mechanical model include its focus on issues of importance to society; it also offers an objective basis for measurement in that diseases can be readily diagnosed and classified. However, counting diseases and deaths is a negative way to measure health, and applied to the analytic conception of population health, the mechanical model sidesteps issues such as the fact that most who are exposed do not get sick. It also focuses on the present, and if prognosis is not considered relevant, there is little virtue in prevention or health promotion. In keeping with the dominance of this perspective, prevention has not played a prominent role in Western medicine.
The holistic model
The rise of noncommunicable diseases forced etiologic epidemiology to edge away from mechanistic models in which there was a single, necessary causal agent to more fluid conceptions with no necessary or sufficient factors, in which lifestyles and subjective factors played a central role. The holistic model of health that emerged emphasized its multidimensionality and incorporated the concept of positive health. Applied to a population, the holistic model might use aggregated individual indicators of well-being to indicate health in the population.6 Alternatively, it could record global measures that capture the distribution of individual indicators—equity—and extend to indicators of the well-being of the population as a whole, such as commitment to social development or concern over fairness. This approach is not yet being widely pursued.22
By focusing on issues such as active participation in life, the holistic model allows more subtle differentiation among people with disabilities, many of whom lead productive lives despite an impairment. The holistic model also has the advantage of allowing finer differentiation among people at the higher end of functioning. But by so doing, it risks incorporating much of life under the rubric of health, including factors such as vitality or creativity that lie “outside the skin.” Thus, the holistic model blurs the distinction between the state of being healthy and the consequences of being healthy; furthermore, it fails to draw a clear boundary between health and the determinants of health.
The dynamic model
These problems in setting boundaries arise if health is viewed as a state, as in the descriptive model of population health. A state is categorical and so must be defined in terms of a particular set of criteria. In 1986, the World Health Organization moved away from viewing health as a state toward a dynamic model that saw it as a process, a means rather than an end. To be healthy, in this conception, “an individual or group must be able to identify and to realize aspirations, to satisfy needs, and to change or cope with the environment. Health is, therefore, seen as a resource for everyday life, not the objective of living. Health is a positive concept emphasizing social and personal resources, as well as physical capacities.”23 According to this conception, a healthy population would be one whose institutions not only function harmoniously, but also balance the maintenance of personal freedom with environmental protection, ensuring that people live in balance with nature and each other. These themes correspond to our concept of health of a population and would be summarized by global health indicators: the level of mutual support among community members, fairness, volunteer participation rates, and so forth.
The dynamic view of health discards the linear thinking about cause and effect that characterized the mechanical model and moves toward a systems model in which health is seen as a force, as both input and output. The mechanical metaphor for health focused attention inward, on how things go wrong: from patient to organ, to cell. The dynamic model looks outward, proposing explanations for why diseases evolve and change over time. This corresponds to the analytic model of population health and involves the notion of agency implied in the emergent conception of population: it includes the circumstances and goals that animate the variables included in descriptive “box and line” models of population health.5
THE BROADENING SCOPE OF POPULATION HEALTH MEASURES
The implication of this discussion is that a measurement protocol for population health must include a broad set of measures that includes aggregate measures of health outcomes used for descriptive purposes, plus environmental and global measures of dynamic population characteristics used for predictive, analytic, and explanatory purposes. The current focus on summary measures is limited to the descriptive domain; it follows mechanical models of health and of population and does not countenance analytic or explanatory purposes of measurement.
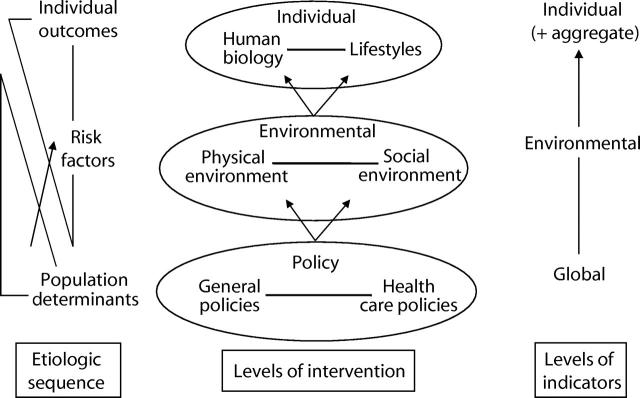
One way to establish a logical structure for such a set of measures is to base it on the etiologic sequence from underlying determinants to final individual health outcomes, and on the range of interventions that correspond to each etiologic stage. This sequence is illustrated in Figure 2 ▶. The underlying causal sequence is illustrated at the left of the figure, and the center column illustrates a range of public or population health interventions. These can directly target individuals (as with immunization campaigns) or modify the environment, or they may work through policy. At each level there is a spectrum of interventions, shown in the ellipses. The overlapping triangles suggest that although population determinants are chiefly addressed via policy interventions, environmental interventions may target risk factors at the population or individual levels. The arrows indicate the general temporal sequence. The right of the diagram outlines a general correspondence between the interventions and Morgenstern’s classes of measurement. From this we can see, for example, that using aggregated measures based on individuals to evaluate policy may provide a distal outcome but cannot offer an explanatory insight into the processes of change involved.
FIGURE 2—
The correspondence between population health measures and types of intervention to enhance health. Interventions may be directed at several levels (shown in the ellipses), and these correspond broadly to stages in the etiologic sequence (shown at the left of the diagram) and Morgenstern’s classification of population health indicators17 (shown at the right).
Our proposal is that the set of population health measures should cover this entire framework, while recognizing that in any particular study only a subset will be used. The objection that this is far too broad, making health include everything, was discussed by Kindig and Stoddart.2(p382) This criticism reflects the narrow definition of population health in terms of current health status and diverges from the general evolution toward recognizing the interrelatedness of health and other domains of society.3 It is this integrated approach to tackling the upstream roots of health problems that distinguishes population health from public health or community medicine. A focus only on indicators of health “within the skin” has the disadvantage that upstream interventions tend to be ignored as lying outside the health domain, consigning population health research to remaining at the level of describing what but not analyzing why. On the other hand, if we take a broad approach and include pollution, or equalopportunity legislation, as indicators of the health of a society and not as external determinants, this focuses attention on the health relevance of these issues.
IMPLICATIONS FOR POPULATION HEALTH MEASUREMENT
The first step in selecting a measure is to arrange the vast array of potential indicators into a framework that clarifies their appropriateness for various purposes. Table 1 ▶ first classifies measures under our contrasting models of health: biomechanical versus holistic or dynamic models (the latter 2 models have been combined for clarity). These roughly correspond to the applications of measures so that, in general, measures that follow the biomechanical model of health are best suited to descriptive or evaluative studies, whereas analytic and prognostic indicators typically correspond to a dynamic model of health. In the columns of the table, measures are classified by the conceptual approach taken to defining population. The cells of the table offer arbitrary illustrations of possible indicators; this is in no way intended as an exhaustive listing, and the actual choice of indicators must be influenced by local considerations including the current level of health, and social and political priorities and values. We also acknowledge that many indicators can serve more than 1 purpose and so could be placed in different cells of the table.
TABLE 1—
A Classification of Themes Represented in Population Health Measurements, Showing Examples of Possible Indicators
| Conception of Population (What to Measure) | |||
| Model of Health | Purpose of Measurement (Why Measure?) | As an Aggregate of Individuals (Health in the Population) | As an Emergent Phenomenon (Health of the Population) |
| Biomechanical model | Descriptive | Mortality and morbidity | Environmental indicators of health status (e.g., water, air quality) |
| Generic health measures from surveys | Global indicators (e.g., social solidarity; sense of identity; artistic output, public interest in health issues) | ||
| Crime rates | |||
| Evaluative | Disease-specific care outcomes based on hospital or clinic records | Indicators of social interactions: changing patterns of crime, club memberships | |
| Existence of clear policies concerning environmental quality (e.g., water, air quality) | |||
| Change scores in pre- and poststudies | Routine monitoring of environmental quality | ||
| Holistic/dynamic model | Predictive | Screening for early disease | Scope of, and access to, social and mental health institutions |
| Population genetic profiling | Health promotion activities; healthy cities movements | ||
| Risk factor rates (e.g., smoking, obesity, exercise) | Indicators of societal support: the “safety net” | ||
| Individual resiliency | Social interactions and networks | ||
| Interpersonal support | Volunteerism, mutual aid | ||
| Social programs | |||
| Analytic | Genetic and risk profiles | Social cohesion, neighbourhood quality, social capital | |
| Risk factor rates (e.g., smoking, obesity, exercise) | Health policies and funding | ||
| Quality of social institutions for health (e.g., health protection laws; environmental quality; hospitals) | |||
This classification is intended to remind us that the purpose of making a measurement should determine the choice of conceptual model and guide the selection of indicators. It points to the wide variety of possible measures of population health and links indicators to the implicit conceptual model of population health being taken. The first row of the table represents the typical scope of measures in the descriptive model of population health. Use of the broader dynamic model, however, implies that we should include prognostic indicators to anticipate future needs. They may be set in a hierarchy from proximal to underlying, the indicators being chosen to reflect the relations about which we are most certain and that focus on themes addressed by health interventions.
Most important, the framework portrayed in Table 1 ▶ suggests that we extend our measurement repertoire beyond aggregated individual indicators. Indicators of current health status give surface representations of processes within the population that form the core of population health. Reliance on aggregated individual indicators portrays an image of a paternalistic health system that promotes the well-being of essentially passive people: patients being treated by professionals or the masses protected by a benign public health system. The dynamic view focuses on the responsibility and capacity of a population to help itself; internal resources, rather than external, are most effective in improving health. Summary measures based on aggregated individual indicators may describe, but cannot analyze or explain, these processes central to population health.
Acknowledgments
B. Kristjansson was supported by a postdoctoral fellowship from the Canadian Institutes of Health Research.
Human Participant Protection No protocol approval was necessary for this study.
Contributors R. A. Spasoff, B. Kristjansson, and I. McDowell drafted the article. All the authors participated in discussions of the content and in revising the text.
Peer Reviewed
References
- 1.Friedman DJ, Starfield B. Models of population health: their value for US public health practice, policy, and research. Am J Public Health. 2003;93:366–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kindig D, Stoddart GL. What is population health? Am J Public Health. 2003;93:380–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kickbusch I. The contribution of the World Health Organization to a new public health and health promotion. Am J Public Health. 2003;93:383–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Glouberman S, Millar J. Evolution of the determinants of health, health policy, and health information systems in Canada. Am J Public Health. 2003;93:388–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coburn D, Denny K, Mykhalovskiy E, McDonough P, Robertson A, Love R. Population health in Canada: a brief critique. Am J Public Health. 2003;93:392–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murray CJL, Salomon JA, Mathers CD, Lopez AD. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications. 1st ed. Geneva, Switzerland: World Health Organization; 2002.
- 7.Murray CJL, Lopez AD. Evidence-based health policy—lessons from the Global Burden of Disease study. Science. 1996;274:740–743. [DOI] [PubMed] [Google Scholar]
- 8.Evans RG, Stoddart GL. Consuming research, producing policy? Am J Public Health. 2003;93:371–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sullivan DF. Disability Components for an Index of Health. Washington, DC: US Department of Health, Education, and Welfare, National Center for Health Statistics; 1971. Data Evaluation and Methods Research Series 2, No. 42. Public Health Service Publication 1000. [PubMed]
- 10.Chiang CL. An index of health: mathematical models. Vital Health Stat 2. 1965; No. 5. [PubMed]
- 11.Chiang CL. Making annual indexes of health. Health Serv Res. 1976;11:442–451. [PMC free article] [PubMed] [Google Scholar]
- 12.Chen MK. The G index for program priority. In: Berg RL, ed. Health Status Indexes. Chicago, Ill: Hospital Research and Educational Trust, 1973:28–34.
- 13.Murray CJL, Salomon JA, Mathers CD. A critical examination of summary measures of population health. In: Murray CJL, Salomon JA, Mathers CD, Lopez AD, eds. Summary Measures of Population Health: Concepts, Ethics, Measurement and Applications. Geneva, Switzerland: World Health Organization, 2002:13–40.
- 14.Murray CJL, Salomon J, Mathers C. A critical examination of summary measures of population health. Bull World Health Organ. 1999;78:981–994. [PMC free article] [PubMed] [Google Scholar]
- 15.Young TK. Population Health: Concepts and Methods. Oxford, England: Oxford University Press; 1998.
- 16.Tugwell P, Bombardier C. A methodologic framework for developing and selecting endpoints in clinical trials. J Rheumatol. 1982;9:758–762. [PubMed] [Google Scholar]
- 17.Morgenstern H. Ecologic studies in epidemiology: Concepts, principles, and methods. Annu Rev Public Health. 1995;16:61–81. [DOI] [PubMed] [Google Scholar]
- 18.Casti JL. Searching for Certainty: What Scientists Can Know About the Future. New York, NY: William Morrow; 1990.
- 19.Kawachi I, Kennedy BP. Health and social cohesion: why care about income inequality? BMJ. 1997;314:1037–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51:843–857. [DOI] [PubMed] [Google Scholar]
- 21.Blane D, Brunner R, Wilkinson R, eds. Health and Social Organization: Towards a Health Policy for the Twenty-First Century. 1st ed. London, England: Routledge; 1996.
- 22.Hancock T, Labonte R, Edwards R. Indicators that count! Measuring population health at the community level. Can J Public Health. 1999;90(suppl 1):S22–S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. Health Promotion: a Discussion Document on the Concept and Principles. Copenhagen, Denmark: WHO Regional Office for Europe; 1984.