Abstract
Objectives. We examined the longitudinal effects of a Housing First program for homeless, mentally ill individuals’ on those individuals’ consumer choice, housing stability, substance use, treatment utilization, and psychiatric symptoms.
Methods. Two hundred twenty-five participants were randomly assigned to receive housing contingent on treatment and sobriety (control) or to receive immediate housing without treatment prerequisites (experimental). Interviews were conducted every 6 months for 24 months.
Results. The experimental group obtained housing earlier, remained stably housed, and reported higher perceived choice. Utilization of substance abuse treatment was significantly higher for the control group, but no differences were found in substance use or psychiatric symptoms.
Conclusions. Participants in the Housing First program were able to obtain and maintain independent housing without compromising psychiatric or substance abuse symptoms.
Current rates of homelessness in New York City are the highest ever documented.1 A small percentage of this population remains chronically homeless, either living on the streets or other public places or intermittently using emergency rooms, shelters, jails, and other short-term services, but never successfully ending their homelessness.2 Members of this chronically homeless group typically have a history of mental illness,3 compounded by substance use disorders.4,5,6 Although much is known about the chronically homeless, these individuals continue to elude existing program efforts.
The predominant service delivery model designed to address the needs of this chronically homeless population, called the Continuum of Care, consists of several program components. It begins with outreach, includes treatment and transitional housing, and ends with permanent supportive housing. The purpose of outreach and transitional residential programs is to enhance clients’ “housing readiness” by encouraging the sobriety and compliance with psychiatric treatment considered essential for successful transition to permanent housing. This approach assumes that individuals with severe psychiatric disabilities cannot maintain independent housing before their clinical status is stabilized. Furthermore, the model presumes that the skills a client needs for independent living can be learned in transitional congregate living. Research in psychiatric rehabilitation indicates, however, that the most effective place to teach a person the skills required for a particular environment is within that actual setting.7
Consumers’ perception of the Continuum of Care offers another divergent perspective. Consumers experience the Continuum as a series of hurdles—specifically, ones that many of them are unable or unwilling to overcome. Consumers who are homeless regard housing as an immediate need, yet access to housing is not made available unless they first complete treatment. By leveraging housing on participation and treatment, continuum program requirements are incompatible with consumers’ priorities and restrict the access of consumers who are unable or unwilling to comply with program terms.
In addition, most consumers prefer to live in a place of their own rather than in congregate specialized housing with treatment services on-site.8,9 Most programs have rules that restrict clients’ choices and that when violated are used as grounds for discharging the consumer from the program. For example, despite having attained permanent housing, clients who relapse and begin to drink mild or moderate amounts of alcohol, may be evicted if the program has strict rules about sobriety maintenance. The chronically homeless population is characterized by its frequent inability to gain access to existing housing programs. Individuals in this group often have multiple disabling conditions, especially psychiatric conditions and substance abuse.10 Most programs are poorly equipped to treat people with dual diagnoses, let alone prepared to address their housing needs.11 Treatment requires time and commitment and is often not available if a program is under pressure to move clients along a continuum.12
The loss of control over one’s life resulting from housing instability, frequent psychiatric hospitalizations, and intermittent substance abuse treatment leaves some consumers mistrustful of the mental health system and unwilling to comply with demands set by providers.13 Others prefer the relative independence of life on the streets to a fragmented treatment system that inadequately treats multiple diagnoses or addresses housing needs.14,15 Paradoxically, consumers’ reluctance to use traditional mental health and substance abuse services as a condition of housing only confirms providers’ perceptions that these individuals are “resistant” to treatment, not willing to be helped, and certainly not ready for housing.16
The Housing First model was developed by Pathways to Housing to meet the housing and treatment needs of this chronically homeless population. The program is based on the belief that housing is a basic right and on a theoretical foundation that includes psychiatric rehabilitation and values consumer choice.17 Pathways is designed to address the needs of consumers from the consumer’s perspective.18 Pathways encourages consumers to define their own needs and goals and, if the consumer so wishes, immediately provides an apartment of the consumers’ own without any prerequisites for psychiatric treatment or sobriety. In addition to an apartment, consumers are offered treatment, support, and other services by the program’s Assertive Community Treatment (ACT) team. ACT is a well defined community based interdisciplinary team of professionals that includes social workers, nurses, psychiatrists, and vocational and substance abuse counselors who are available to assist consumers 7 days a week 24 hours a day. The Pathways program has made two modifications to the standard ACT model: a nurse practitioner was included to address the considerable number of health problems, and a housing specialist was added to coordinate the housing services. Although housing and treatment are closely linked, they are considered separate domains, and consumers in the program may accept housing and refuse clinical services altogether without consequences for their housing status. There are 2 program requirements: tenants must pay 30% of their income (usually Supplemental Security Income [SSI]) toward the rent by participating in a money management program, and tenants must meet with a staff member a minimum of twice a month. These requirements are applied flexibly to suit consumers’ needs.21
Consistent with the principles of consumer choice, Pathways uses a harm-reduction approach in its clinical services to address alcohol abuse, drug abuse, and psychiatric symptoms or crises. At its core, harm reduction is a pragmatic approach that aims to reduce the adverse consequences of drug abuse and psychiatric symptoms.22 It recognizes that consumers can be at different stages of recovery and that effective interventions should be individually tailored to each consumer’s stage.23 Consumers are allowed to make choices—to use alcohol or not, to take medication or not—and regardless of their choices they are not treated adversely, their housing status is not threatened, and help continues to be available to them.
Continuum of Care supportive housing programs subscribe to the abstinence–sobriety model based on the belief that without strict adherence to treatment and sobriety, housing stability is not possible. But studies examining the model’s effectiveness report only modest results in achieving housing stability for individuals who are chronically homeless and mentally ill.24 Alternatively, the approach used by the Pathways program assumes that if individuals with psychiatric symptoms can survive on the streets then they can manage their own apartments. The program posits that providing a person with housing first creates a foundation on which the process of recovery can begin. Having a place of one’s own may—in and of itself—serve as a motivator for consumers to refrain from drug and alcohol abuse.
The purpose of this study was to compare the effectiveness of the Housing First model with that of programs that used the Continuum of Care model for individuals who are chronically homeless and mentally ill.
We tested the following hypotheses: (1) the experimental (Housing First) group would report greater consumer choice over time than the control (Continuum of Care) group; (2) the experimental group would (a) exhibit lower rates of homelessness than the control group and (b) achieve and sustain greater residential stability than the control group; (3) the experimental group would exhibit rates of substance use similar to or lower than those of the control group; (4) the experimental group would participate in fewer substance-abuse treatments over time than the control group (i.e., because substance abuse treatment is not a precondition for the Housing First model, it is expected that there will be a lower rate of service utilization for the experimental group); and (5) the experimental group would exhibit rates of psychiatric symptoms similar to or lower than those of the control group.
METHODS
Participants
The 225 participants were randomized into 2 groups. One hundred twenty-six participants (56%) were assigned to the control group—and entered programs that followed the Continuum of Care model—and 99 (44%) were assigned to the experimental group and to a program that used the Housing First model. The control group was intentionally oversampled, anticipating that a higher number of control group participants may remain homeless and prove more difficult to locate for follow up interviews. The sample comprised 2 subgroups: an original street sample of 157 participants who met eligibility criteria, and a second group of 68 individuals recruited from 2 state psychiatric hospitals. To meet eligibility criteria, the first group had to have spent 15 of the past 30 days on the street or in other public places (shelters were not included), exhibited a history of homelessness over the past 6 months, and had an Axis I diagnosis25 of severe mental illness. Diagnoses were based on previous records from service providers or, in cases in which records were unavailable, on an interview with an independent psychiatrist. Although a diagnosis or history of alcohol or substance abuse disorders was not an eligibility criterion, according to clinical records 90% of all the participants also had a diagnosis or history of alcohol or substance abuse disorders. The street sample was recruited through service agency staff referral of eligible clients who were interested in study participation. The second group met the same entry criteria for homelessness and mental illness immediately before hospitalization as did the street sample.
Because of administrative problems, 12 participants in the experimental condition were not assigned a Pathways apartment, and 7 control participants were erroneously assigned a Pathways apartment. Excluding these 19 participants reduced the number of control participants to 119 (58%) and the number of experimental participants to 87 (42%).
As can be seen in Table 1 ▶, the final sample consisted of 162 (79%) men and 44 (21%) women whose average age was 41.3 years. More than half of the participants (n = 110, 53%) were diagnosed with a psychotic disorder. Seventeen percent (n = 35) had become homeless before the age of 18 years. The longest period ever homeless, on average, was 4.5 years. Fifty-one percent (n = 114) of the participants were literally homeless (staying in the streets or public spaces) at the time of the baseline interview. Another 36% entered the study from psychiatric institutions but had been homeless before hospitalization. After randomization, there were no significant differences between groups for baseline demographic characteristics such as gender, age, education, race, diagnosis, or amount of time homeless.
TABLE 1—
Participant Characteristics at Baseline (n = 206)
| No. (%) | |
| Study group | |
| Experimental | 87 (42) |
| Control | 119 (58) |
| Gender | |
| Female | 44 (21) |
| Male | 162 (79) |
| Age, y | |
| 18–30 | 39 (19) |
| 31–40 | 59 (29) |
| 41–50 | 62 (30) |
| 51–60 | 36 (17) |
| ≥ 61 | 10 (5) |
| Education | |
| 8th grade or less | 21 (10) |
| Some high school | 66 (32) |
| Finished high school | 34 (17) |
| Completed general equivalency diploma | 16 (8) |
| Vocational/trade/business school | 5 (2) |
| Some college | 49 (24) |
| College degree | 10 (5) |
| Graduate degree | 4 (2) |
| Race/ethnicity | |
| White (not Hispanic) | 55 (27) |
| Black (not Hispanic) | 84 (41) |
| Hispanic | 30 (15) |
| Mixed/other/unknown | 37 (18) |
| Diagnosis | |
| Psychotic | 110 (53) |
| Mood—depressive | 29 (14) |
| Mood—bipolar | 29 (14) |
| Other | 10 (5) |
| Unknown | 28 (14) |
| Residence at baseline | |
| Streets/subways/parks/abandoned building/drop-in centers | 114 (51) |
| Shelter/safe haven | 13 (6) |
| Psychiatric hospital | 80 (36) |
| Other | 18 (8) |
Procedures
After completing their baseline interviews, participants were interviewed every 6 months. Interviewers were blind to participants’ assignment for baseline interviews but not for follow-up interviews. Data for the complete 24-month period were collected between December 1997 and January 2001. During each interim period, 5-minute telephone calls were conducted primarily to maintain contact with participants and establish their whereabouts. Participants were paid for all interviews. Six-month interviews were conducted in a variety of locations, including the research office, the participant’s apartment/residential location, or a public place such as a cafe or restaurant. When it was not possible for interviews to be conducted face-to-face (e.g., the participant had moved out of state), interviews were conducted by telephone. For participants in psychiatric hospitals and correctional facilities, research interviewers made onsite visits. The questions asked during each interview period remained the same. The follow-up rates by time period were as follows: 88% at 6 months, 87% at 12 months, 84% at 18 months, and 78% at 24 months. These follow-up rates do not include individuals who were missing at certain time points but who were located subsequently and for whom residential data was collected at a later point. Thus, the follow-up rates reported here are based on conservative calculations.
Measures
A modified version of Consumer Choice, a 16-item, 5-point scale developed by Srebnik, Livingston, Gordon, and King,26 was used to determine (1) how important it was for the participant to have choice at baseline and (2) how much choice the participant actually had, at subsequent time points, in their location, neighbors and housemates, visitors, and so forth.
We measured residential status with a 6-month residential follow-back calendar developed by New Hampshire Dartmouth Research Center.27 The interviewer assessed the participant’s location for each day during the past 6 months on a day-by-day basis. From this information, we calculated the proportion of time spent homeless as well as the proportion of time spent in stable housing.
Following the interview, the interviewer coded the participant’s residential location according to several distinct residential categories. For the purpose of analyses, homelessness was considered as living on the streets, in public places, or in shelter-type accommodations. Residential stability was defined as residing in one’s own apartment; or having a room or studio apartment in a supportive housing program, a group home, a boarding home, or a long-term transitional housing program; or living long-term with parents, friends, or other family members. The number of days spent in any of the locations categorized as “homeless” or “stably housed” was summed and divided by the total number of days of residency reported at the interview.
We measured alcohol and drug use with the Drug and Alcohol Follow-Back Calendar.28,29 Participants reported the number of drinks consumed each day, as well as the number of days that selected drugs were used during a 6-month period. We used an alcohol use variable (measuring the total number of drinks) and a drug use variable (measuring the total number of days of drug use) for each 6-month period in the analyses.
We measured substance abuse treatment service utilization with a modified shorter version of the Treatment Services Inventory.30 In the interview, participants were asked whether they received any substance abuse treatment during the past 2 weeks. Drug and alcohol treatment services use was indicated by an average of 7 items including questions asking whether the participant had received treatment in a detoxification program or other program; consulted with a counselor to talk about substance problems; or attended Alcoholics Anonymous, Narcotics Anonymous, or any other self-help group.
Psychiatric symptoms were measured with the Colorado Symptom Index,31 a 15-item questionnaire including items assessing psychotic symptoms as well as symptoms related to mood and suicidality.
Data Analysis
Repeated-measures analysis of variance (ANOVA) was used to examine group differences, during the 2-year follow-up period, for hypothesis 1 (consumer choice), hypothesis 2 (housing stability assessed as 2 separate outcomes: proportion of time stably housed and proportion of time homeless), and hypothesis 3 (substance abuse assessed as 2 separate outcomes: alcohol abuse and drug abuse). In cases in which repeated-measures ANOVAs yielded significant results, t tests were conducted to compare group differences at each time point. Group differences were then plotted and graphed for the 2 groups across time.
To appropriately examine differences in substance abuse treatment services use, hypothesis 4 was tested with a subsample of participants who were not on the streets but who were in some type of service-related program: namely, experimental participants who were currently housed by the Housing First program and control participants who were housed by one of the Continuum of Care programs. Control participants were included in this analysis if they reported that they lived most recently in one of the following places at the time of the interview: shelters, supportive housing programs, drop-in centers, safe havens, detoxification facilities, crisis housing, intermediate care, boarding houses, transitional housing, group homes, alcohol/drug-free facilities, and treatment/recovery programs. Because participants’ residential status changed from one time point to the next, the subsample also changed; we therefore had to conduct separate t tests for each time point. Because there were 5 time points, we used a Bonferroni adjusted α of .025 to account for Type I error.
Power Analysis
To retain 80% power to detect an effect that explains 4% of the variance in the context of an equation (with 5 covariates) that explains 25% of the variance, we needed to retain 68% of the original sample; moreover, power for repeated-measures analyses would be higher.32 Our retention rates were substantially above this figure, so we did not anticipate any problems in the power to detect group differences.
RESULTS
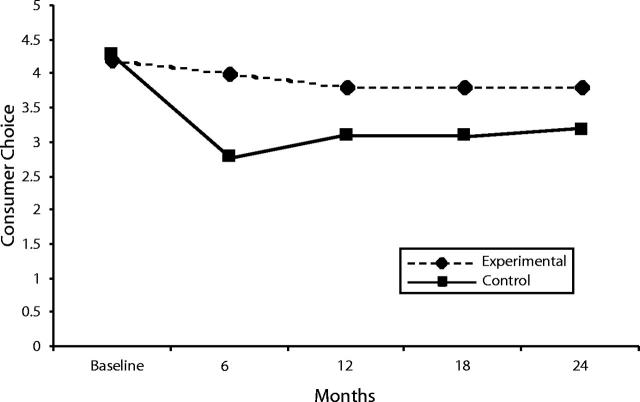
Consumer Choice
Results from repeated-measures ANOVA showed that there was a significant time × group status effect, indicating that participants in the experimental condition perceived their choices to be more numerous than did participants in the control condition (F4,112 = 8.91, P < .001). Additionally, the experimental group’s perceptions were more stable than were those of the control group. As can be seen from Figure 1 ▶, subsequent univariate analyses showed significant differences at 6, 12, 18, and 24 months, with the experimental group reporting significantly more choice than the control group.
FIGURE 1—
Consumer choice in housing: baseline–24 months.
Note. At baseline, participants were asked how much choice they would like to have. Subsequent time-points assess how much choice participants actually have.
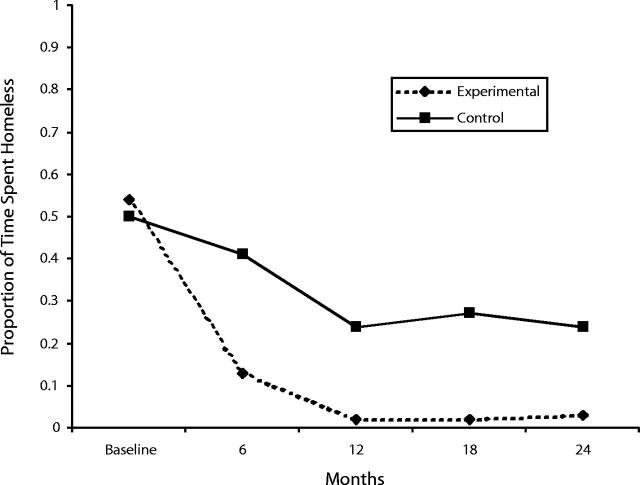
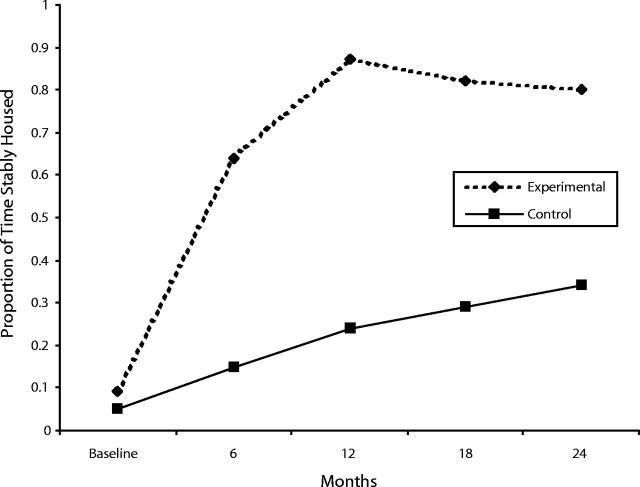
Residential Stability
Repeated-measures ANOVA results showed a significant Time × Group status effect. Participants in the experimental condition had significantly faster decreases in homeless status and increases in stably-housed status relative to participants in the control condition (F4,137 = 10.1, P < .001; F4,137 = 27.7, P < .001). As can be seen from Figures 2 ▶ and 3 ▶, subsequent univariate analyses showed significant differences at 6, 12, 18, and 24 months, with the experimental group reporting less time spent homeless and more time spent stably housed compared with the control group.
FIGURE 2—
Proportion of time spent homeless: baseline–24 months.
FIGURE 3—
Proportion of time stably housed: baseline–24 months.
Substance Use
Repeated-measures analyses showed no significant differences in either alcohol or drug use between the 2 groups by time condition (F4,136 = 1.1, P = .35 for alcohol use; F4,136 = .98, P = .42 for drug use).
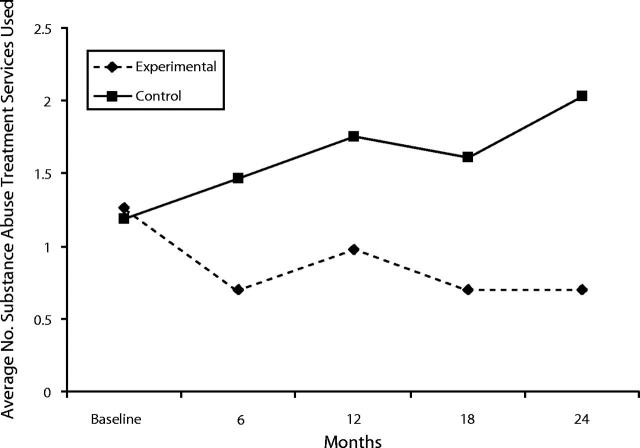
Substance Abuse Treatment Utilization
Five t tests were conducted with an adjusted α level of .025. As can be seen from Figure 4 ▶, these univariate analyses showed significant differences at 6, 18, and 24 months (P < .025) and at 12 months (P < .05), with the Continuum group reporting significantly higher use of substance abuse treatment programs than the Housing First group. In addition, a decrease in service use occurred among the Housing First group and an increase occurred among the Continuum group over time.
FIGURE 4—
Average number of substance abuse treatment services used: baseline–24 months.
Psychiatric Symptoms
Repeated-measures analyses showed no significant differences psychiatric symptoms between the 2 groups by time condition (F4,137 = .348, P = .85).
DISCUSSION
Our results attest to the effectiveness of using the Housing First approach in engaging, housing, and keeping housed individuals who are chronically homeless and dually diagnosed. The Housing First program sustained an approximately 80% housing retention rate, a rate that presents a profound challenge to clinical assumptions held by many Continuum of Care supportive housing providers who regard the chronically homeless as “not housing ready.” More important, the residential stability achieved by the experimental group challenges long-held (but previously untested) clinical assumptions regarding the correlation between mental illness and the ability to maintain an apartment of one’s own. Given that all study participants had been diagnosed with a serious mental illness, the residential stability demonstrated by residents in the Housing First program—which has one of the highest independent housing rates for any formerly homeless population—indicates that a person’s psychiatric diagnosis is not related to his or her ability to obtain or to maintain independent housing. Thus, there is no empirical support for the practice of requiring individuals to participate in psychiatric treatment or attain sobriety before being housed.
Participants’ ratings of perceived choice—one of the fidelity dimensions of the Housing First program—show that tenants at Pathways experience significantly higher levels of control and autonomy in the program. This experience may contribute to their success in maintaining housing and to most consumers’ choice to participate in treatment offered by the ACT team after they were housed. In addition, contrary to the fears of many providers and policymakers, housing consumers without requiring sobriety as a precondition did not increase the use of alcohol or drugs among the experimental group compared with the control group. Providing housing first may motivate consumers to address their addictions to keep their housing, so that providing housing before treatment, may better initiate and sustain the recovery process.
Our findings indicate that ACT programs that combine a consumer-driven philosophy with integrated dual diagnosis treatment based on a harm-reduction approach positively affect residential stability and do not increase substance use or psychiatric symptoms. In addition, because the ACT teams were providing services directly, substance abuse treatment services use was significantly lower for Housing First residents than for Continuum of Care residents. Because treatment for substance abuse is required, along with sobriety, by the Continuum of Care model, it is not surprising that individuals in the control group show greater use of treatment services. However, despite the control group’s higher use of services, their levels of alcohol or drug use were not different from those of the experimental group. This disconnect between drug treatment services use and levels of drug use suggests that the control group may be using treatment facilities as short-term housing.
One limitation of the study is that self-reports of the use of alcohol and drugs and treatment services can be susceptible to reporting bias. Several studies have shown that among people who are homeless and dually diagnosed, there is a high rate of discrepancy between self-reports and client observation for substance use and for utilization of substance abuse treatment services.33,34 Memory error, nondisclosure, social desirability concerns, and intentional misrepresentation can lead to reporting errors. Powerful systemic reasons for underreporting also exist. For example, participants enrolled in Continuum of Care residential programs, for which sobriety is mandatory, may be inclined to underreport the amount of drugs and alcohol consumed out of fear that such information may reach a caseworker or staff member and lead to the loss of their housing. Errors in self-reporting could be reduced if other measures (e.g., case manager’s reports, laboratory drug tests) could be incorporated into a multiple-measure data report.
In conclusion, the outcomes achieved provide grounds for the rejection of the erroneous assumptions underlying the ubiquitous Continuum of Care model, the elimination of treatment requirements as a precondition for housing, and the support of initiatives adopting a Housing First approach to end homelessness and increase integration into the community for individuals with psychiatric disabilities living on our streets.
Acknowledgments
This study was funded in part by Substance Abuse and Mental Health Services Administration (SAMHSA) grant 4UD9SM51970–03–2, SAMHSA/Center for Substance Abuse Treatment grant 1KD1TI12548–01, and the New York State Office of Mental Health grant C005345.
We thank Marybeth Shinn, Ana Stefancic, Ronni Michelle Greenwood, and Nicole Schafer as well as the study participants for their assistance.
Human Participant Protection The protocol was approved by the institutional review boards of Pathways to Housing, Inc. and New York University. Informed consent was obtained from all participants.
Contributors S. Tsemberis oversaw all aspects of the study and preparation of the article. L. Gulchur completed data collection and the statistical analysis. M. Nakae assisted with data analysis and literature review.
Peer Reviewed
References
- 1.Bloomberg plans more housing aid for the homeless. New York Times. 18June2002:A1
- 2.Hopper K, Jost J, Hay T, et al. Homelessness, mental illness and the institutional circuit. Psychiatr Serv. 1997;48:659–665. [DOI] [PubMed] [Google Scholar]
- 3.Sullivan G, Burnam A, Koegel P. Pathways to homelessness among the mentally ill. Social Psychiatry. 2000;35:444–450. [DOI] [PubMed] [Google Scholar]
- 4.Drake RE, McHugo GJ, Clark RE, et al. Assertive community treatment for patients with co-occurring severe mental illness and substance use disorder: a clinical trial. Am J Orthopsychiatry. 1998;68:201–215. [DOI] [PubMed] [Google Scholar]
- 5.Johnson TP, Freels SA, Parsons JA, et al. Substance abuse and homelessness: social selection or social adaptation? Addiction. 1997;92:437–445. [PubMed] [Google Scholar]
- 6.McCarty D, Argeriou M, Huebner RB, et al. Alcoholism, drug abuse, and homelessness. Am Psychol. 1991;46:1139–1148. [DOI] [PubMed] [Google Scholar]
- 7.Anthony WA, Blanch A. Supported employment for persons who are psychiatrically disabled: an historical and conceptual perspective. Psychosoc Rehabil J. 1989;12:55–81. [Google Scholar]
- 8.Carling PJ. Housing and supports for persons with mental illness: emerging approaches to research and practice. Hosp. Community Psychiatry. 1993;44:439–449. [DOI] [PubMed] [Google Scholar]
- 9.Ridgeway P, Zipple AM. Challenges and strategies for implementing supported housing. Psychosoc Rehabil J. 1990;13:115–120 [Google Scholar]
- 10.Kuhn R, Culhane DP. Applying cluster analysis to test a typology of homelessness by pattern of shelter utilization: results form the analysis of administrative data. Am J Community Psychol. 1998;26:207–232. [DOI] [PubMed] [Google Scholar]
- 11.Hurlburt HS, Hough RL, Wood PA. Effects of substance abuse on housing stability and homeless mentally ill persons in supported housing. Psychiatr Serv. 1996;47:731–736. [DOI] [PubMed] [Google Scholar]
- 12.Minkoff K. Developing Standards of care for individuals with co-occurring psychological and substance use disorders. Psychiatr Serv. 2001;52:597–599. [DOI] [PubMed] [Google Scholar]
- 13.Howie the Harp. Independent living with support services: the Goals and future for mental health consumers. Psychosoc Rehabil J. 1990;13:85–89. [Google Scholar]
- 14.Asmussen SM, Romano J, Beatty P, et al. Old answers for today’s problems: helping integrate individuals who are homeless with mental illnesses into existing community-based programs. Psychosoc Rehabil J. 1994;17:17–34. [Google Scholar]
- 15.Osher FC, Drake RE. Reversing a history of unmet needs: approaches to care for persons with co-occurring addictive and mental disorders. Am J Orthopsychiatry. 1996;66:4–11. [DOI] [PubMed] [Google Scholar]
- 16.Lovell AM, Cohn S. The elaboration of “choice” in a program for homeless persons labeled psychiatrically disabled. Hum Organ. 1998;57:8–20. [Google Scholar]
- 17.Tsemberis SJ, Moran L, Shinn M, Asmussen SM, Shern DL. Consumer preference programs for individuals who are homeless and have psychiatric disabilities: a drop-in center and a supported housing program. Am J Community Psychol. 2003;32:305–317. [DOI] [PubMed] [Google Scholar]
- 18.Shern DL, Tsemberis S, Anthony W, et al. Serving street-dwelling individuals with psychiatric disabilities: outcomes of a psychiatric rehabilitation clinical trial. Am J Public Health. 2000;90:1873–1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Teague GB, Bond GR, Drake RE: Program fidelity in assertive community treatment: development and the use of a measure. Am J Orthopsychiatry. 1998;68:216–232. [DOI] [PubMed] [Google Scholar]
- 20.Stein LI, Santos AB. Assertive Community Treatment of Persons with Severe Mental Illness. New York, NY: WW Norton; 1998.
- 21.Tsemberis S, Asmussen S. From streets to homes: Pathways to Housing consumer preference supported housing model. Alcohol Treatment Q. 1999;17:113–131. [Google Scholar]
- 22.Inciardi JA, Harrison LD. Introduction: the concept of harm reduction. In: Inciardi JA, Harrison LD, eds. Harm Reduction: National and International Perspectives. Thousand Oaks, CA: Sage Publications, 2000:2–19.
- 23.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: applications to addictive behaviors. Am Psychol. 1992;47:1102–1114. [DOI] [PubMed] [Google Scholar]
- 24.Lipton FR, Siegel C, Hannigan A, Samuels J, Baker S. Tenure in supportive housing for homeless persons with severe mental illness. Psychiatr Serv. 2000;51:479–486. [DOI] [PubMed] [Google Scholar]
- 25.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington DC: American Psychiatric Association; 1994.
- 26.Srebnik D, Livingston J, Gordon L, et al. Housing choice and community success for individuals with serious and persistent mental illness. Community Ment Health J. 1995;31:139–152. [DOI] [PubMed] [Google Scholar]
- 27.New Hampshire Dartmouth Psychiatric Research Center. Residential Follow-Back Calendar. Lebanon, NH: Dartmouth Medical School; 1995.
- 28.New Hampshire Dartmouth Psychiatric Research Center. Drug and Alcohol Follow-Back Calendar. Lebanon, NH: Dartmouth Medical School; 1995.
- 29.Sobell LC, Sobell MB, Leo GI, et al. Reliability of a timeline method: assessing normal drinker’s reports of recent drinking and a comparative evaluation across several populations. Br J Addict. 1988;83:393–402. [DOI] [PubMed] [Google Scholar]
- 30.McLellan AT, Alterman AI, Woody GE, et al. Treatment Services Review. Philadelphia, PA: University of Pennsylvania; 1992.
- 31.Ciarolo JA, Edwards DW, Kiresuk TJ, Newman FL, Brown TR. Colorado Symptom Index. Washington, DC: National Institute of Mental Health; 1981.
- 32.Cohen J, Cohen P. Applied Regression/Correlation Analysis for Behavioral Sciences. New York, NY: John Wiley & Sons; 1983
- 33.Calsyn RJ, Morse GA, Klinkenberg WD, et al. Reliability and validity of self-report data of homeless mentally ill individuals. Eval Program Plann. 1997;20:47–54. [Google Scholar]
- 34.Goldfinger SM, Schutt RK, Seidman LJ, et al. Self-report and observer measure of substance abuse among homeless mentally ill persons in the cross-section and over time. J Nerv Ment Dis. 1996;184:667–672. [DOI] [PubMed] [Google Scholar]