Abstract
Objectives. We assessed the prevalences of periodontitis by education and income levels among US adults with data from the third National Health and Nutrition Examination Survey.
Methods. The study was limited to non-Hispanic Blacks, Mexican Americans, and non-Hispanic Whites 50 years of age or older with a complete periodontal assessment during the dental examination.
Results. Blacks with higher education and income levels had a significantly higher prevalence of periodontitis than their White and Mexican-American counterparts. The relationship between income level and periodontitis was modified by race/ethnicity. High-income Blacks exhibited a higher prevalence of periodontitis than did low-income Blacks and high-income Whites.
Conclusions. Our findings call attention to the importance of recognizing socioeconomic status–related health differences across racial/ethnic groups within the social, political, and historical context.
The pervasiveness of health disparities by socioeconomic status (SES) in the United States has been documented for years.1–6 Regardless of race or ethnicity, health outcomes for individuals of lower SES continue to be poorer than those of their higher-SES counterparts.3,7 This is also true for periodontal health: for years, the data have shown significant SES differences across racial/ethnic groups.8–18 Many previous studies documenting differences in periodontal health have included SES indicators (i.e., income and education) in their analyses. Some studies have provided cross-tabulations between periodontitis and categories for each SES indicator,19–25 whereas others have included these indicators as covariates in multivariable analysis approaches.22,23,25–29 The first group of studies has reported higher prevalences and severity of periodontitis for those with lower SES compared with their higher-SES counterparts. The second group has documented the persistence of racial/ethnic differences after adjusting for SES indicators. However, the incommensurability of these indicators across racial/ethnic groups has not been discussed in these studies. To date, SES indicators have not been investigated as the main independent covariates in studies of periodontal health. Therefore, their contribution to the existing racial/ethnic differences or to the disparity in the prevalence of periodontitis in general remains unknown.
To address these issues and expand our previous work on racial/ethnic differences in periodontitis, we ascertained prevalences of periodontitis for (1) income and (2) education among non-Hispanic Black, Mexican-American, and non-Hispanic White adults aged 50 years or older using data from the third National Health and Nutrition Examination Survey (NHANES III). In addition, we investigated the combined effect of income and education on the prevalence of periodontitis. Finally, in this article we discuss the pathways by which SES indicators intertwined with race/ethnicity to affect periodontal health.
METHODS
We used data from a subsample of NHANES III, conducted from 1988 to 1994. This survey used a complex sampling design to select the civilian, noninstitutionalized US population aged 2 months or older.30 A complete description of the plan and operation of NHANES III has been given elsewhere.31 Of the total adult sample (n = 20 050), 8654 persons were aged 50 years or older; of these, 5124 (59.2 %) were dentate. Furthermore, 4375 received a periodontal assessment with 80.7% receiving a complete assessment. There were 646 (12.6%) persons excluded from the periodontal assessment for medical reasons. These exclusions were proportional across racial/ethnic groups. Data for this analysis were restricted to 3407 persons aged 50 years or older who reported their racial/ethnic identity as non-Hispanic Black (n = 718), non-Hispanic White (n = 1815), or Mexican American (n = 874) and who received a complete periodontal assessment during the NHANES III dental examination. Hereafter, we refer to non-Hispanic Blacks as Blacks and non-Hispanic Whites as Whites.
Study Variables
During the dental examination, 6 dentists trained in the survey examination protocol conducted the periodontal examinations.31 Briefly, the periodontal examination was conducted in 2 randomly chosen quadrants, 1 maxillary and 1 mandibular, on the assumption that conditions in these 2 quadrants would represent the mouth. Two sites, midbuccal and mesiobuccal, were examined for each tooth. Examiners used a periodontal probe to measure clinical attachment loss (CAL) and pocket depth (PD). CAL was defined as the distance in millimeters from the cementoenamel junction to the base of the pocket/sulcus, and PD as the distance from the free gingival marginal to the base of the pocket/sulcus. Third molars were excluded because of their frequent extraction in young adulthood, so a maximum of 14 teeth and 28 sites per individual were examined. When defining periodontitis, there is very little agreement on the case definitions across studies. However, previous studies have used several combinations of CAL and PD to establish periodontitis case definitions.25,27,32–34 Moreover, these studies have been tailored to test specific hypotheses. For this study, to arrive at the definition used in the analyses, we tested several definitions used in previous studies as well as the distribution of CAL and PD in the total population and in each racial/ethnic group of this study. The final definition was established before any hypothesis testing. Periodontitis was defined as a composite of at least 4 sites with CAL ≥ 5 mm and at least one site with PD ≥ 4 mm. However, these conditions did not have to be present in the same site.
The main covariates for this analysis were education, income, and race/ethnicity. Education was collected as a continuous variable (number of years of education) from zero to 17 years and was categorized as follows: < 12 years and ≥ 12 years of education. The yearly income of a family was collected as a continuous variable and was categorized as follows: < $20 000 and ≥ $20 000. Race/ethnicity was self-reported by the study’s participants and selected from 4 categories: non-Hispanic Black, non-Hispanic White, Mexican American, and Other.
Covariates recognized as risk indicators for periodontitis were selected for the analysis.17–22,35–40 The covariates were age at interview, gender, marital status, time since last dental visit, presence of health insurance, self-reported diabetes, and tobacco use. In addition, dental calculus and missing teeth were investigated as covariates.41–43 Gender (male/female), currently employed (yes/no), and presence of health insurance (yes/no) were used in this analysis as collected in NHANES III. Age at interview was used as a continuous and categorical variable. Age categories used were 50 to 59, 60 to 69, and 70 years or older. Categories for the marital status variable were married (married or living together with someone as married), single, divorced (separated or divorced), and widowed. Time since last dental visit was collected as a continuous variable (days since last seeing a dentist) and categorized as follows: ≤ 6 months, > 6 months to < 1 year, and ≥ 1 year.
The question “Have you ever been told by a doctor that you have diabetes?” was used to assess the history of diabetes. Women who manifested diabetes only during pregnancy were not considered to have diabetes. Smoking status was derived from 2 questions: “Do you smoke cigarettes now?” and “Have you smoked at least 100 cigarettes in your life?” Smoking status was defined as current smokers (subjects who answered “yes” to both questions), former smokers (subjects who answered “no” to the first question and “yes” to the second question), and never smokers (subjects who answered “no” to both questions).
During the periodontal examination, dental calculus was assessed in 2 sites, midbuccal and mesiobuccal, for the 2 randomly selected quadrants. Calculus was recorded as the absence of calculus, presence of supragingival calculus only, or presence of either subgingival calculus only or both types of calculus (supragingival and subgingival). For this analysis, calculus was specified as the presence or absence of calculus on at least 1 site per tooth. A variable to account for missing teeth was created by subtracting the number of teeth present in the mouth from the 28 teeth considered during the dental examination.
Statistical Analysis
Characteristics of the population and prevalence of periodontitis were described for each covariate stratified by race/ethnicity. To assess differences in the prevalence of periodontitis, we performed 3 sets of χ2 tests: first, we used the Cochran–Mantel–Haenszel test to evaluate the independence between periodontitis and race/ethnicity, after controlling for each covariate separately. Second, we applied the homogeneity test for equal prevalence of periodontitis for each racial/ethnic group over covariate categories. Finally, we applied the independence test to examine for equal prevalence of periodontitis across racial/ethnic group within each covariate category.
Unadjusted and adjusted prevalences of periodontitis and 95% confidence limits for (1) income and (2) education categories were estimated from logistic regression models for each racial/ethnic group before and after adjusting for demographic and health-related covariates. We used a step-down method to select the covariates that significantly contributed to each model.44 This method, similar to the backward-selection method, takes into account not only the changes of the β coefficients of the other covariates when including and excluding each nonsignificant covariate from the model but also the possible correlations among covariates. The final model for income includes education during adjustment and vice versa. To investigate the combined effect of income and education, we also estimated the unadjusted and adjusted prevalence of periodontitis and the 95% confidence interval from logistic regression models. Prevalence of periodontitis for 4 cross-classified categories of income and education (i.e., high income and high education, high income and low education, low income and high education, and low income and low education) were calculated for each racial/ethnic group before and after adjusting for all other covariates in the model. Ratios of adjusted prevalence of periodontitis and their 95% confidence interval between racial/ethnic groups were calculated for each category of income and education as well as for the joint effects of income and education. In a logistic regression model including race/ethnicity as an independent covariate, 2-way interaction terms between race/ethnicity and (1) education and (2) income were tested. A significant interaction between race/ethnicity and income was found and reported.
We carried out all data management procedures with SAS45 and carried out the statistical analyses using SUDAAN.46 SUDAAN takes into account the weights provided in the data set yielding unbiased standard error estimates. In the tables, the sample sizes were unweighted. However, estimates for means, proportions, standard errors, and 95% confidence intervals were weighted.
RESULTS
Characteristics of the Population
Table 1 ▶ shows the characteristics of the study population for selected covariates by race/ethnicity. When compared with Whites, Blacks and Mexican Americans were younger, were less educated, had lower income, were less likely to have had a dental visit within the past 6 months, and were more likely to report having diabetes (all P values < .05). In addition, Blacks exhibited the highest proportion of current smokers and were less likely to be married, whereas Mexican Americans were more likely to be males and uninsured.
TABLE 1—
Characteristics of Non-Hispanic Black, Non-Hispanic White, and Mexican American Adults Aged 50 Years and Older: Third National Health and Nutrition Examination Survey, 1988–1994a
| % (SE) | ||||
| Blacks (n = 718) | Mexican Americans (n = 874) | Whites (n=1815) | Totalb (n = 3533) | |
| Age, y, mean (SE) | 61.6 (0.50) | 59.7 (0.33) | 62.6 (0.41) | 62.2 (0.36) |
| Age groups, y | ||||
| 50–59 | 48.3 (0.94) | 54.8 (0.45) | 42.9 (1.97) | 45.2 (1.71) |
| 60–69 | 32.0 (2.29) | 34.5 (2.08) | 33.9 (1.41) | 33.4 (1.11) |
| ≥ 70 | 19.7 (1.85) | 10.7 (1.47) | 23.2 (1.53) | 21.4 (1.33) |
| Gender | ||||
| Male | 45.9 (1.50) | 50.5 (1.91) | 48.6 (1.13) | 48.7 (0.94) |
| Female | 54.1 (1.50) | 49.5 (1.91) | 51.4 (1.13) | 51.2 (0.94) |
| Marital status | ||||
| Married | 52.2 (1.79) | 74.3 (1.77) | 74.2 (1.54) | 72.5 (1.35) |
| Single | 6.0 (0.86) | 2.2 (0.53) | 3.2 (0.41) | 3.6 (0.40) |
| Divorced | 21.3 (1.77) | 11.9 (1.64) | 9.7 (1.03) | 10.7 (0.94) |
| Widowed | 20.5 (1.51) | 11.7 (1.64) | 12.9 (0.88) | 13.2 (0.75) |
| Education, y | ||||
| < 12 | 52.1 (2.53) | 70.8 (2.89) | 19.9 (1.58) | 25.7 (1.55) |
| ≥ 12 | 47.9 (2.53) | 29.2 (2.89) | 80.1 (1.58) | 74.3 (1.55) |
| Income | ||||
| < $20 000 | 53.9 (2.93) | 57.9 (2.62) | 23.8 (1.67) | 28.0 (1.66) |
| ≥ $20 000 | 46.1 (2.93) | 42.2 (2.62) | 76.2 (1.67) | 72.0 (1.66) |
| Presence of health insurance | ||||
| Yes | 92.4 (1.33) | 87.8 (2.34) | 97.9 (0.38) | 97.0 (0.40) |
| No | 7.6 (1.33) | 12.2 (2.34) | 2.1 (0.38) | 3.0 (0.40) |
| Time since last dental visit | ||||
| ≤ 6 mo | 31.6 (2.30) | 35.7 (2.56) | 64.9 (1.65) | 59.8 (1.67) |
| > 6 mo and < 1 y | 20.7 (1.92) | 20.8 (1.97) | 16.9 (1.03) | 17.4 (0.90) |
| ≥ 1 y | 47.7 (2.15) | 43.5 (2.18) | 18.2 (1.16) | 22.8 (1.23) |
| Diabetes | ||||
| Yes | 14.4 (1.31) | 18.2 (1.58) | 7.6 (0.68) | 8.4 (0.51) |
| No | 85.6 (1.31) | 81.8 (1.58) | 92.4 (0.68) | 91.6 (0.51) |
| Smoking status | ||||
| Current smokers | 26.7 (2.08) | 17.8 (1.76) | 14.5 (1.08) | 15.8 (0.94) |
| Former smokers | 26.9 (1.81) | 35.7 (1.98) | 39.8 (1.56) | 37.6 (1.29) |
| Never smokers | 46.3 (2.40) | 46.5 (1.86) | 45.6 (1.65) | 46.6 (1.37) |
aSample sizes are unweighted; means, proportions, and standard errors are weighted to take into account Third National Health and Nutrition Examination Survey sample design.
bTotal includes Others.
Prevalence of Periodontitis
Blacks had worse periodontal clinical conditions than Mexican Americans and Whites (data not shown). In addition, Blacks were more likely to have calculus, higher mean CAL and PD, and a lower mean number of teeth.
Table 2 ▶ shows the prevalence of periodontitis for each racial/ethnic group for selected covariates. The overall prevalence of periodontitis in this population was 6.3%. Blacks exhibited the highest prevalence (14.2%), followed by Mexican Americans (9.4%) and Whites (5.3%). However, the differences between racial/ethnic groups were not statistically significant. In general, the prevalence of periodontitis was highest among males, those without insurance, those without a dental visit within the last 6 months, those with a selfreported history of diabetes, and those who smoked. Blacks exhibited the highest prevalence in all categories except for the presence of health insurance, in which category Whites had the highest prevalence. The prevalence of periodontitis was lowest for the youngest ages in each of the 3 racial/ethnic groups; however, only Whites showed a monotonic increase in prevalence of periodontitis over the 3 age groups. For marital status, the pattern for the prevalence of periodontitis was somewhat different for each racial/ethnic group, with married people exhibiting the lower prevalence regardless of their race/ethnicity.
TABLE 2—
Prevalence of Periodontitis for Selected Covariates Among Non-Hispanic Black, Non-Hispanic White, and Mexican American Adults Aged 50 Years and Older: Third National Health and Nutrition Examination Survey, 1988–1994
| % (SE) | ||||
| Blacks (n = 718) | Mexican Americans (n = 874) | Whites (n = 1815) | Total (n = 3533) | |
| Overall prevalence | 14.2 (1.45) | 9.4 (1.48) | 5.3 (0.62) | 6.3 (0.59) |
| Age groups, y | ||||
| 50–59 | 10.5 (1.99) | 5.7 (1.65) | 4.4 (0.92) | 5.6 (0.83) |
| 60–69 | 18.7 (2.77) | 15.0 (2.17) | 4.9 (0.97) | 6.1 (0.86) |
| ≥ 70 | 15.6 (2.34)a | 9.3 (2.57) | 7.1 (1.25)a | 7.8 (1.22) |
| Gender | ||||
| Male | 19.4 (2.42) | 15.0 (2.60) | 8.0 (1.05) | 9.3 (1.08) |
| Female | 9.9 (1.78) | 3.7 (1.20) | 2.8 (0.59) | 3.5 (0.54) |
| Marital Status | ||||
| Married | 13.0 (2.38) | 9.7 (1.69) | 5.1 (0.74) | 5.9 (0.68) |
| Single | 19.7 (7.45) | 10.0 (6.06) | 6.8 (3.33)b | 7.7 (2.83) |
| Divorced | 14.0 (3.37) | 10.0 (4.73) | 7.2 (1.93)b | 8.4 (1.64) |
| Widowed | 16.2 (3.10)a | 7.0 (2.29)a | 4.7 (1.36)a | 6.5 (1.27) |
| Presence of health insurance | ||||
| Yes | 11.9 (1.89) | 5.1 (1.32) | 4.6 (0.57) | 5.0 (0.57) |
| No | 13.9 (5.24)a | 9.3 (4.60)a | 17.8 (6.95)b | 14.2 (4.41) |
| Time since last dental visit | ||||
| ≤ 6 mo | 8.2 (2.08) | 5.4 (1.57) | 3.0 (0.50) | 3.7 (0.58) |
| > 6 mo | 13.1 (2.40) | 8.3 (1.99) | 6.6 (1.66)b | 7.1 (1.23) |
| ≥ 1 y | 18.4 (2.24) | 12.3 (2.99)a | 11.9 (2.01)b | 12.1 (1.48) |
| Diabetes | ||||
| Yes | 15.3 (3.75) | 12.0 (2.88) | 8.6 (2.57)b | 9.6 (2.02) |
| No | 14.1 (1.47)a | 8.8 (1.48)a | 5.0 (0.63)a | 6.0 (0.61) |
| Smoking status | ||||
| Current smokers | 21.1 (3.02) | 17.1 (3.31) | 14.1 (2.58)b | 16.4 (2.37) |
| Former smokers | 13.8 (2.73) | 9.8 (3.17) | 6.1 (1.07) | 6.5 (0.95) |
| Never smokers | 10.6 (2.08)a | 6.2 (1.16) | 1.8 (0.41) | 2.7 (0.45) |
aChi-squared test of homogeneity (to examine for equal prevalence of periodontitis for each racial/ethnic group over covariate categories) nonsignificant at P ≥ .05.
bChi-squared test of independence (to examine for equal prevalence of periodontitis across racial/ethnic group within each covariate category) nonsignificant at P ≥ .05. Chi-squared tests for Cochran–Mantel–Haenszel test (to evaluate the independence between periodontitis and race/ethnicity, after controlling for each covariate separately) were all significant at P < .0001.
Prevalences and prevalence ratios of periodontitis for education and income categories for each racial/ethnic group are presented in Table 3 ▶. Blacks exhibited the highest prevalence for both categories of education. This pattern remained after adjustment for age, gender, presence of insurance, time since last dental visit, history of diabetes, smoking, and income. Blacks exhibited significantly higher adjusted prevalences of periodontitis independent of their education than their White and Mexican-American counterparts. In fact, Blacks in the higher education group exhibited prevalences of periodontitis that were 2.3 and 4.9 times higher than those of their White and Mexican-American counterparts, respectively. This pattern was consistent for income categories. However, high-income Blacks exhibited higher adjusted prevalence of periodontitis than their low-income counterparts.
TABLE 3—
Prevalence and Prevalence Ratios of Periodontitis and 95% Confidence Intervals for the Independent and Joint Effect of Income and Education for Each Racial/Ethnic Group: Third National Health and Nutrition Examination Survey, 1988–1994
| Prevalence of Periodontitis | |||||||||
| Black (B) | Mexican American (MA) | White (W) | Adjusted Prevalence Ratios | ||||||
| Unadjusted | Adjusteda | Unadjusted | Adjusted | Unadjusted | Adjusted | B:W | B:MA | MA:W | |
| Overall | 14.2 | 6.9 | 9.4 | 3.0 | 5.3 | 5.2 | 1.33 | 2.30 | 0.57 |
| (11.3–17.1) | (4.4–9.4) | (6.4–12.4) | (1.5–4.5) | (4.0–6.5) | (3.8–6.5) | (1.27–1.38) | (2.21–2.39) | (0.56–0.59) | |
| Independent effect | |||||||||
| Education, y | |||||||||
| < 12 | 16.8 | 15.2 | 11.9 | 7.0 | 10.4 | 5.9 | 2.58 | 2.14 | 1.20 |
| (12.7–20.9) | (9.1–21.3) | (8.2–15.6) | (4.3–9.7) | (7.2–13.6) | (3.5–8.3) | (2.37–2.80) | (1.96–2.34) | (1.14–1.27) | |
| ≥ 12 | 11.5 | 10.2 | 3.6 | 2.2 | 4.0 | 4.4 | 2.32 | 4.86 | 0.48 |
| (7.8–15.4) | (6.5–13.9) | (1.0–6.2) | (−0.1–4.5) | (2.8–5.2) | (3.0–5.8) | (2.20–2.44) | (4.57–5.16) | (0.46–0.49) | |
| Income | |||||||||
| < $20 000 | 17.8 | 10.7 | 13.2 | 5.2 | 10.0 | 8.2 | 1.30 | 2.06 | 0.63 |
| (14.0–21.5) | (6.1–15.3) | (9.0–17.4) | (2.2–8.2) | (6.4–13.6) | (5.1–11.2) | (1.21–1.41) | (1.96–2.15) | (0.60–0.67) | |
| ≥ $20 000 | 11.5 | 13.9 | 3.9 | 5.1 | 3.6 | 3.7 | 3.76 | 2.72 | 1.38 |
| (7.6–15.4) | (9.3–18.4) | (1.1–6.7) | (1.8–8.6) | (2.3–4.9) | (2.4–5.0) | (3.56–3.97) | (2.54–2.92) | (1.31–1.45) | |
| Joint effectb | |||||||||
| Low education–low income | 17.6 | 13.4 | 13.4 | 7.2 | 13.0 | 9.3 | 1.44 | 1.86 | 0.77 |
| (13.2–22.0) | (8.2–18.6) | (9.1–17.7) | (2.5–11.8) | (7.8–18.3) | (5.7–12.8) | (1.32–1.57) | (1.69–2.5) | (0.71–0.84) | |
| Low education–high income | 17.6 | 16.4 | 7.9 | 7.0 | 6.8 | 5.3 | 3.09 | 2.34 | 1.32 |
| (7.6–27.6) | (6.5–26.3) | (2.0–13.7) | (2.5–11.5) | (2.3–11.3) | (2.1–8.5) | (2.71–3.53) | (2.03–2.70) | (1.22–1.43) | |
| High education–low income | 18.3 | 8.2 | 12.2 | 1.9 | 7.8 | 8.3 | 0.99 | 4.31 | 0.23 |
| (10.4–26.1) | (1.8–14.5) | (1.4–23.0) | (−0.8–4.6) | (3.8–11.8) | (4.1–12.5) | (0.89–1.10) | (3.94–4.72) | (0.21–0.24) | |
| High education–high income | 8.9 | 11.6 | 1.2 | 2.1 | 3.2 | 3.4 | 3.41 | 5.52 | 0.61 |
| (5.0–12.8) | (7.2–16.0) | (−0.4–2.8) | (−0.8–5.0) | (2.0–4.4) | (2.1–4.7) | (3.22–3.61) | (5.13–5.94) | (0.59–0.64) | |
aPrevalences were estimated from logistic regression models adjusting for age (categorical), gender, presence of health insurance, time since last dental visit, history of diabetes, and smoking. The prevalences for each racial/ethnic group are adjusted for income level and education level. The prevalences of periodontitis in education for each racial/ethnic group are adjusted for income and vice versa (i.e., periodontal prevalences for income level are adjusted for education level).
bThese categories are cross-classified categories of income (< $20 000 vs ≥ $20 000) and education (< 12 years vs ≥ 12 years) for each racial/ethnic group.
When the unadjusted joint effects of income and education were considered, those with both higher education and higher income exhibited the lowest prevalences of periodontitis regardless of racial/ethnic group. After adjusting for all covariates in the model, this pattern remained for Whites, whereas for Mexican Americans and Blacks, those with high education but low income exhibited the lowest prevalence of periodontitis.
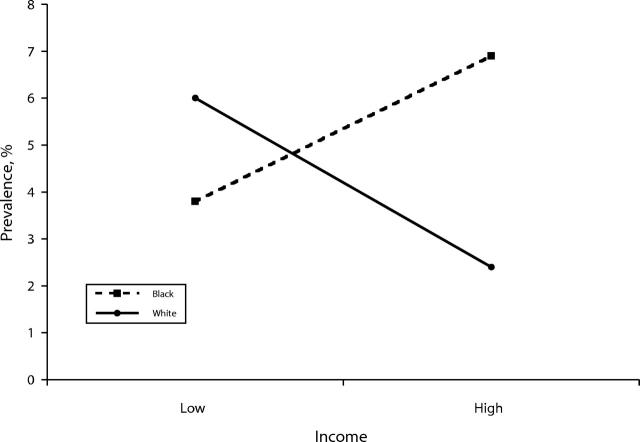
Figure 1 ▶ shows a significant interaction between income and race/ethnicity on the prevalence of periodontitis after adjusting for age, gender, education, presence of insurance, time since last dental visit, smoking, and diabetes (P = .006). Blacks exhibited a direct association between income and periodontitis, whereas their White counterparts exhibited the expected inverse association. This pattern remained unchanged when 3 categories for income (i.e., ≤ $16 999, $17 000–$34 999 and ≥ $35 000) were used in the analysis. Mexican Americans exhibited a prevalence of 2.0% for both categories, low and high income (data not included in the figure). The absolute values of the estimated net effects of income (adjusted for other covariates) on the prevalence of periodontitis for Blacks and Whites were not too different, although they were in different directions (3.1 % increase for Blacks and 3.6% decrease for Whites).
FIGURE 1—
The effect of income on prevalence of periodontitis in Blacks and Whites: Third National Health and Nutrition Examination Survey, 1988–1994.
Note. Interaction obtained from a model with race/ethnicity as an independent covariates and adjusted for age, gender, education, presence of insurance, time since last dental visit, smoking, and diabetes. Income categories were specified as low (< $20 000) and high (≥ $20 000).
DISCUSSION
To our knowledge, there has been no study assessing the association between the prevalence of periodontitis and income and education across racial/ethnic groups in older adults. Our study found that Blacks with higher education and income had a significantly higher prevalence of periodontitis than their White and Mexican-American counterparts. Furthermore, the prevalence of periodontitis for income categories was different for each racial/ethnic group. Highincome Blacks exhibited a higher prevalence of periodontitis than low-income Blacks and high-income Whites. These findings persist when 3 categories for income were considered in the analyses. For Mexican Americans, there was some variation in the prevalence of periodontitis with respect to their White counterparts, ranging from lower to slightly higher prevalences. When crossclassified categories for income and education were considered in the model, Blacks with higher education and income exhibited the lowest decrease in the prevalence of periodontitis compared with their White and Mexican-American counterparts.
When studying periodontitis, one of the major conundrums is the case definition to be used because there is no standard definition. The prevalence of periodontitis thus depends on the definition used. Previous studies have used several combinations of CAL and PD to establish periodontitis case definitions.25,27,32–34 The rationale behind CAL and PD combinations is that CAL represents a cumulative measure of periodontal tissue destruction throughout life, whereas PD indicates the presence of active disease.15,33 For this study, we tested several case definitions based on different combinations of PD and CAL. All the definitions tested led to the same conclusion: Blacks exhibited twice the prevalence of periodontitis as Whites, whereas Mexican Americans exhibited a prevalence intermediate between those for Blacks and Whites. Therefore, it is very unlikely that our results would vary if a different case definition was used in the study.
Previous studies have shown that people with low SES exhibit a higher prevalence of periodontitis than their high-SES counterparts, regardless of the SES indicator used. This finding has been consistently reported across racial/ethnic groups.19–25 Our study, although somewhat consistent with previous studies, shows that the relationship between the prevalence of periodontitis and income and education is different across racial/ethnic groups. When compared with Whites and Mexican Americans, Blacks exhibited the highest prevalence of periodontitis independent of their education, whereas high-income Blacks exhibited the highest prevalence of periodontitis. Mexican Americans exhibited the lowest prevalence of periodontitis regardless of their income and education. When evaluating the contribution of SES on racial/ethnic health differences, some studies suggest that SES could be an important factor in explaining the existing racial/ethnic health differences,47–49 whereas other studies underscore measurement problems when evaluating the effect of SES on health.7,50–53 The latter explanation is because of the incommensurability of SES across racial/ethnic groups, measurement error, and devaluation of particular racial/ethnic groups’ SES resources (for example, housing equity is a major source of wealth. However, Blacks tend to receive smaller returns on their real state investment than Whites). Our findings that Blacks received the lowest benefit from the SES indicators on periodontal health could be a combination of the aforementioned factors or perhaps an indication of how far, in general, Blacks lag behind their White counterparts to begin with. Although Blacks and Whites exhibited an opposite relation between the prevalence of periodontitis and income, the gap between Blacks and Whites was wider at higher income levels than at the lower levels. This finding could suggest different mechanisms by which income influences periodontal health for each racial/ethnic group and perhaps could reflect the incommensurability of income across racial/ethnic groups. Moreover, there is evidence that SES indicators do not carry the same meaning across racial/ethnic groups, leading to residual confounding.50,52 This residual confounding could then translate into the observed racial/ethnic differences in periodontal disease.
The association between income and the prevalence of periodontitis was modified by race/ethnicity. The estimate of this interaction remained nearly unchanged when education was either excluded or included as a 3- or 4-category specification instead of 2 categories in the model (data not shown). These findings suggested that residual confounding by education is an unlikely explanation for this interaction and that the effect of the interaction was independent of education. This interaction, although intriguing because it goes against the common inverse relation between SES indicators and most health outcomes reported by most studies,3,5,7 could help our understanding of the effect of the SES-race/ethnicity association on periodontal health. Very little is known regarding how SES factors operate within each racial/ethnic group, and research in this area could help our understanding regarding the differences between racial/ethnic groups that may contribute to oral health disparities in general.
Although most of the existing evidence suggests an inverse association between SES and periodontal diseases,18–24 and health outcomes in general,3,5,7 a few studies suggest that the social conditions in which groups are embedded could determine different levels of exposure to stress, which then could affect health.54–57 Based on these studies, it is possible that high-income Blacks experienced a higher level of stress trying to cope with their everyday demands. This stress, associated with, and perhaps increased by, other circumstances such as racism58–60 could translate into a higher prevalence of periodontal disease. For example, studies of periodontal health have found an association between periodontitis and stressors related to work,61 stressful life events,62 and psychosocial factors.63 Recently, Genco and colleagues reported that psychosocial measures of stress were significant risk indicators for more severe periodontal disease in an adult population.64 Further studies need to be done to help elucidate our understanding of the interplay among SES indicators, stress, and periodontitis among racial/ethnic groups.
By restricting our study to NHANES III participants who received a complete periodontal examination, questions related to the possibility of selection bias due to a healthy or survivor teeth effect are raised. Analysis (not shown) demonstrated that those participants who received a partial examination (i.e., < 14 teeth examined) exhibited a lower prevalence of periodontitis (P < .001) than their peers with a complete examination. However, there were no differences among racial/ethnic groups between those who received a partial examination and those who received a complete examination (P = .3273). In addition, when compared with those with a complete examination, the racial/ethnic pattern of the prevalence of periodontitis for those with partial examinations was similar to the one presented in our results. Finally, this restriction could question the direct association between income and periodontitis observed in Blacks. However, we repeated the analysis including both Blacks with a complete and a partial periodontal assessment, and the direct association persisted, although not with the same magnitude (10.4% for low income vs 11.7% for high income). Because of the age range of our study population, exclusions for medical reasons were also a concern. Analysis (not shown) indicated that there was no statistically significant association between medical exclusion and (1) race/ethnicity (P = .06) and (2) education (P = .13). However, there was an association between medical exclusion and income, with those with low incomes being more likely to be excluded (P = .01).
The major limitation of the study was its cross-sectional nature, which limited our ability to establish a causal relationship. However, this study has several strengths that include (1) the racial/ethnic diversity and representativeness of the sample, and (2) the age range included in our analysis, which included people who had achieved possibly the highest level of education they would attain during their lifetime. This educational attainment has a stabilizing effect on income.
Our findings suggest that Blacks demonstrated a lower decrease in the prevalence of periodontitis across the education and income categories than their Mexican-American and White peers. These findings could confirm the incommensurability of SES indicators across racial/ethnic groups and perhaps could reflect the historical implications of unequal opportunities for Blacks in our society. Therefore, our findings call attention to the importance of recognizing SES health differences across racial/ethnic groups within our social, political, and historical context. It is clear that race/ethnicity and SES indicators are intertwined in explaining the health status, including the oral health, of the US population. However, studies in this area are far from conclusive, and many questions remain unanswered. As we move forward to reduce and eliminate health disparities, we must do better to disentangle and to explain these differences using a framework that accounts for the implications of social constructs such as race/ethnicity on the health of the US population.
Acknowledgments
This work was supported by Columbia Center for the Active Life on Minority Elders (CALME) pilot fund and the National Institute of Dental and Craniofacial Research (T32 DE 07157) to Luisa N. Borrell.
The authors thank Ana Diez-Roux, Ezra Susser, and Nitsa Gilbert for comments on earlier drafts.
Human Participant Protection The data were collected with the informed consent of the respondents following procedures approved by the institutional review board of the National Center for Health Statistics. In addition, the analysis was approved by the institutional review board at Columbia University.
Contributors L. N. Borrell planned the study, analyzed the data, and wrote the article. B. A. Burt, H. W. Neighbors, and G. W. Taylor contributed to interpreting the analyses and reviewing and writing the article.
Peer Reviewed
References
- 1.Manton KG, Patrick CH, Johnson KW. Health differentials between blacks and whites: recent trends in mortality and morbidity. Milbank Q. 1987;65:100–128. [PubMed] [Google Scholar]
- 2.Miller SM. Race in the health of America. Milbank Q. 1987;65(suppl 2):500–531. [PubMed] [Google Scholar]
- 3.Williams DR, Collins C. US socioeconomic and racial differences in health–patterns and explanations. Annu Rev Sociol. 1995;21:349–386. [Google Scholar]
- 4.Cooper RS. Health and the social status of blacks in the United States. Ann Epidemiol. 1993;3:137–144. [DOI] [PubMed] [Google Scholar]
- 5.Feinstein JS. The relationship between socioeconomic Status and health: a review of the literature. Milbank Q. 1993;71:279–322. [PubMed] [Google Scholar]
- 6.Navarro V. Race or class versus Race and class: mortality differential in the United States. Lancet. 1990;336:1230–1240. [DOI] [PubMed] [Google Scholar]
- 7.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188. [DOI] [PubMed] [Google Scholar]
- 8.Oral Health Coordinating Committee, Public Health Service. Toward improving the oral health of Americans: an overview of oral health status, resources, and care delivery. Public Health Rep. 1993;108:657–672. [PMC free article] [PubMed] [Google Scholar]
- 9.Caplan DJ, Weintraub JA. The oral health burden in the United States: a summary of recent epidemiologic studies. J Dent Educ. 1993;57:853–862. [PubMed] [Google Scholar]
- 10.White BA, Caplan DJ, Weintraub JA. A quarter century of changes in oral health in the United States. J Dent Educ. 1995;59:19–57. [PubMed] [Google Scholar]
- 11.Rozier RG, Hughes JT, Ramsey D. The epidemiology of dental diseases in North Carolina. J Public Health Dent. 1981;41:14–24. [DOI] [PubMed] [Google Scholar]
- 12.Rozier RG, Beck JD. Epidemiology of oral diseases. Curr Opin Dent. 1991;1:308–315. [PubMed] [Google Scholar]
- 13.Brown LJ, Swango PA. Trends in caries experience in US employed adults from 1971–74 to 1985: cross-sectional comparisons. Adv Dent Res. 1993;7:52–60. [DOI] [PubMed] [Google Scholar]
- 14.Brown LJ, Wall TP, Lazar V. Trends in caries among adults 18 to 45 years old. J Am Dent Assoc. 2002;133:827–834. [DOI] [PubMed] [Google Scholar]
- 15.Burt BA, Eklund SA. Dentistry, Dental Practice, and the Community. Philadelphia, Pa: WB Saunders Co; 1999.
- 16.Oral Health in America: A Report of the Surgeon General. Rockville, Md: National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000.
- 17.Davidson PL, Andersen RM, Marcus M, et al. Indicators of oral health in diverse ethnic and age groups: findings from the International Collaborative Study of Oral Health Outcomes (ICS-II) USA research locations. J Med Syst. 1996;20:295–316. [DOI] [PubMed] [Google Scholar]
- 18.Albandar JM. Periodontal diseases in North America. Periodontology 2000. 2002;29:31–69. [DOI] [PubMed] [Google Scholar]
- 19.Oliver RC, Brown LJ, Loe H. Periodontal diseases in the United States population. J Periodontol. 1998;69:269–278. [DOI] [PubMed] [Google Scholar]
- 20.Oliver RC, Brown LJ, Loe H. Variations in the prevalence and extent of periodontitis. J Am Dent Assoc. 1991;122:43–48. [DOI] [PubMed] [Google Scholar]
- 21.Nikias MK, Fink R, Sollecito W. Oral health status in relation to socioeconomic and ethnic characteristics of urban adults in the USA. Community Dent Oral Epidemiol. 1977;5:200–206. [DOI] [PubMed] [Google Scholar]
- 22.Borrell LN, Lynch JW, Neighbors H, Burt BA, Gillespie BW. Is there homogeneity in periodontal health between African Americans and Mexican Americans? Ethn Dis. 2002;12:97–110. [PubMed] [Google Scholar]
- 23.Borrell LN, Burt BA, Gillespie BW, Lynch JW, Neighbors H. Race and periodontitis in the US: beyond black and white. J Public Health Dent. 2002;62:92–101. [DOI] [PubMed] [Google Scholar]
- 24.Elter JR, Beck JD, Slade GD, Offenbacher S. Etiologic models for incident periodontal attachment loss in older adults. J Clin Periodontol. 1999;26:113–123. [DOI] [PubMed] [Google Scholar]
- 25.Locker D, Leake JL. Risk indicators and risk markers for periodontal disease experience in older adults living independently in Ontario, Canada. J Dent Res. 1993;72:9–17. [DOI] [PubMed] [Google Scholar]
- 26.Beck JD, Cusmano L, Green-Helms W, Koch GG, Offenbacher S. A 5-year study of attachment loss in community-dwelling older adults: incidence density. J Periodontal Res. 1997;32:506–515. [DOI] [PubMed] [Google Scholar]
- 27.Beck JD, Koch GG, Rozier RG, Tudor GE. Prevalence and risk indicators for periodontal attachment loss in a population of older community-dwelling blacks and whites. J Periodontol. 1990;61:521–528. [DOI] [PubMed] [Google Scholar]
- 28.Beck JD, Koch GG, Offenbacher S. Incidence of attachment loss over 3 years in older adults—new and progressing lesions. Community Dent Oral Epidemiol. 1995;23:291–296. [DOI] [PubMed] [Google Scholar]
- 29.Borrell LN, Taylor GW, Woolfolk MW, et al. Factors influencing the effect of race on established periodontitis prevalence. J Public Health Dent. 2003;63:20–29. [DOI] [PubMed] [Google Scholar]
- 30.Ezzati TM, Massey JT, Waksberg J, Chu A, Maurer KR. Sample design: Third National Health and Nutrition Examination Survey. Vital Health Stat 2. 1992:No. 113: 1–35. [PubMed] [Google Scholar]
- 31.National Center for Health Statistics. NHANES III Reference Manual and Reports [CD-ROM]. Hyattsville Md: Centers for Disease Control and Prevention; 1996.
- 32.Machtei EE, Christersson LA, Grossi SG, Dunford R, Zambon JJ, Genco RJ. Clinical criteria for the definition of “established periodontitis.” J Periodontol. 1992;63:206–214. [DOI] [PubMed] [Google Scholar]
- 33.Arbes SJ Jr, Agustsdottir H, Slade GD. Environmental tobacco smoke and periodontal disease in the United States. Am J Public Health. 2001;91:253–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Albandar JM, Brunelle JA, Kingman A. Destructive periodontal disease in adults 30 years of age and older in the United States, 1988–1994. J Periodontol. 1999;70:13–29. [DOI] [PubMed] [Google Scholar]
- 35.Melvin WL, Sandifer JB, Gray JL. The prevalence and sex ratio of juvenile periodontitis in a young racially mixed population. J Periodontol. 1991;62:330–334. [DOI] [PubMed] [Google Scholar]
- 36.Loe H, Brown LJ. Early onset periodontitis in the United States of America. J Periodontol. 1991;62:608–616. [DOI] [PubMed] [Google Scholar]
- 37.Beck JD, Koch GG. Characteristics of older adults experiencing periodontal attachment loss as gingival recession or probing depth. J Periodontal Res. 1994;29:290–298. [DOI] [PubMed] [Google Scholar]
- 38.Cherry-Peppers G, Sinkford JC, Newman ES, Sanders CF, Knight RS. Primary oral health care in black Americans: an assessment of current status and future needs. J Natl Med Assoc. 1995;87:136–140. [PMC free article] [PubMed] [Google Scholar]
- 39.Drury TF, Garcia I, Adesanya M. Socioeconomic disparities in adult oral health in the United States. Ann N Y Acad Sci. 1999;896:322–324. [DOI] [PubMed] [Google Scholar]
- 40.Albandar JM. Global risk factors and risk indicators for periodontal diseases. Periodontology 2000. 2002;29:177–206. [DOI] [PubMed] [Google Scholar]
- 41.Albandar JM, Kingman A, Brown LJ, Loe H. Gingival bleeding and subgingival calculus as determinants of disease progression in early-onset periodontitis. J Clin Periodontol. 1998;25:231–237. [DOI] [PubMed] [Google Scholar]
- 42.Albandar JM, Brown LJ, Brunelle JA, Loe H. Gingival state and dental calculus in early-onset periodontitis. J Periodontol. 1996;7:953–959. [DOI] [PubMed] [Google Scholar]
- 43.Mandel ID. Calculus update: prevalence, pathogenicity and prevention. J Am Dent Assoc. 1995;126:573–580. [DOI] [PubMed] [Google Scholar]
- 44.Mantel N. Why stepdown procedures in variable selection. Technometrics. 1970;12:621–625. [Google Scholar]
- 45.SAS/STAT User’s Guide, Version 8.0. Cary NC: SAS Institute Inc; 1999.
- 46.SUDAAN User’s Manual, Release 8.0. Research Triangle Park NC: Research Triangle Institute; 2001.
- 47.Hayward MD, Crimmins EM, Miles TP, Yang Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. Am Sociol Rev. 2000;65:910–930. [Google Scholar]
- 48.House JS, Williams DR. Understanding and reducing socioeconomic and racial/ethnic disparities in health. In: Smedley BD, Syme SL, eds. Promoting Health: Intervention Strategies from Social and Behavioral Research. Washington, DC: National Academy Press; 2000:81–124. [PubMed]
- 49.House JS. Understanding social factors and inequalities in health: 20th century progress and 21st century prospects. J Health Soc Behav. 2001;43:125–142. [PubMed] [Google Scholar]
- 50.Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8:621–628. [PubMed] [Google Scholar]
- 51.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. [DOI] [PubMed] [Google Scholar]
- 52.Williams DR. Race/ethnicity and socioeconomic status: measurement and methodological issues. Int J Health Serv. 1996;26:483–505. [DOI] [PubMed] [Google Scholar]
- 53.Lynch J, Kaplan G. Socioeconomic position. In: Berkman LF, Kawachi I, eds. Social Epidemiology. New York, NY: Oxford University Press; 2000:13–35.
- 54.Pearlin LI. The sociological study of stress. J Health Soc Behav. 1989;30:241–256. [PubMed] [Google Scholar]
- 55.Williams DR, House JS. Stress, social support, control and coping: a social epidemiological view. WHO Reg Publ Eur Ser. 1991;37:147–172. [PubMed] [Google Scholar]
- 56.Brunner E, Marmot M. Social organization, stress and health. In: Marmot MG, Wilkinson RG, eds. Social Determinants of Health. New York, NY: Oxford University Press; 1999:17–43.
- 57.James SA, Hartnett SA, Kalsbeek WD. John Henryism and blood pressure differences among black men. J Behav Med. 1983;6:259–278. [DOI] [PubMed] [Google Scholar]
- 58.Williams DR. Race and health: basic questions, emerging directions. Ann Epidemiol. 1997;7:322–333. [DOI] [PubMed] [Google Scholar]
- 59.Williams DR. Racism and health: a research agenda. Ethn Dis. 1996;6:1–8. [PubMed] [Google Scholar]
- 60.Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethn Health. 2000;5:243–268. [DOI] [PubMed] [Google Scholar]
- 61.Marcenes WS, Sheiham A. The relationship between work stress and oral health status. Soc Sci Med. 1992;35:1511–1520. [DOI] [PubMed] [Google Scholar]
- 62.Green LW, Tryon WW, Marks B, Huryn J. Periodontal disease as a function of life events stress. J Human Stress. 1986;12:32–36. [DOI] [PubMed] [Google Scholar]
- 63.Freeman R, Goss S. Stress measures as predictors of periodontal disease—a preliminary communication. Community Dent Oral Epidemiol. 1993;21:176–177. [DOI] [PubMed] [Google Scholar]
- 64.Genco RJ, Ho AW, Grossi SG, Dunford RG, Tedesco LA. Relationship of stress, distress, and inadequate coping behaviors to periodontal disease. J Periodontol. 1999;70:711–723. [DOI] [PubMed] [Google Scholar]