Abstract
Objectives. We examined current racial/ethnic differences in immunization coverage rates among US preschool children.
Methods. Using National Immunization Survey data from 1996 through 2001, we compared vaccination coverage rates between non-Hispanic White, non-Hispanic Black, Hispanic, and Asian preschool children.
Results. During the 6-year study period, the immunization coverage gap between White and Black children widened by an average of 1.1% each year, and the gap between White and Hispanic children widened by an average of 0.5% each year. The gap between White and Asian children narrowed by an average of 0.8% each year.
Conclusions. Racial/ethnic disparities in preschool immunization coverage rates have increased significantly among some groups; critical improvements in identifying, understanding, and addressing race/ethnicity-specific health care differences are needed to achieve the Healthy People 2010 goal of eliminating disparities.
Although childhood immunization coverage in the United States has reached an all-time high,1 racial/ethnic disparities persist at the national and local levels, even when the effects of socioeconomic differences are considered.2–5 Although gaps in childhood immunization coverage among racial/ethnic groups decreased during the past decade and are substantially smaller than gaps for most other health care indicators,6 we have a national commitment to “leave no child behind.” Eliminating disparities is one of the Healthy People 2010 goals6 and one of the 6 overarching goals identified in the Institute of Medicine’s Crossing the Quality Chasm report.7 In the present study, we examined racial/ethnic differences in immunization coverage rates among United States children aged 19 to 35 months during the years 1996 through 2001.
METHODS
The National Immunization Survey (NIS) is conducted annually by the Centers for Disease Control and Prevention to estimate vaccination coverage among the US population of 19- to 35-month-old children. The NIS is a random-digit-dialed survey of households with age-eligible children followed by a mail survey of the eligible children’s vaccine providers to obtain vaccination information. Analyses of NIS data focus on sampled children whose providers respond to the survey. Although use of provider data in combination with household data significantly reduces response error, provider-reported vaccination status is not without error and can lead to slight underreporting of “true” vaccination coverage levels. Details of NIS methods appear elsewhere.1,8,9
During the random-digit-dialed portion of the NIS interview, respondents identify their child’s race/ethnicity. Respondents are given the following racial categories from which to choose: White, Black, American Indian, Asian, Hispanic, and other.8 For the period 1996 through 2001, we calculated the percentages of Hispanic, non-Hispanic White, non-Hispanic Black, and non-Hispanic Asian children who were up to date for the 4:3:1:3:3 series (4 or more doses of diphtheria and tetanus toxoids and [acellular] pertussis vaccine; 3 or more doses of poliovirus vaccine; 1 or more doses of measles-containing vaccine; 3 or more doses of Haemophilus influenzae type b vaccine; and 3 or more doses of hepatitis B vaccine). Yearly sample sizes varied, but only slightly. For 2001, sample sizes were as follows: Hispanic, 4676; non-Hispanic White, 14 052; non-Hispanic Black, 3555; and non-Hispanic Asian, 925. We did not consider other racial/ethnic groups because the number of children surveyed was small.
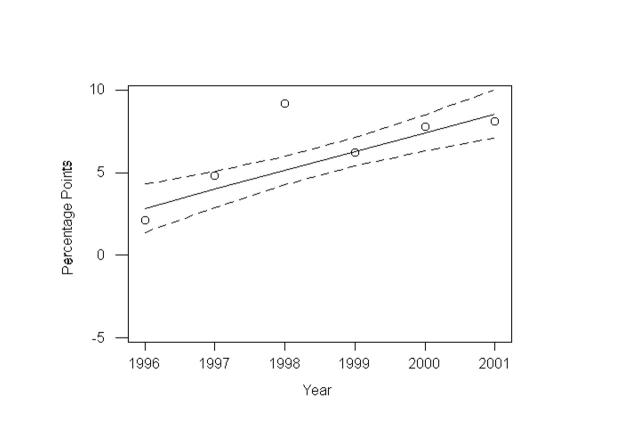
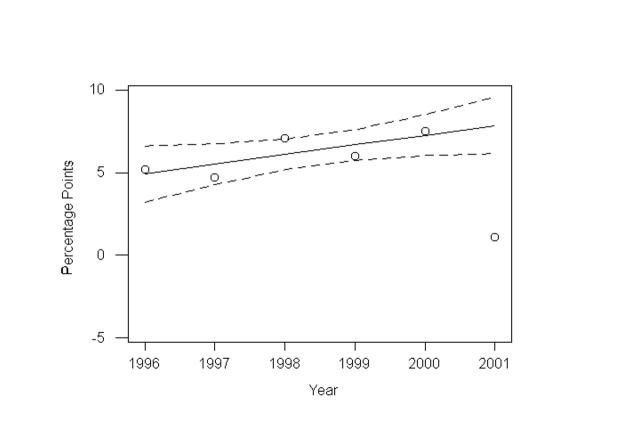
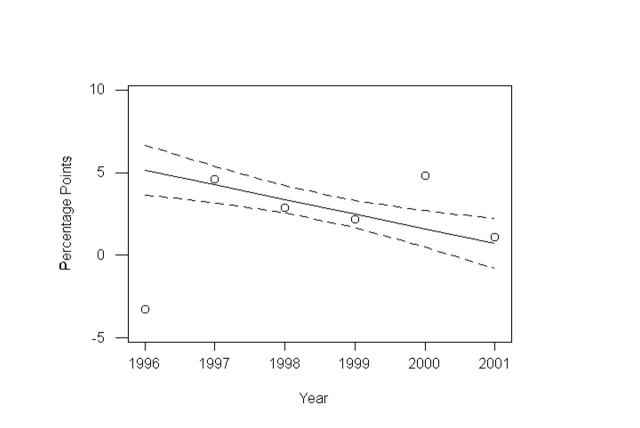
Using these coverage levels, we plotted robust regression models10,11 of annual changes in the differences in immunization coverage rates between non-Hispanic Whites and non-Hispanic Blacks, Hispanics, and Asians, respectively. In robust regression analyses, iteratively reweighted least squares are used to estimate both regression coefficients and standard errors. The procedure assigns weights to each of the observations, with high leverage or influence receiving a lower weight. The slopes of these straight-line models indicated annual changes in differences between immunization coverage rates among non-Hispanic Whites and the other racial/ethnic groups assessed (with the exception of random variation, which was constant for all years). A positive slope signals increasing differences, and a negative slope signals decreasing differences. Pointwise 95% confidence intervals (CIs) were calculated for each regression line. All calculations were performed with Stata (version 7)12 and Minitab (version 12.2).13
We used robust regression for 2 reasons. First, our data contained several possible outliers, such as coverage rates among Hispanics in 2001 and among non-Hispanic Asians in 1996. The results of robust regression are much less sensitive to outliers than those of the more familiar ordinary least squares regression.10,11 Second, least squares regression is valid only when differences between observed and fitted values are normally distributed. In our study, histograms of differences (data not presented) suggested skewed distributions, which could cast the results of ordinary least squares regression into serious doubt but would have relatively little impact on the results of robust regression.10
RESULTS
Immunization coverage rates among non-Hispanic White, Hispanic, non-Hispanic Black, and non-Hispanic Asian children 19 to 35 months of age during 1996 through 2001 are presented in Table 1 ▶. Regression lines for the differences in rates between non-Hispanic Whites and non-Hispanic Blacks, Hispanics, and Asians, respectively, are shown in Figures 1 ▶, 2 ▶, and 3 ▶. According to these models, between 1996 and 2001, the immunization coverage gap between non-Hispanic Whites and non-Hispanic Blacks widened by an average of 1.1% (95% CI = 0.4%, 1.8%; P = .01) each year, and the gap between non-Hispanic Whites and Hispanics widened by an average of 0.5% (95% CI = −0.5%, 1.5%; P = .14). The gap between non-Hispanic Whites and non-Hispanic Asians narrowed by an average of 0.8% (95% CI = 0.0%, 1.6%; P = .06) each year. We have less uncertainty regarding the trend in the White–Black gap, because the 95% confidence interval for the slope of this comparison did not contain zero.
TABLE 1—
4:3:1:3:3 Coverage, by Race/Ethnicity
| Year | Non-Hispanic Whites, % (95% CI) | Hispanics, % (95% CI) | Non-Hispanic Blacks, % (95% CI) | Non-Hispanic Asians, % (95% CI) |
| 1996 | 68.9 (67.7, 70.1) | 63.7 (60.8, 66.6) | 66.8 (64.0, 69.6) | 72.2 (67.1, 77.3) |
| 1997 | 70.4 (69.3, 71.5) | 65.7 (62.8, 68.6) | 65.6 (62.8, 68.4) | 65.8 (60.4, 71.2) |
| 1998 | 75.6 (74.5, 76.7) | 68.7 (66.0, 71.4) | 66.6 (63.9, 69.3) | 72.9 (67.3, 78.5) |
| 1999 | 75.6 (74.5, 76.7) | 69.6 (67.3, 71.9) | 69.4 (66.8, 72.0) | 73.4 (68.7, 78.1) |
| 2000 | 76.0 (74.9, 77.1) | 68.5 (66.3, 70.7) | 68.2 (65.6, 70.8) | 71.2 (66.0, 76.4) |
| 2001 | 75.2 (74.1, 76.3) | 74.1 (72.1, 76.1) | 67.1 (64.4, 69.8) | 74.1 (69.4, 78.8) |
Note. CI = confidence interval. 4:3:1:3:3 = 4 or more doses of diphtheria and tetanus toxoids and (acellular) pertussis vaccine; 3 or more doses of poliovirus vaccine; 1 or more doses of measles-containing vaccine; 3 or more doses of Haemophilus influenzae type b vaccine; and 3 or more doses of hepatitis B vaccine.
FIGURE 1—
4:3:1:3:3 coverage: non-Hispanic Whites vs non-Hispanic Blacks.
Note. 4:3:1:3:3 = 4 or more doses of diphtheria and tetanus toxoids and (acellular) pertussis vaccine; 3 or more doses of poliovirus vaccine; 1 or more doses of measles-containing vaccine; 3 or more doses of Haemophilus influenzae type b vaccine; and 3 or more doses of hepatitis B vaccine. Dashed lines are 95% confidence intervals for the regression line. β = 1.14; 95% CI = 0.46, 1.83; P = .01.
FIGURE 2—
4:3:1:3:3 coverage: non-Hispanic Whites vs Hispanics.
Note. 4:3:1:3:3 = 4 or more doses of diphtheria and tetanus toxoids and (acellular) pertussis vaccine; 3 or more doses of poliovirus vaccine; 1 or more doses of measles-containing vaccine; 3 or more doses of Haemophilus influenzae type b vaccine; and 3 or more doses of hepatitis B vaccine. Dashed lines are 95% confidence intervals for the regression line. β = 0.59; 95% CI = −0.36, 1.54; P = .14.
FIGURE 3—
4:3:1:3:3 coverage: non-Hispanic Whites vs Asians.
Note. 4:3:1:3:3 = 4 or more doses of diphtheria and tetanus toxoids and (acellular) pertussis vaccine; 3 or more doses of poliovirus vaccine; 1 or more doses of measles-containing vaccine; 3 or more doses of Haemophilus influenzae type b vaccine; and 3 or more doses of hepatitis B vaccine. Dashed lines are 95% confidence intervals for the regression line. β = −0.80; 95% CI = −1.64, 0.04; P = .06.
DISCUSSION
National childhood vaccination coverage levels have increased substantially throughout the past decade,14 and immunizations have succeeded in reaching all populations in a more effective manner than most other health interventions; however, until coverage is completely equitable this success is incomplete. Reasons for racial disparities in immunization coverage are incompletely understood but may include the following: limited minority access to primary care, increased guardedness among minority parents in regard to the health care system, misconceptions about the risks and benefits of vaccination, and diminished application or effectiveness in minority populations of the standard recommended interventions used to increase immunization coverage.15
Limited access to preventive health care, including immunizations, may be related to certain known disparities in children’s health care service use patterns. For example, White children see physicians at twice the rate of minority children.16 Black and Hispanic children are overrepresented in emergency rooms and hospital outpatient departments.17 Research on Black preschool children in inner-city Los Angeles showed that late immunizations were more common among children who were not consistently connected to the health care system, and only 25% had been fully immunized by 24 months of age.4 Assessment of vaccination status and vaccine delivery is likely to be compromised among children with fragmented care that results in greater reliance on irregular health care settings such as emergency rooms.
Patients’ trust in the health care system and past experience with providers can influence their acceptance of health care.18 Conscious or unconscious stereotypes and attitudes toward certain racial/ethnic groups on the part of health care providers can significantly shape interpersonal interactions and expectations, although the way in which these attitudes affect clinical behavior and decisions is still poorly understood.19 Experiences of discrimination, whether real or perceived, could discourage members of minority groups from seeking adequate health care or accepting certain preventive services,18 including immunizations.
Parents who do not believe that the benefits of vaccination exceed its risks may be less likely to have their children immunized. Although the NIS does not routinely collect data on parents’ perceptions of vaccination, some questions that provide insight into this issue were asked in a special 2001 NIS module. Results showed that parents from different racial/ethnic groups did not differ regarding whether they believed all children should receive the same immunizations (95% of non-Hispanic White parents, 94% of Black parents, 97% of Hispanic parents, and 78% of Asian parents responded that all children should receive the same immunizations); however, non-Hispanic White parents were less likely than parents in other racial/ethnic groups to believe that their children were likely or very likely to become ill after vaccination (10% of non-Hispanic White parents, 46% of Black parents, 29% of Hispanic parents, and 47% of Asian parents responded that it was likely or very likely that their children would become ill). Although these responses were based on data from only one quarter of the NIS sample, and the data from this module are considered preliminary, such differences in beliefs could affect acceptance of vaccination and should be explored further.
Finally, although a number of interventions are effective in raising immunization coverage rates,20 the persistent gaps in immunization coverage among racial/ethnic groups could indicate that standard recommended interventions may not be equally applied or sufficiently effective in certain populations. For example, the US Task Force on Community Prevention Services strongly recommends the use of provider reminder/recall systems for improving vaccination coverage rates, and such systems have been shown to be effective in several settings, raising coverage rates by an average of 12%.20,21 This increase, though notable, is insufficient to close the gap in many hard-to-reach populations; an example is inner-city minority children, among whom 4:3:1:3:3 immunization coverage rates are considerably lower (23%–57%) than the national rate (79.1% in 2001).5,22–24 Moreover, these interventions—which rely on stable provider–patient relationships—are likely to be less effective in the case of children who have inadequate or no health insurance coverage and no usual source of health care.
Thus, more concerted efforts or additional strategies may be needed to address the needs of minority populations.25 A recent study conducted in Monroe County, New York, extended a recommended practice-level intervention—patient reminder/recall and outreach—to the community level; the result was significantly decreased racial ethnic disparities in immunization rates.26 This study applied a carefully implemented reminder/recall and outreach intervention to the largest primary care practices serving an inner-city community where a large number of minority children resided. Between 1995 and 1999, this community-wide effort reduced immunization rate disparities between White and Black children (from 13% to 7%) and between White and Hispanic children (from 15% to 1%). The authors suggested that applying community-wide interventions in geographic areas where minority children reside may reduce disparities without the need for different interventions according to race or ethnicity.
Interventions that link immunization with distribution of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food vouchers have shown improvements in vaccination coverage rates ranging from 4% to 34% in diverse, low-income populations.21,27 Voucher incentive interventions require families whose children are behind on immunizations to return to the WIC site more frequently than would otherwise be required (e.g., monthly instead of every 2–3 months) and involve a referral for immunizations at the child’s medical home, where continuous, coordinated, family-centered care is given. This intervention effectively reaches minority populations, and the average cost per additional child brought up to date over a 2-year period is relatively low, ranging from $30 to $7328,29; however, these linkages involve considerable resource commitment on the part of WIC clinic staff.
A key goal of Healthy People 2010 is to eliminate racial/ethnic health disparities. In line with this goal, we used fitted straight-line projections to extrapolate immunization coverage differences between non-Hispanic Whites and the other racial/ethnic groups assessed here through 2010. A major assumption was made with these extrapolations: that the rate of change in the differences is constant over time. Obviously, a straight line cannot represent all of the complex factors that influence differences in immunization coverage rates between Whites and minority groups, and prediction limits are wide, especially as one extrapolates further out in time. But given this critical caveat, if current trends continue, the gaps in preschool immunization coverage rates between non-Hispanic Whites and non-Hispanic Blacks and Hispanics will widen significantly (2010 coverage differences: White–Black, 18.8% [95% CI = 11.8%, 25.8%]; White–Hispanic, 13.2% [95% CI = 3.6%, 22.8%]), while the gap between non-Hispanic Whites and non-Hispanic Asians will exhibit a reversal, with higher coverage among Asians than among Whites (2010 Asian–White coverage difference:7.3% [95% CI = −3.4%, 18.0%]). Because the prediction limits for the Asian–White projection include zero, this result involves considerable uncertainty.
However, an assumption we made could in fact accentuate the differences just noted. There is some evidence from the NIS that members of racial/ethnic minority groups are less likely to provide consent to have their children’s providers contacted for vaccination history information. Although statistical adjustments are made to correct for this difference, the correction assumes that racial/ethnic minority children who do not have provider-reported vaccination histories are similar to racial/ethnic minority children who have such histories. This assumption may not be exactly correct, and it is possible that children without provider data are less likely to be fully immunized than children with provider data. If this is the case, the trends in disparities between White children and Black or Hispanic children would be greater than those reported here.
These rough projections should not be taken as dire predictions but should be viewed as a call to action. The sources of these disparities are complex and relate to both historic and contemporary inequities. To eliminate disparities, comprehensive, multilevel strategies should be developed that involve a more complete recognition of the importance of behavioral, social, economic, and environmental influences on health.30 This is also a call for increased awareness. Health disparities must be more carefully measured and monitored. Current data collection methods need to be improved so that racial/ethnic health care disparities are adequately identified, adequately adjusted in terms of socioeconomic status, and adequately sampled, allowing disparities to be understood at the local or, at least, state level.31,32
The nation made a commitment to increase overall childhood immunization coverage rates with the enactment of the Childhood Immunization Initiative in 1993,33 and national childhood coverage rates have risen substantially. It is possible to eliminate disparities in immunization, but efforts in this area will require a similar commitment that is both broad and sustained.
Acknowledgments
We thank Ram Jain, PhD, Abigail Shefer, MD, Lance Rodewald, MD, and Mary McCauley, MTSC, for their critical contributions to this article and Camara P. Jones, MD, PhD, and Marilyn M. Metzler, RN, for their thoughtful review of the article.
Human Participant Protection The National Immunization Survey protocol was approved by the institutional review board of the National Center for Health Statistics.
Contributors All of the authors made substantial contributions to the conception of the study and to the analysis and interpretation of data.
Peer Reviewed
References
- 1.Luman ET, Barker LE, Simpson DM, Rodewald LE, Szilagyi PG, Zhao Z. National, state, and urban-area vaccination-coverage levels among children aged 19–35 months, United States, 1999. Am J Prev Med. 2001;20(suppl 4):88–153. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Vaccination coverage by race/ethnicity and poverty level among children aged 19–35 months—United States, 1997. MMWR Morb Mortal Wkly Rep. 1998;47:956–959. [PubMed] [Google Scholar]
- 3.Herrera GA, Zhao Z, Klevens RM. Variation in vaccination coverage among children of Hispanic ancestry. Am J Prev Med. 2001;20(suppl 1):69–74. [DOI] [PubMed] [Google Scholar]
- 4.Wood DL, Sherbourne CD, Halfon N, et al. Factors related to immunization status among inner-city Latino and African American preschoolers. Pediatrics. 1995;96:295–301. [PubMed] [Google Scholar]
- 5.Kenyon TA, Matuck MA, Stroh G. Persistent low immunization coverage among inner-city preschool children despite access to free vaccine. Pediatrics. 1998;101:612–616. [DOI] [PubMed] [Google Scholar]
- 6.Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington, DC: US Dept of Health and Human Services; 2000.
- 7.Institute of Medicine. Crossing the Quality Chasm. Washington, DC: National Academy Press; 2001.
- 8.Zell ER, Ezzati-Rice TM, Battaglia MP, Wright RA. National Immunization Survey: the methodology of a vaccination surveillance system. Public Health Rep. 2000;115:65–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith PJ, Battaglia MP, Huggins VJ, et al. Overview of the sampling design and statistical methods used in the National Immunization Survey. Am J Prev Med. 2001;20(suppl 4):17–24. [DOI] [PubMed] [Google Scholar]
- 10.Huber P. Robust estimation of a location parameter. Ann Math Stat. 1964;35:73–101. [Google Scholar]
- 11.Li G. Robust regression. In: Hoaglin DC, Mosteller F, Tukey JW, eds. Exploring Data Tables, Trends, and Shapes. New York, NY: John Wiley & Sons Inc; 1985:281–340.
- 12.Stata Statistical Software, Release 7.0. College Station, Tex: Stata Corp; 2001.
- 13.Minitab Statistical Software, Release 12. State College, Pa: Minitab Inc; 1997.
- 14.Centers for Disease Control and Prevention. Impact of vaccines universally recommended for children—United States, 1990–1998. MMWR Morb Mortal Wkly Rep. 1999;48:243–248. [PubMed] [Google Scholar]
- 15.Institute of Medicine. Introduction and literature review. In: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002:21–62.
- 16.Collins KS, Hall A, Neuhaus C. U.S. Minority Health: A Chartbook. New York, NY: Commonwealth Fund; 1999.
- 17.Lillie-Blanton M, Martinez RM, Salganicoff A. Site of medical care: do racial and ethnic differences persist? Yale J Health Policy Law Ethics. 2001;1:1–17. [PubMed] [Google Scholar]
- 18.Institute of Medicine. Assessing potential sources of racial and ethnic disparities in care: patient- and system-level factors. In: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002:101–126.
- 19.Institute of Medicine. Assessing potential sources of racial and ethnic disparities in care: the clinical encounter. In: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002:127–141.
- 20.Shefer A, Briss P, Rodewald L, et al. Improving immunization coverage rates: an evidence-based review of the literature. Epidemiol Rev. 1999;21:96–142. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Vaccine-preventable disease: improving vaccination coverage in children, adolescents, and adults. MMWR Morb Mortal Wkly Rep. 1999;48(RR-8):1–15. [Google Scholar]
- 22.Wood D, Halfon N, Donald-Sherbourne C, et al. Increasing immunization rates among inner-city, African American children: a randomized trial of case management. JAMA. 1998;279:29–34. [DOI] [PubMed] [Google Scholar]
- 23.Fairbrother G, Hanson KL, Friedman S, Butts GC. The impact of physician bonuses, enhanced fees, and feedback on childhood immunization coverage rates. Am J Public Health. 1999;89:171–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Goldstein KP, Lauderdate DS, Glushak C, Walter J, Daum RS. Immunization outreach in an inner-city housing development: reminder-recall on foot. Pediatrics. 1999;104:69. [DOI] [PubMed] [Google Scholar]
- 25.Hambidge SJ, Davidson AJ, Phibbs SL, et al. Strategies to improve immunization rates and well-child care in a disadvantaged population: a cluster randomized trial. Arch Pediatr Adolesc Med. In press. [DOI] [PubMed]
- 26.Szilagyi PG, Schaffer S, Shone L, et al. Reducing geographic, racial, and ethnic disparities in childhood immunization rates by using reminder/recall interventions in urban primary care practices. Pediatrics. 2002;110:58. [DOI] [PubMed] [Google Scholar]
- 27.Hoekstra EJ, LeBaron CW, Megaloeconomou Y, et al. Impact of a large-scale immunization initiative in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). JAMA. 1998;280:1143–1147. [DOI] [PubMed] [Google Scholar]
- 28.Hutchins S, Rosenthal J, Eason P, et al. Effectiveness and cost-effectiveness of linking the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and immunization activities. J Public Health Policy. 1999;20:408–424. [PubMed] [Google Scholar]
- 29.Shefer A, Fritchley J, Stevenson J, et al. Linking WIC and immunization services to improve preventive health care among low-income children in WIC. J Public Health Manage Pract. 2002;8:56–65. [DOI] [PubMed] [Google Scholar]
- 30.Institute of Medicine, National Research Council. Through the Kaleidoscope: Viewing the Contributions of the Behavioral and Social Sciences to Health. Washington, DC: National Academy Press; 2002. [PubMed]
- 31.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283:2579–2584. [DOI] [PubMed] [Google Scholar]
- 32.Institute of Medicine. Guidance for the National Healthcare Disparities Report. Washington, DC: National Academy Press; 2002. [PubMed]
- 33.Centers for Disease Control and Prevention. Reported vaccine-preventable diseases—United States, 1993, and the Childhood Immunization Initiative. MMWR Morb Mortal Wkly Rep. 1994;43:57–60. [PubMed] [Google Scholar]