Abstract
Objectives. We estimated overweight and obesity in New York City elementary school children.
Methods. A multistage cluster sample of New York City public elementary school children was selected. Nurses measured children’s height and weight and used a standard protocol to determine body mass index (BMI). Demographic information was obtained from official school rosters. Overweight and obese were defined as BMI-for-age at or above the 85th and 95th percentiles, respectively.
Results. Of 3069 sampled students, 2681 (87%) were measured. The prevalence of overweight was 43% (95% confidence interval [CI] = 39%, 47%), more than half of whom were obese. Overall prevalence of obesity was 24% (95% CI = 21%, 27%), with at least 20% obesity in each grade, including kindergarten. Hispanic children had significantly higher levels (31%; 95% CI = 29%, 34%) than Black (23%; 95% CI = 18%, 28%) or White children (16%; 95% CI = 12%, 20%). Asian children had the lowest level of obesity among all racial/ethnic groups (14.4%, 95% CI = 10.9, 18.7).
Conclusions. Obesity among public elementary school children in New York City is an important public health issue. Particularly high levels among Hispanic and Black children mirror national trends and are insufficiently understood.
Childhood obesity is a rapidly worsening epidemic in the United States. Findings from the most recent National Health and Nutrition Examination Survey (NHANES) indicate that in 1999–2000, the prevalence of obesity among children aged 6 through 11 years was 15%.1 This was a dramatic increase from earlier NHANES surveys, which documented prevalence at 5% in 1960 and 11% in 1988–1994. Increases were particularly marked in Mexican American and Black children. In both groups, prevalence increased more than 10 percentage points between 1988–1994 and 1999–2000, compared with an increase of less than 5 percentage points in White children.1 Findings from the National Longitudinal Survey of Youth on children aged 4 through 12 years found similar trends and disparities in obesity prevalence.2
Obesity during childhood has important short-term medical consequences, including adverse effects on growth, blood pressure, blood lipids, and glucose metabolism.3,4 Other complications include respiratory conditions, such as asthma and obstructive sleep apnea.5,6 The long-term medical consequences of childhood obesity are also substantial and include a greater risk of hypertension, diabetes, cardiovascular disease, gall bladder disease, and osteoarthritis in adulthood.5,7 Childhood obesity also has been shown to have important short- and long-term psychosocial consequences, such as negative self-image, decreased self-esteem, eating disorders, and lower health-related quality of life.8,9 For obese children, the probability that obesity persists into adulthood increases with a child’s age, from 20% among obese 4-year-olds to 80% among obese teenagers.10 This suggests that a brief yet critical window of opportunity for prevention and intervention exists during childhood if poor health consequences are to be reduced.
National surveys provide important information on prevalence and trends for the country, but more tailored information is often needed for smaller regions to allow targeted local evaluation and intervention. New York City is a large, multiethnic metropolitan area, with more than 550 000 public elementary school children. Routine surveillance on the prevalence of childhood obesity and overweight has not been conducted; thus, the magnitude of the problem can be determined only through special studies.
In May 2003, the New York City Department of Health and Mental Hygiene (DOHMH) and Department of Education conducted a height and weight survey in New York City public elementary schools, including children from all grades from kindergarten through fifth grade. The objective was to estimate the prevalence of obesity by gender, grade, and race/ethnicity, as well as to ascertain whether a substantial change in prevalence had occurred since the last such survey, conducted in 1996.11 Findings from that survey identified that 20% of elementary school children surveyed in New York City (third- and sixth-grade students) were obese. Results of the 2003 survey are the subject of this article.
METHODS
Study Sample
This height-and-weight survey was conducted with a stratified, multistage, probability sample of elementary public school children in New York City. A total of 736 elementary schools were listed and enumerated (all New York City public schools, excluding special education schools), and 70 schools were randomly selected by means of Microsoft Excel–generated random numbers.
From the sampled schools, classes were then selected for inclusion into the study. The process for classroom selection was designed to minimize the burden on schools and to ensure adequate representation across all 6 grades. For each of the 70 schools, 2 grades were selected, by means of systematic assignment of the following groupings: kindergarten and third grade, first and fourth grade, and second and fifth grade. These groupings were applied sequentially to the list of sampled schools. For each school, a list of all classes in the 2 grades was generated, and 1 class in each grade was randomly selected with the same random selection techniques described earlier. A total of 140 classes, 2 from each school, was selected. For each of the selected classrooms in the sample, demographic information on all officially enrolled students was obtained before data collection, including gender, date of birth, and race/ethnicity. Demographic information on students not found on official rosters but currently enrolled in that class was obtained from the classroom teachers.
Data Collection
Public health nurses employed by DOHMH were used to collect measurement data. The same model of Healthometer scale (Model 402KL, Sunbeam Products Inc.) was used in each school. New scales were provided to all schools with existing scales that were purchased before the 2000–2001 school year, or to schools with scales in poor condition. All nurses attended a 2-hour training session on data collection procedures 1 week before initiating the survey; the session addressed measurement protocols and scale calibration. Nurses were trained to calibrate, or tare, according to manufacturer’s instructions. Measurement protocols required that each child be measured to the nearest quarter inch for height and quarter pound for weight, without wearing shoes or heavy clothing.
Nurses measured the height and weight of all children in each of the sampled classrooms. Schools without a DOHMH nurse presence were given the choice of conducting the measurement themselves or having a nurse come into the school to conduct the measurement. Children were measured in a private space to ensure confidentiality. Data collection was conducted during the week of May 12–16, 2003.
Principals in each sampled school distributed consent forms to parents of children in the selected classrooms 1 week before data collection. Parental consent forms used a passive consent mechanism, allowing parents to opt their child out of the study by submitting a signed refusal form. These were available in 9 languages. Each school received $500 of exercise equipment for participating in the study. The protocol for this study was approved by institutional review boards at DOHMH and the Department of Education.
Statistical Analyses
BMI-for-age was calculated by means of a child’s weight, height, age, and gender information, as determined by growth chart formulas (2000 revision) provided by the Centers for Disease Control and Prevention and available at http://www.cdc.gov/growthcharts. BMI-for-age is an anthropometric index of relative weight recommended by both national and international expert committees.12 For this study, the distribution of BMI percentile scores was analyzed to determine prevalence levels for ≥ 85th percentile (defined as overweight) and ≥95th percentile (defined as obese). Underweight was defined as at or below the 5th BMI percentile.
Data were analyzed with SAS, Version 8 (SAS Institute Inc, Cary, NC), and SUDAAN, Version 8 (Research Triangle Institute, Research Triangle Park, NC) was used to generate variance estimates. Selection weights accounted for unequal probabilities of selection and nonresponse (including absenteeism and parental refusal). Poststratification weights were used to adjust the sample estimates according to race, gender, and grade. Use of official school rosters minimized missing demographic data. However, for weighting purposes only, missing race data were imputed on the basis of demographics of the school, and missing gender data were updated for children with names easily assigned to 1 gender. A final weight was generated that incorporated both the selection and poststratification weighting for analysis.
Standard errors were estimated with SUDAAN to account for the complex survey design. Weighted descriptive frequencies, 95% confidence intervals, and population estimates for select subgroups were generated. Multiple logistic regression (PROC RLOGIT) was used to assess independent demographic predictors of obesity.
RESULTS
Sixty-nine schools were included in the final sample; 1 school refused to participate. The 69 sampled schools were distributed across most (27 of 32) of New York City’s school districts. In each of the 69 schools, 2 classes participated in the study (138 classrooms). Average class enrollment was 23 students (range 6 to 32). Of the 3069 students enrolled in the selected classrooms, 233 (7.6%) children were absent during data collection, 146 (4.8%) parents refused to allow their child to participate in the study, and 9 (< 1%) students were present in the classroom but no measurements were taken. Thus, the total sample on which height and weight measurements were takentotaled 2681 (87%) students. Nine of the 10 selected schools with no DOHMH nurse on site opted to have a trained DOHMH nurse complete the measurements.
The prevalence of overweight and obesity in New York City elementary school children was calculated by gender, grade, and race/ethnicity (Table 1 ▶). Overall, 43% of public elementary school children in New York City were overweight, with a BMI-for-age at or above the 85th percentile, according to the Centers for Disease Control and Prevention age growth charts. One in 4 (24%) elementary school children were obese, and an additional 19% of children were overweight but not obese (between the 85th and 95th percentiles); 4% of children measured as under a normal weight. A high prevalence of obesity was observed in all, even younger, grades. Twenty-four percent of the kindergarten and first-grade students were obese. A slightly higher prevalence of obesity was found in boys (26%) compared with girls (22%), although this difference was not statistically significant.
TABLE 1–
Prevalence of Overweight and Obesity Among New York City Public Elementary School Children: May 2003
| Overweight (≥ 85th percentile BMI) | Obese (≥ 95th percentile BMI) | |||
| Demographic Characteristic | Percent (95% CI) | Estimated No. of Childrena | Percent (95% CI) | Estimated No. of Childrena |
| Total | 43.2 (39.3, 47.3) | 168 300 | 23.8 (21.3, 26.6) | 92 700 |
| Gender | ||||
| Male | 45.3 (40.4, 50.4) | 87 900 | 25.7 (21.8, 30.1) | 49 900 |
| Female | 41.2 (36.8, 45.8) | 80 400 | 22.0 (19.3, 24.6) | 42 900 |
| Race/ethnicity | ||||
| Hispanic | 52.0 (47.9, 56.1) | 78 100 | 31.1 (28.7, 33.6) | 46 700 |
| Black | 39.5 (34.5, 44.7) | 41 300 | 22.8 (18.3, 27.9) | 23 800 |
| White | 37.9 (31.5, 44.8) | 26 400 | 15.9 (12.3, 20.3) | 11 100 |
| Asian | 30.2 (24.6, 36.4) | 17 100 | 14.4 (10.9, 18.7) | 8 100 |
| Grade | ||||
| Kindergarten | 48.3 (34.5, 62.3) | 27 700 | 23.3 (13.7, 36.7) | 13 400 |
| First grade | 37.0 (30.9, 43.5) | 24 900 | 25.0 (21.0, 29.4) | 16 800 |
| Second grade | 45.1 (36.6, 54.0) | 30 000 | 25.1 (19.9, 31.2) | 16 500 |
| Third grade | 40.9 (33.8, 48.4) | 31 400 | 22.9 (18.9, 27.4) | 17 600 |
| Fourth grade | 42.8 (32.9, 53.2) | 29 600 | 22.0 (15.3, 30.6) | 15 200 |
| Fifth grade | 47.4 (41.1, 53.9) | 25 200 | 25.0 (20.9, 29.5) | 13 300 |
Note. CI = confidence interval; BMI = body mass index.
aAll population estimates are rounded to the nearest 100.
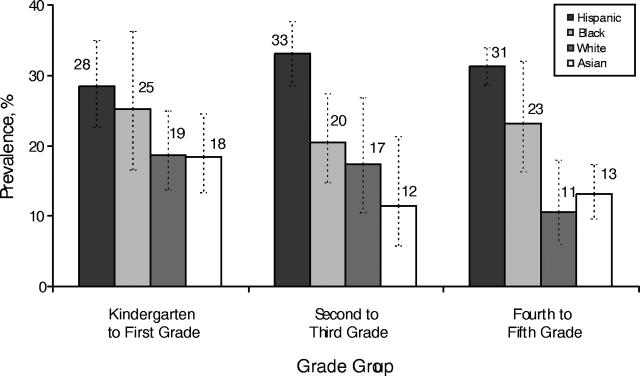
Thirty-one percent of Hispanic children, 23% of Black children, 16% of White children, and 14% of Asian children were obese. When race-specific obesity rates were examined by grade, Hispanic children had the highest obesity for each grade group (Figure 1 ▶). Almost 29% of Hispanic kindergarten and first-grade students were obese (31% among fourth- and fifth-grade students). For White children, obesity decreased in older grade groups. Nineteen percent of White kindergarten and first-grade students were obese, compared with only 11% of White fourth- and fifth-grade students.
FIGURE 1—
Prevalence (with confidence interval bars) of obesity among New York City public elementary school children by grade and race/ethnicity, 2003.
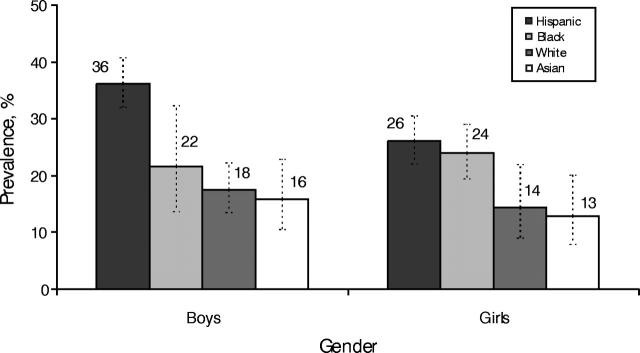
Race- and gender-specific rates indicated that Hispanic boys had the highest prevalence among school children in New York City (Figure 2 ▶). Thirty-six percent of Hispanic boys were obese, compared with 22% of Black boys, 18% of White boys, and 16% of Asian boys. Among girls, Hispanics and Blacks had higher rates of obesity (26% and 24%, respectively) than Whites (14%). Among Hispanic children, boys had significantly higher levels of obesity than girls (36% vs 26%).
FIGURE 2—
Prevalence (with confidence interval bars) of obesity among New York City public elementary school children by gender and race/ethnicity, 2003.
In models simultaneously adjusting for grade, gender, and race, Hispanic and Black children both had significantly higher levels of obesity compared with White children, independent of grade and gender (Hispanic: odds ratio [OR] = 2.1; 95% confidence interval [CI] = 1.5, 2.9; Black: OR = 1.4; 95% CI = 1.1, 1.9). When gender-specific models were examined, Hispanic ethnicity was the only significant predictor among boys (OR = 2.3; 95% CI = 1.5, 3.5), whereas among girls levels of obesity were similarly elevated among both Hispanic (OR = 1.9; 95% CI = 1.2, 3.3) and Black (OR = 1.7; 95% CI = 1.1, 2.9) girls compared with White girls.
DISCUSSION
Findings from this survey demonstrate that almost 1 in every 4 children in New York City public elementary schools is obese. This corresponds to nearly 100 000 New York City elementary school students with serious weight conditions that place them at high risk for medical and psychosocial consequences. Childhood obesity is a growing national concern, and this survey confirms that it has become a major public health challenge in New York City.
In addition to the obese students, another 19% of elementary school children are overweight. In total, nearly half (43%) of elementary school children measured above the 85th percentile of BMI. This is a much larger proportion than the “expected” value of 15% and suggests that a true population shift in weight distribution has occurred. Intervention programs must therefore aim to target all students, with the broad goal of shifting that BMI curve back toward a healthier distribution.
An important finding in our analysis was the high rate of overweight among Hispanic children, particularly Hispanic boys. Comparing the results of this survey to 2 previous height-and-weight surveys in New York City elementary schools,11,13 we found that a larger increase in the prevalence of overweight has occurred among Hispanic children than in children of other racial/ethnic groups. Between 1996 and 2003, overweight prevalence among Hispanic third-grade students escalated significantly, from 21% to 31%, whereas the increase in other groups was less than 5 percentage points and not statistically significant. These findings suggest the need for additional focused intervention efforts in Hispanic communities, which include 40% of children in New York City public elementary schools.
Reasons for the disparate increase across racial/ethnic groups are not well understood.14 Differences in socioeconomic status, maternal BMI, dietary patterns, and adaptive biological mechanisms have been postulated as partial explanations.15–17 Among Hispanic groups, research on overweight has shown both generational and geographic-origin differences.15 Biologically, racial differences in insulin action have been documented.16 Culturally, differences in attitudes toward weight have been found between racial groups.17 Despite limitations in understanding the causes behind overweight disparities, most particularly in New York City’s Hispanic children, it is essential to raise awareness in affected communities about the serious health risks associated with overweight for children, and the importance of developing a sustainable healthy diet and physical activity patterns early in life.
Concomitant with the rapid rise in childhood obesity, increasing sedentary behavior and poor nutrition among children has been documented,18 particularly among children of lower socioeconomic status. Studies have shown that poorer children are less likely to eat fruits and vegetables and more likely to have a higher intake of total and saturated fats.19,20 Efforts to treat childhood obesity have largely focused on attempts to improve nutritional intake and reduce sedentary behavior at the individual behavior level,21 but opportunities to develop these practices must also be encouraged and made accessible through neighborhood-level interventions. This is supported by a previous survey in New York State elementary schools that found that low socioeconomic status was a predictor of heavier weight.22
Although limited in number, school-based interventions to address childhood obesity and overweight have been modestly successful. Programs designed to improve nutrition, increase physical activity, and reduce television viewing have been shown to decrease overweight, improve dietary intake, and reduce sedentary behaviors in some children.18,23–25 The need for a concerted emphasis on nutrition and physical activity in both school and community settings is of critical importance to control overweight in New York City elementary school children.
Treatment guidelines for addressing pediatric obesity in clinical settings recommend a careful assessment of child and family readiness to participate in a weight-management program.26 Depending on a child’s age and BMI percentile and the presence of medical complications, either weight maintenance or weight loss to achieve weight are recommended. Guidelines emphasize that all treatment efforts should involve the entire family and strive toward permanent behavioral change in diet and physical activity habits.
This study has several limitations. First, this study was limited to children enrolled in public elementary schools in New York City, and private schools (in which approximately 20% of elementary school students in New York City are enrolled) were not part of the sampling frame. This not only limits the generalizability of our findings but also limits comparability to previous height and weight surveys in New York City, both of which included private schools.11,13 Unfortunately, we cannot compare the results of our findings to previous New York City public school subsamples (or understand the difference in prevalence between school types) because prior results were not published stratified by type of school. In 1989–1990, the New York State Department of Health examined second- and fifth-grade students in public and private schools in New York City (n = 1400). The Department identified that 20% of second-grade students and 18% of fifth-grade students were obese, numbers that were substantially higher than national figures at that time.13 Seven years later, in 1996, the same researchers selected the third and sixth grades for another survey (n = 637). Findings from this survey were consistent with the first; 20% of third-grade students and 21% of sixth-grade students in New York City were obese, suggesting little change.11 Both surveys used a multistage probability design to select students from both New York City public and private schools. Although the 2003 survey described in this article is not representative of private elementary school children, the larger sample size and higher response rate (87% vs less than 60%) ensures estimate precision and minimal selection bias in our public school findings.
A second limitation refers to the accuracy level of data collected. Although data collection followed a standard protocol, digital scales were not used. Variability in data ascertainment may have introduced error into the prevalence estimates; however, we do not anticipate large or systematic differences.
Third, no additional information regarding students’ nutritional or physical activity patterns was collected; thus, our findings were limited to describing the burden only.
In a large city such as New York, there are multiple agencies and organizations focusing on the health of children, yet better efforts are needed to coordinate physical activity and recreation opportunities, health services, health education, mental health services, community development, and nutrition and food services. Although evidence of successful intervention to reduce childhood overweight is sparse, improving nutrition and increasing physical activity are clearly key components to preventing overweight. In September 2003, a new program of nutrition standards for meals served in New York City schools was launched, including stringent recommendations for fat, calorie, and nutrient content.27 The new school standards apply to food sold in vending machines as well as cafeteria meals. The need for improved physical activity and health education in schools also is being examined. The availability of local surveillance data on overweight can stimulate collaboration and program accountability between agencies, as well as raise public awareness about the magnitude and seriousness of the epidemic.
Acknowledgments
All funding for this survey was provided by the New York City Department of Health and Mental Hygiene.
The authors are greatly indebted to the supervisory school nurses who assisted in the data collection, as well as the school leadership of all schools participating in the survey, including principals, district superintendents, and classroom teachers. Most importantly, we would like to thank the children who were selected and participated in the survey. We extend a special thanks to Anjum Hajat for her statistical expertise with the sample weighting. We also thank Drs Mary Bassett and Kelly Henning for their insightful comments on early drafts of this article.
Human Participant Protection The New York City Departments of Education and Health and Mental Hygiene institutional review boards approved the project as an exemption.
Contributors L. E. Thorpe and S. D. Helgerson conceptualized the survey, and L. E. Thorpe together with D. List, L. May, and T. Marx prepared and supervised the survey data collection. L. E. Thorpe analyzed the data, and D. List and L. E. Thorpe wrote the first draft of the article. T. R. Frieden, S. D. Helgerson, and L. E. Thorpe revised and edited the final draft.
Peer Reviewed
References
- 1.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288:1728–1732. [DOI] [PubMed] [Google Scholar]
- 2.Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. JAMA. 2001;286:2845–2848. [DOI] [PubMed] [Google Scholar]
- 3.Gidding SS, Bao W, Srinivasan SR, Berenson GS. Effects of secular trends in obesity on coronary risk factors in children: the Bogalusa Heart Study. J Pediatr. 1995;127:868–874. [DOI] [PubMed] [Google Scholar]
- 4.Shinha R, Fisch G, Teague B, et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med. 2002;346:802–810. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Consensus statement: type 2 diabetes in children and adolescents. Diabetes Care. 2000;23:381–390. [DOI] [PubMed] [Google Scholar]
- 6.Gennuso J, Epstein LH, Paluc, RA, Cerny F. The relationship between asthma and overweight in urban minority children and adolescents. Arch Pediatr Adolesc Med. 1998;152:1197–1200. [DOI] [PubMed] [Google Scholar]
- 7.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–873. [DOI] [PubMed] [Google Scholar]
- 8.Strauss RS. Childhood obesity and self-esteem. Pediatrics. 2000;105(1):e15. [DOI] [PubMed] [Google Scholar]
- 9.Davison KK, Birch LL. Weight status, parent reaction, and self-concept in five-year-old girls. Pediatrics. 2001;107(1):46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dietz WH. Health consequences of overweight in youth: childhood predictors of adult disease. Pediatrics. 1998;101(3):518–525. [PubMed] [Google Scholar]
- 11.Centers for Disease Control. Prevalence of overweight among third- and sixth-grade children, New York City, 1996. MMWR Morb Mortal Wkly Rept. 1998;47:980–984. [PubMed] [Google Scholar]
- 12.American Academy of Pediatrics. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424–430. [DOI] [PubMed] [Google Scholar]
- 13.Melnick TA, Rhoades SJ, Wales KR, Cowell C, Wolfe WS. Overweight school children in New York City: prevalence estimates and characteristics. Int J Obes. 1998;22;7–13. [DOI] [PubMed] [Google Scholar]
- 14.Flores G, Fuentes-Afflick E, Barbot O, et al. The health of Latino children: urgent priorities, unanswered questions, and a research agenda. JAMA. 2002;288;82–90. [DOI] [PubMed] [Google Scholar]
- 15.Crawford PB, Story M, Wang MC, Ritchie LD, Sabry ZJ. Ethnic issues in the epidemiology of childhood obesity. Pediatr Clin North Am. 2001;48:855–878. [DOI] [PubMed] [Google Scholar]
- 16.Goran MI, Ball GDC, Cruz ML. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J Clin Endocrinol Metab. 2003;88:1417–1427. [DOI] [PubMed] [Google Scholar]
- 17.Davis SP, Northington L, Kolar K. Cultural considerations for treatment of childhood obesity. J Cult Divers. 2000;7:128–132. [PubMed] [Google Scholar]
- 18.Physical Activity and Health: A Report of the Surgeon General. Atlanta, Ga: Centers for Disease Control and Prevention, National Center for Chronic Disease and Prevention and Health Promotion; 1996.
- 19.Krebs-Smith SM, Cook A, Subar AF, Cleveland L, Friday J, Kahle LL. Fruit and vegetable intakes of children and adolescents in the United States. Arch Pediatr Adolesc Med. 1996;150:81–86. [DOI] [PubMed] [Google Scholar]
- 20.Berkey CS, Rockett HR, Field AE, et al. Activity, dietary intake, and eight changes in a longitudinal study of preadolescent and adolescent boys and girls. Pediatrics. 2000;105(4):e56. [DOI] [PubMed] [Google Scholar]
- 21.Robinson TN. Behavioral treatment of childhood and adolescent obesity. Int J Obes. 1999;23:S52–S57. [DOI] [PubMed] [Google Scholar]
- 22.Wolfe WS, Campbell CC, Frongillo Jr EA, Haas JD, Melnik TA. Overweight schoolchildren in New York State: prevalence and characteristics. Am J Public Health. 1994;84:807–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth. Arch Pediatr Adolesc Med. 1999;153;409–418. [DOI] [PubMed] [Google Scholar]
- 24.Gortmaker SL, Cheung LW, Peterson KE, et al. Impact of school-based interdisciplinary intervention on diet and physical activity among urban primary school children. Arch Pediatr Adolesc Med. 1999;153:975–983. [DOI] [PubMed] [Google Scholar]
- 25.Robinson TN. Reducing children’s television viewing to prevent obesity. JAMA. 1999;282;1561–1567. [DOI] [PubMed] [Google Scholar]
- 26.Barlow SE, Dietz WH. Obesity evaluation and treatment: expert committee recommendations. Pediatrics. 1998;102:E29. [DOI] [PubMed] [Google Scholar]
- 27.Platt R. NYC Department of Health and Mental Hygiene on Prohibiting Sale of Minimally Nutritious Foods and Beverages at Public Schools. Testimony Before New York City Council Committees on Health and on Education: 24June2003. Available at: http://www.nyc.gov/html/doh/html/public/testi/testi20030624.html. Accessed June 24, 2004.