Abstract
Objectives. We examined the association between diet quality and estimated diet costs.
Methods. Freely chosen diets of 837 French adults were assessed by a dietary history method. Mean national food prices for 57 foods were used to estimate diet costs.
Results. Diets high in fat, sugar, and grains were associated with lower diet costs after adjustment for energy intakes, gender, and age. For most levels of energy intake, each additional 100 g of fats and sweets was associated with a €0.05–0.40 per day reduction in diet costs. In contrast, each additional 100 g of fruit and vegetables was associated with a €0.18–0.29 per day increase in diet costs.
Conclusions. Diets high in fats and sweets represent a low-cost option to the consumer, whereas the recommended “prudent” diets cost more.
There is solid evidence that high fruit and vegetable consumption plays a major role in lowering risk of heart disease and stroke and in lowering total mortality.1–6 A “prudent” dietary pattern characterized by high intake of vegetables, fruits, whole grains, poultry, and fish has been associated with a lower risk of coronary heart disease1,2 and with better health status overall.
In contrast, consumption of sugar-sweetened beverages, corn syrup, potatoes, and refined grains has been linked to a higher risk of heart disease and type 2 diabetes.1,7,8 “Western” dietary patterns, characterized by high consumption of processed meats, fried foods, sweets, and desserts, fail to protect against disease risk.7,8 Excess consumption of energy-dense snacks,9,10 fast foods,11,12 and soft drinks13–15 has been linked to higher rates of overweight. A World Health Organization report on diet, nutrition, and prevention of chronic diseases pointed out causal links between fats and sweets consumption and the worldwide obesity epidemic.16 Public policy proposals for prevention of obesity increasingly mention taxes and levies on energy-dense, sweet, and high-fat foods.17
Replacement of fats and sweets with vegetables and fruit has become a standard public health recommendation.18,19 Studies on diet and health have focused on the glycemic index of foods,7 on fat content,20,21 and on the energy density of the diet.22,23 Absent from the mainstream literature, however, has been any consideration of diet costs.24–26 Whereas fats and sweets provide dietary energy at a very low cost, the energy cost of lean meats, fish, vegetables, and fruit is likely to be higher. Following advice to replace one with the other, far from being a simple public health application,7 will most likely entail higher consumer diet costs. In this study, we estimated the cost of freely chosen total diets in a community setting in France and examined relationships among diet quality, dietary energy density, and estimated diet costs.
METHODS
The Val-de-Marne dietary survey, conducted in 1988–1989, was based on a 2-stage cluster-design sampling procedure. Of 849 families contacted, 527 took part in the study (62% response rate). The analyses reported in this article were based on dietary intake data for 837 adults (361 men and 476 women). Mean age was 42.5 years for men and 42.8 years for women. Details of the study have been published previously.27
Analyses of dietary trends in France indicate that the major dietary changes occurred between 1950 and 1985.28 As fewer changes have occurred since, the Val-de-Marne data are regarded as representative of the current eating habits in France.
Food Costs and Diet Costs
Dietary intakes (in grams/day) were obtained by means of a dietary history interview, administered by a trained dietitian. Nutrient analyses of dietary intakes were based on the Val-de-Marne nutrient database.27 Cost analyses were based on the edible portion of 57 foods in the database, which were aggregated into 5 major food groups: grains, fruit and vegetables, meats, dairy products, and fats and sweets. For the purpose of cost analysis, alcoholic beverages, tea, coffee, drinking water, and foods consumed by less than 5% of the sample population were excluded. Energy density of foods (MJ/kg) was obtained from food composition tables. Energy density of the diet was calculated by dividing total dietary energy by the weight of foods and caloric beverages only.29
The cost of each of the 57 foods or food categories was based on a single food item, regarded as representative of that category. Cumulative consumption data by weight from a French national food consumption survey allowed us to select the most frequently consumed items. The cost selections tended toward the lower-priced options and an effort was made to include both frozen and canned goods as well as the more expensive fresh meat, fish, and fresh produce. For example, vegetables were represented by potatoes, carrots (fresh), peas, lentils, and mixed vegetables (all canned), and endives (fresh). The cost of meat was based on ground hamburger (frozen), beef filet (fresh) and chicken breasts. The meat group also included liver, organ meats, ham, eggs, canned fish, fresh fish, and shellfish. Prices for dairy products were based on whole milk, low-fat milk, skim milk, pudding, fromage blanc (0%, 20%, and 40% fat), fruit yogurt, plain yogurt, and Emmenthal and Camembert cheeses. The fats and sweets group included fats and oils, sugar, candy, chocolate, and soft drinks. Current national retail prices in euro (€1.00 = approximately US $1.20) per kilogram for each food were provided by the French National Institute of Statistics. Diet costs were estimated by multiplying the amount of each food consumed (g/day) by its unit cost and summing to achieve a total diet cost for all foods and beverages consumed.30
Statistical Analyses
Multivariate regression analyses served to test the relationship between diet composition and diet cost. The standard multivariate method used energy intakes (megajoules per day [MJ/day]) and nutrient intakes (grams per day [g/day]) as terms in a multiple regression model, with diet cost (€/day) as the dependent variable and adjustment for age and gender.31 Participants were stratified by quintiles of food or nutrient intake (in g/day or as percentage energy [% energy]), and the relationship between dietary variables and diet cost was tested with 1-way analyses of variance. Participants also were stratified by quintiles of energy intake (MJ/day) to examine the relationship between diet composition and diet cost at each level of intake in a regression model. Analyses were performed with SPSS version 10.1 (SPSS Inc; Chicago, Ill).
RESULTS
Energy Costs
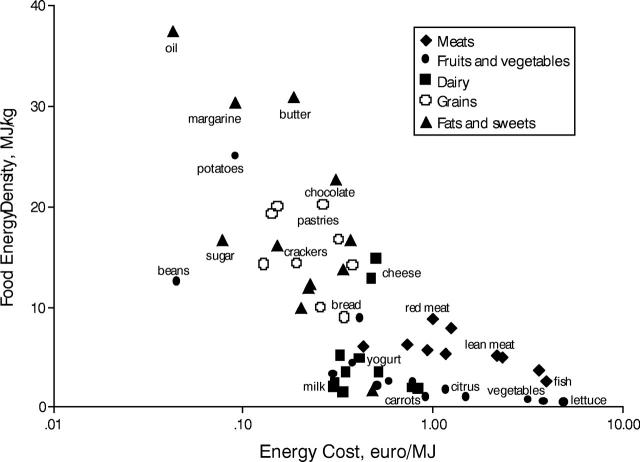
Energy costs (€/MJ) for each food are shown in Figure 1 ▶. Energy costs for oil, margarine, potatoes, sugar, or beans were substantially less than energy costs for lean meat, vegetables, lettuce, or fish. As indicated by the logarithmic scale, disparities in energy cost between fats and fresh produce were in excess of 1000%.
FIGURE 1—
Relationship between food energy density (MJ/kg) and energy costs (€/MJ), as plotted on a log scale.
Note. MJ = megajoules.
Estimated Diet Costs
Mean energy intakes, without alcohol, were 9.89 MJ (2366 kilocalories [kcal]) for men and 7.38 MJ (1765 kcal) for women. Mean estimated diet cost was €5.59 per day for men and €4.62 per day for women. Women consumed more fruit and vegetables, fiber, and vitamin C per 10 MJ of dietary energy than did men. Mean energy cost per 10 MJ was higher for women (€6.56/10 MJ) than for men (€5.85/10 MJ).
Table 1 ▶ shows that higher consumption of grains and of fats and sweets was associated with lower diet costs after adjustment for energy intake, gender, and age. Higher intakes of sucrose and total fat were likewise associated with lower diet costs. In contrast, the consumption of fruit and vegetables was associated with higher diet costs, as was the consumption of meat. Higher consumption of dairy products was not associated with higher or lower diet costs.
TABLE 1—
Regression Coefficients From Multivariate Linear Models, Adjusted for Age, Gender, and Energy Intake
| Food Category | β (95% CI) |
| Grains | −0.15 (−0.21, −0.08)* |
| Vegetables and fruit | 0.19 (0.16, 0.21)* |
| Meat | 0.77 (0.70, 0.83)* |
| Dairy products | −0.02 (−0.05, 0.01) |
| Fats and sweets | −0.11 (−0.18, −0.05)* |
| Total fat | −0.46 (−0.80, −0.12)* |
| Sucrose | −0.93 (−1.15, −0.71)* |
Note. β = regression coefficient; CI = confidence interval. Dependent variable is diet cost (eurocents/day); independent variable is food category and amount consumed (g/day).
*P < .001.
The relationship between diet quality and diet costs is summarized in Table 2 ▶. Participants were divided into quintiles according to their consumption of fats and sweets (g/day), fruits and vegetables (g/day), fat and sucrose (as % energy). The dependent variables, shown as a function of consumption of different-type foods and nutrients, were total energy intakes (MJ/day), dietary energy density (MJ/kg), daily diet costs (€/day), and energy costs (€/10MJ).
TABLE 2—
Energy Intakes, Dietary Energy Density, and Diet and Energy Costs, by Quintiles of Intake of Selected Food Groups (g/Day) and Nutrients (% Energy)
| Quintiles of Intake | ||||||
| Food Category | 1 | 2 | 3 | 4 | 5 | P |
| Fats and sweets (g/day) | 25.6 ±9.7 | 47.2 ±4.9 | 66.3 ±5.7 | 89.5 ±8.8 | 227.0 ±169.5 | |
| Energy intake (MJ) | 6.0 ±0.1 | 7.3 ±0.1 | 8.1 ±0.1 | 9.4 ±0.2 | 11.6 ±0.3 | <.001 |
| Energy density (MJ/kg) | 4.6 ±0.08 | 5.6 ±0.1 | 5.7 ±0.1 | 6.0 ±0.1 | 6.4 ±0.1 | <.001 |
| Diet cost (€/day) | 4.37 ±0.09 | 4.61 ±0.09 | 5.05 ±0.08 | 5.26 ±0.08 | 5.90 ±0.12 | <.001 |
| Energy cost (€/10 MJ) | 7.59 ±0.15 | 6.45 ±0.10 | 6.31 ±0.08 | 5.66 ±0.07 | 5.22 ±0.07 | <.001 |
| Fruit and vegetables (g/day) | 343 ±6 | 494 ±2 | 584 ±2 | 703 ±3 | 977 ±19 | |
| Energy intake (MJ) | 8.1 ±0.2 | 8.1 ±0.2 | 8.1 ±0.2 | 8.7 ±0.2 | 9.4 ±0.2 | <.001 |
| Energy density (MJ/kg) | 6.5 ±0.11 | 6.0 ±0.09 | 5.6 ±0.1 | 5.3 ±0.08 | 5.0 ±0.1 | <.001 |
| Diet cost (€/day) | 4.30 ±0.10 | 4.66 ±0.08 | 4.91 ±0.09 | 5.36 ±0.10 | 5.95 ±0.10 | <.001 |
| Energy cost (€/10 MJ) | 5.55 ±0.09 | 6.01 ±0.10 | 6.48 ±0.12 | 6.49 ±0.11 | 6.72 ±0.14 | <.001 |
| Total fat (% energy) | 29.2 ±0.2 | 35.1 ±0.1 | 39.6 ±0.1 | 42.0 ±0.1 | 48.8 ±0.4 | |
| Energy intake (MJ) | 7.6 ±0.2 | 8.5 ±0.2 | 8.7 ±0.2 | 8.9 ±0.2 | 8.7 ±0.3 | <.001 |
| Energy density (MJ/kg) | 4.9 ±0.1 | 5.5 ±0.1 | 5.7 ±0.1 | 6.0 ±0.1 | 6.3 ±0.1 | <.001 |
| Diet cost (€/day) | 4.76 ±0.11 | 5.04 ±0.10 | 5.08 ±0.10 | 5.28 ±0.09 | 5.01 ±0.11 | <.05 |
| Energy cost (€/10 MJ) | 6.69 ±0.15 | 6.21 ±0.11 | 6.14 ±0.10 | 6.13 ±0.09 | 6.09 ±0.10 | <.001 |
| Sucrose (% energy) | 1.5 ±1.0 | 4.4 ±0.6 | 6.4 ±0.6 | 8.9 ±0.8 | 14.3 ±3.8 | |
| Energy intake (MJ) | 7.2 ±2.4 | 8.2 ±2.9 | 8.4 ±2.3 | 8.7 ±3.1 | 9.7 ±3.6 | <.001 |
| Energy density (MJ/kg) | 5.2 ±1.3 | 5.6 ±1.2 | 5.8 ±1.1 | 5.7 ±1.3 | 6.0 ±1.3 | <.001 |
| Diet cost (€/day) | 4.92 ±1.18 | 5.09 ±1.46 | 5.09 ±1.23 | 4.94 ±1.29 | 5.13 ±1.52 | NS |
| Energy cost (€/10 MJ) | 7.21 ±1.83 | 6.46 ±1.51 | 6.18 ±1.08 | 5.93 ±1.22 | 5.46 ±1.14 | <.001 |
Note. NS = not significant.
Persons in the highest quintile of fats and sweets consumption (g/day) consumed more energy and had higher diet costs (€5.90/day) than did persons in the lowest quintile (€4.37/day). However, this higher diet cost was more than offset by a doubling of energy intake. As a result, energy costs were only €5.22 per 10 MJ for persons in the highest quintile, as opposed to €7.59 per 10 MJ for persons in the lowest quintile of fats and sweets consumption.
Energy costs per 10 MJ were €5.46 for persons in the highest quintile of sucrose intakes and €7.21 for persons in the lowest quintile. Persons in the highest quintile of fat intakes had higher energy intakes and higher dietary energy density, a pattern that is consistent with previous reports.32,33 Higher fat consumption was associated with lower energy costs per 10 MJ (€6.09/10 MJ vs €6.69/10 MJ).
Persons in the highest quintile of fruit and vegetable consumption (g/day) had higher diet costs (€5.95/day) than did persons in the lowest quintile (€4.30/day). Energy costs were €6.62 per 10 MJ for persons in the highest quintile and €5.56 per 10 MJ for persons in the lowest quintile of fruit and vegetable consumption. Whereas fat and sugar were associated with lower energy costs, vegetables and fruit were associated with higher energy costs.
Do “Prudent” Diets Cost More?
To determine whether the relationship between diet structure and diet costs held for all levels of energy intake, participants were stratified by energy intake quintiles (MJ/day).
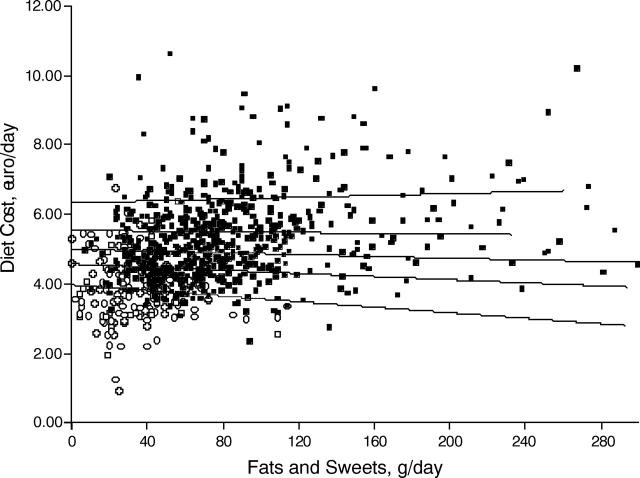
Figure 2 ▶ shows the relationship between the fats and sweets consumption (g/day) and diet costs, with regression lines at each quintile of energy intake indicated by solid lines. For persons in the lowest energy quintile, each additional 100 g of fats and sweets was associated with a reduction in absolute diet cost of €0.40 per day. The relationship flattened as energy intakes increased so that, for persons in the highest energy quintile, each 100 g of fats and sweets was associated with an increase in diet costs of €0.05 per day.
FIGURE 2—
Relationship between fats and sweets consumption (g/day) and diet costs (€/day).
Note. Regression lines are for each quintile of energy intake. Open circles denote lowest quintile.
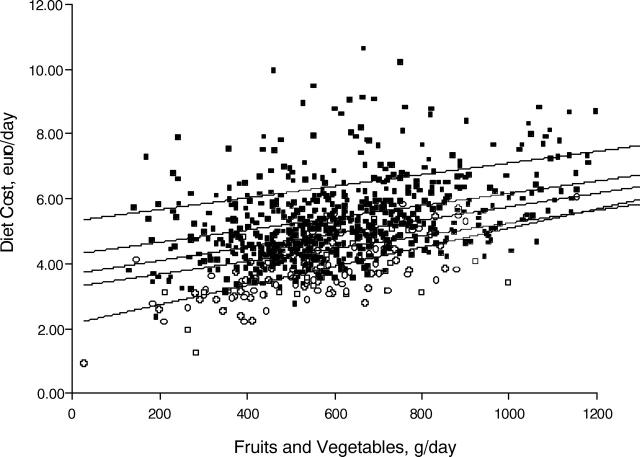
In contrast, higher fruit and vegetable consumption was associated with higher diet costs. Figure 3 ▶ shows that each 100 g/day increment in fruit and vegetable consumption was associated with an increase in diet costs of €0.18–€0.29 per day, depending on energy intake.
FIGURE 3—
Relationship between fruit and vegetable consumption (g/day) and diet costs (€/day).
Note. Regression lines are for each quintile of energy intake. Open circles denote lowest quintile.
DISCUSSION
This cost analysis of freely chosen total diets in a French community sample showed that fats and sweets offer dietary energy at very low cost. At most levels of energy intake, higher consumption of fats and sweets was associated not only with reduced energy costs (€/10 MJ) but also with lower absolute diet costs (€/day). Depending on the level of energy intake, each 100 g of fats and sweets was associated with a net reduction of €0.05–€0.40 in daily diet costs. In contrast, each additional 100 g of vegetables and fruit was associated with a net increase of €0.18–€0.29 per day in diet costs.
The finding that elevated consumption of fats and sweets is associated with lower diet costs is also likely to hold for US diets. The mean retail price of sucrose in the United States is much lower than that in France, and total sugar consumption (including corn sweeteners) is twice as high.34 However, few studies on diet quality and estimated diet costs comparable to ours have been conducted in the United States. This lack of data is a major research gap, given that structural and policy proposals for the prevention of obesity increasingly point to the need for fiscal and policy interventions.11,16 At this time, there are no nationally representative US data on diet costs on which to base fiscal and food policies.
The model we used to estimate diet costs had some important limitations. Diet costs were estimated with mean national food prices, as opposed to actual food expenditures, and studies foods were limited to 57 foods. The model critically depends on the ability of the selected foods to represent each food category; an unrepresentative set of foods would greatly degrade the accuracy of the imputed diet costs. However, our overall estimate of approximately €5 per day was remarkably close to the national mean expenditures for food consumed at home (€14.9/day), as calculated by the French National Institute of Statistics. Our study was based on adults older than 18 years, and children and adolescents were not included. Another limitation was the lack of detailed socioeconomic data on occupation and income.
Nonetheless, the study may provide insight into the effect of price structure on food choices. Sugar and fat consumption by the American public has become a major focus of obesity research.7,20 Metabolic studies have explored the neurobiology of food preference and the nature of cravings for fats and sweets.35 Environmental studies have examined the contributions of snacks,9 fast foods,11 caloric beverages,13,14 eating away from home,12 and growing portion sizes36 to the obesity epidemic. Links were established between excessive weight gain and the energy density of the diet.16,23 Very few studies have considered the economics of food choice24 and the very low energy cost of sugar and fat.35 Low-income consumers may select fats and sweets simply because they are palatable and because they provide dietary energy at the lowest possible cost. Given the current hierarchy of food prices, seeking to minimize diet costs may drive consumer food choices toward refined grains, potatoes, sugar, and fat.37
The US Department of Agriculture dietary guidelines and the Food Guide Pyramid continue to stress the importance of vegetables and fruit.18,19 Public health approaches to obesity prevention have called for the imposition of small taxes and levies on sweet and high-fat foods.16,17 However, very few cost analyses of diet structure exist on which to base dietary guidelines, public health interventions, or fiscal food policy.37,38 It is debatable whether altering the absolute price of some foods without modifying the price hierarchy will have a desired effect on food choices. The relationships among fat and sugar consumption, food costs, and obesity has never been explored.
Epidemiological studies have shown that “prudent” diets based on vegetables, fruit, whole grains, poultry, and fish are more protective than so-called Western diets, characterized by high consumption of added sugars and fat.1 In other words, more costly diets are associated with more favorable health outcomes.2–6 Persons making more costly food choices may well have additional financial resources and social capital, both of which may influence health status.39,40 Higher fruit and vegetable consumption and better health outcomes are generally associated with higher education and higher income levels.41,42 Food costs represent a barrier to dietary change, especially for low-income families,42,43 and our data indicate that the recommended “prudent” dietary patterns are likely to cost more. Public health strategies and approaches to dietary change for health promotion would do well to take diet costs into account.
Acknowledgments
This study was supported by Institut National pour la Science et la Recherche Medicale Unit 557; the Institut National de la Recherche Agronomique, Institut Scientifique et Technique de la Nutrition et de l’Alimentation/Conservatoire National des Arts et Métiers; and a National Institutes of Health Fogarty Senior International Fellowship grant to A. Drewnowski.
Human Participant Protection The Val-de-Marne study was approved by the ethics committee of the Conservatoire National des Arts et Métiers–Paris. Analyses of data sets stripped of all identifying information were declared exempt from review by the University of Washington institutional review board.
Contributors A. Drewnowski contributed to the planning of the study, performed data analyses, and wrote the article. N. Darmon planned and conceptualized the study, performed data analyses, and contributed to the writing of the article. A. Briend contributed to the conception and design of the study, to the analysis and interpretation of data, and to critical revisions of the article.
Peer Reviewed
References
- 1.Hu FB, Rimm EB, Stampfer MJ, Ascherio A, Spiegelman D, Willett WC. Prospective study of major dietary patterns and risk of coronary heart disease in men. Am J Clin Nutr. 2000;72:912–921. [DOI] [PubMed] [Google Scholar]
- 2.Joshipura KJ, Hu FB, Manson JE, et al. The effect of fruit and vegetable intake on risk for coronary heart disease. Ann Intern Med. 2001;134:1106–1114. [DOI] [PubMed] [Google Scholar]
- 3.Bazzano LA, He J, Ogden LG, et al. Fruit and vegetable intake and risk of cardiovascular disease in US adult: the first National Health and Nutrition Examination Survey epidemiologic follow-up study. Am J Clin Nutr. 2002;76:93–99. [DOI] [PubMed] [Google Scholar]
- 4.Fung TT, Wilett WC, Stampfer MJ, Nason JE, Hu FB. Dietary patterns and the risk of coronary heart disease in women. Arch Intern Med. 2001;161:1857–1862. [DOI] [PubMed] [Google Scholar]
- 5.Gillman MW, Cupples LA, Gagnon D, et al. Protective effect of fruits and vegetables on development of stroke in men. JAMA. 1995;273:1113–1117. [DOI] [PubMed] [Google Scholar]
- 6.Joshipura KJ, Ascherio A, Manson JE, et al. Fruit and vegetable intake in relation to risk of ischemic stroke. JAMA. 1999;282:1233–1239. [DOI] [PubMed] [Google Scholar]
- 7.Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes and cardiovascular disease. JAMA. 2002;287:2414–2423. [DOI] [PubMed] [Google Scholar]
- 8.Liu S. Intake of refined carbohydrates and whole grain foods in relation to risk of type 2 diabetes mellitus and coronary heart disease. J Am Coll Nutr. 2002;21:298–306. [DOI] [PubMed] [Google Scholar]
- 9.Kant AK. Consumption of energy-dense, nutrient-poor foods by adult Americans: nutritional and health implications. The third National Health and Nutrition Examination Survey, 1988–1994. Am J Clin Nutr. 2000;72:929–936. [DOI] [PubMed] [Google Scholar]
- 10.Zizza C, Siega-Riz AM, Popkin BM. Significant increase in young adults’ snacking between 1977–1978 and 1994–1996 represents a cause for concern! Prev Med. 2001;32:303–310. [DOI] [PubMed] [Google Scholar]
- 11.French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health. 2001;22:309–335. [DOI] [PubMed] [Google Scholar]
- 12.Lin B-H, Guthrie J, Frazão E. Nutrient contribution of food away from home. In: Frazão E, ed. America’s Eating Habits: Changes and Consequences. Washington, DC: US Dept of Agriculture; 1999:71–95.
- 13.Harnack L, Stang J, Story M. Soft drink consumption among US children and adolescents: nutritional consequences. J Am Diet Assoc. 1999;99:436–441. [DOI] [PubMed] [Google Scholar]
- 14.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357:505–508. [DOI] [PubMed] [Google Scholar]
- 15.Cavadini C, Siga-Riz AM, Popkin BM. US adolescent food intake trends from 1965 to 1996. Arch Dis Child. 2000;83:18–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO Technical Report Series 916. Diet, nutrition, and the prevention of chronic diseases. Report of a joint WHO/FAO expert consultation, WHO, Geneva 2003. [PubMed]
- 17.Jacobson MF, Brownell KD. Small taxes on soft drinks and snack foods to promote health. Am J Public Health. 2000;90:854–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Center for Nutrition Policy and Promotion, US Dept of Agriculture. The Food Guide Pyramid. Home and Garden Bulletin no. 252. Washington DC: US Dept of Agriculture; 1996.
- 19.Center for Nutrition Policy and Promotion, US Dept of Agriculture. Dietary Guidelines for Americans, 5th ed. Washington DC: US Dept of Agriculture; 2000.
- 20.Bray GA, Popkin BM. Dietary fat intake does affect obesity! Am J Clin Nutr. 1998;68:1157–1173. [DOI] [PubMed] [Google Scholar]
- 21.Willett WC. Dietary fat plays a major role in obesity: no. Obes Rev. 2002;3:59–68. [DOI] [PubMed] [Google Scholar]
- 22.Drewnowski A. Energy density, palatability and satiety: implications for weight control. Nutr Rev. 1998;56:347–353. [DOI] [PubMed] [Google Scholar]
- 23.Prentice AM, Poppit SD. Importance of energy density and macronutrients in the regulation of energy intake. Int J Obes. 1996;20(suppl):S18–S23. [PubMed] [Google Scholar]
- 24.Cade J, Booth S. What can people eat to meet the dietary goals and how much does it cost? J Hum Nutr Diet. 1990;3:199–207. [Google Scholar]
- 25.Cade J, Upmeier H, Calvert C, Greenwood D. Costs of a healthy diet: analysis from the UK Women’s Cohort Study. Public Health Nutr. 1999;2:505–512. [DOI] [PubMed] [Google Scholar]
- 26.Mooney C. Costs and availability of healthy food choices in a London health district. J Hum Nutr Diet. 1990;3:111–120. [Google Scholar]
- 27.Drewnowski A, Rock CL, Henderson SA, et al. Serum beta-carotene and vitamin C as biomarkers of vegetable and fruit intakes in a community-based sample of French adults. Am J Clin Nutr. 1997;65:1796–1802. [DOI] [PubMed] [Google Scholar]
- 28.Haut Comité de la Santé Publique. Pour une politique nutritionnelle de santé publique en France [Toward a public health nutrition policy in France]. Available at: http://www.sante.gouv.fr/htm/actu/nutri2000/saisine.htm. Accessed April 19, 2004.
- 29.Cox DN, Mela DJ. Determination of energy density of freely selected diets: methodological issues and implications. Int J Obe. 2000;24:49–54. [DOI] [PubMed] [Google Scholar]
- 30.Bowman SA. A methodology to price foods consumed: development of a food price database. Family Econ Nutr Rev. 1997;10:26–33. [Google Scholar]
- 31.Willett WC. Nutritional Epidemiology. 2nd ed. New York, NY: Oxford University Press; 1998.
- 32.Grunwald GK, Seagle HM, Peters JC, Hill JO. Quantifying and separating the effects of macronutrient composition and non-macronutrients on energy density. Br J Nutr. 2001;86:265–276. [DOI] [PubMed] [Google Scholar]
- 33.Marti-Henneberg C, Capdevila F, Arija V, et al. Energy density of the diet, food volume and energy intake by age and sex in a healthy population. Eur J Clin Nutr. 1999;53:421–428. [DOI] [PubMed] [Google Scholar]
- 34.Drewnowski A. Fat and sugar: an economic analysis. J Nutr. 2003;133:838S–840S. [DOI] [PubMed] [Google Scholar]
- 35.Levine AS, Kotz Catherine M, Gosnell BA. Sugars and fats: the neurobiology of preference. J Nutr. 2003:133:831S–834S. [DOI] [PubMed] [Google Scholar]
- 36.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977–1998. JAMA. 2003;289:450–453. [DOI] [PubMed] [Google Scholar]
- 37.Darmon N, Ferguson EL, Briend A. The adverse effects of a cost constraint on food selection and nutrient density: an analysis of human diets by linear programming. J Nutr. 2002;132:3764–3771. [DOI] [PubMed] [Google Scholar]
- 38.Marshall T. Exploring a fiscal food policy: the case of diet and ischaemic heart disease. BMJ. 2000;320:301–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.James WP, Nelson M, Ralph A, Leather S. Socioeconomic determinants of health. The contribution of nutrition to inequalities in health. BMJ. 1997;314:1545–1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lennernas M, Fjellstrom C, Becker W, et al. Influences on food choice perceived to be important by nationally representative samples of adults in the European Union. Eur J Clin Nutr. 1997;51(suppl 2):S8–S15. [PubMed] [Google Scholar]
- 41.Lutz SM, Blaylock JR, Smallwood DM. Household characteristics affect food choices. Food Rev. 1993;16:12–18. [Google Scholar]
- 42.Michaud C, Baudier F, Londou A, LeBihan G, Janvrin MP, Rotily M. Food habits, consumption and knowledge of a low-income French population. Santé Publique. 1998;10:333–347. [PubMed] [Google Scholar]
- 43.Papadaki A, Scott JA. The impact on eating habits of temporary translocation from a Mediterranean to a Northern European environment. Eur J Clin Nutr. 2002;56:455–461. [DOI] [PubMed] [Google Scholar]