Abstract
Objectives. We examined lengths of hospital stay among individuals categorized according to weight status.
Methods. We used data from the First National Health and Nutrition Examination Survey Epidemiologic Followup Survey to estimate length-of-stay differences.
Results. Individuals with body mass indexes (BMIs) of 35 kg/m2 or above, those with BMIs of 30 to 34 kg/m2, and those with BMIs of 25 to 29 kg/m2 had crude length-of-stay rates greater than those of normal-weight individuals. Association between BMI and length of stay varied over time.
Conclusions. Obese individuals experience longer hospital stays than normal-weight individuals.
Although prevalence rates of obesity have reached epidemic proportions in the United States, the relationship between obesity and health care use has received very little attention.1,2 An even smaller body of literature has focused on use of hospital care among obese individuals. Obesity has been strongly associated with a range of health problems; however, studies that have examined the association between obesity and hospitalization have failed to provide consistent results. Some of these studies have revealed elevated risks of hospitalization associated with obesity,3,4 others have shown no association5–7 or even a decreased risk,8,9 and still others have shown a gender-specific10 or age-specific8 relationship. In most of these studies, data on weight and hospital use were collected concurrently, and in some, information regarding weight was actually collected after information regarding hospitalizations.3–5,7–10
In addressing factors that are part of the causal pathway between obesity and hospitalization, prospective studies have included assessments of data on health conditions.6,8 Statistical control of such health conditions (e.g., type II diabetes) constitutes overadjustment11; studies including health conditions in their analyses have shown no effect of obesity, leading to the erroneous inference that obesity is not an important risk factor for hospitalization.6,8
Our objective in this study was to estimate, by means of a longitudinal analysis, lengths of hospital stay among individuals categorized according to their weight status. Our data were derived from the First National Health and Nutrition Examination Survey (NHANES I) Epidemiologic Followup Survey (NHEFS).
METHODS
Survey Description
The baseline for the NHEFS was NHANES I, conducted between 1971 and 1975.12 In NHANES I, data were collected from a national probability sample of the United States civilian noninstitutionalized population, and the survey included a standardized medical examination and questionnaires covering various health-related topics. The NHEFS cohort consisted of 14 407 individuals who were aged 25 years or older at their baseline interview. A series of 4 follow-up surveys was conducted during 1982 through 1984 and in 1986, 1987, and 1992.
Body Mass Index Measurement
Respondents’ weight status was classified according to National Heart, Lung and Blood Institute (NHLBI) criteria. Body mass indexes (BMIs; weight in kilograms divided by height in meters squared) were calculated at baseline and categorized as follows: less than 18.5 kg/m2, 18.5 to 24.9 kg/m2, 25.0 to 29.9 kg/m2, 30.0 to 34.9 kg/m2, and 35 kg/m2 or above (as described in the NHLBI guidelines).13 Respondents with a BMI of 18.5 to 24.9 kg/m2 were the reference group in the analysis. Women who were pregnant at baseline were excluded (n = 124).
Hospitalizations
Number of inpatient hospitalization days was the outcome measure of interest. Respondents reported hospital admissions that occurred between their baseline and final interviews. Reports of hospital stays were elicited through a series of questions in the NHEFS interviews. Respondents were asked to report the dates of all overnight facility stays since their most recent interview. With respondents’ permission, all reported facilities were contacted by mail and asked to abstract information from respondents’ medical records. We included all hospitalizations for which there were abstracted data, representing 77% of all stays reported in the NHEFS.
Previous studies have evaluated the use of abstract-matched stays versus all stays in analyses of hospitalization risk and concluded that the bias from use of only the former is minimal.6,14,15 We used only abstracted data for our analysis because information regarding inpatient days was available only from these data. After hospitalizations related to pregnancy and birth (n = 809) had been excluded, 29 471 hospitalizations, representing a total of 263 961 inpatient days, were available for analysis.
Statistical Analysis
Longitudinal models, specifically generalized estimating equations,16,17 were used to explore the association between BMI and length of stay. This technique was used to account for the within-subject correlation among a respondent’s repeated observations. Because our outcome of interest, inpatient days, was a count, we assumed a Poisson distribution for the number of inpatient days. We used the exchangeable correlation structure for our working correlation matrix. We obtained rate ratios and 95% confidence intervals by comparing the healthy BMI category (18.5 to 24.9 kg/m2) for the period 1971 through 1975 and all other BMI categories for all other periods.
Follow-up periods were divided into 4 intervals: 1971 to 1975, 1976 to 1980, 1981 to 1985, and 1986 to 1992. Person-years were calculated for each participant at each interval, and inpatient days were aggregated for each participant within each of the 4 intervals.
On the basis of the conceptual model developed by Andersen and others, which categorizes factors affecting health care utilization, we included age, gender, race, marital status, whether respondents had children, smoking status, socioeconomic status (i.e., poverty status), region of residence, and urban-rural residence in our models.18–20 With the exception of smoking status and whether respondents had children, we used baseline values for these covariates. Because data on smoking status and presence of children were not collected at baseline, they were derived from the portion of the survey conducted during 1982 through 1984.
Interactions between BMI categories and time intervals were assessed to examine baseline differences among respondents. Also, through the use of interaction terms (in models not imputing income data), we investigated whether the association between overweight or obesity and length of stay varied according to race, smoking status, or region of residence. To evaluate models fitted with interaction terms, we computed Wald tests and used a significance level of P < .1.
We analyzed the NHEFS as a cohort study, and we present results from analyses that did not incorporate weights or sample design corrections. (As have other authors, we found that analyses incorporating weights and survey design corrections and analyses not incorporating these features produced similar results.21)
Missing Covariates
Several authors have recommended the use of multiple imputation to deal with missing covariates; here we used this method to replace missing data on socioeconomic status (poverty status) for 24% of the sample.22–26 Previous research indicates that income is an important determinant of health care use,18–20,27 and socioeconomic status has been linked to obesity.28 In addition, income and health insurance status have been closely linked, and the NHEFS did not provide complete information on insurance coverage.29
Participants with missing data on a variety of variables other than income were dropped from the analyses (19%). After exclusion of those who did not complete follow-up interviews and those with incomplete data (other than income), the final analytic sample included 11 556 respondents. SAS Version 8.2 (SAS Institute Inc, Cary, NC) was used in conducting all analyses. PROC GENMOD was used to calculate generalized estimating equations, and PROC MI and PROC MIANALYZE were used to carry out multiple imputation.
RESULTS
Table 1 ▶ shows baseline characteristics of the analytic sample according to BMI category. In comparison with other groups, higher percentages of Black, female, inactive, and single individuals were categorized in the 35 kg/m2 or above BMI group. Lower percentages of high school graduates and higher percentages of never smokers were classified in the 30 to 34.9 kg/m2 and 35 kg/m2 and above BMI groups.
TABLE 1—
Percentage Distribution of Baseline Characteristics According to Body Mass Index Category: First National Health and Nutrition Examination Survey Epidemiologic Follow-up Survey (N = 11 556), 1971–1992
| Body Mass Index (kg/m2) | |||||
| Characteristic | < 18.5 (n = 376) | 18.5 to < 25.0 (n = 5430) | 25.0 to < 30.0 (n = 3809) | 30.0 to < 35 (n = 1368) | ≥ 35 (n = 573) |
| Aged ≥ 65 y | 20 | 23 | 30 | 30 | 24 |
| Black | 16 | 10 | 13 | 20 | 26 |
| Female | 75 | 65 | 48 | 65 | 81 |
| Married | 70 | 77 | 79 | 74 | 67 |
| Has childrena | 83 | 85 | 86 | 86 | 82 |
| Completed high school or beyond | 54 | 62 | 53 | 43 | 43 |
| Smoking statusa | |||||
| Current | 56 | 40 | 34 | 26 | 26 |
| Former | 9 | 14 | 20 | 15 | 15 |
| Never | 36 | 46 | 47 | 60 | 59 |
| Urban residence | 63 | 63 | 62 | 58 | 60 |
| Region | |||||
| Northeast | 18 | 22 | 23 | 21 | 22 |
| Midwest | 24 | 25 | 26 | 26 | 28 |
| South | 34 | 27 | 25 | 29 | 28 |
| West | 24 | 27 | 26 | 23 | 22 |
| Physical activity levelb | |||||
| Very active | 51 | 52 | 47 | 43 | 31 |
| Moderately active | 40 | 42 | 45 | 48 | 51 |
| Quite inactive | 10 | 6 | 8 | 10 | 18 |
Note. Percentages may not sum to 100% owing to rounding.
aInformation on presence of children and smoking status was obtained from the 1982–1984 survey.
bPhysical activity level was based on 2 questions asked at baseline about recreational activity and usual activity. Subjects were classified as quite inactive if they reported being the least active for both questions, very active if they reported being very active for either response, and moderately active for all other combinations.
We also compared respondents reinterviewed at a subsequent wave with respondents lost to follow-up. White respondents accounted for 86% of those reinterviewed and 75% of those lost to follow-up; married respondents accounted for 76% of those reinterviewed and 61% of those lost to follow-up; respondents at an educational level of high school or above accounted for 55% of those reinterviewed and 44% of those lost to follow-up; and rural residents accounted for 37% of those reinterviewed and 18% of those lost to follow-up. In the case of other baseline variables—BMI, age, sex, and region—percentage distributions of those reinterviewed and those lost to follow-up were comparable (differences of 5% or less).
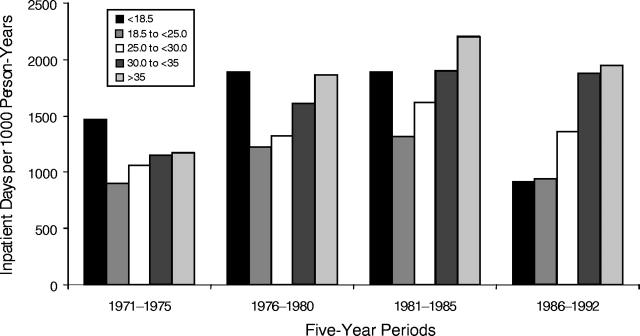
Crude rates of inpatient hospital days for each BMI category are presented in Figure 1 ▶. Participants with normal BMIs exhibited the lowest rates in terms of length of stay during 1971 through 1975. In each subsequent period, lengths of stay increased as respondents’ adiposity increased. Underweight respondents initially exhibited higher rates but leveled off and actually declined between 1986 and 1992.
FIGURE 1—
Lengths of stay (per 1000 person-years) among individuals classified by body mass index category according to National Heart, Lung and Blood Institute criteria: 1971–1992.
Rate ratios for inpatient hospital days are presented in Table 2 ▶. Interaction terms between BMI categories and race, smoking status, and region were not significant, indicating that the effect of BMI did not vary according to these characteristics. However, interactions between BMI categories and time period were significant, and thus we present rate ratios for each period.
TABLE 2—
Length of Stay Rate Ratios and 95% Confidence Intervals: First National Health and Nutrition Examination Survey Epidemiologic Follow-up Survey, 1971–1992
| Rate Ratio (95% Confidence Interval) | ||||
| Body Mass Index (kg/m2) | 1971–1975 | 1976–1980 | 1981–1985 | 1986–1992 |
| < 18.5 | 1.94 (1.22, 3.09) | 2.21 (1.47, 3.33) | 2.17 (1.34, 3.52) | 1.01 (0.61, 1.68) |
| 18.5 to < 25.0 | 1.00 | 1.47 (1.06, 2.02) | 1.61 (1.23, 2.12) | 1.09 (0.82, 1.45) |
| 25.0 to < 30.0 | 1.25 (0.93, 1.67) | 1.60 (1.20, 2.12) | 1.89 (1.42, 2.51) | 1.36 (1.03, 1.79) |
| 30.0 to < 35 | 1.45 (1.06, 1.98) | 1.94 (1.45, 2.61) | 2.11 (1.59, 2.81) | 1.60 (1.19, 2.16) |
| ≥ 35 | 1.54 (1.02, 2.31) | 2.18 (1.62, 2.91) | 2.80 (2.07, 3.78) | 2.31 (1.68, 3.18) |
Note. Results shown are from a generalized estimating equation model with a Poisson distribution. The model includes Body Mass Index × Time interaction terms. Values were adjusted for age, gender, race, marital status, presence of children, education, height, smoking status, region, urban–rural residence, socioeconomic status (i.e., poverty status), and physical activity level.
In the 1971 to 1975 period and thereafter, respondents with BMIs of 30 to 34.9 kg/m2 and those with BMIs of 35 kg/m2 or above exhibited lengths of stay greater than those observed among normal-weight respondents between 1971 and 1975. In comparison with 1971 to 1975, lengths of stay showed increases among normal-weight respondents during 1976 to 1980 and 1981 to 1985 but decreases between 1986 and 1992. Overweight respondents exhibited rates similar to those observed among normal-weight respondents during 1971 to 1975 but exhibited greater rates thereafter.
With the exception of the final follow-up period (1986–1992), underweight respondents exhibited longer lengths of stay than did normal-weight respondents in the 1971 to 1975 interval. During this final period, respondents with BMIs of 30 to 34.9 kg/m2, those with BMIs of 35 kg/m2 or above, and those who were overweight continued to exhibit increased lengths of stay (131%, 60%, and 36% higher rates, respectively) than did normal-weight respondents in the baseline period.
DISCUSSION
To our knowledge, this is the first longitudinal study to demonstrate a time trend in associations between weight status and length of stay. We found increases in length of stay among obese individuals throughout the study period and increases among those at BMI levels below 18.5 kg/m2 for 3 of the 4 follow-ups. These results suggest a U- or J-shaped relationship between BMI and length of stay because the extreme values of BMI, underweight and obesity, exhibited greater lengths of stays while normal-weight exhibited the shortest length of stay. Previous studies have shown that such a relationship exists between BMI and mortality30–32 and between BMI and probability of health care expenditures.33 It is likely that illness-induced weight loss contributed to the elevated risk observed here among individuals with BMIs below 18.5 kg/m2.
An advantage of the long follow-up associated with the NHEFS is that we were able to incorporate time trends. A secular trend in length of stay has been previously noted.34,35 In the present case, the secular trend in length of stay was pronounced among underweight individuals; however, the decline in inpatient days during the 1986 to 1992 period appears not to have been an artifact of sample size: there were approximately 200 hospitalizations among almost 300 underweight respondents during this period.
The analytic approaches used in this study support establishing weight status as a causal factor in the association examined here. Most of the previous research examining the association between weight status and lengths of hospital stay has been based on cross-sectional designs; however, cross-sectional studies cannot provide evidence regarding the temporal sequence of an association. In the present longitudinal investigation, we measured individuals’ hospital use patterns subsequent to measurement of their weight.
We did not control for health conditions in our analyses. As mentioned earlier, because conditions such as type II diabetes are part of the causal pathway between obesity and hospitalization, it is inappropriate to statistically control for these diseases in estimating associations between BMI and health service use. However, on the basis of the model developed by Andersen, we included a large number of covariates that need to be considered in explorations of the effect of weight status on health service use.19,20,27 For example, we included smoking status, often cited as a confounding factor in associations between underweight status and outcomes such as mortality.36 We found an association between underweight and hospitalization in models that included smoking status.
Using the NHLBI criteria, we demonstrated that as respondents’ adiposity levels (measured via BMI groupings) increased from the normal range, so did their number of inpatient hospital days. This dose–response relationship further supports weight status as a causal factor in the relationship studied here.11 Another important aspect of the present weight status values is that they were based on precisely measured weight and height data. Researchers have noted that self-reported BMIs exhibit a characteristic pattern of error.37
We were able to examine effects of obesity on hospitalization only among Blacks and Whites. Further research is needed to determine whether relationships exist among other racial/ethnic groups. Another drawback involved with our cohort was loss to follow-up, and, because we did not have detailed information on reasons for dropout, we were unable to determine whether any biases existed in our results. A further limitation of the present study is that we examined weight at only 1 point in time.
In addition, because appropriate data were not available, we did not examine fat distribution, which is an important predictor of morbidity and mortality38 and thus also may play a role in the BMI–hospitalization relationship. Although we did not control for health insurance coverage (since the NHEFS does not include complete health insurance or Medicaid information), we did include income level, which has been closely linked to health insurance status.29
Finally, our estimates were based on obesity prevalence rate data from the early 1970s, and rates have increased considerably since that period in every US state; in both genders; and across all age groups, races, educational levels, and categories of tobacco use.39–41 These increases in obesity have the potential to severely tax the health care system, particularly given our results indicating that obese individuals have longer hospital stays. In all likelihood, treatment and prevention of obesity will reduce use of hospital care and the subsequent health care costs associated with the obesity epidemic.
Acknowledgments
This study was supported in part by the National Institute of Child Health and Human Development (grant HD39183), the University of North Carolina, and a National Research Service Award (grant T32 HS00032) Postdoctoral Traineeship from the Agency for Healthcare Research and Quality.
Rob Stephenson and Tim Carey provided editorial comments on earlier versions of this article. John Preisser provided statistical advice. We thank Frances Dancy for support in administrative matters and Tom Swasey for assistance in producing the figure.
Human Participation Protection This study was approved by the institutional review board of the University of North Carolina School of Medicine. The study involved a secondary data analysis, and the data were collected by a US federal agency.
Contributors C. Zizza conceived the study, completed the analysis, and led the writing. A. H. Herring assisted with the analysis and interpretation of the data. J. Stevens, B. M. Popkin, and A. H. Herring helped to conceptualize ideas and review drafts of the article.
Peer Reviewed
References
- 1.Fontaine K, Barlett S. Access and use of medical care among obese persons. Obes Res. 2000;8:403–406. [DOI] [PubMed] [Google Scholar]
- 2.Wolf A. What is the economic case for treating obesity? Obes Res. 1998;1(suppl 6):2–7. [DOI] [PubMed] [Google Scholar]
- 3.Heithoff K, Cuffel B, Kennedy S, Peters J. The association between body mass and health care expenditures. Clin Ther. 1997;19:811–820. [DOI] [PubMed] [Google Scholar]
- 4.Quesenberry C, Cann B, Jacobson A. Obesity, health services use, and health care costs among members of a health maintenance organization. Arch Intern Med. 1998;158:466–472. [DOI] [PubMed] [Google Scholar]
- 5.Hauner H, Koster I, von Ferber L. Frequency of obesity in medical records and utilization of out-patient health care by obese subjects in Germany: an analysis of health insurance data. Int J Obes Relat Metab Disord. 1996;20:820–824. [PubMed] [Google Scholar]
- 6.Miller J, Russell L, Davis D, Milan E, Carson J, Taylor W. Biomedical risk factors for hospital admission in older adults. Med Care. 1998;36:411–421. [DOI] [PubMed] [Google Scholar]
- 7.Stirling S, Wadsworth M. The changing pattern of in-patient care. J Public Health Med. 1995;17:51–56. [PubMed] [Google Scholar]
- 8.Ferraro K, Booth T. Age, body mass index, and functional illness. J Gerontol B Psychol Sci Soc Sci. 1999;54B:S339–S348. [DOI] [PubMed] [Google Scholar]
- 9.Trakas K, Lawrence K, Shear N. Utilization of health care resources by obese Canadians. Can Med Assoc J. 1999;160:1457–1462. [PMC free article] [PubMed] [Google Scholar]
- 10.Seidell J, Deerenberg I. Obesity in Europe: prevalence and consequences for use of medical care. PharmacoEconomics. 1994;5(suppl 1):38–44. [DOI] [PubMed] [Google Scholar]
- 11.Rothman K, Greenland S. Modern Epidemiology. 2nd ed. Philadelphia, Pa: Lippincott-Raven; 1998.
- 12.Plan and Operation of the Health and Nutrition Examination Survey, United States, 1971–73. Washington, DC: National Center for Health Statistics; 1979.
- 13.National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res. 1998;2(suppl 6):51–209. [PubMed] [Google Scholar]
- 14.Sichieri R, Everhart J, Roth H. A prospective study of hospitalization with gallstone disease among women: roles of dietary factors, fasting period, and dieting. Am J Public Health. 1991;81:880–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.LaCroix A, Lipson S, Milers T, White L. Prospective study of pneumonia hospitalizations and mortality of US older people: the role of chronic conditions, health behavior, and nutritional status. Public Health Rep. 1989;104:350–360. [PMC free article] [PubMed] [Google Scholar]
- 16.Zeger S, Liang K. An overview of methods for the analysis of longitudinal data. Stat Med. 1992;11:1825–1839. [DOI] [PubMed] [Google Scholar]
- 17.Liang K, Zeger S. Regression analysis for correlated data. Annu Rev Public Health. 1993;14:43–68. [DOI] [PubMed] [Google Scholar]
- 18.Andersen R, Newman J. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 1973;51:95–124. [PubMed] [Google Scholar]
- 19.Aday L, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208–220. [PMC free article] [PubMed] [Google Scholar]
- 20.Andersen R. Revisiting the behavioral model and access to medical care. J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 21.Ingram DD, Makuc DM. Statistical issues in analyzing the NHANES I Epidemiological Followup Study. Vital Health Stat 2. 1994;No. 121. [PubMed]
- 22.Horton N, Lipsitz S. Multiple imputation in practice: comparison of software packages for regression models with missing variables. Am Statistician. 2001;55:244–254. [Google Scholar]
- 23.Rubin D. Multiple Imputation for Nonresponse in Surveys. New York, NY: John Wiley & Sons Inc; 1987.
- 24.Greenland S, Finkle W. A critical look at methods for handling missing covariates in epidemiologic regression analyses. Am J Epidemiol. 1995;142:1255–1264. [DOI] [PubMed] [Google Scholar]
- 25.Faris P, Ghali W, Brant R, Norris C, Galbraith P, Knudtson M. Multiple imputation versus data enhancement for dealing with missing data in observational health care outcome analyses. J Clin Epidemiol. 2002;55:184–191. [DOI] [PubMed] [Google Scholar]
- 26.Brownstone D, Valletta R. The bootstrain and multiple imputations: harnessing increased computing power for improved statistical tests. J Econ Perspect. 2001;15:129–141. [Google Scholar]
- 27.Phillips K, Morrison K, Andersen R, Aday L. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998;33:571–596. [PMC free article] [PubMed] [Google Scholar]
- 28.Sobal J. Obesity and socioeconomic status: a framework for examining relationships between physical and social variables. Med Anthropol. 1991;13:231–247. [DOI] [PubMed] [Google Scholar]
- 29.Shi L. Vulnerable populations and health insurance. Med Care Res Rev. 2000;57:110–134. [DOI] [PubMed] [Google Scholar]
- 30.Reubin A, Muller D, Sorkin J. National Institutes of Health Technology Assessment Conference: long-term effects of change in body weight on all-cause mortality: a review. Ann Intern Med. 1993;119(suppl 7):737–743. [DOI] [PubMed] [Google Scholar]
- 31.Allison D, Faith M, Heo M, Townsend-Butterworth D, Williamson D. Meta-analysis of the effect of excluding early deaths on the estimated relationship between body mass index and mortality. Obes Res. 1999;7:417–419. [DOI] [PubMed] [Google Scholar]
- 32.Stevens J. Obesity and mortality in African Americans. Nutr Rev. 2000;58:346–353. [DOI] [PubMed] [Google Scholar]
- 33.Black D, Sciacca J, Coster D. Extremes in body mass index: probability of healthcare expenditures. Prev Med. 1994;23:385–393. [DOI] [PubMed] [Google Scholar]
- 34.Phelps C. Health Economics. 2nd ed. New York, NY: Addison-Wesley; 1997.
- 35.Popovic JR, Kozak LJ. National Hospital Discharge Survey: annual summary, 1998. Vital Health Stat 13. 2000;No. 148. [PubMed]
- 36.Manson J, Stampfer M, Hennekens C, Willet W. Body weight and longevity. JAMA. 1987;257:353–358. [PubMed] [Google Scholar]
- 37.Plankey M, Stevens J, Flegal K, Rust P. Prediction equations do not eliminate systematic error in self-reported body mass index. Obes Res. 1997;5:308–314. [DOI] [PubMed] [Google Scholar]
- 38.Stevens J, Plankey M, Williamson D, et al. The body mass index-mortality relationship in White and African American women. Obes Res. 1998;6:268–277. [DOI] [PubMed] [Google Scholar]
- 39.Kuczmarski R, Flegal K, Campbell S, Johnson C. Increasing prevalence of overweight among US adults. JAMA. 1994;272:205–211. [DOI] [PubMed] [Google Scholar]
- 40.Mokdad A, Serdula M, Dietz W, Bowman B, Marks J, Koplan J. The spread of the obesity epidemic in the United States, 1991–1998. JAMA. 1999;282:1519–1522. [DOI] [PubMed] [Google Scholar]
- 41.Flegal KM. The obesity epidemic in children and adults: current evidence and research issues. Med Sci Sports Exerc. 1999;31(suppl 11):509–514. [DOI] [PubMed] [Google Scholar]