Abstract
Objectives. We tested the assumption that average job retention duration is shorter for physicians in rural health professional shortage areas (HPSAs) than for physicians in rural non-HPSAs.
Methods. In 1991, we surveyed nationally representative samples of primary care physicians who recently had moved to rural HPSAs and non-HPSAs who were without service obligations. We resurveyed these physicians in 1996 and 1997 to learn of any job changes.
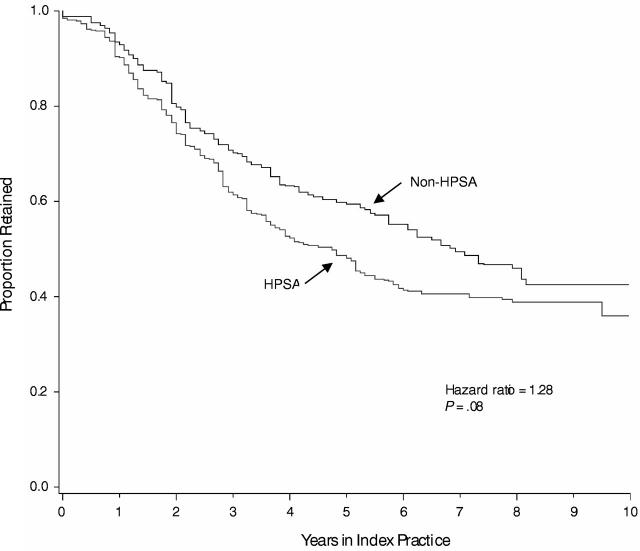
Results. Physicians in rural HPSAs (n=308) demonstrated retention similar to that of the non-HPSA cohort (n=197) (hazard ratio for leaving=1.28; 95% confidence interval=0.97, 1.69; P=.08), even with adjustments for group demographic differences (P=.24).
Conclusions. Average retention duration for generalist physicians in rural HPSAs is identical to or slightly shorter than for those in rural non-HPSAs. Poor recruitment is likely to be the principal dynamic underlying local rural shortages.
In spite of the many public programs developed to recruit and retain physicians in rural areas, physician scarcities continue to threaten health care delivery in many rural communities in the United States.1 The federal Health Professional Shortage Area (HPSA)2 designation identifies 2100 rural areas as underserved. The general understanding about physician shortage areas, and the fundamental rationale for recruitment and retention programs,3–6 is that these communities suffer from both the inability to recruit a sufficient number of physicians and the inability to retain those they have. We question whether this dual assumption is accurate.
Low physician-to-population ratios, the hallmark of underserved areas, reflect only practitioner counts at a given point in time without revealing specifically how often physicians move into and out of these areas. Over time, either inadequate inflow (low recruitment rates) or excessive outflow (low retention rates) alone can yield practitioner shortages.
Understanding whether shortages arise from deficiencies in both recruitment and retention is fundamental to creating informed remedies. We are aware of 2 studies that have assessed recruitment into US underserved areas; both concluded that, indeed, fewer primary care physicians move to HPSAs than to other rural areas.7,8 Similarly, in reports of physicians’ movement into the least populated rural settings—areas that are generally under-served9–11—in-migration was lower than in more populated rural settings.7,12
Studies of retention in underserved areas—the focus of our study—generally have been limited to assessments of physicians working under service obligations to the National Health Service Corps and in special settings such as Indian Health Service sites and community health centers.13–17 Few data characterize how long physicians working without obligations, who constitute the majority of practitioners in rural underserved areas,14 are retained within the full range of practice settings found in shortage areas, including private, public, and nonprofit and large and small practices. Li8 studied turnover for physicians in HPSAs, and Kindig10 assessed turnover in very small counties; both concluded that turnover differed minimally from that in non-HPSAs and more populated rural counties. Perhaps then, retention only appears to be a more frequent problem in underserved areas, possibly because its consequences there are more immediately and painfully evident.
Regardless of whether retention is especially poor in rural underserved areas, little is known about why physicians leave these sites when they do so and how they can be coaxed to stay. When asked, physicians in rural areas report that their retention is affected by local poverty, social and professional isolation, a lack of amenities, and the hardships of rural work—long hours, frequent on-call shifts, and low income.18–22 Because of the especially challenging community and work conditions often found in underserved rural areas, these factors are generally assumed to be particularly salient there.23 However, it is primarily perceptions that link these factors to retention in underserved areas, and perceptions can be inaccurate.24,25
We report data on the retention behavior of primary care physicians working without service obligations in rural HPSAs in all kinds of practice situations. We compared their retention to that of primary care physicians working contemporaneously in non-HPSA rural areas. To identify promising approaches for promoting retention, we assessed how retention in HPSAs varied with the characteristics of physicians, their practices, jobs, and their communities.
METHODS
Sample
We used the American Medical Association’s Physician Masterfile listing of all US physicians to compare sequential end-of-year files from 1986 through 1990 to identify all practicing family physicians, pediatricians, general internists, and general practitioners who appeared at a nonmetropolitan zip code in the continental United States where they had not been the previous year, thus appearing to have moved to a rural address that year.14 Physicians listed in the National Health Service Corps’s files of its obligated physicians were eliminated. We randomly selected 1000 of the 1938 who appeared to have moved to HPSAs and 600 of the 6348 physicians who appeared to have moved to non-HPSA rural areas; the smaller non-HPSA sample was needed for comparison only. Samples were selected after stratifying the HPSA and non-HPSA groups by age, specialty, and US region, specifically the Southeast versus other regions combined.
We sent the 1600 sampled physicians up to 3 survey mailings in 1991. Of these physicians, 87 were never located; 465 did not respond; and 349 responded but were found to be ineligible because they had not moved to a town with a population of less than 50000 during the targeted years, were serving in the National Health Service Corps or military, were not practicing primary care, or had died. The remaining 699 eligible subjects returned completed questionnaires—an estimated 70.9% of those who were both located and met eligibility criteria.26 Response rates were comparable for the HPSA (71.0%) and non-HPSA (70.8%) cohorts but were lower for younger physicians, internists, and physicians in the Southeast.
Respondents provided personal demographic information and identified the first rural practice to which they moved between 1987 and 1990—their “index practice”—specifying its location and their employment dates and describing their practices and work there.
In 1996 and 1997, we used the updated Physician Masterfile to relocate the 699 respondents to the 1991 survey. We resurveyed the physicians by mail, phone, and fax to learn the locations and dates of where they had worked since 1991. Combining responses to the original 1991 and follow-up 1996/1997 surveys enabled us to calculate the exact number of months that 681 of the 699 original respondents (97.4%) remained in their index rural practices.
For these retention analyses, we eliminated 194 of the 699 original respondents based on the locations of their index practices and circumstances of their work. Those excluded were (a) 43 respondents whose practices were determined to be in remote areas of metropolitan counties (1986 Office of Management and Budget metropolitan criteria); (b) 19 respondents whose practices were in towns with a population of more than 35000, larger than generally accepted notions of rural; (c) 130 respondents who reported that they were completing service obligations, typically to states; (d) 30 respondents working in non–primary care positions such as emergency care or full-time teaching; and (e) 44 respondents working fewer than 25 hours in the office each week (categories not mutually exclusive). A relatively uniform cohort of 505 nonobligated practicing rural generalist respondents remained for analysis; 308 worked in HPSAs and 197 worked in non-HPSA communities.
We used the Health Resources and Services Administration’s Area Resource File27 to append 1990 data characterizing the counties where physicians worked. Data on town populations were imported from the 1990 US Census.
Analyses
We used the SUDAAN statistical software package (8.0.0 for PC, Research Triangle Institute, Research Triangle Park, NC), which was designed to analyze survey data from complex samples, including longitudinal analyses. All statistical analyses were weighted to account for sampling probabilities and subgroup response rates to the 1991 survey. A P value of .05 was set as the level of statistical significance for all comparisons.
We defined retention duration as the number of months from the date physicians began working in their index practices, as reported in the 1991 survey, through the date they stopped working there, as reported in 1996 or 1997.
We used statistical tests that accounted for the sampling design and for which approximately normal or χ2 distributions were applicable to compare HPSA and non-HPSA cohorts on physician, practice, job, and community characteristics commonly thought to affect retention. We dichotomized or trichotomized continuous variables reflecting income, on-call frequency, and non-call work hours because we anticipated that their relationships with retention would not be linear over their entire range. We used Cox proportional hazard models, applied in a manner that accounted for the sampling design, to test for differences in the retention duration of the HPSA and non-HPSA cohorts and to identify the correlates of retention within the HPSA cohort.28 Kaplan–Meier survival estimate plots, also weighted, were used to visually contrast the retention of physician subgroups.
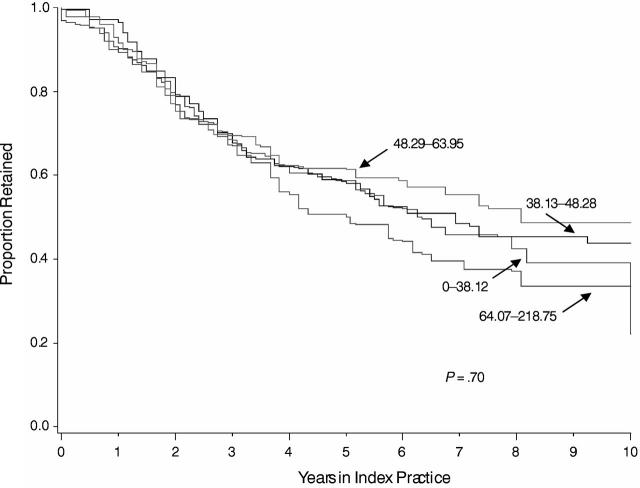
Because secondary criteria are used in making HPSA designations—measures of population economic, cultural, and linguistic needs, and travel distances to nearby communities29—we wondered whether associations between areas of physician scarcity and shorter retention might be obscured in comparisons of HPSA and non-HPSA retention. We therefore also tested for retention differences with a second, purer measure of physician availability: we grouped the physicians of the HPSA and non-HPSA cohorts together and compared the retention duration of those working in counties arrayed into 4 quartiles of primary care physician–to-population ratios with a Cox proportional hazards model.
RESULTS
Description of the Study Populations
These rural generalist physicians were typically young, male, and non-Hispanic White (Table 1 ▶). The HPSA and non-HPSA groups were generally similar in their backgrounds, personal characteristics, and primary care specialty proportions.
TABLE 1—
HPSA and non-HPSA Physician Cohorts, Communities, and Index Practicesa: 1991
| HPSA Cohort(n = 308) | Non-HPSA Cohort (n = 197) | P | |
| Physician Characteristics | |||
| Mean age when arriving at index practice, y | 36.7 | 35.4 | .08 |
| Men, no. (%) | 240 (76.9) | 155 (80.2) | .45 |
| Non-Hispanic White, no. (%) | 259 (81.6) | 174 (88.5) | .07 |
| Has children aged younger than 18 y, no. (%) | 199 (61.3) | 140 (72.4) | .03 |
| Rural upbringing, no. (%) | 152 (48.7) | 95 (48.6) | .98 |
| Raised or trained in state of index practice, no. (%) | 156 (48.9) | 103 (55.2) | .22 |
| International medical school graduate, no. (%) | 51 (20.9) | 26 (14.9) | .19 |
| Specialty, no. (%) | |||
| Family practice | 189 (53.1) | 100 (48.0) | .20 |
| Internal medicine | 65 (25.7) | 52 (29.5) | .24 |
| Pediatrics | 29 (10.0) | 32 (15.0) | .02 |
| General practice | 25 (11.2) | 13 (7.4) | .33 |
| Prior practice experience, no. (%) | 165 (58.0) | 111 (54.1) | .40 |
| Community Characteristics | |||
| Town population, mean | 4926 | 11 985 | <.001 |
| County features | |||
| Population Black, Hispanic, Asian, or Native American, % | 19.5 | 15.7 | .07 |
| Per capita income, mean $ | 12 436 | 14 172 | <.001 |
| Adjacent to metropolitan county, no. (%) | 131 (46.6) | 92 (48.8) | .68 |
| Primary care physicians per 100 000 population, mean | 15.1 | 29.1 | <.001 |
| Practice and Job Characteristics | |||
| Practice ownership, no. (%) | |||
| Owner is the respondent physician | 125 (43.0) | 82 (46.9) | .46 |
| Owner is a hospital, other physicians, or other for-profit entity | 117 (39.9) | 92 (47.0) | .18 |
| Owner is a nonprofit organization | 55 (17.5) | 11 (6.3) | <.001 |
| Solo practice, no. (%) | 124 (42.4) | 45 (25.4) | <.001 |
| Work hours, no. (%) | |||
| On-call 3 or more times per week | 176 (64.2) | 82 (45.6) | .001 |
| Non-call work hours more than 50 per week | 146 (47.6) | 100 (56.5) | .11 |
| Starting income, $, no. (%) | |||
| < 60 000 | 107 (40.2) | 70 (40.2) | .99 |
| > 80 000 | 70 (21.8) | 29 (15.6) | .12 |
Note. HPSA = health professional shortage area.
aAll percentages, mean values, and statistical comparisons are weighted. Counts are not weighted.
As expected, the HPSA cohort worked in smaller towns than the non-HPSA cohort (mean population 4926 vs 11 985, respectively, P < .001 ) and in counties with fewer primary care physicians per 100 000 population (15.1 vs 29.1, P < .001 ) and lower mean per capita incomes ($12 436 vs $14 172, P < .001 ).
More than 40% of each group worked in practices they owned, and somewhat fewer worked in for-profit entities owned by others. Physicians in HPSAs were more likely to work for nonprofit organizations (17.5% vs 6.3%, P < .001 ) and in solo practices (42.4% vs 25.4%, P < .001 ). In addition, HPSA physicians more often worked 3 or more nights on-call each week than the non-HPSA cohort (64.2% vs 45.6%, P = .001 ). The groups had comparable non-call work hours and incomes.
Retention Patterns
Retention in the HPSA and non-HPSA groups was comparable: Figure 1 ▶ shows that the relative risk of leaving at each point in time (the hazard ratio) for the HPSA cohort relative to the non-HPSA cohort was 1.28 (95% confidence interval [CI] = 0.97, 1.69, P = .08). The retention of the HPSA and non-HPSA cohorts remained statistically comparable after adjusting for the personal characteristics on which the physicians of the 2 groups differed or nearly differed statistically—age, race/ethnicity, having children, and international versus US medical school attendance (adjusted hazard ratio, 1.19; 95% CI = 0.89, 1.58, P = . 24). We also compared retention for counties grouped into quartiles of primary care physician–to-population ratios (Figure 2 ▶). We found no significant differences in retention across the 4 quartiles of this second measure of physician availability (P = .70 for equality of hazard ratios).
FIGURE 1—
Retention “survival” curves for primary care physicians in rural HPSA (n = 300) and non-HPSA (n = 195) settings.
FIGURE 2—
Retention of physicians grouped by quartiles of county primary care physician–to-population ratios (n = 485).
Correlates of Retention for the HPSA Cohort
Among the personal and professional characteristics of HPSA physicians, only parenting a minor-age child and working in a state where one grew up or trained correlated with longer retention (Table 2 ▶, Model 1). Other individual characteristics—gender, race/ethnicity, age, rural upbringing, international versus US medical school attendance, medical specialty, and prior practice experience—were unrelated to how long physicians remained in their rural, underserved area practices. Town size and county characteristics (population size, racial/ethnic composition, mean income, physician density) were unrelated to retention for these HPSA physicians (Table 2 ▶, Model 2). Among characteristics of HPSA physicians’ practices and jobs, retention was longer for those who owned their practices and those on-call 2 or fewer times per week (Table 2 ▶, Model 3). When all physician, community, and practice variables were tested together (Table 2 ▶, Model 4), 1 new retention correlate emerged: general practitioners were found to be significantly more likely than family physicians to leave their practices.
TABLE 2—
Correlates of Leaving Sooner vs. Later Among Primary Care Physicians in Rural HPSA Practicesa
| Partial Models | ||||||||
| Model 1: Physician Characteristics (n = 288) | Model 2: Community Characteristics (n = 291) | Model 3: Practice and Job Characteristics (n = 277) | Model 4: All Characteristics (n = 259) | |||||
| Hazard Ratio | P | Hazard Ratio | P | Hazard Ratio | P | Hazard Ratio | P | |
| Physician Characteristics | ||||||||
| Men | 1.00 | .99 | — | — | 1.10 | .70 | ||
| Non–Hispanic White | 1.04 | .88 | — | — | 0.88 | .57 | ||
| Age (per 10 y) | 0.85 | .28 | — | — | 0.79 | .14 | ||
| Has children aged younger than 18 y | 0.61 | .02 | — | — | 0.63 | .05 | ||
| Rural upbringing | 0.79 | .20 | — | — | 0.73 | .11 | ||
| Raised or trained in state of index practice | 0.67 | .04 | 0.69 | .05 | ||||
| International medical school graduate | 0.82 | .46 | — | — | 0.86 | .60 | ||
| Internal medicine specialty (vs family practice) | 1.19 | .41 | — | — | 1.16 | .52 | ||
| Pediatrics specialty (vs family practice) | 0.87 | .70 | — | — | 0.85 | .69 | ||
| General practice specialty (vs family practice) | 1.76 | .10 | — | — | 2.52 | .01 | ||
| Prior practice experience | 0.92 | .67 | — | — | 1.06 | .80 | ||
| Community Characteristics | ||||||||
| Town population (per 1000) | — | 0.98 | .22 | — | 0.99 | .41 | ||
| County population percentage Black, Hispanic, | — | 1.02 | .63 | — | 1.01 | .82 | ||
| Asian, or Native American (per 10%) | ||||||||
| County per capita income (per $1000) | — | 1.04 | .42 | — | 1.04 | .35 | ||
| County adjacent to metropolitan county | — | 1.32 | .17 | — | 1.31 | .21 | ||
| County primary care physicians per 100 000 population (per 10 physicians) | — | 0.98 | .78 | — | 0.93 | .22 | ||
| Practice and Job Characteristics | ||||||||
| Respondent owns the practice (vs practice is for-profit and owned by others) | — | — | 0.42 | <.001 | 0.45 | .001 | ||
| Practice is nonprofit (vs practice is for profit and owned by others) | — | — | 0.91 | .65 | 0.95 | .83 | ||
| Solo practice (vs group) | — | — | 0.92 | .70 | 0.85 | .46 | ||
| On-call 3 or more days per week | — | — | 1.64 | .01 | 1.75 | .008 | ||
| Non-call work hours more than 50 per week | — | — | 1.03 | .89 | 0.98 | .93 | ||
| Starting income less than $60 000(vs $60 000–80 000) | — | — | 1.33 | .17 | 1.35 | .22 | ||
| Starting income greater than $80 000(vs $60 000–80 000) | — | — | 1.16 | .47 | 1.05 | .83 | ||
| Overall model Wald F statistic | 2.26 | 1.14 | 3.17 | 2.21 | ||||
| Model P value | .01 | .34 | .003 | .001 | ||||
Note. HPSA = health professional shortage area.
aAll models are weighted for strata sampling fractions and subgroup response likelihood.
Because retention data were available for nearly all physicians for the first 8 years in their index practices but for fewer subjects thereafter, the tails of the survival curves could be estimated with less certainty than for earlier years. We repeated Table 2 ▶’s models of retention correlates with data for physicians’ first 8 years only; the findings did not change.
We also verified that the number of variables included in the full survival model (Table 2 ▶, Model 4) did not exceed the capacity of the sample size. We reduced this model to include only the 9 variables associated with retention below the P = .25 level of significance in any of the 3 smaller models of physician, community, and practice/job variables. The same previously significant correlates remained in this reduced-form model, but those working in a county adjacent to a metropolitan county also were found to leave sooner (hazard ratio = 1.48; P = .04).
DISCUSSION
Contrary to common belief, these data indicate that retention for generalist physicians is minimally, if at all, different in rural HPSAs and rural non-HPSAs. Therefore, these data suggest that poor retention generally is not the reason that some rural communities develop physician shortages. Coupled with the findings of earlier studies that fewer physicians move into shortage areas,7,8,12 we concluded that the principal dynamic by which rural shortage areas emerge is simply that too few physicians are recruited. Retention issues generally do not worsen relative physician scarcities in rural shortage areas created by poor recruitment. This study does not address physician retention in rural areas relative to that in urban areas, but we noted that 3 of the 4 relevant studies we are aware of found no differences in rural and urban retention,17,30,31 and the 4th found slightly longer retention in rural areas.32
As previous studies have found for physicians in similar settings,10,13,30,31 retention for this study’s rural HPSA physicians was generally unrelated to community socioeconomic indicators; specifically, it was unrelated to local per capita incomes, population racial/ethnic compositions, and town sizes. In previous recruitment studies, these community features repeatedly have been found to correlate with physician in-migration rates and prevalence counts.4,7,30,33 Apparently, social and professional amenities and the economic vitality of communities attract physicians but do not influence their subsequent retention. Similarly, the personal characteristics of physicians previously shown to predict rural recruitment—rural upbringing, male gender, family medicine specialty1,34–38—were generally unrelated to how long generalists in this study remained in underserved area practices. Prior studies of retention in nonunderserved rural areas also have found that the characteristics of the atypical, 1-out-of-10 physician who chooses a rural practice do not characterize those who will remain longer.17,20,30,38,39 Recruiting and retaining are thus distinct processes.
In this study, physicians who owned their practices and those on-call 2 or fewer times per week remained longer. We theorize that buying a practice is a marker of greater commitment from the outset and that buying a practice in and of itself makes physicians more committed to both their practices and communities. Further, it can be difficult to sell a rural practice when a physician wishes to move on. Physicians’ complaints in earlier studies40 about the around-the-clock strain of rural practice may explain why those in this study who were on-call more often left sooner.
The Policy Question
If the forces that affect recruitment and retention differ, and poor retention generally is not the reason for underserved areas, are broad “recruitment and retention” initiatives necessary? Should initiatives perhaps target poor recruitment only?
We note that even if retention is not the usual cause for shortages, physician numbers would nevertheless improve in shortage areas if interventions were taken to lengthen how long physicians stayed. Further, given the retention correlates identified here and in previous studies, retention may be particularly amenable to programmatic interventions. Retention is related to modifiable characteristics of work, whereas recruitment is related to the relatively immutable characteristics of physicians’ backgrounds and professional and lifestyle preferences, as well as the socioeconomic features of communities.16,20,41 To promote retention, local, state, and federal programs can promote practice ownership through low-interest loans and start-up income guarantees. Practice administrators can build a sense of personal investment and control among employed physicians by offering leadership opportunities and providing a greater voice in clinic policies and work schedules.39 Local hospitals and practice networks can reduce on-call frequency by coordinating cross-coverage arrangements. Work demands while on-call can be lessened by providing telephone call triage systems and full-time physician staffing in local emergency rooms.
Limitations
The explanatory variables we used were primarily self-reported and thus subject to reporting inaccuracies. Any inaccuracies are likely nondifferential.
We based our conclusion that retention was similar for physicians in HPSAs and non-HPSAs on a Cox hazard model with a non-significant P value of .08. Perhaps a larger study would have found a significant difference. The sample size of this study provided approximately 90% power to detect a hazard ratio of 1.6 or larger, which corresponds to approximately a 15% difference in percent retained for the 2 groups near the 5-year median retention point for HPSAs. This study had approximately .60 power to detect a hazard ratio of 1.36, or approximately a 10% difference in percent retained at 5 years. Evidence suggesting that group retention would not have differed in a larger study includes (a) the hazard ratio moved further from statistical significance (P=.24) with adjustments for group differences in baseline physician characteristics and (b) retention did not differ (P=.70) across county primary care physician–to-population ratio quartiles, a separate measure of underservice. Nevertheless, with P values for unadjusted comparisons for our primary model hovering close to .05, we qualify our findings by noting that HPSA and non-HPSA retention may have differed statistically in a larger study; however, the difference would have been modest.
The Kaplan–Meier survival curves of the HPSA and non-HPSA cohorts (Figure 1 ▶) visually appear to separate in the middle years studied. We assessed this observation in after-the-fact (post hoc) statistical comparisons and found that unadjusted survival rates indeed differed when examined up through only 7 years (P < .05); however, we also found that this difference was not significant when we controlled for baseline physician characteristics. Whether there is a specific period in physicians’ work tenures when retention rates in HPSAs and non-HPSAs diverge and later re-converge should be reassessed prospectively in other physician cohorts.
Conclusions and Policy Recommendations
A recent Council on Graduate Medical Education report lamented “one of the greatest barriers to better focused health workforce policy has been a lack of research into the causes and consequences of shortages.”1(p6) With little critical research available, theories about the nature of shortages have been loosely conceived and often not confirmed. Physician shortages, poor recruitment, and poor retention have been assumed to go hand-in-hand, with “undesirable” characteristics of communities suspected to be the common root cause. Broad recruitment and retention initiatives have been the reflexive remedy in the United States and elsewhere, but this remedy has met with limited success.
Our study, as well as related studies, suggests physician retention is minimally or not at all worse in rural underserved communities than in rural nonunderserved communities. Instead, the most straightforward interpretation of current evidence is that local rural shortages generally develop when too few physicians are recruited, which often occurs when local amenities, economies, and practice situations are unattractive. Physician retention, by contrast, appears unrelated to the amenities communities offer, but is related to physicians’ work and family situations, their satisfaction, and their relationships with their communities.14,42–46
Underserved communities and state and national health planners should develop separate, tailored recruitment programs and retention programs. Recruitment strategies are important because low recruitment is generally the reason shortages arise. Retention strategies are important because particularly strong retention can offset poor recruitment, the issues affecting retention may be more mutable, and physician turnover at any level is disruptive to patient care and expensive47 for practices. We suggest eliminating the phrase “recruitment and retention” from the lexicon of rural health clichés so that these 2 distinct processes are less often misunderstood to be one and the same.
Acknowledgments
This study was funded by the US Agency for Healthcare Research and Quality (AHRQ) (grant R03-HS10654). The original survey was funded by the AHRQ (then called the Agency for Health Care Policy and Research) (grant R01-HS06544), and the follow-up survey was funded by the US Bureau of Health Professions, Health Resources and Services Administration (grant U76 MB 00005).
The authors are indebted to the many project staff who helped to gather these questionnaire data and to prepare this report and to the physicians who gave their valuable time to complete 2 questionnaires.
Human Participant Protection This study was exempted from review by the office of human research ethics of the School of Medicine of the University of North Carolina at Chapel Hill.
Contributors D. E. Pathman conceived the study, supervised all aspects of its implementation and led the writing. T. R. Konrad assisted with the study conceptualization. R. Dann and G. Koch assisted with the analyses and oversaw statistical issues. All authors helped design the analysis plans, interpreted findings, and reviewed drafts of the article.
Peer Reviewed
References
- 1.Council on Graduate Medical Education. Tenth Report: Physician Distribution and Health Care Challenges in Rural and Inner-City Areas. Washington, DC; Dept of Health and Human Services; 1998.
- 2.Selected Characteristics of Health Professional Shortage Areas. Washington, DC; Health Resources and Services Administration; 2001.
- 3.Health Resources and Services Administration. National Health Service Corps. Available at: http://bhpr.hrsa.gov/nhsc/. Accessed October 26, 2003.
- 4.Health Care in Rural America. Washington, DC; Office of Technology Assessment; 1990. OTA publication OTA-H-434.
- 5.Rosenblatt RA, Hart LG. Physicians and Rural America. In: Ricketts TC, ed. Rural Health in the United States. New York, NY: Oxford University Press, 1999; 38–51.
- 6.Pathman DE, Taylor DH, Konrad TR, et al. State scholarship, loan forgiveness, and related programs: the unheralded safety net. JAMA. 2000; 284:2084–2092. [DOI] [PubMed] [Google Scholar]
- 7.Langwell KM, Drabek J, Nelson SL, Lenk E. Effects of community characteristics on young physicians’ decisions regarding rural practice. Public Health Rep. 1987; 102:317–328. [PMC free article] [PubMed] [Google Scholar]
- 8.Li H. Physician Migration in Non-Metropolitan Counties of the United States from 1987 to 1990 [dissertation]. Chapel Hill, NC: University of North Carolina at Chapel Hill; 1995.
- 9.Frenzen PD. The increasing supply of physicians in urban and rural areas, 1975 to 1988. Am J Public Health. 1991;81:1141–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kindig DA, Schmelzer JR, Hong W. Age distribution and turnover of physicians in nonmetropolitan counties of the United States. Health Serv Res. 1992; 27:565–578. [PMC free article] [PubMed] [Google Scholar]
- 11.Newhouse JP. Geographic access to physician services. Annu Rev Public Health. 1990;11:207–230. [DOI] [PubMed] [Google Scholar]
- 12.Wright GE. Community Characteristics and the Competition for Physicians in Rural America, 1971–1981, Final Report. Washington, DC: Health Policy Division, US Dept of Health and Human Services; 1985.
- 13.Pathman DE, Konrad TR, Ricketts TC. The comparative retention of National Health Service Corps and other rural physicians: results of a 9-year follow-up study. JAMA. 1992;268:1552–1558. [PubMed] [Google Scholar]
- 14.Pathman DE, Konrad TR, Ricketts TC. The National Health Service Corps experience for rural physicians in the late 1980s. JAMA. 1994;272:1341–1348. [PubMed] [Google Scholar]
- 15.Rosenblatt RA, Saunders G, Shreffler J, Pirani MJ, Larson EH, Hart LG. Beyond retention: National Health Service Corps participation and subsequent practice locations of a cohort of rural family physicians. J Am Board Fam Pract. 1996;9:23–30. [PubMed] [Google Scholar]
- 16.Kim C.Recruitment and retention in the Navajo area Indian Health Service. West J Med. 2000;173:240–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singer JD, Davidson SM, Graham S, Davidson HS. Physician retention in community and migrant health centers: who stays and how long? Med Care. 1998;36:1198–1213. [DOI] [PubMed] [Google Scholar]
- 18.Forti EM, Martin KE, Jones RL, Herman JM. Factors influencing retention of rural Pennsylvania family physicians. J Am Board Fam Pract. 1995;8:469–474. [PubMed] [Google Scholar]
- 19.Parker RC, Tuxill TG. The attitudes of physicians toward small-community practice. J Med Educ. 1967; 42:327–344. [DOI] [PubMed] [Google Scholar]
- 20.Parker RC, Sorensen AA. The tides of rural physicians: The ebb and flow, or why physicians move out of and into small communities. Med Care. 1978;16:152–166. [DOI] [PubMed] [Google Scholar]
- 21.Conte SJ, Imershein AW, Magill MK. Rural community and physician perspectives on resource factors affecting physician retention. J Rural Health. 1992;8:185–196. [DOI] [PubMed] [Google Scholar]
- 22.McGinn PR. Rural practice: Long hours, low rates. Am Med News. July 29, 1988:12–13.
- 23.Mullan F. The National Health Service Corps and health personnel innovations: beyond poorhouse medicine. In: Sidel VW, Sidel R, eds. Reforming Medicine: Lessons from the Last Quarter Century. New York, NY: Pantheon; 1984:176–200.
- 24.Pathman DE, Agnew CR. Querying physicians’ beliefs in career choice studies: the limitations of introspective causal reports. Fam Med. 1993;25:203–207. [PubMed] [Google Scholar]
- 25.Pathman DE, Konrad TR, Agnew CR. Studying the retention of rural physicians. J Rural Health. 1994; 10:183–192. [DOI] [PubMed] [Google Scholar]
- 26.Council on American Survey Research Organizations. On the Definition of Response Rates: A Special Report from the CASRO Task Force on Completion Rates. Port Jefferson, NY: Council of American Survey Research Organizations; 1982.
- 27.National Center for Health Workforce Analysis, Health Resources and Services Administration. Area Resource File. Available at: http://www.arfsys.com. Accessed July 28, 2004.
- 28.Cox DR. Regression models and life tables. Journal of the Royal Statistical Society Series B. 1972;34:187–220. [Google Scholar]
- 29.Bureau of Primary Health Care Programs. Guidelines for Primary Care HPSA Designation. Available at: http://bhpr.hrsa.gov/shortage/hpsacritpcm.htm. Accessed October 26, 2003.
- 30.Horner RD, Samsa GP, Ricketts TC. Preliminary evidence on retention rates of primary care physicians in rural and urban areas. Med Care. 1993;31:0640–648. [DOI] [PubMed] [Google Scholar]
- 31.Tilson HH. Stability of physician employment in neighborhood health centers. Med Care. 1973;11:384–400. [DOI] [PubMed] [Google Scholar]
- 32.Kerstein J, Pauly MV, Hillman A. Primary care physician turnover in HMOs. Health Serv Res. 1994;29:17–37. [PMC free article] [PubMed] [Google Scholar]
- 33.Connor RA, Hillson SD, Krawelski JE. Competition, professional synergism, and the geographic distribution of rural physicians. Med Care. 1995;33:1067–1078. [DOI] [PubMed] [Google Scholar]
- 34.Council on Graduate Medical Education. Third Report. Improving Access to Health Care Through Physician Workforce Reform: Directions for the 21st Century. Washington, DC: Department of Health and Human Services; 1992.
- 35.West PA, Norris TE, Gore EJ, Baldwin LM, Hart LG. The geographic and temporal patterns of residency-trained family physicians: University of Washington Family Practice Residency Network. J Am Board Fam Pract. 1996;9:100–108. [PubMed] [Google Scholar]
- 36.Leonardson G, Lapierre R, Hollingsworth D. Factors predictive of physician location. J Med Educ. 1985; 60:37–43. [DOI] [PubMed] [Google Scholar]
- 37.Ellsbury KE, Baldwin LM, Johnson KE, Runyan SJ, Hart LG. Gender-related factors in the recruitment of physicians to the rural Northwest. J Am Board Fam Pract. 2002;15:391–400. [PubMed] [Google Scholar]
- 38.Rabinowitz HK, Diamond JJ, Hojat M, Hazelwood CE. Demographic, educational and economic factors related to recruitment and retention of physicians in rural Pennsylvania. J Rural Health. 1999;15:212–218. [DOI] [PubMed] [Google Scholar]
- 39.Pantell RH, Reilly T, Liang MH. Analysis of the reasons for the high turnover of clinicians in neighborhood health centers. Public Health Rep. 1980;95:344–350. [PMC free article] [PubMed] [Google Scholar]
- 40.Rourke JTB. Politics of rural health care: recruitment and retention of physicians. Can Med Assoc J. 1993;148:1281–1284. [PMC free article] [PubMed] [Google Scholar]
- 41.Singer JD, Davidson SM, Graham S, Davidson HS. Physician retention in community and migrant health centers: who stays and for how long? Med Care. 1998; 36:1198–1213. [DOI] [PubMed] [Google Scholar]
- 42.Cutchin MP, Norton JC, Quan MM, Bolt D, Hughes S, Lindeman B. To stay or not to stay: issues in rural primary care physician retention in Eastern Kentucky. J Rural Health. 1994;10:273–278. [DOI] [PubMed] [Google Scholar]
- 43.Cutchin MP. Community and self: concepts for rural physician integration and retention. Soc Sci Med. 1997;44:1661–1674. [DOI] [PubMed] [Google Scholar]
- 44.Cutchin MP. Physician retention in rural communities: the perspective of experiential place integration. Health & Place. 1997;3:25–41. [DOI] [PubMed] [Google Scholar]
- 45.Pathman DE, Konrad TR, Williams ES, Scheckler WE, Linzer M, Douglas J. Does dissatisfaction promote job turnover among physicians or satisfaction prevent it, or both? J Fam Pract. 2002; 51:593. Also available at: http://www.jfponline.com/content/2002/07/jfp_0702_0593b.asp. Accessed July 7, 2004. [PubMed] [Google Scholar]
- 46.Lichtenstein RL. The job satisfaction and retention of physicians in organized settings: a literature review. Med Care Rev. 1984;41:139–179. [DOI] [PubMed] [Google Scholar]
- 47.Buchbinder SB, Wilson M, Melick CF, Powe NR. Estimates of costs of primary care physician turnover. Am J Manag Care. 1999;5:1431–1438. [PubMed] [Google Scholar]