Abstract
Objectives. We sought to determine whether disparities in health-related quality of life exist between veterans who live in rural settings and their suburban or urban counterparts.
Methods. We determined health-related quality-of-life scores (physical and mental health component summaries) for 767109 veterans who had used Veterans Health Administration services within the past 3 years. We used rural/urban commuting area codes to categorize veterans into rural, suburban, or urban residence.
Results. Health-related quality-of-life scores were significantly lower for veterans who lived in rural settings than for those who lived in suburban or urban settings. Rural veterans had significantly more physical health comorbidities, but fewer mental health comorbidities, than their suburban and urban counterparts. Rural–urban disparities persisted in all survey subscales, across regional delivery networks, and after we controlled for sociodemographic factors.
Conclusions. When compared with their urban and suburban counterparts, veterans who live in a rural setting have worse health-related quality-of-life scores. Policymakers, within and outside the Veterans Health Administration, should anticipate greater health care demands from rural populations.
Vulnerable patient populations that live in rural settings, such as veterans,1 the poor,2 and the elderly3,4 have health care needs similar to those of their urban counterparts in several studies. But providing access to a full spectrum of health care services in a rural setting is a difficult undertaking. Access to expensive technologies5 and specialty care6,7 may be limited by the high costs to the health care system associated with providing that care. Although funded federal8 and nonfederal9 programs have been effective at improving primary care access in rural settings, physicians may be reluctant to locate their practices in rural settings.10–12 The combination of limited numbers of specialists (who for economic reasons need large patient populations to thrive), similar service needs of rural and urban populations, and patients’ tendency to be loyal to local care (preferring their local secondary hospital) in rural settings may result in greater demand for primary care services and may influence primary care practice management.13 Limitations in resources other than health care in rural settings, such as personal finances,14,15 may further restrict access to health care and influence the quality of life of patients.
The Veterans Health Administration (VHA) provides comprehensive health care services to veterans across the United States through regional delivery networks. Because of its relatively small service population, regionalizing services within the VHA has required establishing large referral regions, with all VHA tertiary care referral centers located in urban areas. Travel distances for rural veterans who are remote from referral centers may implicitly restrict veterans’ access to these services, and restricted access may result in underutilization of services.16,17
If rural veterans have a lower health-related quality of life than their urban counterparts, the cost-efficient strategy of regionalization may concentrate services far away from where the greatest needs exist; such disparities would have important implications for redirecting health care resources. We therefore sought to determine whether there are disparities in the health-related quality of life between veterans who live in rural settings and their suburban or urban counterparts, nationally and at the level of coordination of health care delivery.
METHODS
Measures
We conducted a cross-sectional study of health-related quality-of-life scores using the 1999 Large Health Survey of Veteran En-rollees.18 That survey used a modification of the Medical Outcomes Study (MOS) Short Form 36 called the Veterans SF-36.19 The Veterans SF-36 has been widely used, disseminated, and documented as reliable and valid in the veteran population that uses the VHA.20 Like the MOS SF-36, the Veterans SF-36 measures 8 concepts of health: physical functioning, role limitations owing to physical problems, bodily pain, general health perceptions, energy/vitality, social functioning, role limitations owing to emotional problems, and mental health. In veterans, the physical health component summary (PCS) and mental health component summary (MCS) scores, weighted summaries of the 8 scales, demonstrate increased precision over the MOS version.21,22 In late 1999, the survey was administered to a random sample of 1.4 million veterans enrolled in the VHA system who had used VHA services within the prior 3 years or who had enrolled in the VHA, anticipating future service use. Of those, 877775 responded to the survey and 805422 responded with usable Veterans SF-36 data. Zip code data were not available for 38313 veterans, or 4.4% of the total respondents, leaving 767109 veteran respondents in the analysis. From Veterans SF-36 responses, we calculated PCS and MCS scores and 8 subscale scores.
PCS and MCS scores are standardized with a norm of 50 and a standard deviation of 10 in a general US population. Lower scores denote worse health for the summaries and subscales, and differences in Veterans SF-36 of 2.5 points have been associated with increased morbidity.21 For example, when other diseases are controlled, angina is associated with a 2.5-point-lower PCS score, chronic lung disease with a 3.6-point-lower score, and chronic low back pain with a 5.5-point-lower score. Similarly, when other diseases are controlled, depression is associated with an 8.0-point-lower MCS score, alcohol disorders with a 6.6-point-lower score, and chronic low back pain with a 2.8-point-lower score. Lower scores have also been associated with increased health services utilization. For veterans, a 1-point decrease in PCS is associated with an annual $148.20, or 3.2%, increased cost of care over the average cost of $4632 per patient; and a 1-point decrease in MCS, with an independent annual $86.40, or 1.9%, increase in costs of care per patient when age, gender, and International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM)-defined co-morbidities are controlled.23,24 Therefore, population differences in Veterans SF-36 scores can be used to anticipate population differences in morbidity, health care needs, and anticipated health care expenditures.
The survey also collected social security number, self-reported demographic data (age, gender, race, maximal educational attainment, and employment status), and zip code of residence. We linked respondents’ social security numbers to VHA administrative databases to determine the following:
1. Veterans’ VHA priority levels. Priority levels range from 1 to 7, are specific to an individual veteran, and are associated with the severity of service-related disabilities, special status, and income level. Veterans with priority levels 1 through 6 tend to be more disabled, poorer, and more reliant on the VHA for health care services and have lower mean MCS and PCS scores.20
2. Comorbidity indices. Measures of comorbidity were obtained by linking social security numbers to veterans’ VHA utilization record. Mental and physical health comorbidity indices were calculated as the sum of ICD-9-CM codes for 6 mental health and 30 medical diagnoses recorded in outpatient or inpatient treatment for the 3 years before the survey. The indices range from 0 to 6 for mental health and 0 to 30 for physical health.25 For example, a patient who had ICD-9-CM codes for 2 mental health and 4 physical health conditions would have a mental health comorbidity index of 2 and a physical health comorbidity index of 4.
We used zip code of residence to calculate 3 variables:
1. Degree of rurality. To identify veterans as living in a rural, suburban, or urban setting, we used the US Department of Agriculture’s rural–urban commuting area (RUCA) designation,26 a 10-point designation of rural and urban status, based on travel and shopping patterns, and designated at the county level. We then used the University of Washington’s probabilistic zip code–to–county crosswalk file, wherein zip codes are designated with RUCA codes, to assign veterans’ zip codes to their RUCA designations.27 We defined 3 comparison groups: urban (RUCA code 1), suburban (RUCA codes 2 through 6), and rural (RUCA codes 7 through 10). RUCA category definitions, the groupings that we used, the proportion of the general US population in each category, the number of survey respondents in each category, and mean PCS and MCS scores are shown in Table 1 ▶.
TABLE 1—
US Department of Agriculture Rural–Urban Commuting Area (RUCA) Code Definitions
| RUCA Code | Definition | Study Grouping | 1998 US Population in RUCA Category, % | Veteran Respondents in RUCA Category (n = 767 109), % | Mean PCS Score | Mean MCS Score |
| 1 | Metropolitan area | Urban | 65.5 | 56.4 | 36.80 | 45.48 |
| 2 | ≥30% commuting to metropolitan area | Suburban | 9.8 | 8.1 | 34.81 | 45.08 |
| 3 | 5%–30% commuting to metropolitan area | Suburban | 0.3 | 0.4 | 34.28 | 44.40 |
| 4 | Large town (10 000–49 999 residents) | Suburban | 6.6 | 10.0 | 34.55 | 44.79 |
| 5 | ≥30% commuting to large town | Suburban | 3.4 | 3.5 | 33.85 | 44.60 |
| 6 | 5%–30% commuting to large town | Suburban | 0.3 | 0.4 | 33.74 | 44.10 |
| 7 | Small town core (2500 to 9999 residents) | Rural | 5.0 | 8.7 | 33.54 | 44.40 |
| 8 | ≥30% commuting to small town | Rural | 2.3 | 2.6 | 32.97 | 43.96 |
| 9 | 5%–30% commuting to small town | Rural | 0.3 | 0.5 | 33.81 | 44.82 |
| 10 | Primary flow to tract without town of ≥2500 residents | Rural | 6.4 | 9.6 | 33.35 | 44.61 |
Note. PCS = physical health component summary; MCS = mental health component summary.
2. VHA geographic setting. Because we wanted to determine whether any differences found in larger geographic regions had bearing on the VHA’s local service delivery, we also used zip codes of residence to locate each respondent within a single Veterans Integrated Service Network (VISN). VISNs are the budgetary and organizational mechanism for VHA health care delivery. At the time of the study, 22 geographically defined VISNs existed. In the figures and text, we identify these regions by the city in which their headquarters are located.
3. Census region. To examine regional variation across the United States, we examined the 4 major US census regions: Northeast, South, Midwest, and West. VISNs are approximately aligned with US census regions as follows: Northeast: Boston, Mass, Albany and the Bronx, NY, and Pittsburgh, Pa; South: Baltimore, Md, Durham, NC, Atlanta, Ga, Bay Pines, Fla, Nashville, Tenn, and Dallas, Tex; Midwest: Cincinnati, Ohio, Ann Arbor, Mich, Chicago, Ill, Minneapolis, Minn, Omaha, Neb, Kansas City and Jackson, Mo; and West: Phoenix, Ariz, Denver, Colo, Portland, Ore, and San Francisco and Los Angeles, Calif.
Statistical Analysis
We examined analysis of variance for continuous variables and the χ2 test for categorical variables to compare demographic variables among the 3 groups (urban, suburban, and rural). We compared unadjusted mean PCS and MCS scores and 8 subscale scores for the nation and each delivery network using analysis of variance. To compare across degrees of rurality within regional delivery networks, we subtracted suburban and rural scores from urban scores for each network. Multivariate analysis using ordinary least square regression was conducted to examine the association of rural–urban status with Veterans SF-36 controlling for sociodemographic factors (age, gender, employment status, and race), VHA priority status, travel distance to VHA hospitals, comorbidity indices, and US census region. Because data on sociodemographic factors were incomplete, multivariate analysis was limited to 727536 respondents. Because priority-7 veterans have lower health-related quality-of-life scores, are less reliant on VHA care, and represent different proportions of the service population in a number of VISNs, we repeated the analysis for priority-1 through priority-6 veterans and for priority-7 veterans separately.
RESULTS
Veterans who lived in rural settings were somewhat older, had more physical and mental health comorbidities, and lived a greater distance from both private sector and VHA hospital care when compared with those in suburban or urban settings (P<.0001 for all) (Table 2 ▶). Rural veterans were more likely to be male and White but less likely to be employed (P<.0001 for all). Rural veterans were more likely to be in priority groups 3 (service connected 10%–20%, prisoner of war) and 5 (low-income, non–service connected, i.e., indicating a disability that is not related to military service; and 0% service connected, i.e., indicating a disability that has no current adverse impact on veteran’s life), and less likely to be in the other priority groups than their suburban or urban counterparts (P<.0001 for all).
TABLE 2—
Demographics of Sample: United States, 1999
| Mean (SD) | ||||
| Overall (n = 767 109) | Urban (n = 432 285) | Suburban (n = 168 120) | Rural (n = 166 704) | |
| Age, y | 63.4 (13.4) | 62.8 (13.9) | 63.6 (13.0) | 64.7 (12.4) |
| Comorbidities, no. | ||||
| Physical | 2.9 (2.8) | 2.8 (2.8) | 3.0 (2.8) | 3.1 (2.8) |
| Mental | 0.46 (0.96) | 0.49 (1.00) | 0.44 (0.92) | 0.41 (0.88) |
| Miles to VHA hospital care | 41.3 (39.8) | 29.3 (27.2) | 53.1 (37.0) | 62.9 (35.9) |
| Miles to private sector hospital care | 8.1 (7.8) | 3.8 (3.4) | 12.2 (7.9) | 15.2 (8.5) |
| Male, % | 95.9 | 95.3 | 96.3 | 97.2 |
| Race, % | ||||
| White | 77.9 | 71.6 | 85.0 | 87.0 |
| Black | 12.3 | 17.4 | 6.4 | 5.4 |
| Hispanic | 4.2 | 5.6 | 2.8 | 1.9 |
| Other | 5.6 | 5.5 | 5.8 | 5.7 |
| Employment status, % | ||||
| Employed | 21.8 | 23.6 | 20.7 | 18.5 |
| Retired | 41.0 | 41.3 | 40.7 | 40.7 |
| Other | 37.1 | 35.2 | 38.6 | 40.8 |
| Priority group, % | ||||
| 1 (SC ≥50%) | 15.5 | 16.1 | 15.7 | 14.0 |
| 2 (SC 30%–40%) | 9.9 | 10.5 | 10.0 | 8.5 |
| 3 (SC 10%–20%, POW) | 16.5 | 17.9 | 15.7 | 13.7 |
| 4 (Catastrophically disabled) | 2.7 | 2.5 | 2.8 | 3.1 |
| 5 (NSC and 0% SC, low income) | 43.7 | 41.0 | 44.4 | 50.2 |
| 6 (No copay required) | 1.6 | 1.6 | 1.8 | 1.7 |
| 7 (Copay required) | 10.0 | 10.5 | 9.8 | 9.0 |
Note. VHA = Veterans Health Administration; SC = military service–connected disability, rated at a particular impairment percentage; NSC = non–military service–connected disability. Differences among urban, suburban, and rural cohorts are significant at P < .0001 for all variables.
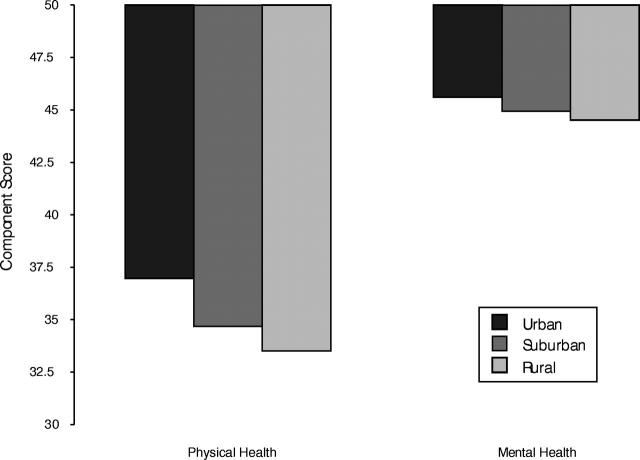
Unadjusted physical and mental health summary scores were significantly lower for veteran respondents who lived in rural settings than for those who lived in suburban or urban settings: rural PCS = 33.53 (95% confidence interval [CI] = 33.48, 33.59) suburban PCS = 34.69 (95% CI = 34.64, 34.75), and urban PCS = 37.00 (95% CI = 36.96, 37.03), P < .001; rural MCS = 44.53 (95% CI = 44.47, 44.60), suburban MCS = 44.95 (95% CI = 44.89, 45.02), and urban MCS = 45.62 (95% CI = 45.58, 45.66), P < .001 (Figure 1 ▶). Veterans who lived in rural settings also had significantly lower scores than their suburban and urban counterparts on all 8 subscale scores (P < .001 for all). Veterans who lived in rural settings had more physical health comorbidities (3.07 [95% CI = 3.06, 3.08] for rural, 2.91 [95% CI = 2.90, 2.93] for suburban, and 2.73 [95% CI = 2.72, 2.74] for urban, P < .001), but fewer mental health comorbidities (0.401 [95% CI = 0.397, 0.405] for rural, 0.426 [95% CI = 0.423, 0.431] for suburban, and 0.476 [95% CI = 0.473, 0.479] for urban, P < .001).
FIGURE 1—
Unadjusted health-related quality-of-life scores, by veterans’ urban/suburban/ rural residence, compared with the general US population scores of 50 for both physical and mental health; a lower score indicates a worse health-related quality of life.
Note. Differences between groups are statistically significant at P < .001. Differences of 2.5 points are considered clinically meaningful.
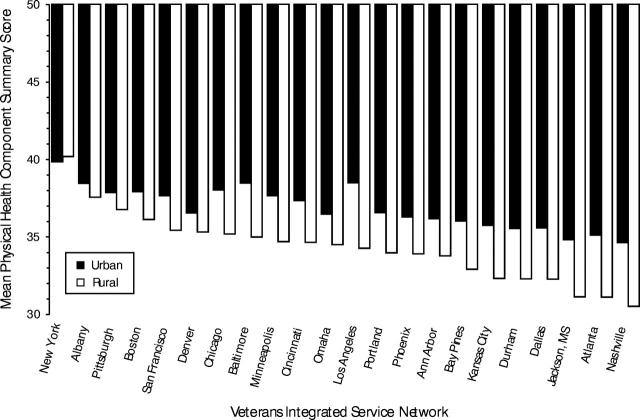
At the regional service delivery network level, veterans who lived in rural settings had significantly lower PCS scores than their suburban (data not shown) and urban counterparts in every VISN except for that headquartered in Bronx, NY (P < .001 for all) (Figure 2 ▶). The few veterans who fell within rural zip codes in this delivery network lived in remote parts of Long Island that house relatively wealthy communities and may not be representative of the overall rural population. Although present, differences in scores between rural and urban veterans within networks were not likely to be clinically meaningful in 8 of the 22 VISNs. All VISNs located in the southern US census region and 5 of 7 VISNs in the Midwest had clinically meaningful differences in physical health–related quality of life when we compared rural to urban veterans.
FIGURE 2—
Urban and rural physical health component summary scores for each veterans integrated service network, arranged by descending urban score and compared with the general US population scores of 50 for both physical and mental health.
Note. The locations of each network headquarters are shown.
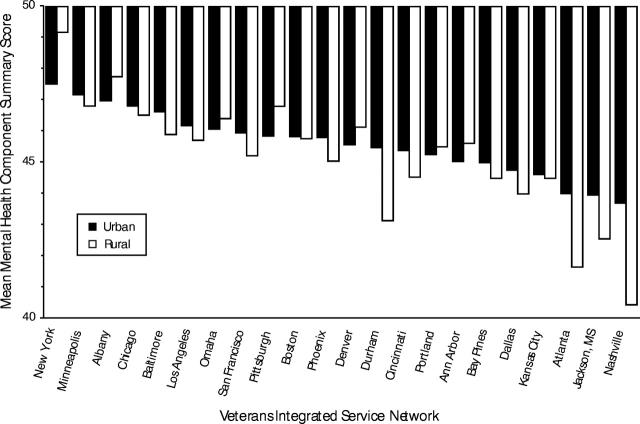
Disparities between rural and urban veterans were much less pronounced when we compared MCS scores across VISNs (Figure 3 ▶). Although urban veterans had statistically higher scores than their rural counterparts in 15 of the 22 VISNs at the P < .001 level, differences were likely to be clinically meaningful only in the VISN headquartered in Nashville, Tenn. Again, disparities were most evident in the southern US census region.
FIGURE 3—
Urban and rural mental health component summary scores for each Veterans Integrated Service Network, arranged by descending urban score and compared with the general US population scores of 50 for both physical and mental health.
Note. The locations of each network headquarters are shown.
Differences that we found between rural and urban veterans using unadjusted data persisted after we controlled for other factors in the multivariate analysis. The mean PCS score for the 727 536 respondents with complete demographic information was 35.6, or 1.4 standard deviation lower than US age-adjusted norms; the mean MCS score was 45.2, or about 0.5 standard deviation lower than US age-adjusted norms. Veterans who were male, unemployed, lived in the southern US census region, and had fewer than 12 years of education had lower PCS and MCS scores. In comparison to priority-7 status, all other priority levels were associated with much lower PCS and MCS scores. Multiple physical comorbidities were associated with lower PCS scores. Finally, after we corrected for other variables, when compared with urban status, rural status was associated with a 2.05-point-lower PCS score and a 0.83-point-lower MCS score. These variables explained 28% of the variance of the PCS scores and 25% of the variance seen in MCS scores. Repeat analyses examining only priorities 1 through 6 and only priority 7 showed similar findings.
DISCUSSION
We found that veterans who lived in rural settings had lower health-related quality-of-life scores than their suburban and urban counterparts. For PCS scores, this relation held at the national and geographic delivery level; for MCS scores, the relation was far less dramatic, although present. Differences in physical health–related quality-of-life scores undoubtedly partially owe to more comorbidity in rural veterans. However, rural–urban disparities persisted after we corrected for age, gender, employment status, priority level, comorbidity, and the US census region in which the veteran lived. Disparities were evident in those who were both most and least dependent on the VHA for health care services.
For those who provide care to rural veterans, these findings offer supportive evidence that living in a rural setting is associated with a worse health-related quality of life. A variety of contributing factors may account for the rural–urban disparities that we found. For instance, it is possible that rurality is a proxy for access to care. In 1 region of the country, we recently demonstrated that rural veterans use fewer VHA and Medicare services than their urban counterparts.28 However, in this cross-sectional analysis, it is impossible to determine whether those with a lower health-related quality of life congregate in more rural settings or rural living results in a lower health-related quality of life.
Our findings have important implications for the resource needs of veterans in rural areas. Others have demonstrated that lower health-related quality-of-life scores are associated with greater health care service needs in the general population.29 The differences that we found suggest that rural veterans will generate health care costs 11% higher than their urban counterparts based on MCS scores and 2% higher based on PCS scores. The combination of lower scores, higher morbidity, higher anticipated greater service needs, and higher anticipated costs suggest that policy-makers should be cautious when comparing costs and utilization of care in rural and urban settings.
In the general population, increasing the number of critical access points, particularly in the southern United States, may help balance access and need. Within the VHA, this balance could be achieved in at least 2 ways. First, the VHA could dedicate more resources to rural health care delivery—through the development of additional programs in rural VHA medical centers, augmented reimbursement for rural delivery systems, or collaboration with the community to enhance non–health care issues that might contribute to a worse quality of life. Since completion of the survey, the VHA has markedly increased the number of primary care access points for all veterans, including those in rural settings, through the establishment of community-based outpatient clinics; the establishment of these clinics may help remedy the disparities that we found. Alternatively, the VHA might consider the development of a coordinated federal health care benefit for veterans who live in rural settings. Veterans are likely to be enrolled in Medicare30; a coordinated federal benefits package for rural veterans could take advantage of existing non-VHA infrastructure in rural settings, thereby improving access to care without expanding infrastructure.
Our study has several limitations. First, it used a cross-sectional database that was limited to self-report of functional status, and the data were obtained 5 years ago, in 1999; we were not able to examine trends over time. Although the sample size was very large and the differences were so dramatic, given the changes that have occurred in health care delivery, patient demographics, and enrollment volume within VHA over the past 5 years, studies using more recent, and longitudinal, data are needed to validate our findings. Second, our study stratified results by rural setting as defined by RUCA codes; the study compared neither the quality of VHA care in rural and urban settings nor the relation between access to that care and health-related quality of life. Additional studies are required to address whether rural veterans’ health-related quality-of-life scores might be enhanced by access to care. Third, we were not able to examine environmental, economic, or social factors that may contribute to lower health-related quality-of-life scores that we found in rural settings. For instance, the differences we found may be facilitated by restricted access to care in rural settings: it is possible that, because of long distance to care for many veterans in rural settings, only those with the greatest health care needs were enrolled in the VHA system and were therefore part of the survey. Fourth, our study was limited to veterans—a population likely to be older, poorer, and sicker than the general population. Although we replicated findings in the healthiest subgroup of veterans, because of the paucity of females and absence of children in our data set, generalization of our findings to the entire US population may be limited. Finally, our study may underestimate differences between rural and urban veterans; the “floor effect” (as the lower bound of the scoring range is approached, scores may fail to capture those who might have even lower health related quality of life)31 that exists at the low score levels that we saw may mitigate the true differences that exist.
Despite these limitations, the findings shed light on health care–related quality of life in the rural population, highlight potential disparities in health care needs, and underscore the challenges of health care delivery to rural populations. These results strongly suggest that administrators anticipate greater health care demands from rural populations and pursue innovative strategies, including coordination of federal health benefits, to meet their health care needs.
Acknowledgments
This work was funded by the Veterans Rural Health Initiative, White River Junction, Vt, VAMC, and by the White River Junction VA Outcomes Group Research Enhancement Award Program (VHA Health Services Research and Development award REA—03–098).
The SF-36 is a registered trademark of the Medical Outcomes Trust.
Human Participant Protection The Dartmouth committee for the protection of human subjects approved the project and designated it as exempt from further review.
Contributors All authors contributed to the design, data collection, writing, and article review. All authors have seen and approved the final version of the article.
Peer Reviewed
References
- 1.Wray N, Weiss T, Christian C, et al. The health status of veterans using mobile clinics in rural areas. J Health Care Poor Underserved. 1999;10:338–348. [DOI] [PubMed] [Google Scholar]
- 2.Auchincloss A, Hadden W. The health effects of rural–urban residence and concentrated poverty. J Rural Health. 2002;18:319–336. [DOI] [PubMed] [Google Scholar]
- 3.Blazer D, Landesman L, Fillenbaum G, Horner R. Health services access and use among older adults in North Carolina: urban vs rural residents. Am J Public Health. 1995;85:1384–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mainous A, Kohrs F. A comparison of health status between rural and urban adults. J Community Health. 1995;20:423–431. [DOI] [PubMed] [Google Scholar]
- 5.Erickson K, Mackenzie K, Marshall A. Advanced but expensive technology. Balancing affordability with access in rural areas. Can Fam Physician. 1993;39(1):29–34. [PMC free article] [PubMed] [Google Scholar]
- 6.Fakhoury W, Roos L. Access to and use of physician resources by the rural and urban populations in Manitoba. Can J Public Health. 1996;87:248–252. [PubMed] [Google Scholar]
- 7.Lambert D, Hartley D. Linking primary care and rural psychiatry: where have we been and where are we going? Psychiatr Serv. 1998;49:965–967. [DOI] [PubMed] [Google Scholar]
- 8.Horner R. Impact of federal primary health care policy in rural areas: empirical evidence from the literature. J Rural Health. 1988;4:13–28. [DOI] [PubMed] [Google Scholar]
- 9.Kukulka G, Christianson J, Moscovice I, DeVries R. Community-oriented primary care. Implementation of a national rural demonstration. Arch Fam Med. 1994;3:495–501. [DOI] [PubMed] [Google Scholar]
- 10.Connor R, Hillson S, Krawelski J. Competition, professional synergism, and the geographic distribution of rural physicians. Med Care. 1995;33:1067–1078. [DOI] [PubMed] [Google Scholar]
- 11.Scroeder S, Beachler M. Physician shortages in rural America. Lancet. 1995;345:1001–1002. [DOI] [PubMed] [Google Scholar]
- 12.Rabinowitz H, Diamond J, Markham F, Paynter N. Critical factors for designing programs to increase the supply and retention of rural primary care physicians. JAMA. 2001;286:1041–1048. [DOI] [PubMed] [Google Scholar]
- 13.Weeks W, Yano E, Rubenstein L. Primary care practice management in rural and urban Veterans Health Administration settings. J Rural Health. 2002;18:298–303. [DOI] [PubMed] [Google Scholar]
- 14.Wadsworth ME, Montgomery SM, Bartley MJ. The persisting effect of unemployment on health and social well-being in men early in working life. Soc Sci Med. 1999;48:1491–1499. [DOI] [PubMed] [Google Scholar]
- 15.Beck RW, Jijon CR, Edwards JB. The relationships among gender, perceived financial barriers to care, and health status in a rural population. J Rural Health. 1996;12:188–189. [DOI] [PubMed] [Google Scholar]
- 16.Leape LL, Hilborne LH, Bell R, Kamberg C, Brook RH. Underuse of cardiac procedures: do women, ethnic minorities, and the uninsured fail to receive needed revascularization? Ann Intern Med. 1999;130:183–192. [DOI] [PubMed] [Google Scholar]
- 17.Mirvis DM, Graney MJ. Variations in the use of cardiac procedures in the Veterans Health Administration. Am Heart J. 1999;137(4):706–713. [DOI] [PubMed] [Google Scholar]
- 18.Kazis L, Ren X, Skinner K, et al. Initial results from the 1999 large health survey of veteran en-rollees. Paper presented at: VA Health Services Research and Development 19th Annual Meeting; February 14–16, 2001; Washington, DC.
- 19.Ware J, Bayliss M, Rogers W, Kosinski M, Tarloy A. Differences in 4-year health outcomes for elderly and poor, chronically ill patients treated in HMO and fee-for-service systems. JAMA. 1996;176:1039–1047. [PubMed] [Google Scholar]
- 20.Perlin J, Kazis L, Skinner K, et al. Health Status and Outcomes of Veterans: Physical and Mental Component Summary Scores, Veterans SF-36, 1999 Large Health Survey of Veteran Enrollees. Washington, DC: Office of Quality and Performance, Veterans Health Administration, Department of Veterans Affairs; 2000.
- 21.Kazis L, Ren X, Lee A, et al. Health status in VA patients: results from the veterans health study. Am J Med Qual. 1999;14(1):28–37. [DOI] [PubMed] [Google Scholar]
- 22.Kazis L. The veterans SF-36 health status questionnaire: development and application in the Veterans Health Administration. Med Outcomes Trust Monitor. 2000;5:1. [Google Scholar]
- 23.Kazis L, Skinner K, Rogers W, et al. Health Status of Veterans: Physical and Mental Component Summary Scores (SF-36V). 1998 National Survey of Ambulatory Care Patients Mid-Year Executive Report. Washington, DC: Office of Performance and Quality, Veterans Health Administration; 1998.
- 24.1998 Cost Data. Austin, Tex: Allocation Resource Center, Department of Veterans Affairs; 1998.
- 25.Selim A, Fincke G, Ren X, et al. The comorbidity index. In: Goldfield N, Pine M, Pine J. Measuring and Managing Health Care Quality. Gaithersburg, Md: Aspen Publishers; 2002.
- 26.Rural Urban Commuting Area Code. Washington, DC: Economic Research Service of the US Department of Agriculture; 2001.
- 27.ZIP Code RUCA Approximation Methodology. Seattle, Wash: WWMAI Rural Health Research Center; 2004.
- 28.Weeks W, Bott D, Lamkin R, Wright S. Veterans Health Administration and Medicare outpatient health care utilization by older rural and urban New England veterans. J Rural Health. In press. [DOI] [PubMed]
- 29.Parkerson G, Broadhead W, Tse C. Health status and severity of illness as predictors of outcomes in primary care. Med Care. 1995;33:53–66. [DOI] [PubMed] [Google Scholar]
- 30.Wright S, Petersen L, Lamkin R, Daley J. Increasing use of Medicare services by veterans with acute myocardial infarction. Med Care. 1999;37:529–537. [DOI] [PubMed] [Google Scholar]
- 31.Bindman AB, Keane D, Lurie N. Measuring health changes among severely ill patients. The floor phenomenon. Med Care. 1990;28:1142–1152. [DOI] [PubMed] [Google Scholar]