Abstract
Objectives. We examined whether Mexican Americans living in high-density Mexican American neighborhoods experience increased morbidity and mortality compared with the rates observed among Mexican Americans living in low-density areas.
Methods. We conducted a prospective analysis of a cohort of 3050 Mexican Americans aged 65 years or older. We examined prevalence of 6 medical conditions and survival over 7 years of follow-up in relation to percentage of Mexican Americans in the census tract.
Results. With adjustment for covariates, odds for disease prevalence among older Mexican Americans as a function of percentage of Mexican Americans in the census tract were 0.33 (95% confidence interval [CI]=0.16, 0.71) for stroke, 0.28 (95% CI= 0.11, 0.70) for cancer, and 0.31 (95% CI=0.10, 0.98) for hip fracture. The hazard ratio for all-cause mortality over 7 years’ follow-up was 0.64 (95% CI=0.42, 0.96).
Conclusions. Sociocultural advantages conferred on Mexican Americans by living in high-density Mexican American neighborhoods outweigh the disadvantages conferred by the high poverty of those neighborhoods.
A growing body of research has examined the effects of neighborhood environments on individual health. These studies have sought to isolate the effects of communities rather than simply of the individuals that compose them. In other words, do neighborhood characteristics confer health risks or benefits on their residents, independent of the individual attributes of those residents? Numerous studies have reported a gradient effect of community socioeconomic status, with higher morbidity and mortality rates in economically disadvantaged neighborhoods.1–4 Similarly, several studies have reported negative health effects of neighborhoods with high concentrations of African Americans. Hypersegregation of African Americans is usually viewed as the product of the exclusion and avoidance that give rise to extreme concentrations of neighborhood poverty. Thus, discussions of racial segregation in US cities relate to discussions of the health effects of economically disadvantaged and unhealthful inner-city settings.5–8
In this study, we focused on ethnic concentration of Mexican Americans as an aspect of neighborhood structure that may affect the health and mortality of older Mexican Americans. At first glance, Mexican American barrios have much in common with inner-city concentrations of disadvantaged African Americans. Many Mexican Americans live in barrio neighborhoods in which the majority of their neighbors also are of Mexican origin. These neighborhoods typically experience very high rates of poverty due at least in part to the low levels of formal schooling and the unskilled manual and service occupations of many of their residents. Accordingly, in the social science literature about community differentiation, barrios are sometimes equated with African American ghettos as sites of neighborhood disadvantage.9–11
Despite their shared economic disadvantage, there are distinct differences between Mexican American neighborhoods and other high-poverty neighborhoods. Rates of labor force participation, intact family structures, home ownership, and residential stability are relatively high in many disadvantaged Mexican American neighborhoods.12–14 Community institutions and kinship support structures that span households remain intact.15 In addition, discrimination and racial avoidance play a smaller role in creating ethnic concentrations of Mexican Americans than in creating similar concentrations of African Americans.16
If pathways linking neighborhood disadvantage and elevated morbidity and mortality pass through the negative health-related effects of disorderly and threatening environments, then it is not clear whether neighborhood concentrations of Mexican Americans will be associated with the higher levels of morbidity and mortality that are commonly associated with disadvantaged neighborhoods. If the quality of social support from kinship and community is an important determinant of health,17,18 then Mexican Americans who live in barrio communities may experience health advantages relative to those in other neighborhood settings; this support may be stronger in these communities than in ethnically mixed environments where informal ethnic community structures are attenuated. These health advantages may be most salient to older persons, for whom social network support structures are an important component of successful adaptation to declining physical function.19–21
In this study, we examined the relationship between the percentage of neighborhood residents who are Mexican or Mexican American (hereafter “neighborhood percentage Mexican American”) and morbidity and mortality for a longitudinal study of a community-dwelling sample of older Mexican Americans. We use a file in which records for individual respondents have been linked to census data reporting the characteristics of neighborhood of residence at baseline. We examine the relationship of community ethnic composition to morbidity for 6 medical conditions and disability at baseline and to mortality during a 7-year follow-up period.
METHODS
Sample
The Hispanic Established Population for the Epidemiological Study of the Elderly (H-EPESE) is a panel study that examines the health status of older community-dwelling Mexican Americans (“Mexican American” denotes persons classified as Mexican on the US Census Hispanic-origin question, whether native or foreign-born). The initial wave of the survey was conducted during 1993/1994. There were 3 subsequent follow-up interviews, in 1995/1996, 1998/ 1999, and 2000/2001. The H-EPESE baseline cohort of 3050 older Mexican Americans (i.e., those aged 65 years or older) was selected from the 5 Southwestern states of Texas, California, Arizona, Colorado, and New Mexico, using a multistage area probability cluster sample that involved selection of counties, census tracts, census blocks, and households. In the first stage, counties were selected if at least 6.6% of the county population was of Mexican American ethnicity. In the second stage, census tracts in the listed counties were selected with probability proportional to the size of their older Mexican American population. In the third stage, census blocks were selected at random to obtain at least 400 households within each census tract. These households were screened to identify persons in the target population of older Mexican Americans. In-home interviews were conducted in Spanish or English at the option of the participant.22
The sampling procedure ensures a sample that is generalizable to the approximately 500 000 older Mexican Americans living in the Southwest. The 5 states in the H-EPESE sampling frame are home to 85% of the population of Mexican Americans aged 65 years and older living in the United States.
The response rate at baseline (1993/1994) was 83%. Among the 3050 baseline respondents, 329 could not be located at the third (7-year) follow-up (2000/2001). An additional 52 persons had missing responses on questions about medical conditions or disability at baseline. Analysis was restricted to the remaining 2669 respondents for whom medical and mortality information was complete.
Measures
Mortality.
Vital status was determined for a 7-year follow-up period after the 1993/1994 baseline interview. Vital status was ascertained by field information at the 3-, 5-, and 7-year follow-up interviews and through a search of death records for members of the H-EPESE cohort in the Social Security Administration Death Master File. Among the 2669 respondents, 878 were reported deceased at 7-year follow-up.
Morbidity and disability.
Data about the prevalence of 6 baseline medical conditions—stroke, cancer, heart attack, hip fracture, hypertension, and diabetes mellitus—were derived from self-report of a physician’s diagnosis. Respondents were coded as disabled at baseline if they reported limitations in 1 of 7 activities from a modified Katz Activities of Daily Living (ADL) scale: bathing, using the toilet, transferring from bed to chair, walking across a small room, personal grooming, dressing, and eating.23
Neighborhood characteristics.
Neighborhood characteristics were measured with data from the 1990 US Census for the 210 census tracts in which the respondents lived at baseline. The median population size of the tracts is 5885.24 Census tracts have been found to be a useful approximation of neighborhood environments in numerous studies of contextual influences on social behavior and health.25–27 Sample respondents have a high degree of residential stability. The median year in which respondents had moved into their current dwelling at the 1993/1994 baseline was 1974. Neighborhood percentage Mexican American was stratified into 5 categories for tabular presentation of baseline prevalence—0 to 29%, 30% to 49%, 50% to 69%, 70% to 89%, or 90% or more—and was scaled from 0 to 1 in regression and hazard models. Neighborhood socioeconomic status was operationalized as the percentage of persons living in households with income below poverty by the census definition28 and was scaled from 0 to 1.
Conditioning adjustments.
Multivariate models include adjustments for age, gender, marital status, highest school grade completed, household income, immigrant status (foreign vs US birth), and language of interview. Respondents were offered the choice to be interviewed in English or Spanish by bilingual interviewers. Choice of English for interview was used as an indicator of individual-level acculturation. Highest grade completed was categorized as 0 to 6 years, 7 to 11 years, or 12 years or more. Household income was dichotomized as less than $10 000 vs $10 000 or more. Respondents who were missing data on schooling and income were retained in the analysis, and missing status was entered as a category in all models.
Loss to Follow-up
To investigate the effects of loss to follow-up on the reported results, we estimated models in which respondents lost to follow-up were included in the analysis and censored when lost to follow-up. We reestimated models, this time excluding all respondents from the 3 primary sampling units with high rates and numbers of loss to follow-up, to address concerns that poor follow-up in these areas influenced estimates of the effects of tract characteristics. In none of these models did coefficients and significance levels of estimated parameters differ substantially from the reported models. We also examined correlates of loss to follow-up, because these losses indicate a possibly selective failure to observe deaths in the follow-up period. Tract percentage Mexican American was negatively but nonsignificantly associated with loss to follow-up (odds ratio [OR]=0.58; 95% confidence interval [CI]=0.24, 1.53). The higher rate of follow-up with increasing tract percentage Mexican American and tract poverty is compatible with other evidence that both variables are correlated with residential stability. Median years at address for persons in the highest quartile of tract percentage Mexican American at baseline was 23 years, compared with 19 years for persons in the lowest quartile. These patterns suggest that it is unlikely that reported findings are an artifact of selectively high loss to follow-up from tracts with a high percentage of Mexican American residents.
Analysis
We gathered baseline morbidity and 7-year mortality data for the H-EPESE cohort. First, we determined percentages of respondents who reported a diagnosis of each of the 6 medical conditions of interest and 1 or more activity limitations, stratified by neighborhood percentage Mexican American, together with coefficients from logistic regression models relating increasing neighborhood percentage Mexican American (scaled 0 to 1) to baseline prevalence for each condition, with adjustments for age and gender. Second, we estimated hazard ratios from Cox proportional hazards models for the impact of neighborhood percentage Mexican American on 7-year mortality, with adjustment for demographic, medical condition, and disability covariates. All models were estimated with Stata (Stata Corp, College Station, Tex), with robust estimation of variance to adjust for tract-level clustering of outcomes. Baseline characteristics and odds ratios were estimated with sample weights to reflect population prevalence.
RESULTS
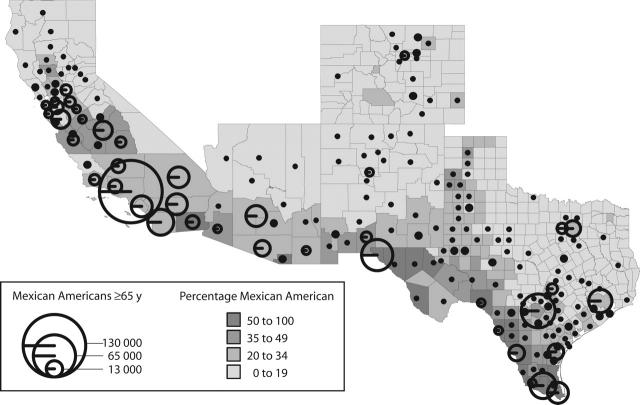
Older Mexican Americans in the 5 Southwestern states live in environments in which Mexican Americans form a majority of the population at both a neighborhood and county level. This concentration especially occurs in areas that are in close proximity to the United States–Mexico border (Figure 1 ▶). Among H-EPESE respondents, 29% live within 50 miles of a port of entry on the border, and 70% live within 150 miles of such a port. Mexican Americans form an especially large share of local populations in the Texas border region.
FIGURE 1—
Number of Mexican Americans aged 65 years and older and percentage of population Mexican American, by county, in 5 Southwestern states. Note. Circles represent the size, scaled by square root, of the Mexican American population aged 65 years and older, in each county. Shading represents the percentage of all county residents of all ages who are of Mexican origin. Source. US Bureau of the Census.24
Table 1 ▶ shows demographic characteristics of the sample at baseline across the 5 strata of neighborhood percentage Mexican American. There are no significant differences among neighborhoods in age, gender, marital status, or immigration status of older Mexican Americans. There are significant differences among neighborhood environments in choice of English-language interview, education, household income, and neighborhood poverty rates. Older Mexican Americans with a low percentage of Mexican American neighbors were most likely to choose an English-language interview and had the highest average levels of formal schooling, although both years of schooling and choice of English for the interview were low in all neighborhoods.
TABLE 1—
Demographic Characteristics of H-EPESE Respondents, by Mexican American Population Share in Local Environment
| Neighborhood Percentage Mexican American | ||||||
| Characteristic | 0–29 | 30–49 | 50–69 | 70–89 | 90–100 | Pa |
| Age at baseline, % | ||||||
| 65–74 y | 60.3 | 67.2 | 68.5 | 63.6 | 68.4 | . . . |
| 75–84 y | 34.0 | 23.4 | 25.9 | 28.7 | 26.0 | 0.548 |
| ≥ 85 y | 5.7 | 9.4 | 5.6 | 7.7 | 5.7 | 0.285 |
| Female, % | 40.9 | 41.9 | 46.0 | 42.5 | 44.3 | 0.366 |
| Married, % | 58.6 | 52.6 | 55.6 | 52.7 | 61.5 | 0.622 |
| Immigrant, % | 44.2 | 46.1 | 47.1 | 47.0 | 50.2 | 0.454 |
| English-language interview, % | 38.2 | 24.8 | 30.0 | 19.7 | 18.5 | 0.000 |
| Years of schooling, % | ||||||
| 0–6 | 62.3 | 63.8 | 69.8 | 74.0 | 76.9 | . . . |
| 7–11 | 23.6 | 19.9 | 18.8 | 14.3 | 12.2 | 0.011 |
| ≥ 12 | 11.2 | 14.2 | 10.3 | 9.4 | 9.9 | 0.095 |
| Schooling not reported, % | 2.9 | 2.1 | 1.1 | 2.2 | 1.0 | 0.129 |
| Annual household income, % | ||||||
| < $10 000 | 30.1 | 41.4 | 41.7 | 49.8 | 59.8 | . . . |
| ≥ $10 000 | 60.6 | 44.7 | 45.2 | 37.1 | 35.9 | 0.009 |
| Income not reported, % | 9.3 | 13.9 | 13.1 | 13.1 | 4.3 | 0.038 |
| Mean tract poverty rate | 14.3 | 20.8 | 29.5 | 35.2 | 45.6 | 0.000 |
| n (unweighted) | 105 | 363 | 433 | 1014 | 754 | . . . |
Note. H-EPESE = Hispanic Established Population for the Epidemiological Study of the Elderly.
a The final column reports significance values for coefficient for trend of the value for each characteristic as it varies with percentage Mexican American residing in the census tract of the H-EPESE subject. Significance values are from logistic regression (female, married, immigrant, English-language interview), multinomial logistic regression (age, schooling, income), or ordinary least squares regression (tract poverty rate) models.
Table 2 ▶ shows baseline prevalence of 6 medical conditions, disability, and 7-year mortality among older Mexican Americans as a function of the proportion of Mexican Americans in their neighborhoods. Also shown are the odds ratios for each condition as a function of neighborhood percentage Mexican American, with adjustment for age and gender composition. There is a broad and generally monotonic trend for increasing percentage of Mexican Americans in neighborhoods to be associated with decreasing prevalence of several of the medical conditions as well as with decreasing 7-year mortality. The linear trend relating increased neighborhood percentage Mexican American and lower disease prevalence is statistically significant for stroke, cancer, and hip fracture. The only condition for which there is increasing prevalence with increasing neighborhood percentage Mexican American is diabetes, although the coefficient is not statistically significant.
TABLE 2—
Baseline Prevalence of 6 Medical Conditions, Disability, and 7-Year Mortality by Mexican American Population Share in Local Environments
| Neighborhood Percentage Mexican American | |||||||
| 0–29 | 30–49 | 50–69 | 70–89 | 90–100 | OR (95% CI) for Condition With Increasing Neighborhood Percentage Mexican Americana | Pa | |
| Percentage reporting medical condition | |||||||
| Stroke | 11.5 | 9.5 | 6.6 | 5.9 | 5.2 | 0.33 (0.16, 0.71) | 0.005 |
| Cancer | 11.1 | 8.9 | 7.1 | 5.9 | 3.2 | 0.28 (0.11, 0.70) | 0.008 |
| Heart attack | 12.4 | 12.9 | 11.0 | 10.7 | 10.0 | 0.82 (0.38, 1.76) | 0.602 |
| Hip fracture | 6.1 | 5.5 | 5.2 | 2.8 | 2.4 | 0.31 (0.10, 0.98) | 0.046 |
| Hypertension | 58.1 | 44.0 | 45.4 | 46.3 | 37.9 | 0.84 (0.49, 1.44) | 0.521 |
| Diabetes mellitus | 26.2 | 26.1 | 24.6 | 30.3 | 26.1 | 1.24 (0.70, 2.23) | 0.460 |
| Percentage reporting disability | 19.5 | 14.8 | 12.4 | 16.0 | 11.7 | 0.70 (0.32, 1.50) | 0.353 |
| 7-year mortality rate | 38.1 | 37.1 | 32.6 | 34.0 | 28.9 | 0.60 (0.38, 0.94) | 0.026 |
Note. OR = odds ratio; CI = confidence interval.
aThe final columns report ORs, CIs, and significance from a logistic regression model associating increasing neighborhood percentage Mexican American and each condition, adjusted for age and gender. Neighborhood percentage Mexican American is scaled continuously from 0 to 1 in the regression model.
Table 3 ▶ shows the relationship of neighborhood percentage Mexican American and hazard of death during the 7 years of follow-up. Model 1 shows a statistically significant trend between increasing neighborhood percentage Mexican American and lower age- and gender-adjusted mortality. Model 2 further adjusts for baseline health status with respect to demographic characteristics, medical conditions, and disability at baseline. With these adjustments, the mortality advantage associated with increasing neighborhood percentage Mexican American increases from 0.71 to 0.64. This parameter implies that the ratio of the hazard for 7-year all-cause mortality among older Mexican Americans living in census tracts with a 100% concentration of Mexican American residents to that among older Mexican Americans living in census tracts with a 0% concentration of Mexican Americans is 0.64, with adjustment for covariates.
TABLE 3—
Hazard Ratios and 95% Confidence Intervals (CIs) for 7-Year All-Cause Mortality as a Function of Increasing Neighborhood Percentage Mexican American and Covariatesa
| Variable | Model 1 Hazard Ratio (95% CI) | P | Model 2 Hazard Ratio (95% CI) | P |
| Neighborhood percentage Mexican American (0–1) | 0.71 (0.53, 0.95) | 0.023 | 0.64 (0.42, 0.96) | 0.033 |
| Age (vs 65–74 y) | ||||
| 75–84 y | 2.03 (1.75, 2.38) | 0.000 | 1.85 (1.57, 2.17) | 0.000 |
| ≥ 85 y | 4.59 (3.88, 5.43) | 0.000 | 3.41 (2.74, 4.24) | 0.000 |
| Female | 0.68 (0.60, 0.79) | 0.000 | 0.60 (0.52, 0.69) | 0.000 |
| Married | . . . | . . . | 0.95 (0.81, 1.12) | 0.557 |
| Years of schooling (vs 0–6 y) | ||||
| 7–11 y | . . . | . . . | 1.02 (0.85, 1.23) | 0.804 |
| ≥ 12 y | . . . | . . . | 1.03 (0.81, 1.32) | 0.802 |
| Schooling not reported | . . . | . . . | 1.45 (0.92, 2.28) | 0.110 |
| Annual household income (vs < $10 000) | ||||
| ≥ $10 000 | . . . | . . . | 0.89 (0.77, 1.03) | 0.122 |
| Income not reported | . . . | . . . | 1.15 (0.03, 1.41) | 0.193 |
| Immigrant (vs native) | . . . | . . . | 0.95 (0.84, 1.07) | 0.398 |
| English-language interview | . . . | . . . | 0.93 (0.78, 1.11) | 0.424 |
| Neighborhood percentage poor (0–1) | . . . | . . . | 1.46 (0.75, 2.86) | 0.266 |
| Medical condition | ||||
| Stroke | . . . | . . . | 1.11 (0.89, 1.38) | 0.363 |
| Cancer | . . . | . . . | 1.95 (1.47, 2.57) | 0.000 |
| Heart attack | . . . | . . . | 1.16 (0.96, 1.41) | 0.133 |
| Hip fracture | . . . | . . . | 1.33 (0.99, 1.79) | 0.056 |
| Hypertension | . . . | . . . | 1.14 (1.00, 1.31) | 0.049 |
| Diabetes mellitus | . . . | . . . | 1.61 (1.41, 1.85) | 0.000 |
| Disability | . . . | . . . | 2.06 (1.73, 2.47) | 0.000 |
| Log likelihood | −6672.1037 | . . . | −6632.1235 | . . . |
| χ2 (df) | 356.42 (4) | . . . | 624.79 (20) | . . . |
a This table reports hazard ratios, CIs, and significances from Cox proportional hazards models associating neighborhood percentage Mexican American and 7-year mortality. Neighborhood percentage Mexican American and neighborhood percentage poor are continuously scaled from 0 to 1.
DISCUSSION
Mexican Americans have lower mortality rates than non-Hispanic Whites for several of the top 10 causes of death, which leads to overall lower disease-related mortality in Hispanics compared with non-Hispanic Whites.31,32 This mortality advantage for a population with low socioeconomic status has been called the “Hispanic paradox.”33 Data from the H-EPESE show that this advantage has a sociospatial dimension for older Mexican Americans: morbidity and mortality are lowest in neighborhoods with high proportions of Mexican Americans and are greatest in neighborhoods where Mexican Americans are most integrated with non-Hispanics.
The “barrio advantage” appears to contradict the thesis of negative health effects of neighborhood disadvantage. Our results suggest that for older Mexican Americans, the negative effects of neighborhood poverty are counterbalanced by positive effects associated with living among a high density of Mexican Americans. The limited negative effect of neighborhood poverty and apparent protective effects of ethnic concentration in neighborhoods for Mexican Americans are consistent with several recent reports from multiethnic studies for a variety of health outcomes and behaviors.34–37
Debates about the Hispanic paradox have focused on competing hypotheses concerning the protective effects of Mexican and other Hispanic cultures versus patterns of immigration and return migration that select for better health status.38 Hypothesized protective effects of Mexican culture include a lower prevalence of smoking, drinking, and recreational drug use in some Mexican American subpopulations; superior nutrition among less-assimilated Mexican Americans; lower levels of socially induced stress and psychiatric morbidity; and higher levels of social support.39–44
With respect to each of these mechanisms, it is likely that the transmission of culture has a spatial dimension in which ethnic concentration effects operate. The map presented in Figure 1 ▶ illustrates that a large number of older Mexican Americans continue to live in Southwestern environments in which Mexican cultural influences are extremely strong. If there are unhealthful aspects of the US culture associated with harried lifestyles, consumption of fast food, and atomistic social relationships, many Mexican Americans in the Southwest may be buffered from the full effects by continued immersion in special sociocultural environments. The older Mexican Americans represented in the H-EPESE data may benefit in particular from stronger social support in the face of declining physical functioning.
One limitation of the study is that the baseline data were collected for a population aged 65 years and older. In such data sets, it is always possible that the study cohort is selected for relatively good health. One selection mechanism concerns the possibility that some older Mexican American immigrants may return to Mexico and that their deaths are not recorded in data sets and the vital registration system of the United States.29,30,38 With respect to the current study, such outmigration—either before or after baseline—could produce the false appearance of a protective effect of residence in a high-percentage Mexican American neighborhood if return migration to Mexico is correlated with the onset of illness and is more likely to occur in neighborhoods with a high concentration of Mexican Americans.
Critical to evaluating this concern is the fact that high neighborhood concentration of Mexican Americans does not occur only or primarily in immigrant barrios. The Southwest border region, particularly Texas and New Mexico, is home to many concentrated Mexican American communities of long standing. “Return” migration to Mexico is not an option for the predominantly US-born population of these communities. There are also several indications in the H-EPESE data that the bias produced by return migration is small. First, immigrant status is not strongly correlated with tract percentage Mexican American (r=.02). Second, there is no indication of substantial return migration to Mexico after baseline. Third, loss to follow-up, a possible indicator of unobserved emigration, is negatively and nonsignificantly correlated with tract percentage Mexican American. Finally, there are no significant interactions between US versus Mexican birth and reported results. The hazard ratio for tract percentage Mexican American among US-born respondents was 0.65 (95% CI=0.37, 1.13), compared with 0.64 for the full sample, and the associations between tract percentage Mexican American and lower prevalence rates for cancer, stroke, and hip fracture were strongest for the US-born.
Another possible selection effect concerns the possibility of higher rates of mortality before baseline in high-percentage Mexican American neighborhoods. The presence of such effects is made more credible when it is noted that neighborhoods with the highest percentage of Mexican Americans in the H-EPESE sample occur in impoverished communities close to the Texas–Mexico border with significant deficits in sanitation and medical services.45,46 Neighborhood differences may also be partially explained by genetic differences in the Mexican American population living in different places. The San Antonio Heart Study, for example, reported that American Indian genetic admixture varied by neighborhood type, with the highest representation in homogenous barrios and the lowest in more integrated, high-socioeconomic-status suburban communities.47,48 Both of these issues merit further attention to gain a full understanding of both the barrio advantage and the epidemiological Hispanic paradox.
Our findings suggest the need for investigation of the relationship between community characteristics and health for Mexican Americans and other immigrant and ethnic communities. The findings generalize immediately to the older Mexican American population in the Southwest. It remains to be explored whether the same effects will be found for younger populations, for more recent immigrants, and across a broader spectrum of social class contexts than those experienced by the members of the H-EPESE cohort. Similarly, it will be useful to investigate whether the neighborhood concentration effects reported here are associated with the environments of Mexican American numerical predominance in the immediate border region, or whether they also occur in interior cities where Mexican American populations form a smaller fraction of local populations.
The influence of diversity in community environments on health may become increasingly important for Mexican Americans because of the increasing dispersal of Mexican Americans outside the Southwestern states, in which this population has historically been concentrated. In conducting studies of the influence of such contextual variation on health, it is important to broaden investigation beyond the effects of neighborhood economic characteristics that have been the focus of most research on contextual effects. The mechanisms linking neighborhood disadvantage to poorer health outcomes remain an important area for research. However, some ethnic communities may possess advantages associated with the maintenance of favorable health-related behaviors, social cohesion, and social support mechanisms that offset negative effects of low economic standing and poor material amenities.
Acknowledgments
This research was supported by the National Institute on Aging (grants AG10939-10, AG00270-04, and F31 AG021872-01).
Human Participant Protection
Study protocols were approved by the institutional review board of the University of Texas Medical Branch at Galveston.
Contributors All of the authors contributed to the study design, data analysis, and writing of the article.
Peer Reviewed
References
- 1.Haan M, Kaplan G, Camacho T. Poverty and health. Prospective evidence from the Alameda County Study. Am J Epidemiol. 1987;125:989–998. [DOI] [PubMed] [Google Scholar]
- 2.Anderson RT, Sorlie P, Backlund E, Johnson N, Kaplan GA. Mortality effects of community socioeconomic status. Epidemiology. 1997;8:42–47. [DOI] [PubMed] [Google Scholar]
- 3.Pickett KE, Pearl M. Multilevel analyses of neighborhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001; 55:111–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary artery disease. N Engl J Med. 2001;345:99–106. [DOI] [PubMed] [Google Scholar]
- 5.Massey DS, Gross AB, Eggers ML. Segregation, the concentration of poverty and the life chances of individuals. Soc Sci Res. 1991;20:397–420. [Google Scholar]
- 6.Polednak AP.Segregation, discrimination and mortality in US Blacks. Ethn Dis. 1996;6:99–108. [PubMed] [Google Scholar]
- 7.Jackson SA, Anderson RT, Johnson NJ, Sorlie PD. The relation of residential segregation to all-cause mortality: a study in black and white. Am J Public Health. 2000;90:615–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McLaughlin DK, Stokes CS. Income inequality and mortality in US counties: does minority racial concentration matter? Am J Public Health. 2002;92:99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glazer N, Moynihan DP. Beyond the Melting Pot: The Negroes, Puerto Ricans, Jews, Italians, and Irish of New York City. Cambridge, Mass: MIT Press; 1963.
- 10.Lewis O. La Vida: A Puerto Rican Family in the Culture of Poverty—San Juan and New York. New York, NY: Random House; 1966.
- 11.Jargowsky PA. Poverty and Place: Ghettos, Barrios, and the American City. New York, NY: Russell Sage Foundation; 1997.
- 12.James F. Persistent Urban Poverty and the Under-class: A Perspective Based on the Hispanic Experience. Claremont, Calif: Tomás Rivera Policy Institute; 1988.
- 13.Moore J.Is there an Hispanic underclass? Soc Sci Q. 1989;70:265–283. [Google Scholar]
- 14.Moore J, Pinderhughes R, eds. In the Barrios: Latinos and the Underclass Debate. New York, NY: Russell Sage Foundation; 1993.
- 15.Vélez-Ibáñez C.US Mexicans in the borderlands: being poor without the underclass. In: Moore J, Pinderhughes R, eds. In the Barrios: Latinos and the Under-class Debate. New York, NY: Russell Sage Foundation; 1993:195–210.
- 16.Massey DM, Mullen BP. Processes of Hispanic and Black spatial assimilation. Am J Sociol. 1984;89:836–873. [Google Scholar]
- 17.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. [DOI] [PubMed] [Google Scholar]
- 18.Seeman T. Social ties and health: the benefits of social integration. Ann Epidemiol. 1996;6:442–451. [DOI] [PubMed] [Google Scholar]
- 19.Lawton MP. Competence, environmental press, and the adaptation of older people. In: Lawton MP, Windley PG, Byerts TO, eds. Aging and the Environment: Theoretical Approaches. New York, NY: Springer Publishing; 1982:33–39.
- 20.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. [DOI] [PubMed] [Google Scholar]
- 21.Mendes de Leon CF, Glass TA, Beckett LA, Seeman TE, Evans DA, Berkman LF. Social networks and disability transitions across eight intervals of yearly data in the New Haven EPESE. J Gerontol B Psychol Sci Soc Sci. 1999;54:S162–S172. [DOI] [PubMed] [Google Scholar]
- 22.Markides KS, Rudkin L, Angel RJ, Espino DV. Health status of Hispanic elderly. In: Martin LG, Soldo BJ, eds. Racial and Ethnic Differences in the Health of Older Americans. Washington, DC: National Academy Press; 1997:285–300. [PubMed]
- 23.Branch LG, Katz S, Kniepmann K. A prospective study of functional status among community elders. Am J Public Health. 1984;74:266–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.US Bureau of the Census. Census 2000 Summary File 2 (SF 2). Washington, DC: US Bureau of the Census; 2001.
- 25.Ricketts ER, Sawhill IV. Defining and measuring the underclass. J Policy Anal Manage. 1988;7:316–325. [Google Scholar]
- 26.South SJ, Crowder KD. Escaping distressed neighborhoods: individual, community, and metropolitan influences. Am J Sociol. 1997;102:1040–1084. [Google Scholar]
- 27.Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42:258–276. [PubMed] [Google Scholar]
- 28.US Bureau of the Census. Current Population Reports: Poverty in the United States, 1999. Washington, DC: US Bureau of the Census; 2000.
- 29.Rosenwaike I. Mortality of Hispanic Populations: Mexicans, Puerto Ricans and Cubans in the United States and in the Home Countries. New York, NY: Greenwood Press; 1991.
- 30.Sorlie PD, Backlund E, Johnson NJ, Rogot E. Mortality by Hispanic status in the United States. JAMA. 1993;270:2464–2468. [PubMed] [Google Scholar]
- 31.Markides K, Coreil J. The health of Southwestern Hispanics: an epidemiological paradox. Public Health Rep. 1986;101:253–265. [PMC free article] [PubMed] [Google Scholar]
- 32.Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. J Health Soc Behav. 1996;37:293–310. [PubMed] [Google Scholar]
- 33.LeClere F, Rogers RG, Peters KD. Ethnicity and mortality in the United States: individual and community correlates. Soc Forces. 1997;76:169–198. [Google Scholar]
- 34.Pearl M, Braverman P, Abrams B. The relationship of neighborhood socioeconomic characteristics to birth-weight among 5 ethnic groups in California. Am J Public Health. 2001;91:1808–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee RE, Cubbin C. Neighborhood context and youth cardiovascular health behaviors. Am J Public Health. 2002;92:428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palloni A, Morenoff JD. Interpreting the paradoxical in the Hispanic paradox: demographic and epidemiologic approaches. Ann N Y Acad Sci. 2001;954:140–174. [DOI] [PubMed] [Google Scholar]
- 37.Coreil J, Markides KS, Ray LA. Predictors of smoking among Mexican Americans: findings from the Hispanic HANES. Prev Med. 1991;20:508–517. [DOI] [PubMed] [Google Scholar]
- 38.Balcazar H, Castro FG, Krull JL. Cancer risk reduction in Mexican American women: the role of acculturation, education and health risk factors. Health Educ Q. 1995;22:61–84. [DOI] [PubMed] [Google Scholar]
- 39.Aranda MP, Miranda MR. Hispanic aging, social support, and mental health: does acculturation make a difference? In: Markides KS, Miranda MR, eds. Minorities, Aging and Health. Thousand Oaks, Calif: Sage Publications; 1997:271–294.
- 40.Guendelman S, Abrams B. Dietary intake among Mexican American women: generational differences and a comparison with white non-Hispanic women. Am J Public Health. 1995;85:20–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hazuda HP, Espino DV. Aging, chronic disease, and physical disability in Hispanic elderly. In: Markides KS, Miranda MR, eds. Minorities, Aging and Health. Thousand Oaks, Calif: Sage Publications; 1997:127–148.
- 42.Escobar J, Hoyos Nervi C, Gara MA. Immigration and mental health: Mexican Americans in the United States. Harv Rev Psychiatry. 2000;8:64–72. [PubMed] [Google Scholar]
- 43.Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89:1543–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11:496–518. [PubMed] [Google Scholar]
- 45.Ward PM. Colonias and Public Policy in Texas and Mexico: Urbanization by Stealth. Austin, Tex: University of Texas Press; 1999.
- 46.Patel KV, Eschbach K, Rudkin LL, Peek MK, Markides KS. Neighborhood context and self-rated health in older Mexican Americans. Ann Epidemiol. 2003;13:620–628. [DOI] [PubMed] [Google Scholar]
- 47.Gardner LI Jr, Stern MP, Haffner SM, et al. Prevalence of diabetes in Mexican Americans. Relationship to percent of gene pool derived from native American sources. Diabetes. 1984;33:86–92. [DOI] [PubMed] [Google Scholar]
- 48.Diehl AK, Stern MP. Special health problems of Mexican Americans: obesity, gallbladder disease, diabetes mellitus, and cardiovascular disease. Adv Intern Med. 1989;34:73–96. [PubMed] [Google Scholar]