Abstract
Objective. We explored methods and potential applications of a systematic approach to studying and monitoring social disparities in health and health care.
Methods. Using delayed or no prenatal care as an example indicator, we (1) categorized women into groups with different levels of underlying social advantage; (2) described and graphically displayed rates of the indicator and relative group size for each social group; (3) identified and measured disparities, calculating relative risks and rate differences to compare each group with its a priori most-advantaged counterpart; (4) examined changes in rates and disparities over time; and (5) conducted multivariate analyses for the overall sample and “at-risk” groups to identify particular factors warranting attention.
Results. We identified at-risk groups and relevant factors and suggest ways to direct efforts for reducing prenatal care disparities.
Conclusions. This systematic approach should be useful for studying and monitoring disparities in other indicators of health and health care.
With this article, we propose an approach to studying and monitoring social disparities in health and health care, using prenatal care as an example. We use the term “social disparities in health” broadly here to refer to differences in health—or likely determinants of health—that are systematically1,2 associated with different levels of underlying social advantage or position in a social hierarchy.3 Social advantage or position is reflected by economic resources, occupation, education, racial/ethnic group, gender, sexual orientation, and other characteristics associated with greater resources, influence, prestige, and social inclusion.3–7
Social disparities in health place people already disadvantaged by belonging to particular social groups at further disadvantage with respect to their health3,8,9; good health in turn is essential to escape from social disadvantage.9–11 Efforts to reduce social disparities in health and equalize opportunities for optimal health reflect social and ethical values,8,12 including solidarity or compassion8,13 and distributive justice,13 and are consonant with human rights principles.3,13,14 The goals of Healthy People 2010 include eliminating social disparities in health and health care.15
Social disparities in health, including gaps in maternal and child health and health care, are large and persistent in the United States.16–39 There is widespread recognition that closing these gaps will require more effective strategies, including monitoring and research to guide and evaluate policies.5,40–48 However, apart from racial/ethnic breakdowns of vital statistics, routine monitoring of social disparities in health in the United States has generally been limited.40,41,49–51 This article was based on work supported by the Centers for Disease Control and Prevention and the Kaiser Family Foundation that examined socioeconomic and racial/ethnic disparities in 3 maternal and infant health indicators—unintended pregnancy, breastfeeding, and delayed or no prenatal care—in California during 1994–1995 and 1999–2001. A separate report52 on that work, aimed at a wide nontechnical audience, highlights issues that policies should address. The focus of our article is primarily methodological, aiming to illustrate a systematic approach for studying and monitoring disparities that can be adapted for other indicators and populations. Space constraints limit us here to using 1 indicator—delayed or no prenatal care—as an example. Although the ideal content and number of prenatal visits are unknown,53,54 few would contest the importance of at least 1 first-trimester visit for timely assessment and health promotion.55–57 Healthy People 2010 objectives15 include first-trimester care for at least 90% of childbearing women.
METHODS
Data Sources
We used cross-sectional data from 2 California statewide representative postpartum surveys, with approval from the University of California, San Francisco committee on human research and the California Health and Human Services Agency committee for the protection of human subjects. The 1999–2001 data (n=10519) were obtained from the Maternal and Infant Health Assessment (MIHA). A collaborative effort of the California Department of Health Services Maternal and Child Health Branch and University of California, San Francisco, modeled on the Centers for Disease Control and Prevention’s Pregnancy Risk Assessment Monitoring System,58 MIHA is an annual population-based mail survey (with telephone follow-up of nonresponders) of mothers a few months after they give birth to live-born infants in California. Data for 1994 and 1995 were obtained from the Access to Maternity Care (ATM) survey, in which 10132 mothers of live-born infants were interviewed during their postpartum stays in 19 randomly selected California hospitals. The ATM survey was conducted with support from the Agency for Health Care Policy Research, the California Department of Health Services, and the Robert Wood Johnson Foundation. Both surveys were linked with birth certificates and with census data from 2000 (MIHA) or 1990 (ATM). Residential addresses from birth certificates were geocoded to the census tract level (approximately 4000–8000 people per tract) using MapMarker Plus software59 for MIHA and services from Geographic Data Technology, Inc. (Lebanon, NH), for ATM. Both procedures use several reliable and regularly updated sources of address files (e.g., US Postal Service, Census TIGER files),60 and geocoding was successful for 97.4% of addresses in MIHA and 83.8% (87.3% after excluding 1 hospital without linked birth certificates) in ATM. Both statistically weighted samples were similar to the statewide maternity populations during corresponding time periods. MIHA and ATM response rates were 71% and 86%, respectively. Methods for both surveys have been described elsewhere.29,61,62
Variables
The indicator of health and health care used as an example was delayed or no care, which was defined as either beginning prenatal care after the first trimester or receiving no prenatal care during the index pregnancy. Social groups were defined according to (1) 3 socioeconomic variables (i.e., family income, maternal education, and neighborhood poverty), chosen a priori to categorize the sample into groups reflecting different dimensions of socioeconomic status or position plausibly related to delayed or no care28,56,61,63–65; and (2) race/ethnicity.
Family income.
Family income was defined as the self-reported family income during pregnancy in 100% increments of the federal poverty level for the relevant year (e.g., $17 650 for a family of 4 in 2001). Income of the nuclear family (the woman, her partner, and dependent children) was used instead of household income to conform with eligibility criteria for Medi-Cal and other programs that could influence prenatal care use.
Maternal education.
Maternal education was defined as the respondent’s self-reported highest completed educational level (i.e., did not complete high school, high-school graduate, some college, college graduate).
Neighborhood poverty.
The definition of neighborhood poverty was based on women’s residences at the index birth, defining a “poor” neighborhood as a census tract with at least 20% of persons below the federal poverty level66 in 1990 (ATM) or 2000 (MIHA). We used census tracts rather than smaller block groups because tracts generally geocode at a higher rate and are simpler to use; previous studies have found similar results using tracts or block groups to define neighborhoods.67–69 Although multiple characteristics of neighborhoods ideally should be examined,28,70–72 for brevity we examined only poverty concentration, which has been widely used68,73–78 and is easily understood by policymakers. Sample size constraints (e.g., few women in the highest income or education categories lived in “poor” neighborhoods) limited us to 2 poverty concentration categories; the 20% cutoff reflects the US Census Bureau definition of “poverty area”79 and is supported by previous studies.73–76
Race/ethnicity.
Self-reported racial/ethnic identification was categorized as African American, Asian/Pacific Islander, European American (including women from the Middle East), immigrant Latina, US-born Latina, or Native American/Alaska Native. Small numbers precluded separate multivariate analyses for Native Americans and categorizing non-Latina women by nativity.
Other covariates in 1999–2001 MIHA data were chosen on the basis of the literature56,63,65,80,81 as being plausibly associated with delayed or no care, either as confounders or as mediators on pathways between social factors and prenatal care: paternal education, maternal first-trimester insurance coverage,81 age, parity, marital status at the time of birth, primary language spoken at home, having a regular source of health care before pregnancy, whether the respondent felt her receipt of prenatal care was “very important” to others close to her, unintended pregnancy, initial unhappiness about the pregnancy, the respondent’s general “sense of control” over her life (“mastery”),82 and both smoking and drinking during pregnancy (as markers of general knowledge, attitudes, or beliefs that could influence use of care).
Statistical Analyses
Describing social disparities in prenatal care.
After categorizing women in each time period into social groups defined by family income, education, neighborhood poverty, and race/ethnicity, we estimated rates of delayed or no care in each group and calculated rate differences and relative risks for each group compared with the a priori most-advantaged corresponding group (Table 1 ▶). For example, each of the 4 lower income groups was compared with the highest income group. Because both risk levels and relative size of groups are relevant, we further examined disparities by income and education in 2 ways: (1) using bar graphs, with bar width reflecting the proportion of the population in each group (suggested to us by work published by Wagstaff et al.83; this approach was used by Krieger and colleagues in 200268); and (2) estimating 2 “summary (composite) measures”—the population-attributable risk and the relative index of inequality83–85 (defined in Table 1 ▶ footnotes). Comparing 1994–1995 and 1999–2001, we examined changes between the 2 periods in the group-specific rates of delayed or no care, the sizes of the disparities, and the socioeconomic distributions.
TABLE 1—
Rates, Rate Differences, and Relative Risks of Delayed or No Care, by Income, Education, Race/Ethnicity, and Neighborhood Poverty, and Summary Measures of Socioeconomic Disparities: Postpartum Women Surveyed in California, 1994–1995 and 1999–2001
| % of Total | % Delayed or No Care | 95 % CI | Rate Difference | Relative Risk | 95 % CI | PAR%a | RIIb | |
| 1994–1995 (n = 10 132)c | ||||||||
| % of federal poverty level | ||||||||
| Missing | 3.2 | 25.0 | (14.2, 35.8) | 21.2 | 6.6 | (2.5, 17.2)* | ||
| 0–100 | 44.9 | 37.5d | (34.4, 40.6)d | 33.7d | 9.9 | (5.6, 17.5)* | ||
| 101–200 | 18.1 | 17.9 | (13.4, 22.4) | 14.1 | 4.7 | (2.1, 10.6)* | 77.06 | −2.03 |
| 201–300 | 11.9 | 11.8 | (9.4, 14.2) | 8.0 | 3.1 | (1.6, 5.9)* | ||
| 301–400 | 8.6 | 8.1 | (3.0, 13.2) | 4.3 | 2.1 | (0.6, 7.4) | ||
| ≥401 | 13.2 | 3.8 | (1.8, 5.8) | 1.0 | ||||
| 100.0 | ||||||||
| Maternal educatione (completed level) | ||||||||
| < High school | 30.0 | 38.0d | (32.9, 43.1)d | 31.5d | 5.8 | (3.8, 8.9)* | ||
| High school graduate/GED | 31.3 | 24.4 | (20.5, 28.3) | 17.9 | 3.7 | (2.7, 5.2)* | ||
| Some college | 23.9 | 14.6 | (10.3, 18.9) | 8.1 | 2.2 | (1.2, 4.1)* | 72.22 | −1.69 |
| College graduate | 14.8 | 6.5 | ( 3.8, 9.2) | 1.0 | ||||
| 100.0 | ||||||||
| Neighborhood poverty | ||||||||
| Missing | 18.2 | 22.2 | (10.6, 25.9) | 2.0 | 1.2 | (0.7, 2.0) | ||
| ≥20% poor | 22.7 | 31.6d | (27.9, 35.3)d | 11.4d | 1.6 | (1.4, 1.7)* | ||
| < 20% poor | 59.2 | 20.2 | (17.1, 23.3) | 1.0 | ||||
| 100.0 | ||||||||
| Race/ethnicity f | ||||||||
| African American | 6.8 | 21.6 | (15.7, 27.5) | 6.5 | 1.4 | (0.8, 2.6) | ||
| Asian/Pacific Islander | 9.9 | 25.9 | (17.5, 34.3) | 10.8 | 1.7 | (0.9, 3.2) | ||
| Foreign-born Latina | 35.4 | 31.5 | (26.8, 36.2) | 16.4 | 2.1 | (1.4, 3.1)* | ||
| US-born Latina | 12.5 | 24.0 | (18.5, 29.5) | 8.9 | 1.6 | (1.3, 1.9)* | ||
| Native American/Alaska Native | 0.4 | 26.5 | ( 3.6, 49.4) | 11.4 | 1.8 | (0.7, 4.4) | ||
| European American | 34.9 | 15.1 | (10.0, 20.2) | 1.0 | ||||
| 100.0 | ||||||||
| 1999–2001 (n=10,519)g | ||||||||
| % of federal poverty level | ||||||||
| Missing | 9.9 | 22.3 | (19.6, 25.0) | 18.9 | 6.6 | (5.0, 8.6)* | ||
| 0–100 | 31.2 | 27.9d | (26.3, 29.5)d | 24.5d | 8.2 | (6.4, 10.5)* | ||
| 101–200 | 20.6 | 18.3 | (16.5, 20.1) | 14.9 | 5.4 | (4.2, 7.0)* | 75.50 | −2.19 |
| 201–300 | 9.9 | 12.8 | (10.6, 15.0) | 9.4 | 3.8 | (2.8, 5.0)* | ||
| 301–400 | 7.3 | 6.0 | (4.2, 7.8) | 2.6 | 1.8 | (1.2, 2.6)* | ||
| ≥401 | 21.1 | 3.4 | (2.6, 4.2) | 1.0 | ||||
| 100.0 | ||||||||
| Maternal educatione (completed level) | ||||||||
| < High school | 22.8 | 28.4d | (26.4, 30.4)d | 22.0d | 4.4 | (3.7, 5.3)* | ||
| High school graduate/GED | 23.6 | 21.9 | (20.1, 23.7) | 15.5 | 3.4 | (2.8, 4.1)* | ||
| Some college | 30.4 | 12.7 | (11.5, 13.9) | 6.3 | 2.0 | (1.6, 2.4)* | 62.38 | −1.70 |
| College graduate | 23.1 | 6.4 | (5.2, 7.6) | 1.0 | ||||
| 100.0 | ||||||||
| Neighborhood poverty | ||||||||
| Missing | 2.8 | 15.2 | (10.7, 19.7) | 0.9 | 1.1 | (0.8, 1.4) | ||
| ≥20% poor | 30.0 | 23.8d | (22.2, 25.4)d | 9.5d | 1.7 | (1.5, 1.8)* | ||
| < 20% poor | 67.1 | 14.3 | (13.4, 15.2) | 1.0 | ||||
| 100.0 | ||||||||
| Race/ethnicity f | ||||||||
| African American | 6.4 | 18.8 | (16.6, 21.0) | 9.5 | 2.0 | (1.7, 2.4)* | ||
| Asian/Pacific Islander | 10.2 | 17.8 | (15.3, 20.3) | 8.5 | 1.9 | (1.6, 2.3)* | ||
| Foreign-born Latina | 28.6 | 25.1 | (23.3, 26.9) | 15.8 | 2.7 | (2.4, 3.1)* | ||
| US-born Latina | 16.0 | 19.2 | (17.0, 21.4) | 9.9 | 2.1 | (1.8, 2.4)* | ||
| Native American/Alaska Native | 0.6 | 17.8 | (7.0, 28.6) | 8.5 | 1.9 | (1.0, 3.5) | ||
| European American | 38.2 | 9.3 | (8.3, 10.3) | 1.0 | ||||
| 100.0 | ||||||||
Note. CI = confidence interval; GED = general equivalency diploma.
a PAR%: Population attributable risk percentage (PAR) is the percentage reduction in delayed or no care in the population overall that would occur if all groups of pregnant women were to experience the rate of the most-advantaged group.
b RII: The relative index of inequality (RII) reflects the experiences of the entire population, taking into account the relative size of each socioeconomic group. It involves calculating the mean health status of each socioeconomic group and then ranking the groups by their socioeconomic status. A summary measure (the slope index of inequality) is formed by means of weighted regression analysis. The RII is calculated above by dividing the slope index of inequality (the average decline in the standardized rate of delayed or no care moving from the most-disadvantaged to the most-advantaged socioeconomic group) by the rate of delayed or no care among women overall.
c Overall rate of delayed or no care in 1994–1995: 23.5% (95% CI = 20.3, 26.7).
d Significantly different (P < .05) from the corresponding estimates in the other time period.
e Excludes women with unknown education: 0.3% in 1994–1995 and 0.9% in 1999–2001.
f Excludes women with unknown or other race/ethnicity: 0.8% in 1994–1995 and 2.4% in 1999–2001.
g Overall rate of delayed or no care in 1999–2001: 17.1% (95% CI = 16.3, 17.9).
*Statistically significant difference compared with most-advantaged group (P < .05).
Identifying issues that warrant attention in efforts to reduce disparities.
Using logistic regression to estimate the odds ratio for delayed or no care in each disadvantaged social group relative to its counterpart a priori most-advantaged group, we assessed the potential contributions of different variables to the observed disparities by comparing the unadjusted and adjusted odds ratios from a series of models. We considered the variables used to define the social groups of a priori interest—income, maternal education, neighborhood poverty, and racial/ethnic group—together in the initial model. We next added other covariates in sequential models and in a final model including all variables, observing the effects on the odds ratios for each social variable. For simplicity, and because the results generally had similar implications, we report only the findings from the (1) unadjusted models, (2) initial multivariate model including the 4 social variables, and (3) full model; sequential models are not displayed.
Using 1999–2001 data, we identified at-risk social groups warranting particular attention because they did not meet the Healthy People 2010 objective of 90% with early care and had elevated risks relative to their a priori most-advantaged counterparts. We conducted separate logistic regression analyses, including all covariates listed above, to explore risk factors for delayed or no care in each at-risk group. Because policy implications depend in part on numbers of affected people, we also calculated the prevalence of each covariate within each at-risk group.
All analyses were conducted with SUDAAN software86 to account for effects of the clustered survey sampling designs87 and to alleviate difficulties with statistical inference introduced by including both individual and family- and neighborhood-level variables in models.88,89 Previous studies used a similar approach.71,90–94 Explicit multilevel linear modeling techniques were not used here because generally few women were sampled per tract (< 5 in 90% of tracts in 1999–2001).95
RESULTS
Describing Social Disparities in Prenatal Care
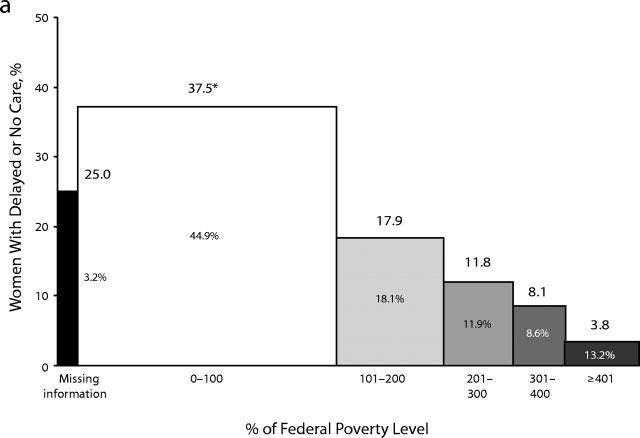
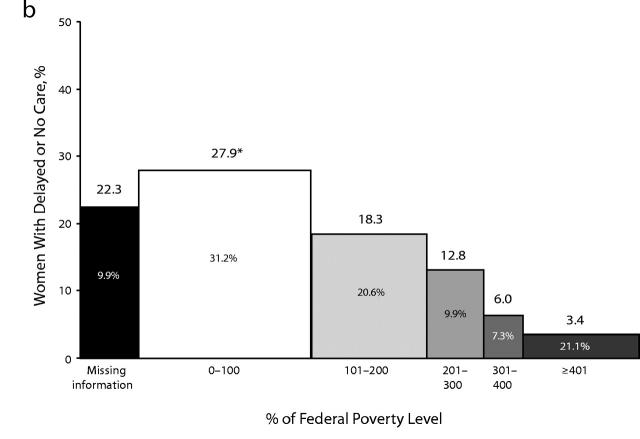
Table 1 ▶ displays the income, maternal education, neighborhood poverty, and race/ethnicity distributions and corresponding delayed or no care rates during 1994–1995 and 1999–2001. In both periods, an income gradient in delayed or no care rates was suggested: the lower a woman’s income, the more likely she was to lack first-trimester care. Figure 1 ▶ displays this graphically, along with the proportions of women in each income group. Compared with the highest income group, significantly higher rates (i.e., significant rate differences) and relative risks of delayed or no care were seen in both periods not only for the poorest women but for each income group up to 300% of poverty, and first-trimester care rates in all of these groups were below the 90% Healthy People 2010 objective. Similarly, even women who had attended but not graduated from college had higher rates of delayed or no care than college graduates. At both times, delayed or no care rates were higher for women in poor compared with nonpoor neighborhoods; this difference was observed within most income, education, and racial/ethnic groups (not displayed). During both periods, all other racial/ ethnic groups appeared to have higher rates of delayed or no care than European Americans, although these differences were not always statistically significant.
FIGURE 1—
Proportions of women with delayed or no prenatal care, by income: postpartum women surveyed in California in (a) 1994–1995 and (b) 1999–2001.
Note. Width of bar shows percentage of population in each income group.
*The proportion for this group in 1999–2001 was significantly different from that in 1994–1995 (at α = .05).
As shown in Table 1 ▶ and Figure 1 ▶, the percentage of women who were poor declined from 45% in 1994–1995 to 31% in 1999–2001. Comparing the 2 periods, we found declines in delayed or no care rates overall and within the most disadvantaged socioeconomic groups (poor, not high school graduates, residents of poor neighborhoods), with apparent declines in the corresponding rate differences for these groups. Comparing relative risks in the 2 periods, we found no significant reductions in the size of the disparities in care initiation. For example, although a smaller percentage of poor women had delayed or no care in 1999–2001 compared with 1994–1995, the relative gap between the poorest and most affluent groups was not significantly smaller. Comparing summary measures of socioeconomic disparities for the 2 periods also suggested no significant improvement in income or education disparities.
Identifying Issues that Warrant Attention in Efforts to Reduce Disparities
Table 2 ▶ displays prevalence rates and unadjusted odds ratios of delayed or no care in the entire 1999–2001 sample for each social group variable and covariate, along with multivariate results. Results from the initial model (model 1), including only the 4 variables defining the social groups of a priori concern, show that adjusted odds ratios for all income groups up to 300% of poverty remained significantly elevated and were not significantly lower than the unadjusted estimates; adjusted odds ratios for the education groups without any college remained elevated but were significantly reduced; and differences by neighborhood poverty were no longer significant. Compared with European Americans, other racial/ethnic groups remained at significantly higher risk of delayed or no care, but the odds ratio for each group except Asian/Pacific Islanders was significantly reduced after adjusting for the 3 socioeconomic variables. Full model (model 2) results again showed marked and statistically significant income disparities; however, no other social group except Asian/Pacific Islanders appeared to be at elevated risk.
TABLE 2—
Odds Ratios for Delayed or No Prenatal Care, by Income, Maternal Education, Race/Ethnicity, and Neighborhood Poverty: Postpartum Women (n = 10 210) Surveyed in California, 1999–2001
| Adjusted Odds Ratio (95% CI) | ||||
| % of Total | Unadjusted Odds Ratio (95% CI) | Model 1 | Model 2 | |
| Primary social variable | ||||
| % of federal poverty level | ||||
| Missing | 10.2 | 8.28 (6.18, 11.10) | 5.98 (4.32, 8.29) | 3.42 (2.32, 5.04) |
| 0–100 | 31.9 | 10.91 (8.41, 14.14) | 6.94 (5.05, 9.54) | 2.98 (2.03, 4.39) |
| 101–200 | 20.4 | 6.31 (4.80, 8.30) | 4.55 (3.31, 6.26) | 2.39 (1.64, 3.49) |
| 201–300 | 9.5 | 4.02 (2.93, 5.53) | 3.33 (2.35, 4.70) | 2.62 (1.78, 3.85) |
| 301–400 | 7.1 | 1.65 (1.09, 2.52) | 1.49 (0.96, 2.30) | 1.46 (0.89, 2.37) |
| ≥401 | 20.8 | Reference | Reference | Reference |
| Maternal education (completed level) | ||||
| Less than high school | 23.8 | 5.90 (4.80, 7.25) | 1.95 (1.49, 2.54) | 1.33 (0.96, 1.85) |
| High school/GED | 23.8 | 4.16 (3.37, 5.13) | 1.66 (1.28, 2.14) | 1.30 (0.95, 1.78) |
| Some college | 29.6 | 2.16 (1.74, 2.67) | 1.20 (0.93, 1.54) | 1.05 (0.78, 1.40) |
| College graduate | 22.8 | Reference | Reference | Reference |
| Neighborhood povertya | ||||
| ≥20% poor | 30.9 | 1.90 (1.69, 2.13) | 0.99 (0.87, 1.13) | 1.01 (0.87, 1.18) |
| < 20% poor | 69.1 | Reference | Reference | Reference |
| Race/ethnicityb | ||||
| African American | 6.5 | 2.25 (1.87, 2.70) | 1.25 (1.01, 1.53) | 1.26 (1.00, 1.60) |
| Asian/Pacific Islander | 10.3 | 2.10 (1.69, 2.60) | 2.17 (1.74, 2.72) | 2.29 (1.70, 3.09) |
| Foreign-born Latina | 29.8 | 3.26 (2.80, 3.78) | 1.38 (1.16, 1.65) | 1.20 (0.88, 1.63) |
| US-born Latina | 16.0 | 2.31 (1.94, 2.76) | 1.23 (1.01, 1.49) | 1.24 (0.98, 1.57) |
| European American | 37.5 | Reference | Reference | Reference |
| Covariate | ||||
| Paternal education (completed level) | ||||
| Missing | 8.0 | 6.49 (5.10, 8.26) | 1.20 (0.85, 1.71) | |
| Less than high school | 23.6 | 5.52 (4.49, 6.78) | 1.15 (0.82, 1.59) | |
| High school/GED | 28.5 | 3.44 (2.80, 4.22) | . . . | 1.13 (0.83, 1.52) |
| Some college | 17.0 | 1.98 (1.56, 2.52) | 1.03 (0.76, 1.41) | |
| College graduate | 23.0 | Reference | Reference | |
| Unmarried | 34.5 | 2.67 (2.38, 2.99) | . . . | 1.26 (1.06, 1.49) |
| Maternal age, y | ||||
| 15–17 | 3.9 | 5.17 (3.96, 6.74) | 2.45 (1.65, 3.62) | |
| 18–19 | 6.8 | 2.50 (1.95, 3.20) | . . . | 1.38 (0.97, 1.96) |
| 20–34 | 73.5 | 1.47 (1.23, 1.75) | 1.12 (0.88, 1.43) | |
| ≥35 | 15.7 | Reference | Reference | |
| Parity | ||||
| ≥5 births | 4.3 | 2.40 (1.89, 3.05) | 1.75 (1.23, 2.48) | |
| 2–4 births | 55.7 | 1.14 (1.01, 1.28) | . . . | 1.37 (1.15, 1.63) |
| First birth | 40.1 | Reference | Reference | |
| No coverage in first trimester | 17.5 | 6.60 (5.81, 7.50) | . . . | 4.61 (3.93, 5.40) |
| No usual source of prepregnancy care | 30.0 | 2.05 (1.82, 2.30) | . . . | 1.10 (0.94, 1.28) |
| Non-English language spoken at home | 40.3 | 2.18 (1.94, 2.43) | . . . | 1.09 (0.86, 1.39) |
| Prenatal care not “very important” to others | 6.8 | 3.01 (2.52, 3.59) | . . . | 1.92 (1.52, 2.42) |
| Smoked during pregnancy | 10.5 | 1.84 (1.57, 2.15) | . . . | 1.33 (1.07, 1.64) |
| Drank during pregnancy | 18.7 | 1.12 (0.97, 1.29) | . . . | 1.50 (1.25, 1.81) |
| Sense of control (7 = least, 28 = most), mean | 23.05 | 0.90 (0.88, 0.91) | . . . | 0.99 (0.97, 1.01) |
| Unintended pregnancy | 46.7 | 2.84 (2.52, 3.19) | . . . | 1.52 (1.29, 1.80) |
| Somewhat/very unhappy about pregnancy | 18.7 | 2.55 (2.25, 2.89) | . . . | 1.36 (1.15, 1.61) |
Note. CI = confidence interval; GED = general equivalency diploma.
a Women with missing data on neighborhood poverty were excluded.
b Native American/Alaska Native, other, or unknown race/ethnicity were excluded because of too few numbers.
Separate models were run for the 3 groups of women—those with incomes up to 300% of poverty, lacking college degrees, or living in poor neighborhoods—identified as at-risk (not displayed). In all 3 groups, significantly higher risks of delayed or no care were seen among women who were multiparous, lacked first-trimester insurance, reported that their prenatal care was not “very important” to others close to them, had unintended pregnancies, were initially unhappy about being pregnant, or were Asian/Pacific Islanders. Elevated risks also were seen (but not in all 3 groups) among women who were young teens, unmarried, or who smoked or drank during pregnancy. Most of these risk factors were experienced by at least 10%—unintended pregnancy by over 40%—of women in each at-risk group.
DISCUSSION
The objective of this article was to demonstrate the methods and potential applications of a systematic approach for studying and monitoring social disparities in health and health care. Using routinely collected population-based information for childbearing women in California during 1994–1995 and 1999–2001 and focusing on prenatal care as an example indicator, we (1) identified and measured disparities in delayed or no prenatal care across social groups defined by family income, maternal education, neighborhood poverty, and race/ethnicity; and (2) identified factors to consider in future efforts to reduce disparities. Results on the example indicator—delayed or no care—are discussed here to illustrate how this approach might provide useful information for other indicators, rather than to provide a comprehensive discussion of how to reduce prenatal care disparities.
Despite significant improvements in early prenatal care rates among childbearing women in California overall and within disadvantaged groups, disparities did not appear significantly smaller in 1999–2001 than in 1994–1995. In both periods, most groups of childbearing women in California had elevated delayed or no care rates, in absolute and relative terms. Only women with incomes above 300% of poverty, college graduates, and European Americans met the Healthy People 2010 target. Although the proportion of childbearing women in poverty declined, as did rates of poverty in the general population at that time,96 disparities by income persisted. In earlier work, we found marked improvements and reduced disparities in early prenatal care corresponding with federal and state initiatives during the late 1980s and early 1990s.65,97 The absence of continued reductions in disparities during the later 1990s may reflect a lack of major new initiatives, “welfare reform,” or changes in policies affecting immigrants.98–103
The findings presented here suggest that interventions to further reduce prenatal care disparities should be more broadly targeted to reach women with incomes up to 300% of poverty (approximately three quarters of the California maternity population in 1999–2001) and those without college degrees (also approximately three quarters of childbearing women), as well as Asian/ Pacific Islanders (10% of childbearing women) who are not generally considered at-risk. Our results confirmed earlier evidence that interventions to promote early prenatal care should focus on first-trimester insurance coverage,81 family planning,63 and general population attitudes about prenatal care.63 Even with these efforts, the findings suggest that social disparities in prenatal care are unlikely to be eliminated without addressing underlying economic inequalities. Significant income disparities persisted after adjusting for education, insurance, and many other factors that may be on pathways from economic disadvantage to delayed or no prenatal care. Notably, racial/ethnic disparities were greatly reduced for most groups when income, education, and neighborhood poverty were considered.
We believe that the general approach presented here and summarized in Table 3 ▶ provides a model for monitoring social disparities and informing efforts to reduce them. Particularly relevant for states with Centers for Disease Control and Prevention Pregnancy Risk Assessment Monitoring System surveys, the approach requires routinely collected population-based data—on key social factors, potential risk or protective factors, and indicators of health (including health status, health care, health-related behaviors, and other likely health determinants)—that can be disaggregated to compare groups with different levels of underlying social advantage.5,41,104–106 Socioeconomic, racial/ethnic, gender, and geographic groups should always be considered when potentially relevant. Another crucial element of the approach is to examine indicators of health separately for each social group, comparing all other social groups with the a priori most-advantaged group. With that group as a reference, disparities can be measured using rate differences and relative risks (and, when feasible, more complex summary measures), and at-risk social groups can be identified. Examining changes over time provides critical information for guiding policy. Although not definitive, a narrowing disparity may indicate that current policies should continue; a widening gap may suggest the need for changes. Policy responses are also informed by changes in the sizes of different socioeconomic groups (particularly in the proportions who are poor or near-poor, of low educational levels, or living in poor neighborhoods) and in the prevalence of likely risk factors.
TABLE 3—
Overview of an Approach to Studying Social Disparities in Health and Health Care
|
When informing policymakers about social disparities in health, a major challenge is to present information clearly and meaningfully without being simplistic. Descriptive findings can be presented in tables and graphically. Although summary measures (reflecting both the overall distribution of a socioeconomic variable and differences in risk across groups defined by that variable83–85) are not widely used in research and may have limited intuitive meaning for policymakers, they can help to confirm conclusions based on simpler measures and to compare socioeconomic (but not racial/ ethnic) disparities across states or time. A simpler alternative, illustrated in Figure 1 ▶, is to graphically display changes over time in both the observed socioeconomic disparities and the socioeconomic distribution. Policymakers are familiar with the concepts involved in these descriptive analyses, and health departments should have the necessary capabilities. When the requisite technical expertise is available, multivariate modeling can help identify risk factors to consider. Regardless of the analytic techniques used, quantitative results must be interpreted in the context of policies in all sectors that could influence health, informed by the literature and local knowledge. Although beyond the scope of this discussion, for many reasons we recommend that any study of disparities include representatives of relevant social groups to help identify issues and interpret findings.105,107,108
Work to describe and understand disparities, including selecting social groups to compare and covariates to examine, must be tailored to each health or health care indicator.109 Using this approach with other indicators and in other states will require adaptations to accommodate differences in data sources, population sizes and characteristics, and technical capabilities. Several limitations we encountered are also likely to affect other efforts. No study can capture all relevant socioeconomic information, but every study should include at least 1 measure of economic resources. Income is limited as a measure of economic resources; however, at least in the US, data are more widely available on income than on accumulated assets. Education is important in itself but should not be used as a proxy for income.5,72,110,111 The choice of socioeconomic and racial/ethnic variables will generally be limited in studies like this that rely on existing data. The surveys we used were restricted to women who spoke or read English or Spanish, which could have affected findings on Asian-Pacific Islanders. With data from different surveys and only 2 time periods, we could not formally assess trends over time. Differences in neighborhood-level poverty results between time periods should be interpreted with particular caution for several reasons, including the following: the neighborhoods of surveyed women may not represent neighborhoods statewide; geocoding completeness and accuracy could differ between surveys (e.g., 16.2% of the earlier sample could not be geocoded); and effects may vary depending on the neighborhood socioeconomic characteristic being studied.28,70,71 Because our primary goal was to demonstrate an overall approach, we did not explore many other area-level factors (e.g., the geographic distribution of health care facilities or providers) with potential relevance for prenatal care. Other states will also face limitations related to sample size, particularly for less prevalent indicators, requiring longer periods of data collection.
We hope that this work will generate discussion leading to more systematic and comprehensive approaches to studying and monitoring social disparities in health, particularly at the state level. Analyses must be framed and findings interpreted with the explicit goal of informing efforts to reduce disparities, systematically focusing on improvements among the socially disadvantaged.112 Although health policymakers cannot dictate policies in other sectors, they can call attention to health-related disparities and advocate for action in other sectors. The economic recession and budget crises currently faced by California and other states threaten to severely cut back services that very likely contributed to earlier improvements.65,97 In this environment, ongoing monitoring and analysis of state-level disparities are critical to inform policies and to ensure that scarce resources are used effectively. Monitoring and research are clearly not sufficient to eliminate disparities in health, but they are crucial.5,41,105,113,114
Acknowledgments
This publication was made possible by a Cooperative Agreement between the Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, and the Association of Teachers of Preventive Medicine (subaward TS 521-16/16). Additional support was provided by the Kaiser Family Foundation (grant 00-1735A).
The authors wish to acknowledge helpful suggestions from Gilberto Chavez, MD, MPH, State Epidemiologist, California Department of Health Services; Amy Lansky, PhD, Coordinator, Pregnancy Risk Assessment and Monitoring System, Centers for Disease Control and Prevention, Atlanta; Juliet VanEenwyck, PhD, State Epidemiologist, Washington State Department of Health; and an anonymous reviewer. We also thank Mah-Jabeen Soobader, PhD, MPH, for assistance with data analyses and Jennie Kamen and Nicole Wojtal for their assistance with research and preparation of the article.
Note. The contents of this article are the responsibility of the authors and do not necessarily reflect the official views of the Centers for Disease Control and Prevention or the Association of Teachers of Preventive Medicine.
Human Participant Protection Approval for the original surveys and for the use of survey data in this work was obtained from the University of California, San Francisco committee on human research and the California Health and Human Services Agency committee for the protection of human subjects.
Contributors All of the authors were involved in developing the conceptual framework and analytic approach presented in the article. P. A. Braveman contributed to writing the article, supervised all aspects of the project, and was the lead investigator on both postpartum surveys used in this work. S. A. Egerter contributed to writing the article and was involved in the methodological development of both surveys. C. Cubbin analyzed the data and contributed to writing the article. K. S. Marchi analyzed the data, contributed to writing the article, and was the project director for both surveys.
Peer Reviewed
References
- 1.Starfield B. Improving equity in health: a research agenda. Int J Health Serv. 2001;31:545–566. [DOI] [PubMed] [Google Scholar]
- 2.International Society for Equity in Health (ISEqH). Working definitions. Available at: http://www.iseqh.org/en/workdef.htm. Accessed June 6, 2003.
- 3.Braveman P, Gruskin S. Defining equity in health. J Epidemiol Community Health. 2003;57:254–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv. 1999;29: 295–352. [DOI] [PubMed] [Google Scholar]
- 5.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. [DOI] [PubMed] [Google Scholar]
- 6.Amick BC, Levine S, Tarlov AR, Walsh DC, eds. Society and Health. New York: Oxford University Press; 1995.
- 7.Berkman LF, Kawachi I, eds. Social Epidemiology. New York: Oxford University Press; 2000.
- 8.Whitehead M. The concepts and principles of equity in health. Int J Health Serv. 1992;22:429–445. [DOI] [PubMed] [Google Scholar]
- 9.Sen A. Development as Freedom. New York: Random House; 1999.
- 10.An andand S. The concern for equity in health. J Epidemiol Community Health. 2002;56:485–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Macroeconomics and Health: Investing in Health for Economic Development. Report of the Commission on Macroeconomics and Health. Geneva: World Health Organization; 2001.
- 12.Chang W-C. The meaning and goals of equity in health. J Epidemiol Community Health. 2002;56: 488–491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mooney G. What does equity in health mean? World Health Stat Q. 1987;40:296–303. [PubMed] [Google Scholar]
- 14.Mann JM, Gruskin S, Grodin MA, Annas GJ, eds. Health and Human Rights. New York: Rutledge; 1999.
- 15.Healthy People 2010: Understanding and Improving Health. Washington, DC: US Dept of Health and Human Services; 2000.
- 16.Pamuk E, Makuc D, Heck K, Reuben C, Lochner K. Socioeconomic Status and Health Chartbook: Health, United States, 1998. Hyattsville, Md: National Center for Health Statistics; 1998.
- 17.Hogan VK, Richardson JL, Ferre CD, Durant T, Boisseau M. A public health framework for addressing black and white disparities in preterm delivery. J Am Med Womens Assoc. 2001;56:177–180. [PubMed] [Google Scholar]
- 18.Hogue CJR, Hargraves MA. Class, race, and infant mortality in the United States. Am J Public Health. 1993;83:9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kleinman JC, Kessel SS. Racial differences in low birth weight. N Engl J Med. 1987;317:749–753. [DOI] [PubMed] [Google Scholar]
- 20.Kogan MD, Alexander GR. Social and behavioral factors in preterm birth. Prenat Neonat Med. 1998;6: 29–31. [Google Scholar]
- 21.Kogan MD, Kotelchuck M, Alexander GR, Johnson WE. Racial disparities in reported prenatal care advice from health care providers. Am J Public Health. 1994;84:82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Montgomery LE, Kiely JL, Pappas G. The effects of poverty, race, and family structure on US children’s health: data from the NHIS, 1978 through 1980 and 1989 through 1991. Am J Public Health. 1996;86: 1401–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh GK, Yu SM. Infant mortality in the United States: trends, differentials, and projections, 1950 through 2010. Am J Public Health. 1995;85:957–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singh GK, Yu SM. Adverse pregnancy outcomes: differences between US- and foreign-born women in major US racial and ethnic groups. Am J Public Health. 1996;86:837–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Braveman P, Oliva G, Miller MG, et al. Adverse outcomes and lack of health insurance among newborns in an eight-county area of California, 1982 to 1986. N Engl J Med. 1989;321:508–513. [DOI] [PubMed] [Google Scholar]
- 26.Braveman PA, Egerter S, Bennett T, Showstack J. Differences in hospital resource allocation among sick newborns according to insurance coverage. JAMA. 1991;266:3300–3308. [PubMed] [Google Scholar]
- 27.Braveman P, Egerter S, Edmonston F, Verdon M. Racial/ethnic differences in the likelihood of cesarean section. Am J Public Health. 1995;85:625–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pearl M, Braveman P, Abrams B. The relationship of neighborhood socioeconomic characteristics to birth-weight among 5 ethnic groups in California. Am J Public Health. 2001;91:1808–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cubbin C, Braveman P, Marchi K, et al. Socioeconomic and racial/ethnic disparities in unintended pregnancy among postpartum women in California. Matern Child Health J. 2002;6:237–246. [DOI] [PubMed] [Google Scholar]
- 30.Gazmararian JA, Adams MM, Pamuk ER. Associations between measures of socioeconomic status and maternal health behavior. Am J Prev Med. 1996;12: 108–115. [PubMed] [Google Scholar]
- 31.Cramer JC. Social factors and infant mortality: identifying high-risk groups and proximate causes. Demography. 1987;24:299–322. [PubMed] [Google Scholar]
- 32.Institute of Medicine. Preventing Low Birthweight. Washington, DC: National Academy Press; 1985. [PubMed]
- 33.Starfield BH. Child health and socioeconomic status. Am J Public Health. 1982;72:532–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Starfield B, Shapiro S, Weiss J, et al. Race, family income, and low birth weight. Am J Epidemiol. 1991; 134:1167–1174. [DOI] [PubMed] [Google Scholar]
- 35.Starfield B, Riley AW, Witt WP, Robertson J. Social class gradients in health during adolescence. J Epidemiol Community Health. 2002;56:354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trends in the Well-Being of America’s Children and Youth. Washington, DC: US Dept of Health and Human Services; 2002.
- 37.Wise PH, Kotelchuck M, Wilson ML, Mills M. Racial and socioeconomic disparities in childhood mortality in Boston. N Engl J Med. 1985;313:360–366. [DOI] [PubMed] [Google Scholar]
- 38.Newacheck PW, Hughes DC, Stoddard JJ. Children’s access to primary care: differences by race, income, and insurance status. Pediatrics. 1996;97: 26–32. [PubMed] [Google Scholar]
- 39.Krieger N, Rowley DL. Re: Race, family income, and low birth weight. Am J Epidemiol. 1992;136: 501–502. [DOI] [PubMed] [Google Scholar]
- 40.Krieger N, Fee E. Measuring socioeconomic status inequalities in health in the United States: a historical review, 1990–1950. Int J Health Serv. 1996;26: 391–418. [DOI] [PubMed] [Google Scholar]
- 41.Krieger N. The making of public health data: paradigms, politics, and policy. J Public Health Policy. 1992;13:412–427. [PubMed] [Google Scholar]
- 42.Krieger N, Moss NE. Accounting for the public’s health: an introduction to selected papers from a US conference on “Measuring Social Inequalities in Health.” Int J Health Serv. 1996;26:383–390. [DOI] [PubMed] [Google Scholar]
- 43.Krieger N, Moss NE, Syme L. Recommendations of the conference “Measuring Social Inequalities in Health.” Int J Health Serv. 1996;26:521–527. [DOI] [PubMed] [Google Scholar]
- 44.Williams DR. Race, socioeconomic status, and health: the added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188. [DOI] [PubMed] [Google Scholar]
- 45.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Ann Rev Sociol. 1995;21:349–386. [Google Scholar]
- 46.Williams DR. Race and health: basic questions, emerging directions. Ann Epidemiol. 1997;7:322–333. [DOI] [PubMed] [Google Scholar]
- 47.Rowley DL. Beyond the medical models: research on social factors and preterm delivery. Prenat Neonat Med. 1998;3:170–172. [Google Scholar]
- 48.Kramer MS. Preventing preterm birth: are we making progress? Prenatal Neonat Med. 1998;3:10–12. [PMC free article] [PubMed] [Google Scholar]
- 49.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams DR. Race/ethnicity and socioeconomic status: measurement and methodological issues. Int J Health Serv. 1996;26:483–505. [DOI] [PubMed] [Google Scholar]
- 51.Krieger N, Fee E. Social class: the missing link in U.S. health data. Int J Health Serv. 1994;24:25–44. [DOI] [PubMed] [Google Scholar]
- 52.Egerter S, Marchi K, Cubbin C, Braveman P. Socioeconomic and Racial/Ethnic Disparities in Maternal and Infant Health in California. Kaiser Family Foundation; 2004.
- 53.Tyson J, Guzick D, Rosenfeld CR, et al. Prenatal care evaluation and cohort analyses. Pediatrics. 1990; 85:195–204. [PubMed] [Google Scholar]
- 54.Kogan MD, Martin JA, Alexander GR, Kotelchuck M, Ventura SJ, Frigoletto FD. The changing pattern of prenatal care utilization in the United States, 1981–1995, using different prenatal care indices. JAMA. 1998;279: 1623–1628. [DOI] [PubMed] [Google Scholar]
- 55.Brown S, ed. Prenatal Care: Reaching Mothers, Reaching Infants. Washington, DC: National Academy Press; 1988. [PubMed]
- 56.Caring for Our Future: The Content of Prenatal Care. Washington, DC: US Dept of Health and Human Services; 1989.
- 57.American Academy of Pediatrics, American College of Obstetrics and Gynecology. Guidelines for Perinatal Care. Elk Grove Village, Ill: American Academy of Pediatrics; 1997.
- 58.Pregnancy Risk Assessment Monitoring System (PRAMS). Available at: http://www/cdc.gov/nccdphp/drh/srv_prams.htm. Accessed December 22, 2003.
- 59.MapMarker Plus software (MapInfo Corp, Troy, NY).
- 60.Krieger N, Waterman P, Lemieux K, Zierler S, Hogan JW. On the wrong side of the tracts? Evaluating the accuracy of geocoding in public health research. Am J Public Health. 2001;91:1114–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Braveman P, Egerter S, Marchi K. The prevalence of low income among childbearing women in California: implications for the private and public sectors. Am J Public Health. 1999;89:868–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Galbraith A, Egerter S, Marchi K, Chavez G, Braveman P. Newborn early discharge revisited: are California newborns receiving recommended postnatal services? Pediatrics. 2003;111:364–371. [DOI] [PubMed] [Google Scholar]
- 63.Braveman P, Marchi K, Egerter S, Pearl M, Neuhaus J. Barriers to timely prenatal care among women with insurance: the importance of prepregnancy factors. Obstet Gynecol. 2000;95:874–880. [DOI] [PubMed] [Google Scholar]
- 64.Roberts EM. Neighborhood social environments and the distribution of low birthweight in Chicago. Am J Public Health. 1997;87:597–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Braveman P, Marchi K, Sarnoff R, Egerter S, Rittenhouse D, Salganicoff A. Promoting Access to Prenatal Care: Lessons from the California Experience. Washington, DC: Kaiser Family Foundation; 2003.
- 66.O’Hare WP. A new look at poverty in America. Popul Bull. 1996;51:2–46. [Google Scholar]
- 67.Soobader M, LeClere F, Hadden W, Maury B. Using aggregate geographic data to proxy individual socioeconomic status: does size matter? Am J Public Health. 2001;91:632–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramariam SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? The Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156: 471–482. [DOI] [PubMed] [Google Scholar]
- 69.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramariam SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: the Public Health Disparities Geocoding Project (US). J Epidemiol Community Health. 2003;57:186–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lee RE, Cubbin C. Neighborhood context and cardiovascular behavioral risk factors in youth. Am J Public Health. 2002;92:428–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cubbin C, LeClere FB, Smith GS. Socioeconomic status and fatal injuries: individual and neighborhood determinants. J Epidemiol Community Health. 2000;54: 517–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Braveman P, Cubbin C, Marchi K, Egerter S, Chavez G. Measuring socioeconomic status in studies of racial/ethnic disparities: examples from maternal and child health. Public Health Rep. 2001;116: 449–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Health, United States, 1982. Washington, DC: US Dept of Health and Human Services; 1982.
- 74.Cunradi CB, Caetano R, Clark C, Schafer J. Neighborhood poverty as a predictor of intimate partner violence among white, black, and Hispanic couples in the United States: a multi-level analysis. Ann Epidemiol. 2000;10:297–308. [DOI] [PubMed] [Google Scholar]
- 75.Polednak AP. Stage at diagnosis of prostate cancer in Connecticut by poverty and race. Ethn Dis. 1997;7: 215–220. [PubMed] [Google Scholar]
- 76.Ensminger ME, Lamkin RP, Jacobson N. School leaving: a longitudinal perspective including neighborhood effects. Child Dev. 1996;67:2400–2416. [PubMed] [Google Scholar]
- 77.McWhorter WP, Schatzkin AG, Horm JW, Brown CC. Contribution of socioeconomic status to black/white differences in cancer incidence. Cancer. 1989;63: 982–987. [DOI] [PubMed] [Google Scholar]
- 78.Breen N, Figueroa JB. Stage of breast and cervical cancer diagnosis in disadvantaged neighborhoods: a prevention policy perspective. Am J Prev Med. 1996;12: 319–326. [PubMed] [Google Scholar]
- 79.Statistical Brief: Poverty Areas. Washington, DC: US Dept of Commerce; 1995.
- 80.Nothnagle M, Marchi K, Egerter S, Braveman P. Risk factors for late or no prenatal care following Medicaid expansions in California. Matern Child Health J. 2000;4:251–259. [DOI] [PubMed] [Google Scholar]
- 81.Egerter S, Braveman P, Marchi K. The timing of insurance coverage and use of prenatal care among low-income women. Am J Public Health. 2002;92: 423–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981;22: 337–356. [PubMed] [Google Scholar]
- 83.Wagstaff A, Paci P, van Doorslaer E. On the measurement of inequalities in Health. Soc Sci Med. 1991; 33:545–557. [DOI] [PubMed] [Google Scholar]
- 84.Mackenbach JP, Kunst AE. Measuring the magnitude of socioeconomic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44:757–771. [DOI] [PubMed] [Google Scholar]
- 85.Pamuk E. Social-class inequality in infant mortality in England and Wales from 1921 to 1980. Eur J Popul. 1988;4:1–21. [DOI] [PubMed] [Google Scholar]
- 86.SUDAAN Version 8.0 User’s Manual. Research Triangle Park, NC: Research Triangle Institute; 2001.
- 87.Skinner CN, Holt D, Smith TMF, eds. Analysis of Complex Surveys. New York: John Wiley & Sons; 1989.
- 88.Soobader M. Effects of Income Inequality on Morbidity (Dissertation). Ann Arbor, Mich: University Professors Program, Boston University, UMI; 1998.
- 89.Goldstein H. Multilevel Statistical Models. London, England: Arnold Publishers; 1999.
- 90.LeClere FB, Rogers RG, Peters K. Neighborhood social context and racial differences in women’s heart disease and mortality. J Health Soc Behav. 1998;39: 91–107. [PubMed] [Google Scholar]
- 91.Cubbin C, Hadden WC, Winkleby MA. Neighborhood context and cardiovascular disease risk factors: the contribution of material deprivation. Ethn Dis. 2001;11:687–700. [PubMed] [Google Scholar]
- 92.Soobader MJ, LeClere FB. Aggregation and the measurement of income inequality: effects on morbidity. Soc Sci Med. 1999;48:733–744. [DOI] [PubMed] [Google Scholar]
- 93.Robert SA. Community-level socioeconomic status effects on adult health. J Health Soc Behav. 1998;39: 18–37. [PubMed] [Google Scholar]
- 94.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91: 1783–1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Duncan C, Jones K, Moon G. Context, composition and heterogeneity: using multilevel models in health research. Soc Sci Med. 1998;46:97–117. [DOI] [PubMed] [Google Scholar]
- 96.Historical Poverty Tables, Table 21. Number of Poor and Poverty Rate, by State: 1980 to 2001. Washington, DC: US Bureau of the Census; 2002. Available at: http://www.census.gov/hhes/poverty/histpov/hstpov21.html. Accessed December 22, 2003.
- 97.Rittenhouse DR, Braveman P, Marchi K. Improvements in prenatal insurance coverage and utilization of care in California: an unsung public health victory. Matern Child Health J. 2003;7:75–86. [DOI] [PubMed] [Google Scholar]
- 98.Chavkin W, Wise PH. The data are in: health matters in welfare policy. Am J Public Health. 2002;92: 1392–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chavkin W, Romero D, Wise PH. State welfare reform policies and declines in health insurance. Am J Public Health. 2000;90:900–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Baumeister L, Hearst N. Why children’s health is threatened by federal immigration policies. West J Med. 1999;171:58–61. [PMC free article] [PubMed] [Google Scholar]
- 101.Fenton JJ, Moss N, Khalil HG, Asch S. Effect of California’s proposition 187 on the use of primary care clinics. West J Med. 1997;166:16–20. [PMC free article] [PubMed] [Google Scholar]
- 102.Pati S, Romero D, Chavkin W. Changes in use of health insurance and food assistance programs in medically underserved communities in the era of welfare reform: an urban study. Am J Public Health. 2002;92: 1441–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Park LS, Sarnoff R, Bender C, Korenbrot C. Impact of recent welfare and immigration reforms on use of Medicaid for prenatal care by immigrants in California. J Immigr Health 2000;2:5–22. [DOI] [PubMed] [Google Scholar]
- 104.Krieger N, Chen JT, Ebel G. Can we monitor socioeconomic inequalities in health? A survey of US health departments’ data collection and reporting practices. Public Health Rep. 1997;112:481–494. [PMC free article] [PubMed] [Google Scholar]
- 105.Braveman P. Monitoring Equity in Health and Health Care: A Policy-Oriented Approach in Low- and Middle-Income Countries. Geneva: World Health Organization; 1998. Equity Initiative Document No. 3, WHO document WHO/CHS/HSS98.1.
- 106.Braveman P, Tarimo E. Social inequalities in health within countries: not only an issue for affluent nations. Soc Sci Med. 2002;54:1621–1635. [DOI] [PubMed] [Google Scholar]
- 107.Metzler MM, Higgins DL, Beeker CG, et al. Addressing urban health in Detroit, New York City, and Seattle through community-based participatory research partnerships. Am J Public Health. 2003;93: 803–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Global Equity Gauge Alliance. The Equity Gauge: Concepts, Principles, and Guidelines. Durban, SA: Health Systems Trust; 2003. 30 pp. Available at: http://www.gega.org.za or http://www.hst.org.za. Accessed December 22, 2003.
- 109.Braveman P, Cubbin C. Optimal SES indicators cannot be prescribed across all outcomes. Am J Public Health. 2003;93:12–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Daly MC, Duncan GJ, McDonough P, Williams DR. Optimal indicators of socioeconomic status for health research. Am J Public Health. 2002;92: 1151–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Backlund E, Sorlie PD, Johnson NJ. The shape of the relationship between income and mortality in the United States: evidence from the National Longitudinal Morality Study. Ann Epidemiol. 1996;6:12–20. [DOI] [PubMed] [Google Scholar]
- 112.Whitehead M. Equity and Ethics in Health. Regional Committee for Europe, 44th session, 1994: Technical discussions: Annex. Copenhagen: World Health Organization Regional Office for Europe; 1995. (EUR/ICP/RPD 419).
- 113.Dahlgren G, Whitehead M. Policies and Strategies to Promote Equity in Health. Copenhagen: World Health Organization Regional Office for Europe; 1992.
- 114.De Kadt E, Tasca R. Promoting Equity: A New Approach from the Health Sector. Washington, DC: Pan American Health Organization (PAHO/WHO); 1993.