Abstract
Objective:
The aim of the study was to compare laparoscopic-assisted and open ileocolic resection for primary Crohn's disease in a randomized controlled trial.
Methods:
Sixty patients were randomized for laparoscopic-assisted or open surgery. Primary outcome parameter was postoperative quality of life (QoL) during 3 months of follow-up, measured by SF-36 and GIQLI questionnaire. Secondary parameters were operating time, morbidity, hospital stay, postoperative morphine requirement, pain, and costs.
Results:
Patient characteristics were not different. Conversion rate was 10% (n = 3). Median operating time was longer in laparoscopic compared with open surgery (115 versus 90 minutes; P < 0.003). Hospital stay was shorter in the laparoscopic group (5 versus 7 days; P = 0.008). The number of patients with postoperative morbidity within the first 30 days differed between the laparoscopic and open group (10% versus 33%; P = 0.028). There was no statistically significant difference in QoL between the groups during follow-up. Significant time effects were found on all scales of the SF-36 (P < 0.001) and the GIQLI score (P < 0.001). QoL declined in the first week, returned to baseline levels after 2 weeks, and was improved 4 weeks and 3 months after surgery. Median overall costs during the 3 months follow-up were significantly different: €6412 for laparoscopic and €8196 for open surgery (P = 0.042).
Conclusions:
Although QoL measured by SF-36 and GIQLI questionnaires was not different for laparoscopic-assisted compared with the open ileocolic resection, morbidity, hospital stay, and costs were significantly lower.
The aim of this randomized trial was to evaluate postoperative recovery after laparoscopic or open ileocolic resection in patients with Crohn's disease. Sixty patients were randomized. Postoperative recovery, in terms of quality of life, was comparable after laparoscopic or open ileocolic resection. Hospital stay and total costs were significantly lower after laparoscopic resection.
Ileocolic resection is the most frequent performed surgical procedure for the treatment of Crohn's disease, usually performed because of obstruction. Acceptable morbidity rates and improved quality of life (QoL) have been reported after surgery.1–3
Since the introduction of laparoscopic colectomy in 1991,4 the experience in laparoscopic bowel surgery has increased gradually. Improved laparoscopic skills and introduction of new instruments have led to broad application of laparoscopy in benign and malignant diseases.5–7 Recently, institutional and multicenter randomized trials have shown that laparoscopic surgery for colorectal cancer is safe and an acceptable alternative for open surgery.8–11 Laparoscopic colorectal surgery for benign diseases has also met with great enthusiasm and widespread acceptance. Although a variety of laparoscopic intestinal surgical procedures have been done in different settings, many surgeons have been reluctant about its application in patients with inflammatory bowel disease. Induration of intestinal mesentery, active inflammation, fistula, immunodepression, and friable and dense adhesions can significantly complicate what is sometimes already technically challenging in open surgery. Only one randomized and a few comparative studies have been reported to compare laparoscopic-assisted ileocolic resection with the open procedure for Crohn's disease,2,12–16 indicating the feasibility of the laparoscopic procedure in selected patients. The randomized trial by Milsom et al13 also measured postoperative recovery in terms of recovery of pulmonary function. The question is whether this is a valid and clinically important endpoint in these usually young patients.
The aim of this study was to compare laparoscopic-assisted with open ileocolic resection for primary Crohn's disease in a randomized controlled trial with emphasis on feasibility and postoperative recovery measured by using validated QoL questionnaires.
PATIENTS AND METHODS
Patients eligible for an elective ileocolic resection for Crohn's disease were included in a randomized 3-center trial (Academic Medical Center and VU University Medical Center, Amsterdam; and the Isala Clinics, Zwolle). All procedures were done by or supervised by colorectal and/or laparoscopic surgeons having sufficient experience in open and laparoscopic approach (at least 20 laparoscopic ileocolic and/ or right colectomies).
All patients had small bowel series and colonoscopy to establish the diagnosis Crohn's disease in the terminal ileum plus or minus the cecum and to rule out Crohn's disease in the remaining large bowel. When suspected, either an ultrasound or CT scan was performed to diagnose and treat abscesses.
Inclusion criteria were patients with Crohn's disease scheduled for an elective procedure and age above 16 years. Exclusion criteria were a fixed palpable inflammatory mass prior to surgery, prior median laparotomy, earlier bowel resection, or pregnancy. Patients were asked to participate in this study in the outpatient department. After informed consent was obtained and after completing preoperative QoL questionnaires, patients were randomized. Patients were allocated to one of the 2 groups using sealed envelope randomization. Randomization was performed by an independent research fellow in the Academic Medical Center Amsterdam. The study was approved by the Medical Ethical Committee of all the participating centers.
Operative Procedures
Patients were preoperatively prepared with anterograde intestinal cleansing (Klean Prep). Surgery was performed under general anesthesia. Patients received antibiotics according to hospital protocol for 24 hours.
Laparoscopic-Assisted Ileocolic Resection
Patients were placed in the French position. A 3-trocar approach was used (subumbilical, 10 mm; right fossa, 10 mm; suprapubic, 5 mm). The surgeon stood between the legs of the patient with the camera holder in his left hand and laparoscopic scissors with electrocautery in his right hand. The surgeon's assistant was standing on the left side of the patient, manipulating the cecum with a retractor. After full mobilization of the right colon, the distal ileum and the cecum were exteriorized by a 4- to 5-cm vertical incision through the umbilicus. Vascular ligation, bowel division, and a sutured end-to-side anastomosis were performed extracorporeally.
In case of enterosigmoidal fistula, enterovesical fistula, or a large inflammatory mass, a small Pfannenstiel incision (8 cm) was performed instead of the transumbilical incision to facilitate mobilization and extraction of the mass and treatment of the fistula.
Open Surgical Technique
Through a midline incision from the umbilicus to the pubic bone, the right colon was mobilized. After vascular and bowel division, usually an end-to-side ileocolic anastomosis was performed.
Postoperative Care
Postoperatively, all patients were treated equally with regard to feeding, mobilization, and postoperative care. Postoperative pain management was performed by either patient-controlled analgesia (PCA), continuous morphine infusion, or by epidural anesthesia. The amount of morphine required during the first 3 days after surgery was registered if a patient had a PCA pump (B Braun, Oss, The Netherlands).
At the time of the start of the study, it was still common practice to remove the nasogastric tube the morning after surgery. Nowadays, the nasogastric tube is removed at the end of surgery. Oral intake was started with clear liquids and advanced as soon as tolerated. Patients were discharged when a normal diet was tolerated. Hospital stay was defined as the time from the intervention to hospital discharge.
Primary Endpoints
Postoperative QoL was measured with the SF-36 Health Survey,17 and the total score of the Gastro-Intestinal Quality of Life Index (GIQLI).18 Two subscales of the SF-36 (physical function and bodily pain) and the total GIQLI score served as primary endpoints. The SF-36 is a generic QoL measurement, consisting of 36 questions combined to form 8 domains. The SF-36 has 0–100 scales in the 8 domains. The GIQLI is a disease-specific questionnaire, consisting of 36 questions with 5 response categories. The responses to questions are summed to give a total numerical score. The QoL in both groups was measured preoperatively and at 1, 2, 4 weeks, and 3 months after surgery.
Secondary Endpoints
The remaining 6 subscales of the SF-36 were secondary endpoints. Furthermore, operating time, blood loss, conversion rate, early morbidity, morphine requirement, pain VAS scores, mortality, hospital stay, and costs were secondary endpoints.
Wound infections, urinary tract infections, pulmonary infections, and deep venous thrombosis were considered minor complications. Intra-abdominal abscesses, anastomotic leakage, bleeding, perforation, sepsis, burst abdomen, respiratory insufficiency, and prolonged ileus were considered major complications. An ileus was considered to be prolonged if patients did not have bowel sounds and/or flatus 5 days after surgery. Morbidity was scored as early morbidity if the event occurred within 30 days after surgery and late if morbidity occurred more than 30 days after surgery. Readmissions and reinterventions were included up to 3 months after surgery.
The calculation of costs for the 2 procedures was based on the mean costs in the main participating center (Academic Medical Center), consisting of costs for material used during the procedure, costs for use of an operating theater with personnel per minute, costs for relaparotomies, and costs for a day of admission.
The median costs for a surgical procedure were calculated by multiplying the mean costs for the use of an operating theater with personnel with the operating time and adding the mean costs for material used during the procedure. Overall costs were calculated by adding costs for hospital stay, readmissions, and reoperations to the costs of the surgical procedure.
Statistical Analysis and Power Analysis
Patients were analyzed according to the intention-to-treat principle. The hypothesis was that patients who underwent a laparoscopic-assisted ileocolic resection would have a faster postoperative recovery during the first month. The subscales physical function and bodily pain of the SF-36 could show clinically significant differences. Accepting the assumption that 20% was a relevant clinical difference in these subscales (standard deviation of 20%–25%) 2 to 4 weeks after surgery; a sample size of 30 patients per group was sufficient to find a statistically significant differences between the open and the laparoscopic-assisted group (α = 0.05, β = 0.1). The same calculation was performed for a 20-point difference in the total GIQLI score after 4 weeks between the 2 groups; again, a total of 60 patients was sufficient to show significant differences. These assumptions were made based on the QoL measurements by Liem et al comparing open versus laparoscopic hernia repair.19
Data are presented as median (range). Groups were compared using parametric tests for QoL results, nonparametric Mann-Whitney U tests for patient characteristics and operative parameters, and the χ2 test when appropriate. For QoL analysis, a repeated-measures analysis of variance was used to test between-group differences over time in scores on the QL measures. Statistical analysis was performed using the statistical program Statistical Package for the Social Sciences 11.5 for Windows (SPSS, Chicago, IL).
RESULTS
The trial flow diagram is shown in Figure 1. Between January 2000 and October 2003, 60 patients were operated according to the procedure allocated after randomization. In both groups, 4 patients refused to fill in the questionnaires after surgery. However, data such as return to diet, hospital stay, morbidity, and costs could be collected in these patients. Patient characteristics at baseline are presented in Table 1; there were no differences between the 2 groups. Results in terms of surgical parameters for the 2 procedures are shown in Table 2. The operation time was significantly longer in the patients operated by laparoscopy (115 minutes) compared with the open procedure (90 minutes, P < 0.003).
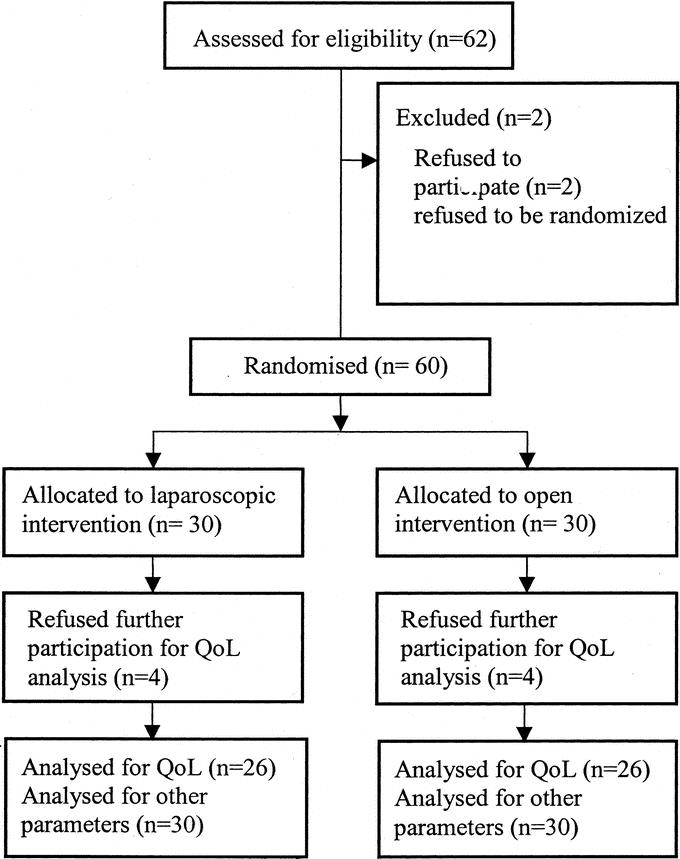
FIGURE 1. Trial flow diagram.
TABLE 1. Patient Characteristics Before Laparoscopic Assisted or Open Ileocolic Resection for Crohn's Disease
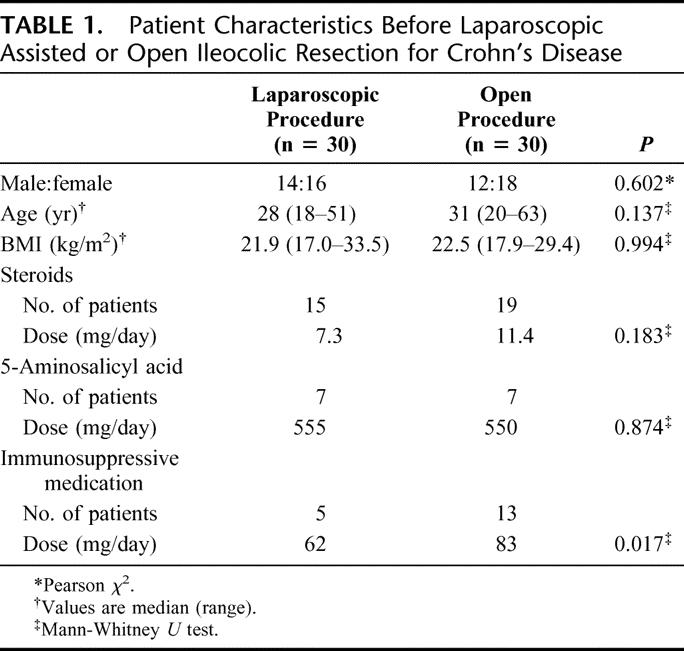
TABLE 2. Results of Laparoscopic Assisted or Open Ileocolic Resection for Crohn's Disease
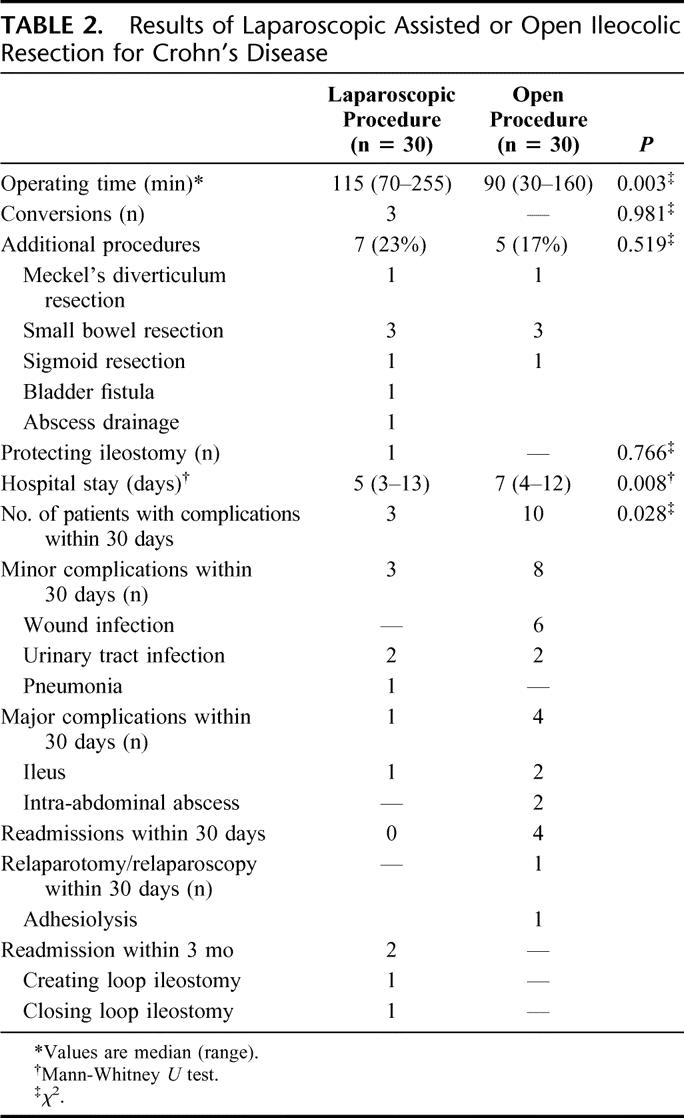
There was one conversion to an open procedure and 2 to a hand-assisted laparoscopic procedure (Omniport; Advanced Surgical Concepts Ltd., Wicklow, Ireland) due to a large inflammatory mass in the former, and extended disease in the latter two. There was no mortality. Twelve patients in the laparoscopic group and 11 patients in the open group had fistula to bladder, small bowel, or the colon, which were excised with an additional resection if necessary. Additional procedures were performed in 23% in the laparoscopic group and 17% in the open. One patient received a protecting loop ileostomy after laparoscopic ileocolic resection and sigmoidectomy because of ileosigmoidal fistula.
During the first 30 days after surgery, 3 patients had 4 complications in the laparoscopic group; 1 patient had a major complication viz. a prolonged ileus and a urinary tract infection. There were 2 other minor complications viz. pneumonia and a urinary tract infection.
In the open group, 10 patients had 12 complications in the first 30 days after surgery. Four patients had major complications, with or without a minor complication, 1 patient had a relaparotomy because of an intra-abdominal abscess that was not amenable for percutaneous drainage. The other 3 patients were treated conservatively: 2 patients had an ileus, and the third patient had an intra abdominal abscess. There were 8 minor complications in these 10 patients: 6 wound infections and 2 urinary tract infections. Four of the 6 patients with wound infection used steroids and/or immunosuppressive medication. The number of patients with morbidity within the first 30 days was different between the laparoscopic and open group (10% versus 33%; P = 0.028).
Hospital stay was significantly longer in the open group compared with the laparoscopic group; 7 days (range, 4–12 days) versus 5 days (range, 3–13 days) (P = 0.008).
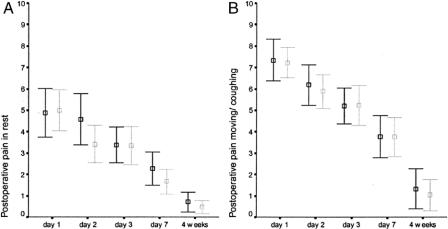
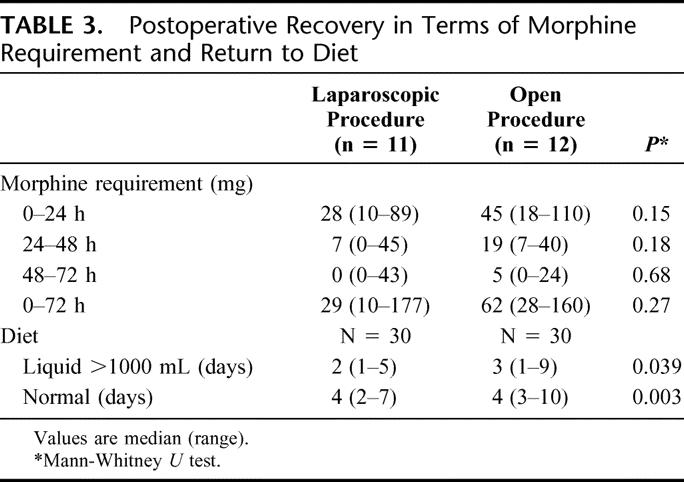
All patients had adequate analgesia since the mean VAS was lower than 5 in rest. There were no significant differences in pain VAS scores in rest or while moving/coughing (Fig. 2). In the laparoscopic group, patients needed less morphine than in the open group according to registration with the PCA pump; however, this was not a significant difference. The median return to a normal diet did not differ between groups; however, overall laparoscopic patients returned to a normal diet faster (mean 3.8 days after laparoscopy versus 5.0 days after open surgery, P < 0.003) (Table 3).
FIGURE 2. Results of postoperative pain measured with VAS scores (mean ± 2 SEM). The x-axis represents the time when the VAS scores were taken after surgery. The gray bars represent the laparoscopic group; the black bars represent the open group.
TABLE 3. Postoperative Recovery in Terms of Morphine Requirement and Return to Diet
The results of the SF-36 and the GIQLI questionnaire are shown in Figure 3. Preoperative QoL levels were not significantly different (Table 4). No statistically significant difference was shown in QoL over time between the 2 surgical approaches. There was a decline in QoL over time on all scales of the SF-36 and total GIQLI-score in the first week. QoL returned to baseline levels after 2 weeks. Particularly during the first 2 weeks, slight differences were seen for physical function, bodily pain, and social function in favor of laparoscopy. However, these differences were not significant.
FIGURE 3. Results of postoperative quality of life measured with SF-36 questionnaire for subscales physical function and bodily pain and the GIQLI questionnaire. The x-axis represents the time when the questionnaires were done, before and after surgery. The gray bars represent the laparoscopic group; the black bars represent the open group.
TABLE 4. Results of Postoperative Quality of Life Measured With SF-36 and GIQLI
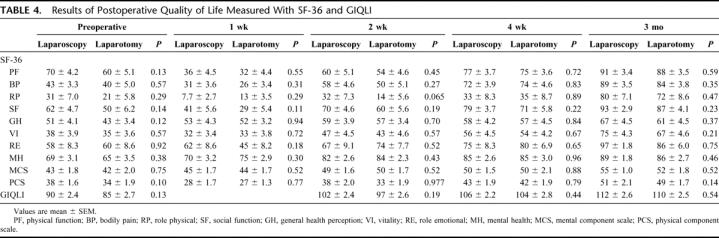
There was a significant time effect in both groups. QoL had improved in both groups during the 3-month follow-up compared with preoperative levels (SF-36, P < 0.001; and GIQLI, P < 0.001).
Costs of material used during the procedure were different for laparoscopy (€545), compared with the open procedure (€307). The difference could not be attributed to the use of disposables because they were rarely used. During a laparoscopic procedure 2 sets of instruments were used: an open and a laparoscopic set increasing the cleaning and sterilization costs.
The median costs for a laparoscopic assisted procedure were €1.103 (range, €885–€2.318) and for open surgery this was €744 (range, €453–€1.083; P < 0.001, Mann-Whitney U). Median overall costs, including relaparotomies, hospital stay, and readmission costs, were €6.412 (range, €4.195–€35.569) for the laparoscopic procedure and € 8.196 (range, €4.964–€19.018) for the open procedure (P = 0.042, Mann-Whitney U).
DISCUSSION
This study presents the results obtained by the first multicenter prospective randomized controlled trial comparing laparoscopic-assisted versus open ileocolic resection in 60 patients with Crohn's disease. Potential advantages of laparoscopy, such as less morbidity, shorter hospital stay, and faster return to normal diet are discriminating parameters in this study in favor of laparoscopy. Since outcome parameters such as return to diet and hospital stay are very likely to be biased, QoL was chosen as the primary efficacy parameter. Restoration of QoL postoperatively was not different for the laparoscopic procedure compared with the open procedure as measured by the SF-36 and the GIQLI questionnaires. QoL decreased immediately after surgery, but levels were back at baseline levels after 2 weeks and had increased after 3 months.
The differences in QoL between the 2 groups were limited, while assuming that a 20% difference would be of clinical relevance.19 The lack of significant differences between the 2 surgical approaches can be explained as follows: the SF-36 measures generic QoL; this questionnaire might not be specific for these patients. However, the GIQLI is disease specific, and this questionnaire did not show significant differences between the 2 approaches either. A second explanation might be that the assumption that a 20% difference in certain subscales as discriminating factor was wrong. At the start of the trial, this was thought to be acceptable for the power analysis. Nowadays, it is generally accepted that 10% difference is clinically significant. However, this depends on baseline levels, expected differences, the domain of interest, score distribution, etc. When looking at the results at 2 weeks after surgery, a difference of about 10% was found on the domains physical function, bodily pain, and social function. A larger sample size is probably required to make these figures significant. At 4 weeks and beyond, all possible differences had disappeared.
Thaler et al20 obtained similar results in a nonrandomized study. No different results in QoL were found comparing laparoscopic and open colectomy for benign diseases, particularly not for long-term results.
Since open ileocolic resection was, at the start of this study, still considered the standard procedure, laparoscopy was only offered in context of this trial. This partly explains the high percentage of patient accrual in this trial. Other hospitals with sufficient institutional laparoscopic experience were asked to participate in this study, but some refused since they considered the laparoscopic approach as the preferred procedure. Therefore, only 3 centers included patients in this multicenter study.
The present study showed that laparoscopic ileocolic resection is feasible, with a low conversion rate, and acceptable operating times. Postoperative morphine requirement was less in the laparoscopic group, although not significantly, which can be explained by the limited sample size. Furthermore, the laparoscopic approach is safe in terms of postoperative morbidity, which was significantly lower compared with open surgery. This difference was mainly due to a higher rate of wound complications in the open group. These data are in accordance with those from the institutional randomized trial of Milsom et al.13 The difference in postoperative stay was 2 days in favor of the laparoscopic approach. These figures must be interpreted carefully, since neither the patient nor the medical staff were blinded. Blinding the patient and medical staff for the type of procedure has been tried in a previous study, but was abandoned, since blinding turned out to be very difficult despite all measures to blind personnel and patients for the type of procedure. Although there were no restrictions with respect to advancement of diet and mobilization in both groups, nonblinding still might be a cause of bias in favor of the laparoscopic group.
Hospital stay as outcome parameter in studies comparing laparoscopy with open techniques has further been criticized since the implementation of “fast track” colon surgery protocols. The fast track multimodal perioperative care demonstrated that even after open segmental colonic resection patients can be discharged within 3 to 4 days after surgery.21 However, fast track multimodal approach is demanding both for the patient and the medical staff, and has not been that successful in every hospital. Nevertheless, it is likely that fast track protocols will further reduce the difference in hospital stay between the open and laparoscopic approaches.22
One of the most obvious advantages of the laparoscopic approach is the improved cosmesis.23 The preferred extraction site of the specimen was a transumbilical vertical incision. Since the incision was made right through the umbilicus, most of the scar disappeared in the shallow of the umbilicus. Sometimes it was not possible to extract the specimen through a small 4- to 5-cm incision due to the size of the inflammatory mass. In these cases, a Pfannenstiel incision was used to maintain the cosmetic advantages of the operation despite a relatively large extraction incision.
In this study, costs for the surgical procedure were significantly higher in the laparoscopic group (P < 0.001). However, overall costs (costs of surgical procedure, use of an operating theater, personnel, hospital stay, readmissions, and reoperations, etc.) were significantly lower for laparoscopy in comparison to open surgery (P = 0.042). The overall healthcare costs were calculated for the situation in the Academic Medical Hospital and might not be representative for other hospitals. In the literature, results of studies reporting costs for laparoscopic and open surgery are conflicting. Chapman et al24 and Janson et al25 concluded that laparoscopy was more expensive. However, in a review, Ballantyne26 reported comparable costs, while Delaney et al27 showed that costs for laparoscopic colorectal surgery were lower than for open surgery. Furthermore, Duepree et al15 and Shore et al16 have shown that the laparoscopic ileocolic resection was cheaper than the open resection in patients with Crohn's disease.
At present, there is no clear evidence yet with respect to other potential advantages of the laparoscopic approach such as an easier approach for a reresection, a lower rate of small bowel obstruction, or a lower rate of incisional hernias. The present study demonstrated that laparoscopic-assisted ileocolic resection is safe and cost-effective compared with open ileocolic resection for patients with primary Crohn's disease. Therefore, laparoscopy is the preferred approach treating distal ileitis in Crohn's disease provided the surgery is done by expert laparoscopists ensuring low conversion rates, acceptable operating times, and low morbidity.
Footnotes
Reprints: Willem A. Bemelman, MD, Department of Surgery, Academic Medical Center, Meibergdreef 9, 1105 AZ Amsterdam, The Netherlands. E-mail: W.A.Bemelman@amc.uva.nl.
REFERENCES
- 1.Tillinger W, Mittermaier C, Lochs H, et al. Health-related quality of life in patients with Crohn's disease: influence of surgical operationā prospective trial. Dig Dis Sci. 1999;44:932–938. [DOI] [PubMed] [Google Scholar]
- 2.Bemelman WA, Slors JF, Dunker MS, et al. Laparoscopic-assisted vs. open ileocolic resection for Crohn's disease: a comparative study. Surg Endosc. 2000;14:721–725. [DOI] [PubMed] [Google Scholar]
- 3.Delaney CP, Kiran RP, Senagore AJ, et al. Quality of life improves within 30 days of surgery for Crohn's disease. J Am Coll Surg. 2003;196:714–721. [DOI] [PubMed] [Google Scholar]
- 4.Jacobs M, Verdeja JC, Goldstein HS. Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc. 1991;1:144–150. [PubMed] [Google Scholar]
- 5.Dunker MS, Bemelman WA, Slors JF, et al. Laparoscopic-assisted vs open colectomy for severe acute colitis in patients with inflammatory bowel disease (IBD): a retrospective study in 42 patients. Surg Endosc. 2000;14:911–914. [DOI] [PubMed] [Google Scholar]
- 6.Meijerink WJ, Eijsbouts QA, Cuesta MA, et al. Laparoscopically assisted bowel surgery for inflammatory bowel disease: the combined experiences of two academic centers. Surg Endosc. 1999;13:882–886. [DOI] [PubMed] [Google Scholar]
- 7.Bemelman WA, Ringers J, Meijer DW, et al. Laparoscopic-assisted colectomy with the dexterity pneumo sleeve. Dis Colon Rectum. 1996;39(suppl):59–61. [DOI] [PubMed] [Google Scholar]
- 8.Lacy AM, Garcia-Valdecasas JC, Delgado S, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet. 2002;359:2224–2229. [DOI] [PubMed] [Google Scholar]
- 9.A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350:2050–2059. [DOI] [PubMed] [Google Scholar]
- 10.Leung KL, Kwok SP, Lam SC, et al. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet. 2004;363:1187–1192. [DOI] [PubMed] [Google Scholar]
- 11.Abraham NS, Young JM, Solomon MJ. Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg. 2004;9:1111–1124. [DOI] [PubMed] [Google Scholar]
- 12.Alabaz O, Iroatulam AJ, Nessim A, et al. Comparison of laparoscopically assisted and conventional ileocolic resection for Crohn's disease. Eur J Surg. 2000;166:213–217. [DOI] [PubMed] [Google Scholar]
- 13.Milsom JW, Hammerhofer KA, Böhm B, et al. Prospective, randomized trial comparing laparoscopic vs. conventional surgery for refractory ileocolic Crohn's disease. Dis Colon Rectum. 2001;44:1–9. [DOI] [PubMed] [Google Scholar]
- 14.Wu JS, Birnbaum EH, Kodner IJ, et al. Laparoscopic-assisted ileocolic resections in patients with Crohn's disease: are abscesses, phlegmons, or recurrent disease contraindications? Surgery. 1997;122:682–688. [DOI] [PubMed] [Google Scholar]
- 15.Duepree HJ, Senagore AJ, Delaney CP, et al. Advantages of laparoscopic resection for ileocecal Crohn's disease. Dis Colon Rectum. 2002;45:605–610. [DOI] [PubMed] [Google Scholar]
- 16.Shore G, Gonzalez QH, Bondora A, et al. Laparoscopic vs conventional ileocolectomy for primary Crohn disease. Arch Surg. 2003;138:76–79. [DOI] [PubMed] [Google Scholar]
- 17.Aaronson NK, Muller M, Cohen PD, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51:1055–1068. [DOI] [PubMed] [Google Scholar]
- 18.Eypasch E, Williams JI, Wood-Dauphinee S, et al. Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. Br J Surg. 1995;82:216–222. [DOI] [PubMed] [Google Scholar]
- 19.Liem MS, Halsema JA, van der GY, et al. Cost-effectiveness of extraperitoneal laparoscopic inguinal hernia repair: a randomized comparison with conventional herniorrhaphy: Coala trial group. Ann Surg. 1997;226:668–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thaler K, Dinnewitzer A, Mascha E, et al. Long-term outcome and health-related quality of life after laparoscopic and open colectomy for benign disease. Surg Endosc. 2003;17:1404–1408. [DOI] [PubMed] [Google Scholar]
- 21.Basse L, Thorbol JE, Lossl K, et al. Colonic surgery with accelerated rehabilitation or conventional care. Dis Colon Rectum. 2004;47:271–277. [DOI] [PubMed] [Google Scholar]
- 22.Basse L, Madsen JL, Billesbolle P, et al. Gastrointestinal transit after laparoscopic versus open colonic resection. Surg Endosc. 2003;17:1919–1922. [DOI] [PubMed] [Google Scholar]
- 23.Dunker MS, Stiggelbout AM, van Hogezand RA, et al. Cosmesis and body image after laparoscopic-assisted and open ileocolic resection for Crohn's disease. Surg Endosc. 1998;12:1334–1340. [DOI] [PubMed] [Google Scholar]
- 24.Chapman AE, Levitt MD, Hewett P, et al. Laparoscopic-assisted resection of colorectal malignancies: a systematic review. Ann Surg. 2001;234:590–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Janson M, Bjorholt I, Carlsson P, et al. Randomized clinical trial of the costs of open and laparoscopic surgery for colonic cancer. Br J Surg. 2004;91:409–417. [DOI] [PubMed] [Google Scholar]
- 26.Ballantyne GH. Laparoscopic-assisted colorectal surgery: review of results in 752 patients. Gastroenterologist. 1995;3:75–89. [PubMed] [Google Scholar]
- 27.Delaney CP, Kiran RP, Senagore AJ, et al. Case-matched comparison of clinical and financial outcome after laparoscopic or open colorectal surgery. Ann Surg. 2003;238:67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]