Abstract
Objective:
To determine the rate of postmastectomy reconstruction and investigate the impact of socioeconomic status on the receipt of reconstruction.
Summary Background Data:
The National Comprehensive Cancer Network (NCCN) Outcomes Project is a prospective, multi-institutional database that contains data on all newly diagnosed breast cancer patients treated at one of the participating comprehensive cancer centers.
Methods:
The study cohort consisted of 2174 patients with DCIS and stage I, II, and III invasive breast cancer who underwent mastectomy at one of 8 NCCN centers. Rates of reconstruction were determined. Logistic regression analyses were used to evaluate whether socioeconomic characteristics are associated with breast reconstruction.
Results:
Overall, 42% of patients had breast reconstruction following mastectomy. Patients with Medicaid and Medicare were less likely to undergo reconstruction than those with managed care insurance; however, there was no difference for indemnity versus managed care insurance. Homemakers and retired patients had fewer reconstructions than those employed outside the home. Patients with a high school education or less were less likely to have reconstruction than those with more education. Race and ethnicity were not significant predictors of reconstruction.
Conclusions:
The reconstruction rate in this study (42%) is markedly higher than those previously reported. The type of insurance, education level, and employment status of a patient, but not her race or ethnicity, appear to influence the use of breast reconstruction. Because all patients were treated at an NCCN institution, these socioeconomic differences cannot be explained by access to care.
The NCCN Outcomes Database is used to investigate current rates and socioeconomic determinants of breast reconstruction. Patients of lower socioeconomic status underwent fewer reconstructions after controlling for clinical and other demographic features. Because all patients are treated at comprehensive cancer centers, this variation cannot be explained by access to care.
The utilization of preventive services and common surgical procedures is higher among patients with higher socioeconomic status (SES), while lower SES is associated with nonelective “last resort” procedures.1 The etiology of these disparities in healthcare utilization has not been explained; however, access to care has often been hypothesized as a major contributor. Since breast reconstruction is largely an elective high-cost procedure, one can hypothesize that higher SES is associated with a higher likelihood of reconstruction.
The National Comprehensive Cancer Network (NCCN) is a coalition of 19 U.S. comprehensive cancer centers. The NCCN facilitates multi-institutional, prospective data collection on patients with newly diagnosed breast cancer as part of the NCCN Outcomes Project. This data can be used to analyze current practice patterns within these institutions. The NCCN database contains detailed socioeconomic, demographic, and clinical data that can only be gathered by individual chart review and cannot be found in administrative databases. Because all patients in this database are treated at comprehensive cancer centers, access to care will not explain any observed socioeconomic variations in the receipt of breast reconstruction.
This study uses the NCCN Outcomes Project database: 1) to determine the current rates and patterns of reconstruction in NCCN institutions; and 2) to evaluate the role of SES in the utilization of reconstruction following mastectomy in a cohort of patients with similar access to care.
METHODS
Subjects
The study cohort consisted of women with newly diagnosed ductal carcinoma in situ (DCIS) or stage I, II, or III (American Joint Committee on Cancer, 5th edition) breast cancer who received their primary cancer care at one of the 8 institutions participating in the NCCN Breast Cancer Outcomes Project between July 1, 1997 and June 25, 2002.2 The 8 institutions are as follows: Arthur G. James Cancer Hospital and Richard Solove Research Institute at Ohio State University, Columbus, OH; City of Hope National Medical Center, Duarte, CA; Dana-Farber Cancer Institute, Boston, MA; Fox Chase Cancer Center, Philadelphia, PA; H. Lee Moffitt Cancer Center and Research Institute at the University of South Florida, Tampa, FL; University of Texas MD Anderson Cancer Center, Houston, TX; Roswell Park Cancer Institute, Buffalo, NY; and University of Michigan Comprehensive Cancer Center, Ann Arbor, MI. Each center is an academic comprehensive cancer center where the majority of surgical and medical oncologists treating breast cancer devote most or all of their clinical effort to breast cancer care. The Institutional Review Board at each center has approved the study, data collection process, data transmission methods, and data storage protocols.
Exclusion criteria for the database included bilateral breast cancer, patients presenting for second opinions, those receiving no primary therapy at the NCCN institution, and patients referred for bone marrow transplantation. If a woman had multiple breast cancer episodes, only the first episode of breast cancer was included.
Among 8492 eligible patients, we identified 3542 patients who had a mastectomy as their definitive surgery for breast cancer. We excluded 401 patients who received their definitive surgery at an institution outside the NCCN in an effort to examine a homogeneous cohort with comprehensive baseline information and similar access to care. To ensure sufficient time for breast reconstruction to have been completed and documented in the medical record, only patients with at least 365 days of follow-up after initial presentation to the NCCN institution were included. In addition, patients who transferred their care out of the NCCN center, had a bone marrow transplant, or developed a new cancer (other than breast cancer) within 365 days of presentation were excluded. Our final sample consisted of 2174 eligible women who had a mastectomy.
Data Sources
Data collected from the patients’ medical records for the NCCN Outcomes Project included sociodemographics, type of health insurance at presentation, TNM staging based on the AJCC (5th edition), tumor pathology, all treatments administered (surgery, radiation, and systemic therapy), and recurrences.2–6 Comorbidity at presentation to the NCCN center was assigned using either the Charlson Index (based on chart review) or the modified version of that index using a patient survey developed by Katz et al.7,8 The data from these indices have been shown to be highly correlated.7 Employment status at diagnosis and educational status at presentation to the NCCN center (defined as highest level of education completed at presentation) were collected via patient survey at baseline. Height and weight at presentation were collected via patients’ medical records and were used to calculate the body mass index (BMI) for each patient. The 2000 Census data on median household income were linked to the eligible patients’ records from the NCCN database by zip code. The patient group was then divided into quartiles based on the distribution of median household income in our cohort (defined as [$14,125–<$35,240], [$35,240–<$45,245], [$45,245–<$59,918], and [≥$59,918]).
Rigorous data quality assurance processes were in place for the study, including initial and follow-up data management training; on-line edit checking during web-based data entry; programmed logic checks against the pooled data repository; routine quality assurance reports to the centers for rectification by the data managers; and on-site audits of a random sample of source documents against the submitted data within the first few months of data collection, and annually thereafter.
Definition of Receipt of Reconstruction and Types of Reconstruction
The receipt of breast reconstruction was determined by identifying a start date for a breast reconstruction surgery code that occurred within 365 days of presentation, and prior to the date of a recurrence. If no breast reconstruction surgery code was identified within this timeframe, then it was considered that the patient did not have breast reconstruction. Only breast reconstructions to the diseased breast were included. The following types of breast reconstruction are collected in the NCCN database: implant (including tissue expanders), transverse rectus abdominus myocutaneous (TRAM) pedicle flap, TRAM free flap, other pedicle flap, and other free flap. If a patient received both a tissue flap and implant, tissue flap was the type of reconstruction coded in the database. Receipt of reconstruction, the primary endpoint, was considered as a binary variable.
Statistical Analysis
The overall proportion of women undergoing reconstruction following mastectomy across NCCN institutions was calculated, along with the proportion receiving implants and flaps. To evaluate determinants of breast reconstruction, and in particular whether socioeconomic factors influence who undergoes reconstruction, we conducted univariate logistic regression analyses using the following potential explanatory variables related to SES: type of health insurance at presentation, educational status at presentation, race and ethnicity, employment status at diagnosis, and median household income based on 2000 Census zip code data. To account for potential clinical and treatment factors influencing use of reconstruction, we analyzed the following variables: age at diagnosis, stage at diagnosis, number of comorbidities at presentation, BMI presentation, and receipt of radiation therapy and chemotherapy.
Results for the univariate and multivariable analyses are presented as odds ratios (ORs, representing the increased odds of reconstruction for each category of patient when compared with the baseline category or reference group), along with 95% confidence intervals. P values less than the alpha level of 0.05 were considered to be statistically significant. If any category of an explanatory variable consisted of 10 or fewer patients, the category was excluded from further multivariable analysis.
After these exclusions, multivariable logistic regression was conducted on the final sample of 2162 patients to determine the best overall model associated with the socioeconomic determinants of breast reconstruction while controlling for NCCN institution and all significant clinical characteristics. Each logistic regression model was evaluated for goodness-of-fit using the Hosmer and Lemeshow test. In all cases, the goodness-of-fit tests were not statistically significant, indicating adequate fit of the regression models. The models also demonstrated good predictive value, with a c-index of 0.839 for the final multivariable regression model. Interaction terms were included when significant to account for varying rates in the use of reconstruction for certain combinations of independent variables. All possible combinations of independent variables were tested for significant interactions. A 2-sided alpha level of 0.05 was used to determine statistical significance.
RESULTS
Description of Cohort
Of the 2174 patients undergoing mastectomy, 42% had breast reconstruction with 95% being performed at the time of the mastectomy. Forty-three percent of all reconstructions were implants or tissue expanders while the remaining 57% were flap reconstructions. Among the flap reconstructions, 46% were pedicle and 54% were free flaps.
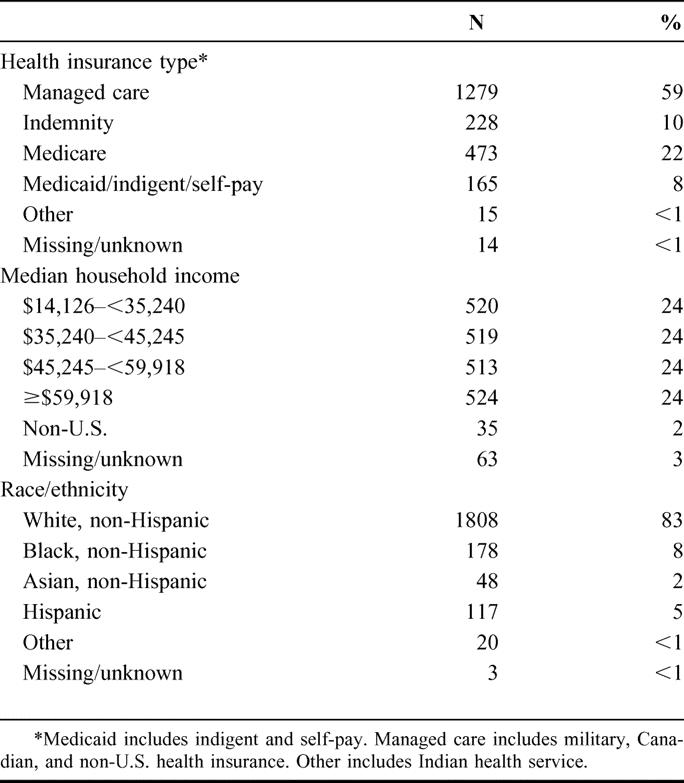
Table 1 presents the clinical and socioeconomic characteristics of the cohort. Seventy-one percent of these patients were less than 60 years of age at the time of diagnosis, and the most patients were white (83%). Eighty-seven percent of the patients had invasive breast cancer, and 13% were diagnosed with DCIS. Approximately one third of the women had a normal BMI and 80% had no comorbidity. Managed care was the predominant source of health insurance (59%). Forty-four percent of the patients were employed outside of the home and 50% had more than a high school education.
TABLE 1. Clinical and Socioeconomic Characteristics for 2174 Women Undergoing Mastectomy for DCIS, Stage I, II, and III Breast Cancer
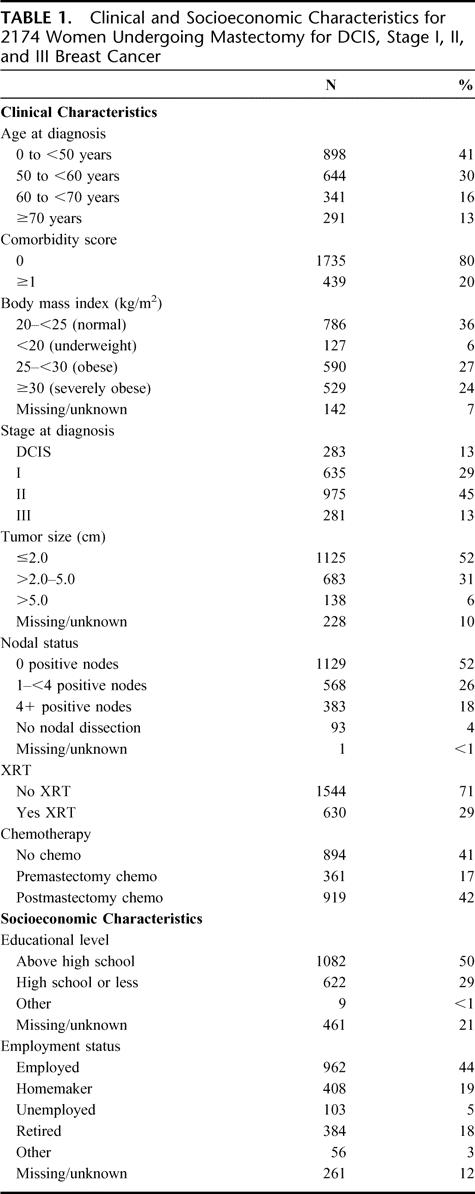
Table
Univariate Analyses
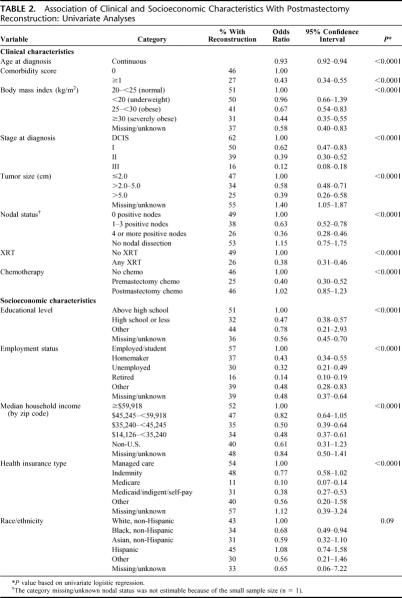
Table 2 shows the clinical and socioeconomic variables available in the NCCN database and potentially associated with reconstruction. Based on univariate analysis, the following socioeconomic variables were significantly associated with a decreased likelihood of reconstruction: high school education or less (or unknown education level), lack of employment outside the home at the time of diagnosis, Medicare or Medicaid insurance status, and lower median household income. While race was not significant (P = 0.09), these results suggest a trend toward lower rates of reconstruction in black and Asian groups.
TABLE 2. Association of Clinical and Socioeconomic Characteristics With Postmastectomy Reconstruction: Univariate Analyses
The significant clinical covariates associated with a lower likelihood of reconstruction included older age, a comorbidity score of 1 or more, stage I to III at diagnosis (versus DCIS), tumor size greater than 2.0 cm, one or more positive lymph nodes, receipt of radiation therapy, receipt of chemotherapy prior to mastectomy, and increased BMI (Table 2). These significant clinical factors were included in the multivariable model, with the exception of nodal status and tumor size, which contribute to the overall disease stage. Given this interdependency and the similar significance levels among these 3 variables, only overall stage was included in the multivariable analysis.
Multivariable Model
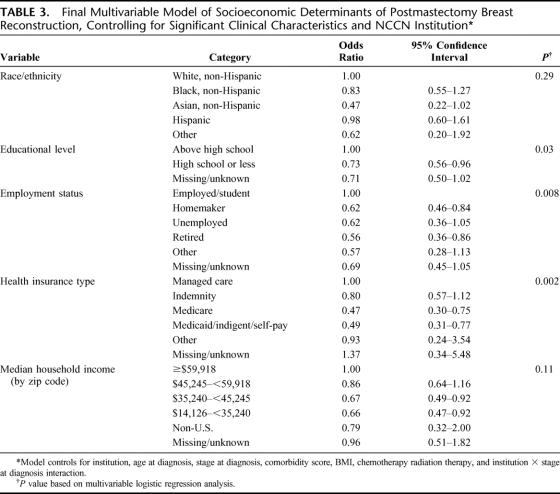
The results for the socioeconomic variables in the multivariable model, controlling for NCCN institution, significant clinical factors, and significant interaction terms, are presented in Table 3. Educational level and employment status were significant determinants of breast reconstruction. Patients with a high school diploma or less were less likely (OR, 0.73; 95% confidence interval [CI], 0.56–0.96) to undergo reconstruction than those with higher levels of education. Similarly, homemakers (OR, 0.62; 95% CI, 0.46–0.84) and retired patients (OR, 0.56; 95% CI, 0.36–0.86) were less likely to have breast reconstruction than those who were employed outside the home. There was a trend toward lower rates of reconstruction for unemployed patients (OR, 0.62; 95% CI, 0.36–1.05) as compared with those who were employed; however, this difference did not reach significance in the multivariable model. Patients in the 2 lower quartiles for household income were less likely to receive reconstruction than those in the highest income quartiles ($35,240–<$45,245; OR, 0.67; 95% CI, 0.49–0.92 and $14,126–<$35,240; OR, 0.66; 95% CI, 0.47–0.92); however, income as an overall variable was not significant (P = 0.11).
TABLE 3. Final Multivariable Model of Socioeconomic Determinants of Postmastectomy Breast Reconstruction, Controlling for Significant Clinical Characteristics and NCCN Institution
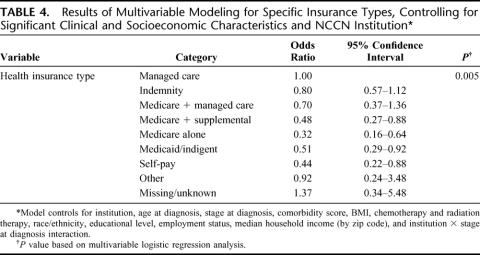
Because type of insurance was found to be a significant predictor of reconstruction, specific associations with this variable were evaluated further using a second multivariable regression model with health insurance redefined (Table 4). The second model included the same socioeconomic and clinical variables as the first model, except for the health insurance status at presentation variable. The Medicare patients were subdivided into Medicare alone, Medicare + supplemental insurance, and Medicare managed care. Medicaid/indigent/self-pay patients were subdivided into 2 categories: Medicaid/indigent and self-pay. Compared with Managed Care as the baseline, Medicare + supplemental insurance, Medicare alone, Medicaid/indigent, and self-pay were found to be associated with decreased use of reconstruction. However, there was no significant difference in reconstruction for patients with indemnity insurance or Medicare + managed care when compared with patients with managed care alone.
TABLE 4. Results of Multivariable Modeling for Specific Insurance Types, Controlling for Significant Clinical and Socioeconomic Characteristics and NCCN Institution
DISCUSSION
The decision to proceed with breast reconstruction following mastectomy is a complicated one, influenced by the clinical situation, as well as patient preference, provider preference, and access to care. The role that each of these factors plays in determining which patients get reconstruction is unclear. Furthermore, the SES of the patient may influence both patient and provider preferences, as well as access to care. This study sought to investigate the rate at which women undergo breast reconstruction and whether there are differences in the utilization of reconstruction based on indicators of SES. We have shown a correlation between SES, as reflected in educational level, employment status, insurance status, and the likelihood of getting postmastectomy breast reconstruction. We offer evidence that these differences reflect patient and/or provider preference as opposed to access to care.
The rate of reconstruction found in this study (42%) is markedly higher than those previously reported, which range from 8% to 15%.9–12 There are a number of possible explanations for this. First, these results represent the most up-to-date practices, with data gathered from 1997 to 2002, while previous studies used data from the late 1980s and early 1990s. Two of the previous studies demonstrated a marked increase in the observed rate of reconstruction over the study period, which would suggest breast reconstruction rates today would be higher. A study using the National Cancer Data Base reported an increase in the use of early or immediate reconstruction from 3.4% (1985–1990) to 8.3% (1994–1995), while a second study from Connecticut found an increase in the percentage of reconstructions from 9% to 16% over a 4-year period.10,11 In addition, the introduction of the Women's Health and Cancer Rights Act of 1998, requiring group health plans and individual health insurance to pay for reconstruction after mastectomy, has likely further increased the rates of breast reconstruction.13 Finally, the data are compiled from patients treated at comprehensive cancer centers participating in the NCCN. Overall rates for reconstruction in the United States may be lower than the rates in these centers; however, a recent study of community practice patterns in the northeastern United States reported a reconstruction rate of 20.8% within 1 year of mastectomy.14 Another recent study from a California university hospital reported that, between 1995 and 2002, 50% of women treated with mastectomy at that hospital had immediate reconstruction.15 This suggests that the rates of breast reconstruction are likely increasing in all types of hospitals.
There are studies documenting a relationship between SES and rates of reconstruction. A study from Australia found a strong correlation between higher SES and breast reconstruction; however it is not clear how these results will translate to the United States.16 As part of a study on the role of breast reconstruction in the physical and emotional outcomes after breast cancer, researchers were able to show that patients having reconstruction were more likely to be white, affluent, and college educated.17 These results were based on questionnaire data, and no multivariable analyses were performed. Several large studies have shown that age, race, and income, influence the likelihood of reconstruction.9–12 These studies relied on administrative and registry data with a limited range of patient-specific variables. In contrast, we had access to detailed patient-specific data allowing us to examine a wider range of socioeconomic and clinical factors than previous studies.
Some of the clinical factors associated with postmastectomy reconstruction in this study are similar to previous reports. For example, patients receiving reconstruction were younger with less advanced disease. A factor not previously reported to be related to reconstruction is obesity. Our data show that obese and severely obese patients had fewer reconstructions than normal or underweight patients. This could be related to an expectation of higher complication rates or other provider or patient concerns.
Payer status has not been studied specifically in previous reports examining determinants of breast reconstruction but has been shown to correlate with both health outcomes and healthcare utilization for other procedures.18–20 In univariate analysis, Medicare recipients appeared to have a significantly lower rate of reconstruction (11%) than any other insurance group, including Medicaid. On multivariable modeling adjusting for age and other variables, we found that both Medicare and Medicaid patients were less likely to undergo reconstruction compared with patients with managed care or indemnity insurance. This suggests that there may be a bias based on reimbursement, as federal agencies tend to provide lower rates of reimbursement than private payers.20
While it is not clear if this bias is at an institutional or surgeon level, our findings suggest that it is not likely to reflect patient preference alone. If this association were due to patient preference, one would expect the effect to be substantially diminished in multivariable analysis when other measures of SES, such as race, income, education, and employment, which are more likely to reflect patient preference, are considered. In fact, the OR for Medicaid/indigent/self-pay only changed by 20% in the multivariable analysis that adjusts for all other factors. The larger change for Medicare is likely due to the older age of Medicare patients.
In an attempt to further elucidate the effect of payer status on reconstruction, we remodeled our data after subdividing Medicare recipients into the following categories: Medicare alone, Medicare + managed care, and Medicare + private supplement and separating Medicaid and indigent patients from self-pay. Medicare recipients with managed care or indemnity supplement have breast reconstruction rates similar to those of patients with managed care alone, while patients with Medicare alone have a 44% lower OR than when Medicare is considered en bloc. This again supports an effect of reimbursement rates on provider recommendation, although further investigation is warranted.
A recent report from the Institute of Medicine emphasized that there is no one best measure of SES.21 Rather, there are a number of different measures, including income, education, occupation, and race, that are associated with the differences in healthcare observed across SES. Because of the richness of the NCCN prospective data collection method, our study was able to investigate a wider range of socioeconomic indicators than other studies that have relied on administrative data. We found an association between lower SES and reduced rates of reconstruction for all SES indicators on univariate analysis. The trend toward lower rates of reconstruction for black patients as compared with whites that was observed on univariate analysis was not seen in the multivariable model, suggesting that this trend reflected other factors. This is consistent with findings in other studies of socioeconomic disparities in health care.22–26 Few studies have sufficiently robust data to investigate multiple indicators of SES and must rely on less ideal proxies such as race. In this study, we have shown that multiple indicators of SES have significant independent associations with the likelihood of having breast reconstruction. Educational level and employment status were significant predictors of reconstruction in multivariable modeling. Lower rates of reconstruction were observed for the 2 lowest quartiles of income, but the overall variable was not significant. Income in this study was determined by linking the zip code of the patient with census data to determine average income for that area. This is a much grosser measure than our other variables and may explain why this variable does not reach significance.
The etiology of healthcare disparities is not well understood. It has been suggested that the differences in healthcare utilization and outcomes reflect differences in access to care. Access to care can be defined as the extent to which an individual is able to receive the right service at the right time in the right place for a given health condition.27–29 It is a function of whether people can enter and use a healthcare system to attain a given service. Traditional definitions of access to care have focused on whether a patient is able to enter the healthcare system, including such factors as the insurance status of the patient, whether specialized services are available to a given patient, and whether they have a primary care provider to help them negotiate the system and the means to travel long distances for better care. More recently, it has been suggested that we need to broaden this definition to include the appropriateness of care once the patient has entered the system, including such issues as provider bias. In this study, we are using the term “access to care” in its traditional sense: whether or not the patients are able to gain access to the system. The goal was to investigate whether socioeconomic differences exist once a patient has entered a healthcare system.
Patients of lower SES are less likely to have insurance or a primary healthcare provider making it more difficult for them to access the system. Several recent studies suggest that such lack of access cannot explain the observed socioeconomic and racial disparities, however. Black patients received fewer cardiac procedures following acute myocardial infarction than white patients in the Veterans Affairs Healthcare System.30 Additionally, black patients and patients with lower income in the Medicare population have substantially higher mortality rates and lower utilization of preventive health procedures.31 While neither of these systems has achieved the “universal access” to health care for which they were designed, they have minimized variations in access to care. A recent Canadian study of SES gradients in the utilization of angiography following acute myocardial infarction sought to specifically determine the contribution of access to care to disparities in utilization. They found that the availability of a tertiary care hospital and on-site angiography had minimal influence on the observed SES gradient.32
Another possible explanation for healthcare disparities relates to differences in clinical status. It has been reported that patients of lower SES tend to present with more advanced disease and more severe comorbidities.22,33–37 Additionally, it has been suggested that these patients may be more likely to partake in “risky” behaviors such as the use tobacco and alcohol.38
Finally, healthcare differences according to SES could reflect differences in culture, patient preference, and attitudes toward healthcare, as well as provider bias.39,40 In discussing racism in health care, Jones states that “social classification results in profound differences in life experiences and life opportunities.”41 There is evidence from questionnaire data that patients perceive discrimination based on race and SES and that there are perceived differences in the patient-physician relationship based on race, both of which can influence healthcare choices and utilization.42 The use of breast reconstruction following mastectomy has been shown to be strongly influenced by patient preference and personal values, suggesting that such differences could underlie potential differences in the rates of reconstruction observed across SES.43
All patients in this cohort received their care at an NCCN institution, which are all tertiary cancer care centers. In other words, all patients have access to similar resources for their cancer care. Therefore, the results of this study documenting a consistent relationship between SES and the likelihood of reconstruction should not reflect disparities in accessing the system. One component of access to care that may still influence reconstruction rates is insurance status. The results suggest that there is financial incentive for provider bias at either the individual provider or the institutional level based on insurance status. However, by including insurance status in the multivariable model, we have shown that this contributes to, but does not completely account for, the observed differences in reconstruction according to SES. We adjusted for disease stage at presentation and other clinical factors, in the event that patients with lower SES did present with more advanced disease and comorbidities. Our results suggest that personal preferences and attitudes toward health care play a major role in this socioeconomic gradient. As mentioned, previous studies have documented both a strong difference in patient preferences and attitudes across socioeconomic classes, as well as a strong influence of personal preference on the decision to undergo postmastectomy reconstruction.
The utilization of postmastectomy breast reconstruction decreases with decreasing SES, as reflected by educational level, employment status, and insurance status. This likely represents a combination of both patient preference and provider bias, but not access to care. A limitation of this study is the inability to distinguish between patient preference and provider bias. Further studies are warranted to determine the contribution of each of these to the observed socioeconomic differences in breast reconstruction. A thorough understanding of the factors underlying the decision to proceed with breast reconstruction will help assure that every woman has the opportunity to have postmastectomy breast reconstruction regardless of SES.
ACKNOWLEDGMENTS
The NCCN Breast Cancer Outcomes Project acknowledges the efforts of clinical research associates at each participating center who collected and entered the data for this study.
Footnotes
Supported in part by P50CA89393 to the Dana-Farber Cancer Institute from the National Cancer Institute.
Reprints: Jane C. Weeks, MD, MSc, Dana-Farber Cancer Institute, Center for Outcomes and Policy Research, 44 Binney Street, 454BRK S21-25, Boston, MA 02115. E-mail: Jane_Weeks@dfci.harvard.edu.
REFERENCES
- 1.Gornick ME. A decade of research on disparities in Medicare utilization: lessons for the health and health care of vulnerable men. Am J Public Health. 2003;93:753–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fleming ID, Henson CJ, eds. American Joint Committee on Cancer. AJCC Cancer Staging Handbook, 5th ed. Philadelphia: Lippincott Williams & Wilkins, 1997. [Google Scholar]
- 3.Weeks JC. Outcomes assessment in the NCCN. Oncology (Huntingt). 1997;11:137–140. [PubMed] [Google Scholar]
- 4.Weeks J. Outcomes assessment in the NCCN: 1998 update. National Comprehensive Cancer Network. Oncology (Huntingt). 1999;13:69–71. [PubMed] [Google Scholar]
- 5.Niland JC. NCCN. Internet-based data system for the conduct of outcomes research. Oncology (Huntingt). 1998;12:142–146. [PubMed] [Google Scholar]
- 6.Niland JC. NCCN outcomes research database: data collection via the Internet. Oncology (Huntingt). 2000;14:100–103. [PubMed] [Google Scholar]
- 7.Katz JN, Chang LC, Sangha O, et al. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84. [DOI] [PubMed] [Google Scholar]
- 8.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 9.Desch CE, Penberthy LT, Hillner BE, et al. A sociodemographic and economic comparison of breast reconstruction, mastectomy, and conservative surgery. Surgery. 1999;125:441–447. [PubMed] [Google Scholar]
- 10.Morrow M, Scott SK, Menck HR, et al. Factors influencing the use of breast reconstruction postmastectomy: a National Cancer Database study. J Am Coll Surg. 2001;192:1–8. [DOI] [PubMed] [Google Scholar]
- 11.Polednak AP. How frequent is postmastectomy breast reconstructive surgery? A study linking two statewide databases. Plast Reconstr Surg. 2001;108:73–77. [DOI] [PubMed] [Google Scholar]
- 12.Alderman AK, McMahon L Jr, Wilkins EG. The national utilization of immediate and early delayed breast reconstruction and the effect of sociodemographic factors. Plast Reconstr Surg. 2003;111:695–703; discussion 704–705. [DOI] [PubMed]
- 13.http://umet-vets.dol.gov/dol/topic/health-plans/womens.htm.
- 14.Bloom BS, de Pouvourville N, Chhatre S, et al. Breast cancer treatment in clinical practice compared to best evidence and practice guidelines. Br J Cancer. 2004;90:26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mortenson MM, Schneider PD, Khatri VP, et al. Immediate breast reconstruction after mastectomy increases wound complications: however, initiation of adjuvant chemotherapy is not delayed. Arch Surg. 2004;139:988–991. [DOI] [PubMed] [Google Scholar]
- 16.Hall SE, Holman CD. Inequalities in breast cancer reconstructive surgery according to social and locational status in Western Australia. Eur J Surg Oncol. 2003;29:519–525. [DOI] [PubMed] [Google Scholar]
- 17.Rowland JH, Desmond KA, Meyerowitz BE, et al. Role of breast reconstructive surgery in physical and emotional outcomes among breast cancer survivors. J Natl Cancer Inst. 2000;92:1422–1429. [DOI] [PubMed] [Google Scholar]
- 18.Mancini MC, Cush EM, Sweatman K, et al. Coronary artery bypass surgery: are outcomes influenced by demographics or ability to pay? Ann Surg. 2001;233:617–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shen JJ, Wan TT, Perlin JB. An exploration of the complex relationship of socioecologic factors in the treatment and outcomes of acute myocardial infarction in disadvantaged populations. Health Serv Res. 2001;36:711–732. [PMC free article] [PubMed] [Google Scholar]
- 20.Wenneker MB, Weissman JS, Epstein AM. The association of payer with utilization of cardiac procedures in Massachusetts. JAMA. 1990;264:1255–1260. [PubMed] [Google Scholar]
- 21.Medicine IO. Measuring the Effects of Socioeconomic Status on Health Care. Washington, DC: National Academy Press, 2002. [Google Scholar]
- 22.Bradley CJ, Given CW, Roberts C. Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer Inst. 2002;94:490–496. [DOI] [PubMed] [Google Scholar]
- 23.Franzini L, Williams AF, Franklin J, et al. Effects of race and socioeconomic status on survival of 1,332 black, Hispanic, and white women with breast cancer. Ann Surg Oncol. 1997;4:111–118. [DOI] [PubMed] [Google Scholar]
- 24.Michalski TA, Nattinger AB. The influence of black race and socioeconomic status on the use of breast-conserving surgery for Medicare beneficiaries. Cancer. 1997;79:314–319. [PubMed] [Google Scholar]
- 25.Miller BA, Hankey BF, Thomas TL. Impact of sociodemographic factors, hormone receptor status, and tumor grade on ethnic differences in tumor stage and size for breast cancer in US women. Am J Epidemiol. 2002;155:534–545. [DOI] [PubMed] [Google Scholar]
- 26.Muss HB. Factors used to select adjuvant therapy of breast cancer in the United States: an overview of age, race, and socioeconomic status. J Natl Cancer Inst Monogr. 2001;30:52–55. [DOI] [PubMed] [Google Scholar]
- 27.Rogers A, Flowers J, Pencheon D. Improving access needs a whole systems approach. BMJ. 1999;319:866–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gold M, Stevens B. Measuring access to care through population-based surveys in a managed care environment: synopsis and priorities for future efforts. Health Serv Res. 1998;33(3 Pt 2):611–624. [PMC free article] [PubMed] [Google Scholar]
- 29.Gulliford M, Figueroa-Munoz J, Morgan M, et al. What does ‘access to health care’ mean? J Health Serv Res Policy. 2002;7:186–188. [DOI] [PubMed] [Google Scholar]
- 30.Peterson ED, Wright SM, Dlaey J, et al. Racial variation in cardiac procedure use and survival following acute myocardial infarction in the Department of Veteran's Affairs. JAMA. 1994;271:1175–1180. [PubMed] [Google Scholar]
- 31.Gornick ME, Eggers PW, Reilly TW, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335:791–799. [DOI] [PubMed] [Google Scholar]
- 32.Alter DA, Naylor CD, Austin PC, et al. Geography and service supply do not explain socioeconomic gradients in angiography use after acute myocardial infarction. Cmaj. 2003;168:261–264. [PMC free article] [PubMed] [Google Scholar]
- 33.Ayanian JZ, Kohler BA, Abe T, et al. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med. 1993;329:326–331. [DOI] [PubMed] [Google Scholar]
- 34.Merkin SS, Stevenson L, Powe N. Geographic socioeconomic status, race, and advanced-stage breast cancer in New York City. Am J Public Health. 2002;92:64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Naik AM, Joseph K, Harris M, et al. Indigent breast cancer patients among all racial and ethnic groups present with more advanced disease compared with nationally reported data. Am J Surg. 2003;186:400–403. [DOI] [PubMed] [Google Scholar]
- 36.Roetzheim RG, Gonzalez EC, Ferrante JM, et al. Effects of health insurance and race on breast carcinoma treatments and outcomes. Cancer. 2000;89:2202–2213. [DOI] [PubMed] [Google Scholar]
- 37.Schrijvers CT, Coebergh JW, Mackenbach JP. Socioeconomic status and comorbidity among newly diagnosed cancer patients. Cancer. 1997;80:1482–1488. [PubMed] [Google Scholar]
- 38.Angell M. Privilege and health: what is the connection? N Engl J Med. 1993;329:126–127. [DOI] [PubMed] [Google Scholar]
- 39.Dein S. Explanatory models of and attitudes towards cancer in different cultures. Lancet Oncol. 2004;5:119–124. [DOI] [PubMed] [Google Scholar]
- 40.Whaley AL. Ethnicity/race, ethics, and epidemiology. J Natl Med Assoc. 2003;95:736–742. [PMC free article] [PubMed] [Google Scholar]
- 41.Jones C. The impact of racism on health. Ethn Dis. 2002;12(suppl 2):10–13. [PubMed] [Google Scholar]
- 42.Bird ST, Bogart LM. Perceived race-based and socioeconomic status (SES)-based discrimination in interactions with health care providers. Ethn Dis. 2001;11:554–563. [PubMed] [Google Scholar]
- 43.Reaby LL. Reasons why women who have mastectomy decide to have or not to have breast reconstruction. Plast Reconstr Surg. 1998;101:1810–1818. [DOI] [PubMed] [Google Scholar]