Abstract
Objective:
To demonstrate the use of Chang's needle for hepatic resections.
Summary Background Data:
Specialized instruments, fine surgical skills, and good control of hepatic inflow and backflow are essential for hepatic resections. This needle was specifically designed to simplify these requirements.
Methods:
Whole-thickness interlocking sutures of the liver can first be made along the designed resection line with a Chang's needle; then parenchyma transection can follow without inflow or backflow control. This was consecutively performed on 69 patients with primary (41), metastatic (10), and benign (18) diseases since 1997.
Results:
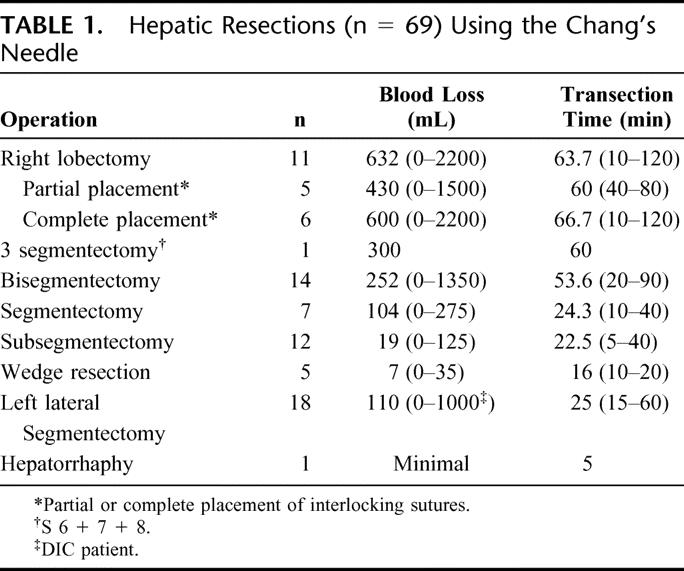
Blood loss during parenchyma transection was reduced in 11 right lobectomies (652 mL), 1 3-segmentectomy (300 mL), 14 bisegmentectomies (252 mL), 7 segmentectomies (104 mL), 12 subsegmentectomies (19 mL), 5 wedge resections (7 mL), 18 left lateral segmentectomies (110 mL), and 1 hepatorrhaphy (minimal). There was no procedure-related mortality. A mild bile leakage occurred in 1 case (1.5%) but healed spontaneously.
Conclusions:
The preliminary results demonstrate that this maneuver is a simple, easy, and safe method for performing hepatic resections.
Chang's needle can simplify various kinds of hepatic resections. Blood loss was reduced with minimal procedure-related morbidity and mortality.
Hepatic resections always carry a high risk of intraoperative hemorrhage and postoperative hepatic failure. Although mortality rate is decreasing with the refinement of surgical techniques, instruments, and postoperative care, bleeding during parenchyma transection remains a critical hurdle to overcome. Currently, some instruments such as the Lin's clamp,1 Cavitron ultrasound aspiration,2 water jet knife,3 Harmonic scapel,4 and microwave coagulator5 are used to facilitate hepatic resections. We have designed a simpler, cheaper needle6 to further simplify hemorrhage control and parenchyma transection procedures for various types of major and minor hepatic resections.
MATERIALS AND METHODS
In September 1997, the first right hepatic lobectomy was successfully performed using this specially designed straight needle (Chang's needle, Fig. 1, Chong Quey L.L.C. Kaohsiung, Taiwan) on a cirrhotic, hepatocellular carcinoma patient with minimal blood loss. Since then, this kind of operation has been performed consecutively on 69 patients with liver tumor, intrahepatic duct (IHD) stone, and liver trauma, all of whom were suitable for applying the Chang's needle. Those patients with IHD and common bile duct stones underwent concomitant cholecystectomy and choledocholithotomy with or without choledochoduodenostomy. The amount of blood lost during liver parenchyma transection period as well as the length of the operation were specifically recorded in addition to the routine data on a standard anesthetic recording sheet. Postoperative bleeding, bile leakage, liver infarction, liver abscess, subphrenic abscess, and ensuing sepsis were considered as procedure-related complications.
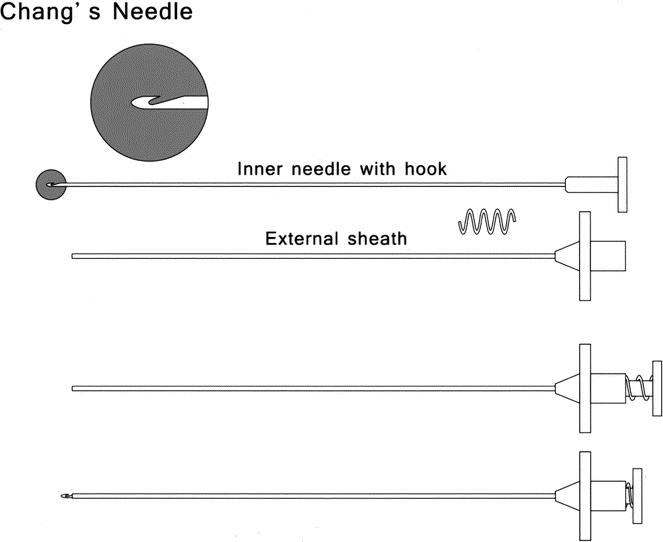
FIGURE 1. A new version of the Chang's needle.
Surgical Technique
A Chang's needle is composed of a straight, 18-cm inner needle, with a hook near its top to catch thread, and a 15-cm-long, 18-gauge stainless steel outer sheath (Fig. 1). A right subcostal incision, with or without extension to the lower xyphoid or to the left subcostal area, was used to open the abdomen. First, the right or left side of the liver was thoroughly mobilized and routinely examined by palpation. Intraoperative ultrasonography was performed to assess the resectability and to determine a suitable division line at least 1 cm away from the tumor. Next, the Chang's needle was applied repeatedly to make overlapping interlocking sutures with No. 1 silks along the inner side of the division line as we had previously published.6 Then, without the use of Pringle's maneuver or any other procedures for blocking hepatic inflow and backflow, the liver parenchyma was divided directly by scissors, electrocautery, or by a Kelly clamp using the clamping and dividing method. Any tubular structures of significant size were suture-ligated for reinforcement. After resections, no fibrin sealant or collagen sheets were applied to the raw liver surface. Routinely, a large caliber drainage tube was placed to the dependent portion if necessary.
In several cases, the tumors were either too big or too close to the inferior vena cava (IVC) and disturbed the placement of the interlocking sutures; thus, the Chang's needle was only used partially (Fig. 2).
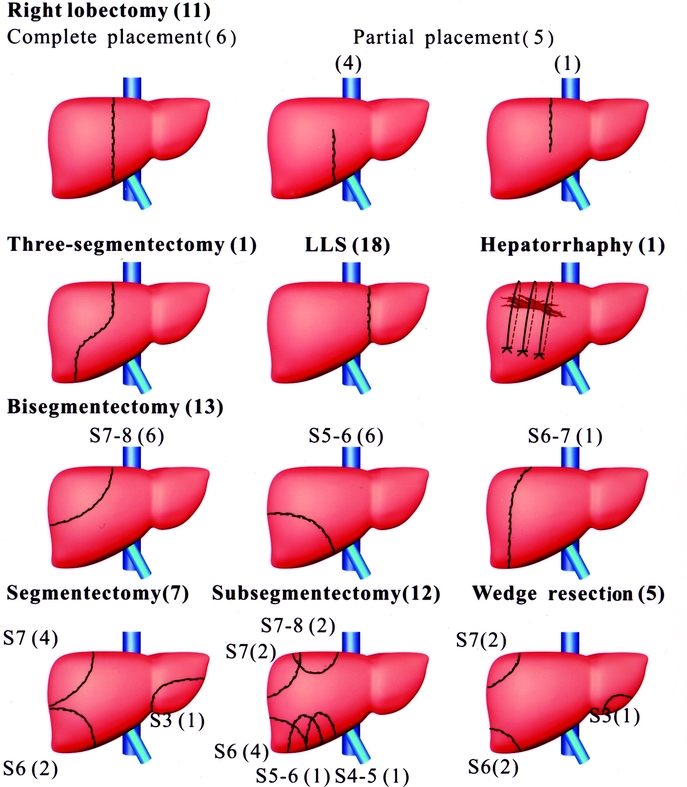
FIGURE 2. Schematic representations of the hepatic resections in current series.
The same technique was also applied on severely lacerated liver trauma patients for compression hemostasis (Fig. 2). Two to 3 bigger bites of the liver parenchyma adequately compressed the liver and stopped the intractable bleeding. This technique, in general, can be applied to hepatic resections away from the IVC area (Fig. 3).
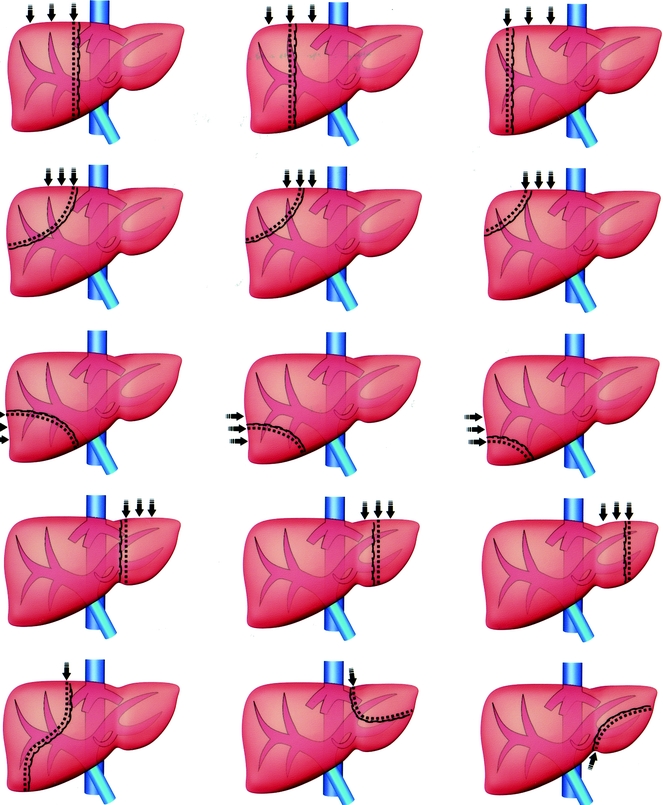
FIGURE 3. Schematic representations of the free, designable hepatic resections suitable for Chang's needle.
RESULTS
There were 37 hepatocellular carcinomas, 4 cholangiocarcinomas, 10 colon metastases, 1 angiomyolipoma, 1 hemangioma, 1 liver trauma, and 15 IHD stones. Nineteen patients had mild to severe degrees of liver cirrhosis and 2 patients had chronic active hepatitis. The remaining 48 patients all had a normal liver. However, in 2 of the 4 patients with cholangiocarcinoma, one liver showed marked cholestasis, while the other showed signs of sepsis before the operation. The Chang's needle was used for hepatic resections on 11 right lobectomies, 1 3-segmentectomy, 14 bisegmentectomies, 7 segmentectomies, 12 subsegmentectomies, 5 wedge resections, 18 left lateral segmentectomies, and 1 hepatorrhaphy (Fig. 2). There was no procedure-related mortality. One patient had severe multiple injuries from a motor vehicle accident and died of multiorgan failure despite the successful hemostasis for her liver laceration. Minor bile leakage occurred in 1 case (1.5%) but healed spontaneously. Several patients with IHD stones experienced minor wound infections as a result of contamination from the pus discharged from the bile duct. In most cases, only minimal hemorrhage was encountered during hepatic transection. The average durations of hepatic transections (Table 1), excluding the time required for the placement of interlocking mattress sutures, were 63.7, 53.6, 24.3, and 25 minutes for right lobectomy, bisegmentectomy, segmentectomy, and left lateral segmentectomy, respectively. It only took 5 minutes for the hemostasis of liver laceration bleeding by compression sutures.
TABLE 1. Hepatic Resections (n = 69) Using the Chang's Needle
DISCUSSION
A successful hepatic resection requires a skillful surgical technique, a safe volume of the remnant liver, and the reduction or elimination of unnecessary ischemic and reperfusion injuries. Skillful surgeons must aim to minimize blood loss during parenchyma division, to secure bleeding or bile leakage from the raw surface of the liver, and to keep remnant major vessels and ducts intact. If all of the above are fulfilled, the postoperative course will be uneventful. Otherwise, cumbersome care becomes necessary.
To reduce blood loss, both inflow and backflow controls are necessary. Several methods can be applied to block the inflow intermittently or continuously at the level of the hepatoduodenal ligament (eg, Pringle's maneuver7), hilar,8–11 or individual segmental branches.11,12 Partial blockage of the individual inflow can avoid ischemia and reperfusion injuries on the remnant liver. To prevent hepatic failure, the determination of the appropriate ischemic time is critical, especially for a cirrhotic liver.13 Backflow can be controlled with IVC exclusion13–15 or hepatic vein.16–21 However, IVC exclusion may compromise the hemodynamic stability; therefore, the use of overloading fluid prior to clamping would add a burden to postoperative recovery.21
Widely accepted specialty instruments, such as the Lin's clamp,1 Cavitron ultrasound aspiration,2 water jet knife,3 Harmonic scapel,4 and microwave coagulator,5 as well as other22–24 lesser known instruments, have been used to facilitate liver resection and to reduce blood loss during parenchymal transection. Comparatively, Chang's needle is cheaper, simpler, more compact, and easier to use. As we have shown in Figures 2 and 3, various kinds of designable nonanatomic hepatic resections are possible with the Chang's needle if the tumor is away from the IVC and if biliary drainage, inflow, and outflow of the remnant liver can be preserved. This maneuver requires neither inflow nor backflow controls; thus, it obviates hilar dissection, spares the complex procedures and management of hepatic vascular exclusion, and avoids the ischemia and reperfusion injury to the remnant liver. In most cases, bleeding during the division of the liver parenchyma was minimal; blood transfusion was thus avoided. Major blood loss was encountered during the learning period due to the selection of improper thread size, the making of insecure ties by the assistant, or in cases with huge tumors where a complete placement of the interlocking sutures was impossible. In a few cases, oozing from the short hepatic vein remained unnoticed after the mobilization and persisted during parenchymal transection. On the whole, blood loss was minimal in well-controlled and securely tied liver resections. Liver congestion, which occurs as a result of secured outflow but unsecured inflow ties, may cause intractable and unnecessary bleeding during transection. In such instances, interlocking sutures over the hepatic vein should be severed and reapplied after dividing the inflow vessels. During the evolution of this technique, hepatic resections through small abdominal incisions were successfully performed using the Chang's needle. Although this operation can be completed with minimal wound, a larger incision gives a wider operation field and makes the completion of interlocking sutures easier in difficult cases. In the entire series, no fibrin sealant or collagen sheets were applied to the raw liver surface to stop the bleeding or bile leakage, yet no postoperative bleeding and only one mild bile leakage was encountered. These preventive measures may be omitted when using the Chang's maneuver since it can offer a secure seal of the raw liver surface.
The advantages of this maneuver can be summarized as follows: 1) the use of cheap, simple, and reusable instrument; 2) no need for the use of Rummel tape in Pringle's maneuver; 3) shortened operation time; 4) reduction or avoidance of blood transfusion in most cases; 5) no need for fibrin glue; 6) fewer ischemic and reperfusion injury of the remnant liver; thus simpler postoperative care; 7) lower level of stress for the surgeon during parenchyma transection due to lack of bleeding; 8) shortened training time for surgeons; and 9) an easier maneuver that allows more surgeons to perform hepatic resections.
CONCLUSION
The preliminary results demonstrate that this maneuver is not only simple and cheap, but also safe for hepatic resections. It allows for designable nonanatomic hepatic resections, which previously involved complicated procedures. Most importantly, this instrument enables less-experienced general surgeons around the world to perform most hepatic resections and makes the operation less dependent on tertiary specialized facilities.
Footnotes
Reprints: Yu-Chung Chang, MD, PhD, Department of Surgery, College of Medicine, National Cheng Kung University, 138 Sheng Li Road, Tainan 70428, Taiwan. E-mail: changyc@mail.ncku.edu.tw.
REFERENCES
- 1.Lin TY. A simplified technique for hepatic resection: the crush method. Ann Surg. 1974;180:285–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hodgson WJB, DelGuercio RM. Surgical technique: preliminary experience in liver surgery using the ultrasonic scalpel. Surgery. 1984;95:230–234. [PubMed] [Google Scholar]
- 3.Persson BG, Jeppsson B, Tranberg KG, et al. Transection of the liver with a water jet. Surg Gynecol Obstet. 1989;168:267–268. [PubMed] [Google Scholar]
- 4.Amaral JF. The experimental development of an ultrasonically activated scalpel for laparoscopic use. Surg Endosc Laparosc. 1994;4:92–99. [PubMed] [Google Scholar]
- 5.Tabuse K, Katsumi M, Kobayashi Y, et al. Microwave surgery: hepatectomy using a microwave tissue coagulator. World J Surg. 1985;9:136–143. [DOI] [PubMed] [Google Scholar]
- 6.Chang YC, Nagasue N, Lin XZ, et al. Easier hepatic resections with a straight needle. Am J Surg. 2001;182:260–264. [DOI] [PubMed] [Google Scholar]
- 7.Pringle JG. Notes on the arrest of hepatic hemorrhage due to trauma. Ann Surg. 1908;48:541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Couinaud CM. A simplified method for controlled left hepatectomy. Surgery. 1985;97:358–361. [PubMed] [Google Scholar]
- 9.Lazorthes F, Chiotasso P, Cheverau P, et al. Hepatectomy with initial suprahilar control of intrahepatic portal pedicles. Surgery. 1993;113:103–108. [PubMed] [Google Scholar]
- 10.Yanaga K, Nishizaki T, Yamamoto K, et al. Simplified inflow control using stapling devices for major hepatic resection. Arch Surg. 1990;131:105–106. [DOI] [PubMed] [Google Scholar]
- 11.Launois B, Jamieson GG. The posterior intrahepatic approach for hepatectomy or removal of segments of the liver. Surg Gynecol Obstet. 1992;174:155–158. [PubMed] [Google Scholar]
- 12.Mazziotti A, Maeda A, Ercolani G, et al. Isolated resection of segment 8 for liver tumors. Arch Surg. 2000;135:1224–1229. [DOI] [PubMed] [Google Scholar]
- 13.Nagasue N, Yukaya H, Ogawa Y, et al. Segmental and subsegmental resections of the cirrhotic liver under hepatic inflow and outflow occlusion. Br J Surg. 1985;72:565–568. [DOI] [PubMed] [Google Scholar]
- 14.Cherqui D, Malassagne B, Colau PI, et al. Hepatic vascular exclusion with preservation of the caval flow for liver resections. Ann Surg. 1999;230:24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elias D, Lasser P, Debane B, et al. Intermittent vascular exclusion of the liver (without vena cava clamping) during major hepatectomy. Br J Surg. 1995;82:1535–1539. [DOI] [PubMed] [Google Scholar]
- 16.Heaney JP, Stanton WK, Halbert DS, et al. An improved technique for vascular isolation of the liver: experiment study and case reports. Ann Surg. 1966;163:237–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bismuth H, Castaing D, Garden OJ. Major hepatic resection under total vascular exclusion. Ann Surg. 1989;210:13–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huget C, Addario-Chieco P, Gavelli A, et al. Technique of hepatic vascular exclusion for extensive liver resection. Am J Surg. 1992;163:602–605. [DOI] [PubMed] [Google Scholar]
- 19.Emre S, Schwatz ME, Katz E, et al. Liver resection under total vascular isolation: variations on a theme. Ann Surg. 1993;217:15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Evans PM, Vogt DP, Mayes JT 3rd, et al. Liver resection using total vascular exclusion. Surgery. 1998;124:807–815. [DOI] [PubMed] [Google Scholar]
- 21.Belghiti J, Noun R, Zante E, et al. Portal trial clamping or hepatic vascular exclusion for major liver resection: a controlled study. Ann Surg. 1996;224:155–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nagao T, Kawano N, Morioka Y. A new instrument for hepatic resection. Surg Gynecol Obstet. 1988;166:269–271. [PubMed] [Google Scholar]
- 23.Ezaki T, Okamura T, Yoshida Y, et al. Hepatic resection with a long sheathed needle: a simple technique. Br J Surg. 1994;81:578. [DOI] [PubMed] [Google Scholar]
- 24.Wendel W. Beiträge zur Chirurgie der Leber. Arch Klin Chirurg. 1911;95:887–895. [Google Scholar]


