Abstract
Objective:
To determine whether robotic-assisted pyeloplasty (RLP) has any significant clinical or cost advantages over laparoscopic pyeloplasty (LP) for surgeons already facile with intracorporeal suturing.
Summary Background Data:
LP has become an established management approach for primary ureteropelvic junction obstruction. More recently, the da Vinci robot has been applied to this procedure (RLP) in an attempt to shorten the learning curve. Whether RLP provides any significant advantage over LP for the experienced laparoscopist remains unclear.
Methods:
Ten consecutive cases each of transperitoneal RLP and LP performed by a single surgeon were compared prospectively with respect to surgical times and perioperative outcomes. Cost assessment was performed by sensitivity analysis using a mathematical cost model incorporating operative time, anesthesia fees, consumables, and capital equipment depreciation.
Results:
The RLP and LP groups had statistically indistinguishable demographics, pathology, and similar perioperative outcomes. Mean operative and total room time for RLP was significantly longer than LP by 19.5 and 39.0 minutes, respectively. RLP was much more costly than LP (2.7 times), due to longer operative time, increased consumables costs, and depreciation of the costly da Vinci system. However, even if depreciation was eliminated, RLP was still 1.7 times as costly as LP. One-way sensitivity analysis showed that LP operative time must increase to almost 6.5 hours for it to become cost equivalent to RLP.
Conclusions:
For the experienced laparoscopist, application of the da Vinci robot resulted in no significant clinical advantage and added substantial cost to transperitoneal laparoscopic dismembered pyeloplasty.
A prospective comparison of transperitoneal robotic (RLP) and laparoscopic (LP) dismembered pyeloplasty was performed, focusing on operative times and cost issues. RLP took significantly longer than LP and was 2.7 times as costly, arguing against a significant advantage for RLP over LP for the experienced urologic laparoscopist.
The management of ureteropelvic junction obstruction has evolved dramatically over the past 20 years in response to the development of new technology. Endoscopic and laparoscopic approaches have largely supplanted open pyeloplasty for the majority of primary ureteropelvic junction obstruction cases.1 Yet laparoscopic pyeloplasty (LP) remains a technically demanding procedure requiring advanced intracorporeal suturing skills.
The development and dissemination of robotic surgical tools, such as the da Vinci system (Intuitive Surgical, Inc., Sunnyvale, CA), have the potential to alter the way urologists approach complex laparoscopic reconstructive procedures. Proponents of da Vinci cite the device's 3-dimensional visualization, damping of tremor, and more sophisticated surgical tools with greater degrees of freedom than traditional laparoscopic instruments.2 Certainly, the device eases the technical challenge of intracorporeal suturing and may make reconstructive laparoscopic procedures more accessible to surgeons without extensive laparoscopic experience. There is mounting evidence that the da Vinci provides significant benefits during laparoscopic radical prostatectomy,3,4 particularly in shortening operating time and decreasing surgeon fatigue. The robot is not, however, without significant disadvantages as compared with traditional laparoscopy. These include greater expense and consumption of operating room resources such as space and the availability of skilled technical staff, complete elimination of tactile feedback, and more limited options for trocar placement.
With its dependence on extensive and precise intracorporeal suturing, pyeloplasty is one of the retroperitoneal laparoscopic procedures most likely to benefit from robotic assistance. For experienced laparoscopic surgeons, however, the tangible benefits of integrating the robot into their surgical pyeloplasty practice remain unclear. To explore this issue, we initiated a prospective comparison of traditional laparoscopic and robotic-assisted dismembered pyeloplasty performed by a single surgeon with extensive prior LP experience.
METHODS
All patients with primary ureteropelvic junction obstruction scheduled for laparoscopic dismembered pyeloplasty during the period from March through November 2004 were candidates for this study. Patients with previous ipsilateral renal surgery of any type were excluded. Data were collected in a prospective fashion, and a single surgeon (L.R.K.) performed all the procedures to minimize operator variability factors. The surgeon had experience with the da Vinci system (>20 cases) and just prior to initiating the da Vinci arm of the study performed 3 robotic pyeloplasty cases to define steps and optimal port placement.
Ten consecutive patients were treated with transperitoneal laparoscopic dismembered pyeloplasty (RLP) using the da Vinci system and compared with a subsequent cohort of 10 consecutive patients undergoing transperitoneal LP. Cystoscopy and stent placement was performed in all cases. For the LP cases, intracorporeal suturing was performed using standard curved needles rather than the Endostitch device (Autosuture Company, Norwalk, CT) to allow equivalent comparison to the RLP cases. An AESOP robotic camera holder (Intuitive Surgical, Inc.) was used during the LP cases to de-emphasize the role of the surgical assistant. To minimize operating room variables, the same surgical team was used for all cases. This group had extensive prior experience with both the da Vinci system (>100 cases) and with standard LP. In addition, a representative from Intuitive Surgical was on-site to aid in setup of the robot as needed.
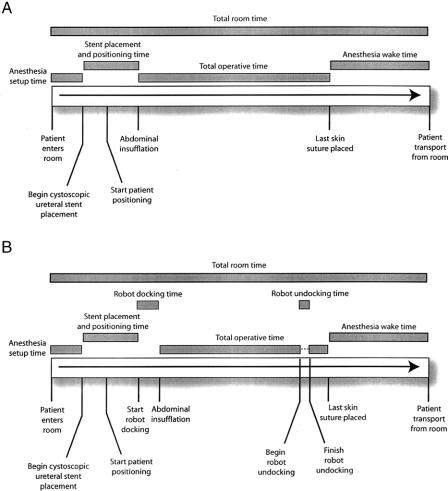
Operative times were recorded in a prospective fashion with an active facilitator monitoring for maximal efficiency. Definitions of the recorded time intervals for RLP and LP are shown graphically in Figure 1. “Total room time” was defined as the elapsed time from the moment the patient entered the operating theater until his or her transport to the recovery room. “Total operative time” was defined as the interval from abdominal insufflation to placement of the last suture in the skin. Note that da Vinci undocking time was recorded separately and was not included in the total operative time of RLP cases. Statistical analysis was performed using the SPSS 11 statistical package (SPSS, Inc., Chicago, IL). The independent Student t test assuming equal variance was used to test significant differences in mean time intervals (P < 0.05).
FIGURE 1. Definitions of recorded times during LP and RLP. A timeline of both LP (a) and RLP (b) is shown with critical events noted. The gray bars above the timeline show the definitions of various recorded time intervals. Note that total operative time for RLP does not include robot undocking time, hence the dashed line.
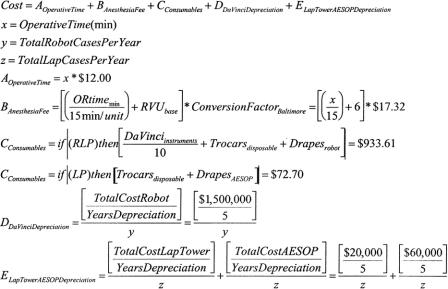
We have previously reported a basic cost comparison between RLP and LP.5 For the cost analysis reported here, we developed a more comprehensive second-generation mathematical model focused on the perioperative costs of RLP or LP (Fig. 2). Cost centers include operative time, anesthesia professional fees, depreciation of the da Vinci robot and laparoscopy video tower equipment, and the cost of specialized consumables such as the AESOP and da Vinci robot drapes, disposable trocars, and da Vinci instruments. To simplify the analysis, factors that did not differ between RLP and LP were excluded from the model. Examples include costs for surgeon professional fees, inpatient room and board, analgesics and postoperative visits, and the standard disposable laparoscopic instruments used in both cases. Anesthesiologist's professional fees were derived from 2004 Medicare reimbursement rates. Operating room time includes updated direct and indirect costs for the second half of 2004 and was provided by our hospital administration. Consumable costs represent the cost for replacement of items for the operating room and not charges to patients. Depreciation of the da Vinci system is based on 5 years with an institutional use of 150 da Vinci cases per year. Likewise, depreciation of the laparoscopy tower equipment and AESOP was over 5 years with an estimated 400 cases per year. These numbers are estimates based on our current caseload at Johns Hopkins. We routinely use the AESOP robot to hold the camera in all our laparoscopic cases. da Vinci instruments were estimated to have a lifespan of 10 cases. Nondisposable standard laparoscopic instruments were excluded from depreciation analysis either because they are used in both RLP and LP or because their long lifespan (ie, needle drivers, nondisposable trocars) made their per-case cost negligible. Sensitivity analysis was performed using TreeAge Pro Healthcare software (TreeAge Software, Inc., Williamstown, MA).
FIGURE 2. Cost analysis model comparing the perioperative costs of robotic and laparoscopic pyeloplasty.
RESULTS
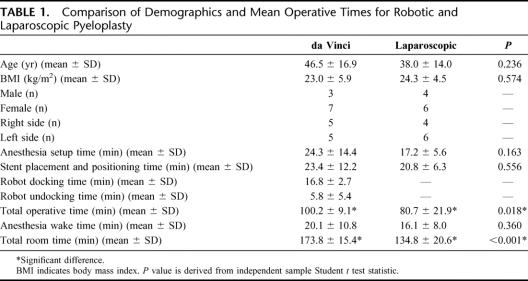
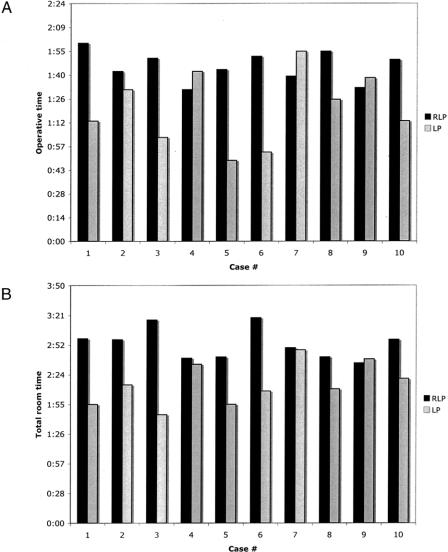
The demographics of patients undergoing RLP and LP are shown in Table 1. There were no significant differences in age, body mass index, sex, surgical side, presence of crossing vessels, or need for renal pelvic reduction. Despite the theoretical technical advantages of the da Vinci robot for intracorporeal suturing, total operative time for the LP cases (80.7 ± 21.9 minutes) was significantly shorter than for RLP (100.2 ± 9.1 minute; P = 0.018; Table 1). Note that operative time does not include robot docking or undocking, which might bias it toward LP. A similar advantage for LP was observed with total room time (134.8 ± 20.6 minutes) as compared with RLP (173.8 ± 15.4 minutes; P < 0.001). In contrast, no significant differences were found for anesthesia setup time, stent placement and positioning time or anesthesia wake time. When operative time or total room time were plotted against consecutive case number, no significant learning curve trends were observed for RLP or LP (Fig. 3).
TABLE 1. Comparison of Demographics and Mean Operative Times for Robotic and Laparoscopic Pyeloplasty
FIGURE 3. Evaluating the learning curve for LP and RLP. Operative time (a) and total room time (b) were plotted against consecutive case number for both LP and RLP. No significant downward trend in times was observed for these cases arguing against a significant learning curve effect.
There were no intraoperative complications and no significant differences were observed in estimated blood loss or length of stay following LP or RLP. One patient in the RLP group developed a urine leak at home several days after removal of her flank suction drain. This necessitated replacement of the drain percutaneously after which the leak sealed and she had an otherwise unremarkable course. No urine leaks were identified in the LP patients. Although no failures were noted in either group, mean follow-up in this series was only 5.6 ± 2.2 months, which is too short to assess pyeloplasty success rates.
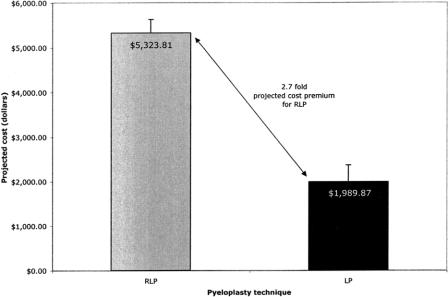
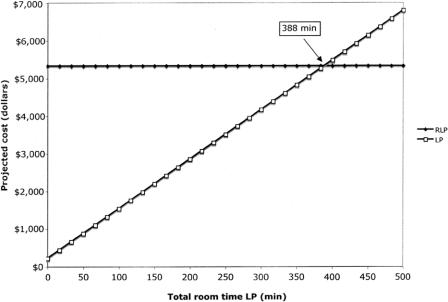
Projected perioperative costs were calculated from a mathematical model (Fig. 2). Longer operative time combined with substantial expense for robot depreciation and consumables made RLP a much more expensive procedure than LP (2.7 times; Fig. 4). One-way sensitivity analysis holding RLP operative time constant projected that LP operative time must increase to 388 minutes (6.5 hours) for RLP to be cost equivalent with LP (Fig. 5).
FIGURE 4. Projected costs of robotic and laparoscopic pyeloplasty derived from the perioperative cost model. Error bars represent standard deviation.
FIGURE 5. One-way sensitivity analysis. RLP total room time was held constant and LP total room time was varied over a range of 0 to 500 minutes. Cost equivalence between RLP and LP would be reached at 388 minutes of operative time for LP.
da Vinci robot depreciation based on an estimated utilization of 150 cases per year (of all types) resulted in a $2000 premium for da Vinci use per case solely due to depreciation of capital equipment. This represents 46% of the total projected cost for RLP. However, even if da Vinci depreciation was eliminated from the model, RLP was still 1.7 times more costly than LP based on increased consumables and operative time costs.
DISCUSSION
The da Vinci robot is clearly a marvel of technology that has the potential to change the practice of urologic surgery. Three-dimensional vision, sophisticated wristed instruments, dampening of tremor, and excellent ergonomics all favor its application to a variety of urologic laparoscopic procedures. However, disadvantages such as high cost, loss of tactile feedback, and consumption of operating room resources counsel a reasoned assessment of da Vinci's application. For some procedures, most notably the laparoscopic radical prostatectomy, suggestions have been made that the robot shortens operative time and eases the learning curve. Similar evidence in the case of LP, however, is currently lacking.
Several groups have reported the use of the da Vinci system for performing RLP with favorable results.6–8 In this study, we performed a direct comparison of primary laparoscopic dismembered pyeloplasty performed with and without the da Vinci by a single surgeon experienced with both the robotic and traditional laparoscopic techniques. As many variables as possible, such as the experience of the operating room staff, were kept constant to provide a valid comparison. Despite the theoretical suturing advantages of the da Vinci, the RLP cases had significantly longer mean operative (by 19.5 minutes) and total room (by 39.0 minutes) times than the LP cases. In contrast, anesthesia setup and wake times, ureteral stenting and positioning times, age, and body mass index were not significantly different between the 2 techniques.
To evaluate the potential cost difference between RLP and LP, we developed a mathematical cost model. We previously reported a basic cost analysis comparing LP and RLP.5 The current model refines this analysis by updating the operative time costs for 2004 and including cost centers for anesthesia professional fees (a time-dependent variable) as well as depreciation costs for the AESOP robotic camera holder. AESOP was included in this analysis to assure that a skilled assistant was not required to hold the laparoscope in either the LP or RLP cases. The second-generation cost model predicts that RLP will be far more costly than LP (2.7 times). This discrepancy is due not only to longer room times but also to more than 10 times greater consumables costs and the oppressive capital equipment depreciation costs associated with a million-dollar robot. Certainly, the impact of depreciation would be blunted if the total institutional volume of robot cases were to dramatically increase. For example, increasing the da Vinci utilization to 400 cases a year would decrease the per-case depreciation premium from $2000 to only $750. Certainly, this increased volume will not come from LP, although the rising number of robotic radical prostatectomy cases will have a positive impact. It remains unclear, however, whether most academic tertiary referral centers will be able to support such a high volume of robot cases, not to mention smaller community hospitals that might be considering a robot purchase.
Our results differ significantly from those reported by Gettman et al in 2002.9 In that study, mean LP operative time (235 minutes) was 1.7 times that for RLP (140 minutes). However, significant limitations hamper interpretation of these previous results. Only 4 cases of RLP and LP were reported, and no statistical analysis was done to determine significance of these differences. Likewise, the LP cases were historical cases performed up to 2 years previously, time data were not collected prospectively, and variables such as the operating room staff were not kept constant. Finally, the impact of resident and fellow training on operative times in the LP cases was not clarified. These limitations have been addressed in the current report.
The purpose of this study is not to discourage the use of the da Vinci system for LP. Certainly, for surgeons unfamiliar with intracorporeal suturing, the robot may lower the learning curve for LP. Rather, this report should serve as a cautionary tale arguing against the indiscriminate application of the da Vinci based only on a perception that it should accelerate suturing. Our results suggest that, for surgeons facile with intracorporeal suturing, dependence on the da Vinci robot adds little speed or quality advantage to the LP procedure and results in substantially greater costs.
Footnotes
Reprints: Richard E. Link, MD, PhD, Scott Department of Urology, Baylor College of Medicine, 6560 Fannin, Suite 2100, Houston, TX 77030. E-mail: rlink@www.urol.bcm.tmc.edu.
REFERENCES
- 1.Baldwin DD, Dunbar JA, Wells N, et al. Single-center comparison of laparoscopic pyeloplasty, Acucise endopyelotomy, and open pyeloplasty. J Endourol. 2003;17:155–160. [DOI] [PubMed] [Google Scholar]
- 2.Eichel L, Ahlering TE, Clayman RV. Role of robotics in laparoscopic urologic surgery. Urol Clin North Am. 2004;31:781–792. [DOI] [PubMed] [Google Scholar]
- 3.Menon M, Tewari A, Peabody JO, et al. Vattikuti Institute prostatectomy. A technique of robotic radical prostatectomy for management of localized carcinoma of the prostate: experience of over 1100 cases. Urol Clin North Am. 2004;31:701–717. [DOI] [PubMed] [Google Scholar]
- 4.Smith JA. Robotically assisted laparoscopic prostatectomy: an assessment of its contemporary role in the surgical management of localized prostate cancer. Am J Surg. 2004;188(suppl 4A):63–67. [DOI] [PubMed] [Google Scholar]
- 5.Bhayani SB, Link RE, Varkarakis IM, et al. Complete da Vinci pyeloplasty vs. laparoscopic pyeloplasty: cost analysis. J Endourol. In press. [DOI] [PubMed]
- 6.Bentas W, Wolfram M, Brautigam R, et al. Da Vinci robot assisted Anderson-Hynes dismembered pyeloplasty: technique and 1 year follow-up. World J Urol. 2003;21:133–138. [DOI] [PubMed] [Google Scholar]
- 7.Peschel R, Neururer R, Bartsch G, et al. Robotic pyeloplasty: technique and results. Urol Clin North Am. 2004;31:737–741. [DOI] [PubMed] [Google Scholar]
- 8.Gettman MT, Neururer R, Bartsch G, et al R. Anderson-Hynes dismembered pyeloplasty performed using the da Vinci robotic system. Urology. 2002;60:509–513. [DOI] [PubMed] [Google Scholar]
- 9.Gettman MT, Peschel R, Neururer R, et al. A comparison of laparoscopic pyeloplasty performed with the da Vinci robotic system versus standard laparoscopic techniques: initial clinical results. Eur Urol. 2002;42:453–457; discussion 457–458. [DOI] [PubMed]